Abstract
Two or more antihypertensive agents are required to achieve blood pressure control for the most hypertensive patients. However, comparison of clinical outcomes between fixed‐dose combinations (FDC) and free‐equivalent combinations of renin‐angiotensin system (RAS) inhibitor and thiazide diuretic is lacking nowadays. Patients who were newly diagnosed with hypertension between July 1st, 2008 and December 31st, 2011 and prescribed with FDC (n = 13 176) or free combinations of RAS inhibitors and thiazide diuretic (n = 4392) were identified from the National Health Insurance Research Database of Taiwan and matched in 3:1 ratio using the propensity score method. The primary end point was major adverse cardiovascular events (MACE). The secondary end points were hospitalization of heart failure, new diagnosis of chronic kidney disease, and the initiation of dialysis. Compared with he FDC group was associated with better medication adherence compared with the free combination group. FDC of RAS inhibitor and thiazide diuretic reduced MACE (hazard ratio [HR]: 0.85; 95% confidence interval [CI]: 0.74‐0.97; P = 0.017), hospitalization for heart failure and initiation of dialysis compared with the free combination regimens. The outcome benefits of FDC was mainly driven by reduced cardiovascular and renal events in the patients with proportion of days covered <80%. In this retrospective claims database analysis, compared with the free combination regimens, the use of FDC of RAS inhibitor and thiazide diuretic was associated with improved medication compliance and clinical outcomes in the management of hypertension, particularly in the patients with poor medication adherence.
1. INTRODUCTION
Hypertension has long been recognized as a global public health challenge and the leading preventable risk factor for cardiovascular diseases (CVD).1, 2, 3 Clinical studies had demonstrated that adequate blood pressure control substantially reduces end organ damage and improves cardiovascular outcomes.4, 5 Despite enormous advances in medical therapy, the control rates of hypertension worldwide seem to remain low,6 specifically 47% in the United States,7 34% in England, 66% in Canada,8 and 25% in Taiwan.9 This leads to the incentive to explore more effective antihypertensive regimens.
Two or more antihypertensive agents are usually required to achieve desirable blood pressure control for the majority of hypertensive patients.10, 11, 12 However, medication nonadherence and lack of persistence have been recognized as critical factors of inadequate blood pressure control.13, 14 Previous study have demonstrated that single‐pill fixed‐dose combinations (FDC), compared with free‐equivalent combinations,15 are more effective in improving medication compliance and therefore may possibly result in the reduction of major adverse cardiovascular events (MACE) and healthcare expenditure.16 Despite the numerous combinations of angihypertensive agents, the outcome data of FDC regimens in hypertenstion treatment is still lacking. The combination of renin‐angiotensin system (RAS) inhibitor and thiazide diuretic is a well accepted and increasingly prescribed regimen in Taiwan, particularly in drug‐naïve hypertensive patients.17 Given the lack of large‐scale randomized controlled trials, we aimed to perform a retrospective claims database analysis to compare the clinical outcomes of FDC vs free combinations of RAS inhibitor and thiazide diuretic in real‐world hypertension management.
2. METHODS
2.1. Data source
We used the National Health Insurance Research Database (NHIRD) of Taiwan to conduct this retrospective cohort analysis. The National Health Insurance (NHI) program, a state operated, universal health insurance program implemented since 1995, covers 99% of the entire Taiwanese population.18, 19, 20, 21 The NHIRD of Taiwan contains inpatient and outpatient registries from all medical facilities contracted with the National Health Insurance Administration and provides patient information on gender, birthday, diagnosis, prescribed medications, and invasive procedures. These data could be identified using the diagnosis and procedure codes of the International Clinical Diseases, the Ninth Revision, Clinical Modification (ICD‐9‐CM). The Bureau of NHI encrypted all personal identifiers before information was released to researchers. Confidentiality was addressed by following the data processing regulations set by the Bureau of NHI. The Institutional Review Board approval was waived.
2.2. Study cohort and design
Figure 1 illustrates the flow chart of patient enrollment. Patients with the diagnosis of hypertension (ICD‐9‐CM: 401.x) between January 2008 and December 2012 were identified from the NHIRD of Taiwan. To ensure all the patients enrolled in this study were newly diagnosed with hypertension, we excluded the patients who were diagnosed with hypertension or prescribed with any antihypertensive drug before July 1st, 2008. We also excluded those who were diagnosed after December 31st, 2011 to ensure that all the patients had a least 1 year of follow‐up in the present study. This study aimed to compare the clinical outcomes of FDC vs free combination of RAS inhibitor and thiazide diuretic. The index date was defined as the date of the first prescription of single‐pill fixed‐dose combination of RAS inhibitor and thiazide diuretic in the FDC group and the concomitant prescription of free components of RAS inhibitor and thiazide diuretic in the free combination group. Considering there were occasional users of the study drugs, we excluded the patients who were not prescribed with the study drugs uninterruptedly for at least 3 months. This 3‐month period was chosen because the NHI reimbursement policy of Taiwan allows a maximum length of 3 months for medication refills for chronic illnesses. We also excluded the patients who were aged <18 years, who were diagnosed with pregnancy or cancer, and those with concurrent prescription of angiotensin‐converting enzyme (ACE) inhibitor and angiotensin receptor blocker (ARB) or switch between these two classes of drugs during the study period.
Figure 1.
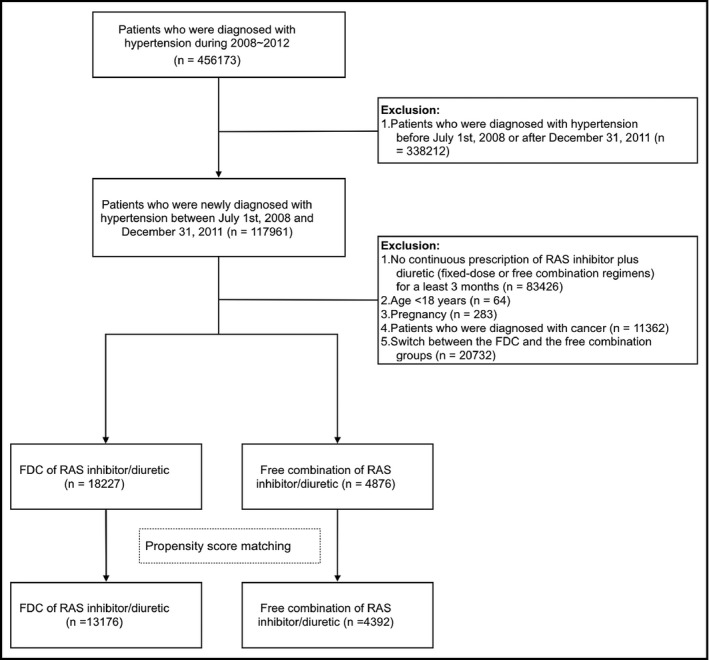
Patient enrollment. FDC, fixed‐dose combination; RAS, renin‐angiotensin system
Propensity score matching was performed to eliminate the differences in the baseline characteristics of the two study groups. The variables used in the matching process included age, gender, coronary artery disease (including a history of myocardial infarction, percutaneous coronary intervention (PCI), coronary artery bypass surgery (CABG), peripheral artery disease, congestive heart failure, diabetes mellitus, dyslipidemia, chronic kidney disease (CKD), Carlson score, and baseline medications (antiplatelet agent, calcium channel blocker [CCB], beta‐blocker, other classes of antihypertensive drugs, statins, and oral antidiabetic agents). The FDC group was matched in 3:1 ratio to the free combination group.
2.3. Study end points and follow‐up
The primary end point was MACE, including all‐cause mortality, myocardial infarction (410‐410.9), stroke (430‐437), and coronary revascularization (PCI: 36.0‐36.03 and 36.05‐36.09; CABG: 36.1‐36.99 and V45.81). Mortality was identified using death certificate data files of the NHIRD of Taiwan. The secondary end points included hospitalization for heart failure (428.0‐428.10), new diagnosis of CKD (585), and the initiation of dialysis. All patients were followed up for at least 1 year or till the occurrence of clinical end points, whichever came first. Medication adherence was assessed using proportion of days covered (PDC), which is defined as the total number of days covered by the study drugs divided by the total number of days of the study period.
2.4. Statistical analysis
Continuous variables were compared using Student's t test, and categorical variables were analyzed by the Chi‐square test. Data are presented as means, standard deviations, or percentages. Cox proportional hazard model was used for time to event analysis. Analysis of clinical outcomes was further stratified by medication adherence (PDC ≥80% and PDC <80%). All analyses were conducted using SAS Statistical Software, Version 9.3 (SAS Institute Inc, Cary, NC) and R Statistical Software, Version 3.0.1 (the R Foundation for Statistical Computing, Vienna, Austria). A P value <0.05 was considered to be statistically significant.
3. RESULTS
Table 1 demonstrates the demographic and baseline characteristics of the two study groups. From July 1st, 2008 to December 31st, 2011, a total of 13 176 hypertensive patients who received FDC and 4392 patients who received free combinations of RAS inhibitors and thiazide diuretics were identified from the NHIRD of Taiwan and matched in 3:1 ratio using the propensity score method. The mean age of the study patients was 58, with 53% of them with male. Approximately 23% of the study patients had diabetes mellitus, 19% had dyslipidemia, 4.4% had CKD, and 10% had previous documented CVD, including coronary artery disease, peripheral artery disease, and heart failure. The mean Carlson score was 1.5 for both the two groups. No significant difference was observed between the two groups in terms of demographic characteristics, comorbidities, and baseline medications after propensity score matching.
Table 1.
Baseline characteristics
| Before matching | After matching | |||||
|---|---|---|---|---|---|---|
| Fixed‐dose combination | Free combination | P‐value | Fixed‐dose combination | Free combination | P‐value | |
| (n = 18 227) | (n = 4876) | (n = 13 176) | (n = 4392) | |||
| Demographics | ||||||
| Male, n (%) | 9785 (53.7) | 2633 (54.0) | 0.707 | 6968 (52.9) | 2352 (53.6) | 0.453 |
| Age, mean (SD) | 58.72 (13.42) | 60.01 (14.20) | <0.001 | 58.79 (13.48) | 58.98 (13.80) | 0.420 |
| Age, n (%) | ||||||
| 18‐29 | 179 (1.0) | 47 (1.0) | <0.001 | 124 (0.9) | 46 (1.0) | 0.981 |
| 30‐39 | 1057 (5.8) | 269 (5.5) | 741 (5.6) | 251 (5.7) | ||
| 40‐49 | 3446 (18.9) | 897 (18.4) | 2621 (19.9) | 859 (19.6) | ||
| 50‐59 | 5397 (29.6) | 1287 (26.4) | 3727 (28.3) | 1235 (28.1) | ||
| 60‐69 | 3939 (21.6) | 1028 (21.1) | 2798 (21.2) | 935 (21.3) | ||
| >69 | 4209 (23.1) | 1348 (27.6) | 3165 (24.0) | 1066 (24.3) | ||
| Comorbidities, n (%) | ||||||
| Diabetes mellitus | 4293 (23.6) | 1166 (23.9) | 0.612 | 3040 (23.1) | 1021 (23.2) | 0.828 |
| Dyslipidemia | 3512 (19.3) | 984 (20.2) | 0.159 | 2534 (19.2) | 876 (19.9) | 0.311 |
| Chronic kidney disease | 919 (5.0) | 319 (6.5) | <0.001 | 585 (4.4) | 213 (4.8) | 0.277 |
| Coronary artery disease | 1599 (8.8) | 533 (10.9) | <0.001 | 1056 (8.0) | 383 (8.7) | 0.148 |
| Peripheral artery disease | 244 (1.3) | 78 (1.6) | 0.189 | 185 (1.4) | 64 (1.5) | 0.854 |
| Congestive heart failure | 570 (3.1) | 299 (6.1) | <0.001 | 73 (0.6) | 32 (0.7) | 0.235 |
| Charlson score, mean (SD) | 1.16 (1.56) | 1.28 (1.62) | <0.001 | 1.10 (1.51) | 1.14 (1.53) | 0.201 |
| Charlson score, n (%) | ||||||
| 0 | 9481 (52.0) | 2354 (48.3) | <0.001 | 7042 (53.4) | 2305 (52.5) | 0.563 |
| 1 | 2508 (13.8) | 710 (14.6) | 1752 (13.3) | 590 (13.4) | ||
| 2 | 3087 (16.9) | 838 (17.2) | 2243 (17.0) | 747 (17.0) | ||
| 3+ | 3151 (17.3) | 974 (20.0) | 2139 (16.2) | 750 (17.1) | ||
| Baseline medications, n (%) | ||||||
| Antiplatelet agents | 5350 (29.4) | 1586 (32.5) | <0.001 | 3754 (28.5) | 1308 (29.8) | 0.106 |
| Calcium channel blocker | 10 728 (58.9) | 3072 (63.0) | <0.001 | 8267 (62.7) | 2758 (62.8) | 0.964 |
| Beta‐blocker | 6954 (38.2) | 2065 (42.4) | <0.001 | 5217 (39.6) | 1731 (39.4) | 0.845 |
| Other antihypertensive drugs | 887 (4.9) | 351 (7.2) | <0.001 | 373 (2.8) | 114 (2.6) | 0.442 |
| Statins | 3778 (20.7) | 1057 (21.7) | 0.153 | 2671 (20.3) | 922 (21.0) | 0.315 |
| Oral antidiabetic agents | 4827 (26.5) | 1243 (25.5) | 0.168 | 3439 (26.1) | 1100 (25.0) | 0.173 |
The use of FDC was associated with better medication adherence (PDC 58.01% vs 46.96%; P < 0.001) compared with the free combination group (Table 2). Regarding the clinical outcomes, FDC was associated with a significant reduction in MACE compared with the free combination regimen (hazard ratio [HR]: 0.85; 95% confidence interval [CI]: 0.74‐0.97; P = 0.017; Table 3 and Figure 2). The FDC group also had better outcomes in terms of hospitalization for heart failure (HR 0.76; 95% CI 0.6‐0.95; P = 0.015) and initiation of dialysis (HR 0.69, 95% CI 0.53‐0.89; P = 0.005). There was no significant difference between the two groups regarding new diagnosis of CKD (HR 0.91; 95% CI 0.81‐1.01; P = 0.087). We further stratified the outcome analysis based on PDC (Table S1). In patients with PDC ≥80%, the clinical outcomes did not differ significantly between the two groups (Figure 3). On the other hand, among the patients with PDC <80%, FDC was associated with better survival free from MACE and all the secondary end points (Figure 4).
Table 2.
Comparison of follow‐up duration and medication adherence
| Fixed‐dose combination | Free combination | P‐value | |
|---|---|---|---|
| Duration of follow‐up (d), mean (SD) | 887.89 (456.09) | 830.22 (462.50) | <0.001 |
| Proportion of days covered (PDC), mean (SD) | 58.01% (33.01%) | 46.96% (36.52%) | <0.001 |
| PDC ≥80%, n (%) | 4670 (35.4) | 1240 (28.2) | <0.001 |
Table 3.
Comparison of clinical outcomes of fixed‐dose vs free combination of RAS inhibitor and thiazide diuretic
| Outcomes | Group | Event number | Person‐year | Incidence rate (per 100 person‐year) | Hazard ratio (95% confidence interval) | P‐value |
|---|---|---|---|---|---|---|
| Primary end point (MACE) | Free combination | 293 | 10 941.830 | 2.678 | 1 | (Reference) |
| Fixed‐dose | 785 | 34 495.321 | 2.276 | 0.85 (0.74‐0.97) | 0.017 | |
| Hospitalization for heart failure | Free combination | 108 | 11 258.419 | 0.959 | 1 | (Reference) |
| Fixed‐dose | 257 | 35 402.573 | 0.726 | 0.76 (0.6‐0.95) | 0.015 | |
| New diagnosis of CKD | Free combination | 407 | 10 751.701 | 3.785 | 1 | (Reference) |
| Fixed‐dose | 1164 | 33 971.951 | 3.426 | 0.91 (0.81‐1.01) | 0.087 | |
| New initiation of dialysis | Free combination | 80 | 11 343.786 | 0.705 | 1 | (Reference) |
| Fixed‐dose | 173 | 35 600.836 | 0.486 | 0.69 (0.53‐0.89) | 0.005 |
CKD, chronic kidney disease; MACE, major adverse cardiac events; RAS, renin‐angiotensin system.
Figure 2.
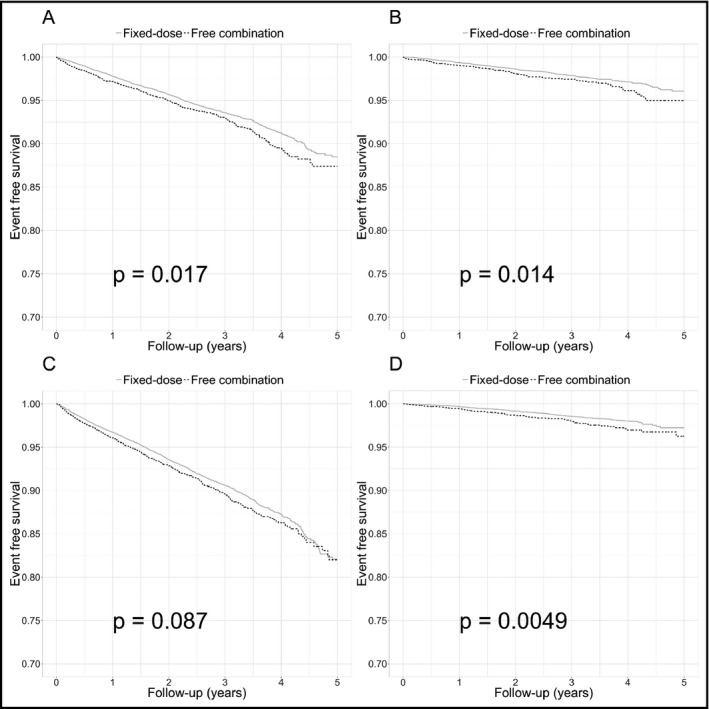
Comparison of event‐free survival between fixed‐dose vs free combinations of RAS inhibitor and thiazide diuretic. A, major adverse cardiac events; B, hospitalization for heart failure; C, new diagnosis of chronic kidney disease; D, initiation of dialysis. RAS, renin‐angiotensin system
Figure 3.
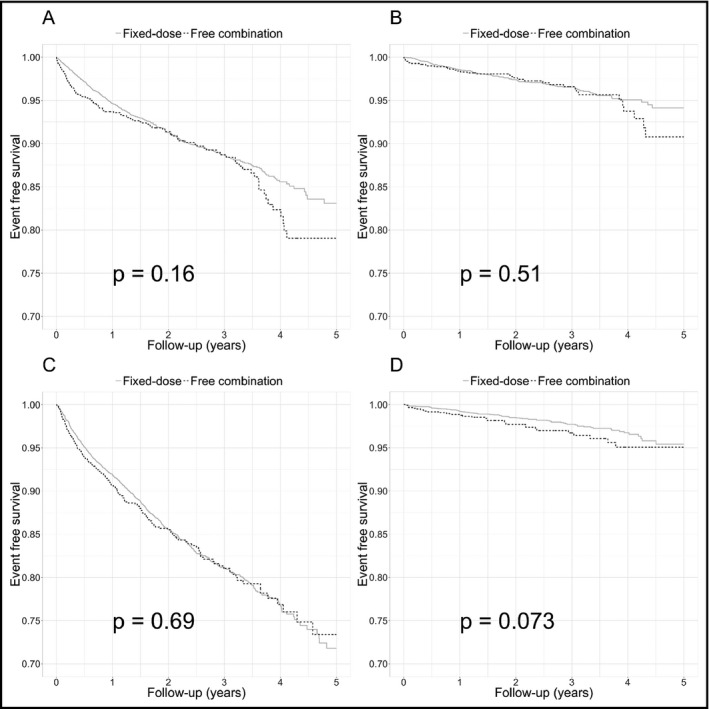
Comparison of event‐free survival in patients with PDC ≥80% who received fixed‐dose vs free combinations of RAS inhibitor and thiazide diuretic. A, major adverse cardiac events; B, hospitalization for heart failure; C, new diagnosis of chronic kidney disease; D, initiation of dialysis. PDC, proportion of days covered; RAS, renin‐angiotensin system
Figure 4.
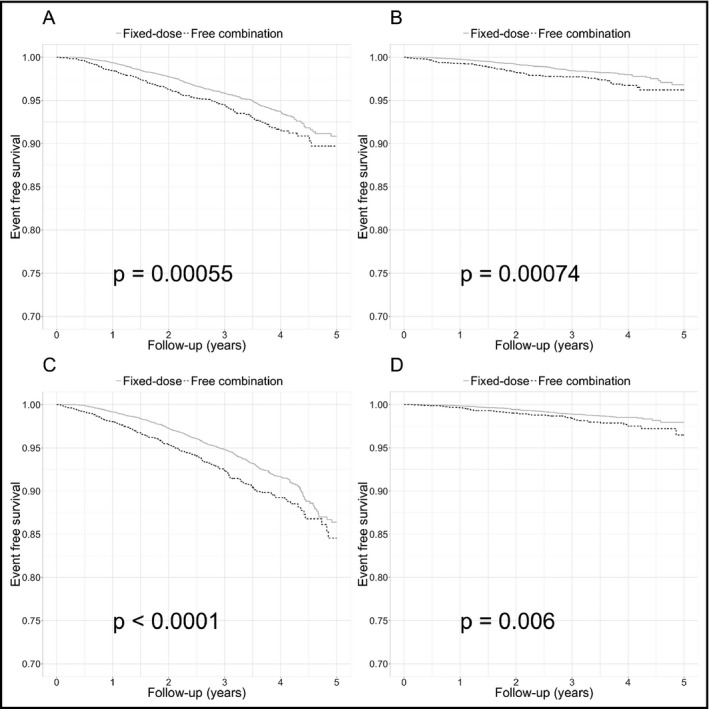
Comparison of event‐free survival in patients with PDC <80% who received fixed‐dose vs free combinations of RAS inhibitor and thiazide diuretic. A, major adverse cardiac events; B, hospitalization for heart failure; C, new diagnosis of chronic kidney disease; D, initiation of dialysis. PDC, proportion of days covered; RAS, renin‐angiotensin system
4. DISCUSSION
In this retrospective cohort analysis, we used the NHIRD of Taiwan to evaluate the clinical outcomes of fixed‐dose and free combinations of RAS inhibitor plus thiazide diuretic. We found that compared with the free combination regimen group, the FDC of RAS inhibitor and thiazide diuretic was associated with better medication adherence and persistence and improved clinical outcomes in the treatment of hypertension. Subgroup analysis showed that the FDC and free combination regimens had comparable outcomes in patients with good medication adherence (PDC ≥80%). In patients with PDC <80%, the FDC of RAS inhibitor and thiazide diuretic was associated with better outcomes compared with the free combination regimens.
Several classes of blood pressure lowering drugs, including diuretics, ACE inhibitors, ARB, CCBs, and beta‐blockers, had been proven to be effective in reducing blood pressure and preventing morbidity and mortality of uncontrolled hypertension.22, 23, 24, 25, 26, 27 Diuretics enhance the antihypertensive efficacy of multidrug regimens and are more affordable than other antihypertensive agents.28 The benefits of diuretic‐based therapy in the prevention of cardiovascular disease and stroke have been established in the earliest randomized clinical trials in the 1960s and in the contemporary studies.25, 29 Among the different classes of diuretics, thiazide diuretics have been regarded as the cornerstone of antihypertensive therapy, especially in the elderly (the Systolic Hypertension in the Elderly Program [SHEP] study)30 and the African‐Americans (the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack [ALLHAT] study).25 On the other hand, the RAS is a major therapeutic target in hypertension management, especially for patients with high cardiovascular risk, left ventricular dysfunction, and heart failure.31, 32, 33, 34, 35 The Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) study has revealed that benazepril plus amlodipine decreases the rate of cardiovascluar events compared to benazepril plus hydrochlorothiazide.36 Nevertherless, the combiations of RAS inhibitors and thiazide diuretics are still widely prescribed in contemporary hypertension management. In Taiwan, an increasing number of treatment‐naïve patients receive FDC of RAS inhibitor and thiazide diuretic as their first drug for hypertension treatment.36
The single‐pill combinations of antihypertensive drugs have been shown to improve patient compliance37, 38, 39, 40, 41 and have therefore been recommended by current guidelines in hypertension management.42, 43, 44, 45 However, no trial has ever been performed to compare the clinical outcomes of the FDC of RAS inhibitor and thiazide diuretic vs the free combinations of separate drugs. In the present study, we found that FDC regimens was associated with improved medication adherence and persistence compared with the free combination regimens, which is in line with results of the previous studies. We hypothesized that through the improvement in medication compliance, FDC may have beneficial impact on cardiovascular and renal outcomes in patients with hypertension. Furthermore, the benefits of FDC seemed to be driven by the improved outcomes in patients with PDC <80%. Therefore, in the management of hypertension, patients with poor adherence should be identified and clinicians may consider FDC as a reasonable alternative in this particular subgroup to improve medication compliance and long‐term prognosis.
4.1. Study limitations
There are severel inherent limitations in this retrospective claims database analysis. The NHIRD of Taiwan collected prescription information and therefore does not contain data on laboratory tests or blood pressure recods. The lack of blood pressure records at baseline and follow‐up visits precludes the analysis of the control rate of hypertension in our study cohorts. Despite the use of propensity score matching to balance the difference in the prescriptions of statins and hypoglycemic agents, we could not exclude the potential differences in the levels of low‐density lipoprotein cholesterol and glycohemoglobin between the two groups, which have been shown to affect the long‐term cardiovascular outcomes in hypertensive patients. Similarly, the lack of creatinine data may confound the secondary end points of new CKD and the initiation of dialysis. Furthemore, the reasons behind the prescription of FDC or free combination regimens was not provided by the NHIRD of Taiwan. The preferences of patients or physicians may also lead to selection bias in our study. Finally, the study cohort was limited to the Taiwanese population and therefore the results of the present study may not be generalized to other popluations.
5. CONCLUSIONS
In this retrospective claims database analysis, compared with the free combination regimens, the FDC of RAS inhibitor and thiazide diuretic was associated with improved medication compliance and clinical outcomes in the management of hypertension, particularly in the patients with poor medication adherence.
CONFLICT OF INTEREST
None.
Supporting information
Ho C‐T, Tung Y‐C, Chou S‐H, et al. Clinical outcomes in hypertensive patients treated with a single‐pill fixed‐dose combination of renin‐angiotensin system inhibitor and thiazide diuretic. J Clin Hypertens. 2018;20:1731–1738. 10.1111/jch.13413
Chien‐Te Ho, Ying‐Chang Tung and Pao‐Hsien Chu contributed equally to this work.
Funding information
This study is supported by grant from Chang Gung Memorial Hospital (grant No. CORPG3F0571, CORPG3G0751, and CMRPG3E1051).
REFERENCES
- 1. Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436‐1442. [DOI] [PubMed] [Google Scholar]
- 2. Angell SY, De Cock KM, Frieden TR. A public health approach to global management of hypertension. Lancet. 2015;385:825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2224‐2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA. 1996;275:1571‐1576. [PubMed] [Google Scholar]
- 5. Collaboration B. Effects of different blood‐pressure‐lowering regimens on major cardiovascular events: results of prospectively‐designed overviews of randomised trials. Lancet. 2003;362:1527‐1535. [DOI] [PubMed] [Google Scholar]
- 6. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high‐, middle‐, and low‐income countries. JAMA. 2013;310:959‐968. [DOI] [PubMed] [Google Scholar]
- 7. Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599‐606. [DOI] [PubMed] [Google Scholar]
- 8. Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross‐sectional study. BMJ Open. 2013;3:e003423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Su T‐C, Bai C‐H, Chang H‐Y, et al. Evidence for improved control of hypertension in Taiwan: 1993–2002. J Hypertens. 2008;26:600‐606. [DOI] [PubMed] [Google Scholar]
- 10. Gradman AH. Strategies for combination therapy in hypertension. Curr Opin Nephrol Hypertens. 2012;21:486‐491. [DOI] [PubMed] [Google Scholar]
- 11. Gorostidi M, de la Sierra A. Combination therapy in hypertension. Adv Ther. 2013;30:320‐336. [DOI] [PubMed] [Google Scholar]
- 12. Blood Pressure Lowering Treatment Trialists' Collaboration . Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger people: meta‐analysis of randomised trials. BMJ. 2008;336:1121‐1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Elliott WJ. Improving outcomes in hypertensive patients: focus on adherence and persistence with antihypertensive therapy. J Clin Hypertens. 2009;11:376‐382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gerth WC. Compliance and persistence with newer antihypertensive agents. Curr Hypertens Rep. 2002;4(6):424‐433. [DOI] [PubMed] [Google Scholar]
- 15. Egan BM, Bandyopadhyay D, Shaftman SR, Wagner CS, Zhao Y, Kristina S. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension. 2012;59:1124‐1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tung YC, Lin YS, Wu LS, Chang CJ, Chu PH. Clinical outcomes and healthcare costs in hypertensive patients treated with a fixed‐dose combination of amlodipine/valsartan. J Clin Hypertens (Greenwich). 2015;17:51‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hsu C‐N, Wang T‐D. Secular trends in prescription patterns of single‐pill combinations of an angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker plus a thiazide diuretic for hypertensive patients in Taiwan. Acta Cardiol Sin. 2013;29:49. [PMC free article] [PubMed] [Google Scholar]
- 18. Boyko E, Barr E, Zimmet P, Shaw J. Two‐hour glucose predicts the development of hypertension over 5 years: the AusDiab study. J Hum Hypertens. 2008;22:168‐176. [DOI] [PubMed] [Google Scholar]
- 19. Chiang C‐H, Huang W‐C, Yang J‐S, et al. Five‐year outcomes after acute myocardial infarction in patients with and without diabetes mellitus in Taiwan, 1996–2005. Acta Cardiol Sin. 2013;29:387. [PMC free article] [PubMed] [Google Scholar]
- 20. Chou S‐H, Tung Y‐C, Lin Y‐S, et al. Major adverse cardiovascular events in treated periodontitis: a population‐based follow‐up study from Taiwan. PLoS ONE. 2015;10:e0130807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lin Y‐S, Liu P‐H, Wu L‐S, Chen Y‐M, Chang C‐J, Chu P‐H. Major adverse cardiovascular events in adult congenital heart disease: a population‐based follow‐up study from Taiwan. BMC Cardiovasc Disord. 2014;14:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Neal B, Pressure Lowering Treatment Trialists' Collaboration . Effects of ACE inhibitors, calcium antagonists, and other blood‐pressure‐lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration. Lancet. 2000;356:1955‐1964. [DOI] [PubMed] [Google Scholar]
- 23. Black HR, Elliott WJ, Grandits G, et al. Principal results of the controlled onset verapamil investigation of cardiovascular end points (CONVINCE) trial. JAMA. 2003;289:2073‐2082. [DOI] [PubMed] [Google Scholar]
- 24. Kjeldsen SE, Dahlöf B, Devereux RB, et al. Effects of losartan on cardiovascular morbidity and mortality in patients with isolated systolic hypertension and left ventricular hypertrophy: a Losartan Intervention for Endpoint Reduction (LIFE) substudy. JAMA. 2002;288:1491‐1498. [DOI] [PubMed] [Google Scholar]
- 25. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial . Major outcomes in high‐risk hypertensive patients randomized to angiotensin‐converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002;288:2981‐2997. [DOI] [PubMed] [Google Scholar]
- 26. Wing LM, Reid CM, Ryan P, et al. A comparison of outcomes with angiotensin‐converting–enzyme inhibitors and diuretics for hypertension in the elderly. New Engl J Med. 2003;348:583‐592. [DOI] [PubMed] [Google Scholar]
- 27. Psaty BM, Lumley T, Furberg CD, et al. Health outcomes associated with various antihypertensive therapies used as first‐line agents: a network meta‐analysis. JAMA. 2003;289:2534‐2544. [DOI] [PubMed] [Google Scholar]
- 28. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560‐2571. [DOI] [PubMed] [Google Scholar]
- 29. Krakoff LR. Diuretics for hypertension. Circulation. 2005;112:e127–e129. [DOI] [PubMed] [Google Scholar]
- 30. Kostis JB, Wilson AC, Freudenberger RS, et al. Long‐term effect of diuretic‐based therapy on fatal outcomes in subjects with isolated systolic hypertension with and without diabetes. Am J Cardiol. 2005;95:29‐35. [DOI] [PubMed] [Google Scholar]
- 31. Rosendorff C, Black HR, Cannon CP, et al. REPRINT treatment of hypertension in the prevention and management of ischemic heart disease. Hypertension. 2007;50:e28–e55. [Google Scholar]
- 32. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure. Circulation. 2013;128:e240–e327. [DOI] [PubMed] [Google Scholar]
- 33. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST‐elevation myocardial infarction. Circulation. 2013;127:529‐555. [DOI] [PubMed] [Google Scholar]
- 34. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119‐177. [DOI] [PubMed] [Google Scholar]
- 35. Probstfield JL, O'Brien KD. Progression of cardiovascular damage: the role of renin–angiotensin system blockade. Am J Cardiol. 2010;105:10A–20A. [DOI] [PubMed] [Google Scholar]
- 36. Bovill EG, Terrin ML, Stump DC, et al. Hemorrhagic events during therapy with recombinant tissue‐type plasminogen activator, heparin, and aspirin for acute myocardial infarction: results of the Thrombolysis in Myocardial Infarction (TIMI). Phase II Trial. Ann Inter Med. 1991;11:256‐265. [DOI] [PubMed] [Google Scholar]
- 37. Sanz G, Fuster V. Fixed‐dose combination therapy and secondary cardiovascular prevention: rationale, selection of drugs and target population. Nat Clin Pract Cardiovasc Med. 2009;6:101‐110. [DOI] [PubMed] [Google Scholar]
- 38. Wan X, Ma P, Zhang X. A promising choice in hypertension treatment: Fixed‐dose combinations. Asian J Pharm Sci. 2014;9:1‐7. [Google Scholar]
- 39. Dickson M, Plauschinat CA. Compliance with antihypertensive therapy in the elderly. Am J Cardiovasc Drug. 2008;8:45‐50. [DOI] [PubMed] [Google Scholar]
- 40. van Galen KA, Nellen JF, Nieuwkerk PT. The effect on treatment adherence of administering drugs as fixed‐dose combinations versus as separate pills: systematic review and meta‐analysis. AIDS Res Treat. 2014;2014:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Gupta AK, Arshad S, Poulter NR. Compliance, safety, and effectiveness of fixed‐dose combinations of antihypertensive agents. Hypertension. 2010;55:399‐407. [DOI] [PubMed] [Google Scholar]
- 42. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507‐520. [DOI] [PubMed] [Google Scholar]
- 43. Chiang CE, Wang TD, Ueng KC, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015;78:1‐47. [DOI] [PubMed] [Google Scholar]
- 44. Council ES, Redon J, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. Eur Heart J. 2013;34:2159‐2219. [DOI] [PubMed] [Google Scholar]
- 45. Rosendorff C, Lackland DT, Allison M, et al. Treatment of hypertension in patients with coronary artery disease. Hypertension. 2015;65:1372‐1407. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


