Abstract
This periodic review aims to identify, summarize, and appraise studies relating to the implementation of salt reduction strategies that were published between September 2016 and February 2017. A total of 41 studies were included as relevant to the design, assessment, and implementation of salt reduction strategies, and a detailed appraisal was conducted on the seven studies that evaluated the impact of salt reduction strategies. Of these, three were national studies or included large populations and four were conducted in communities with small participant sample sizes. Each study used a different strategy for reducing salt intake varying from category‐specific sodium targets for packaged food to use of a low‐sodium salt substitute to behavior change interventions. Four studies found statistically significant decreases in dietary salt intake and one study showed statistically significant decreases in mean sodium density of packaged food products. Four of the seven studies used either spot or 24‐hour urine samples to measure dietary salt intake and five were conducted in East or Southeast Asia—two of which were in low‐ and middle‐income countries. Study quality varied among the seven studies and all except one had one or more risks related to bias.
Keywords: hypertension—general, salt, sodium, systematic review
1. INTRODUCTION
As a result of the high profile of public health efforts to reduce dietary salt, the number of publications on dietary salt is rapidly increasing.1 Low‐quality research producing inconsistent findings has led to challenges for clinicians and policy stakeholders to keep informed on the effects of salt on health outcomes,2 while higher‐quality research that aligns with existing evidence often goes unnoticed.3 In response to this, an initiative was established in 2014 that aimed to publish a regular systematic and up‐to‐date critical appraisal of all studies that examine the relationship between dietary salt and health or assess the impact of strategies designed to achieve population dietary salt reduction.4 Accordingly, studies included in each review are evaluated based on a series of established quality indicators to provide a more objective and balanced interpretation of study conclusions. In addition, specific focus is on the methods used for the assessment of dietary salt, using criteria developed for the Cochrane review of the health impact of dietary salt.5
Initially designed as a summarized MEDLINE search communicated through a weekly email newsletter, the Science of Salt Weekly, 6 alternating narrative summaries of the reviewed articles are periodically published focusing on: (1) the relationship between dietary salt and health outcomes, and (2) evaluating salt reduction initiatives in populations.7, 8, 9, 10, 11 In addition, two annual systematic reviews incorporating studies published between 2013 and 2015 were published.4, 12 To date there have been five periodic systematic reviews published—three focused on evaluating the implementation of salt reduction strategies identified as part of the Science of Salt Weekly systematic review series, with a view to informing future implementation of interventions to lower population salt consumption7, 8, 11 and two summarizing the volume of studies reporting on the effects of salt intake on health outcomes.9, 10
The reviews evaluating intervention studies provide important recommendations for the implementation of salt reduction strategies including government commitment, the need for multicomponent interventions extending the focus beyond targeting consumer behavior, and using standardized methodologies to rigorously monitor the salt content of processed foods. Additionally, the need for greater emphasis on external validity, and an evaluation framework that supports both scientific robustness and external validity is highlighted as an important element in providing further evidence of effectiveness in real‐world situations. Notably, most studies included in these reviews were from high‐income countries, emphasizing the need for more research in low‐ and middle‐income countries (LMICs). To keep key stakeholders up‐to‐date with new literature on current salt reduction strategies worldwide, and maintain the momentum already achieved through regular critical appraisal review articles, the objective of the current review is to summarize and critically appraise the literature on the effectiveness of salt reduction programs published from September 2016 to February 2017.
2. METHODOLOGY
A detailed description of the methods used to identify and screen studies for eligibility has been previously published.1 Articles related to dietary salt reduction in populations were identified through a standardized weekly MEDLINE literature search and summaries were published in the Science of Salt Weekly newsletter. Studies published between September 1, 2016, and February 28, 2017, were screened for eligibility by two independent authors using previously established inclusion and exclusion criteria.11
Studies evaluating the impact of salt reduction interventions that met the inclusion criteria were appraised for risk of bias by two independent reviewers using the Cochrane risk of bias tool for randomized controlled trials (RCTs) and a modified version of the tool for nonrandomized intervention studies.13, 14 Additionally, detailed critical appraisal and summaries were prepared. Other studies with a focus on: (1) monitoring and surveillance of salt intake; (2) salt content in foods and meals; (3) consumers’ knowledge, attitudes, and behaviors toward salt; (4) economic evaluation or modelling studies of salt reduction strategies; and (5) other studies related to implementation of salt reduction initiatives are summarized in Appendix S1.
3. RESULTS
The MEDLINE search identified 5062 potentially relevant studies, of which 75 full text articles were assessed against the eligibility criteria after studies were screened based on abstracts. A total of 41 studies were considered relevant to the implementation of population‐wide salt reduction interventions, seven of which evaluated the impact of strategies to reduce salt intake, 14 that focused on the monitoring and surveillance of salt intake levels in populations or salt levels in foods or on knowledge, attitudes and behaviors relating to salt intake, four that were modelling studies related to salt reduction, and the remaining 16 that were related to implementation of salt reduction interventions including reviews and studies examining the acceptability of different strategies (Figure 1).
Figure 1.
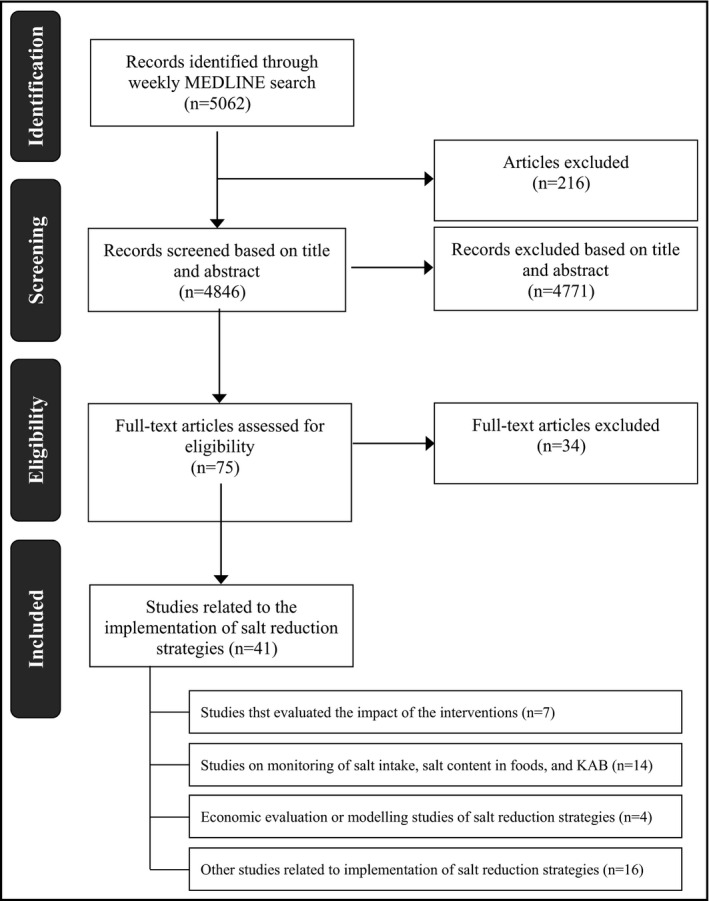
Studies included in the current review—September 2016 to February 2017. KAB indicates knowledge, attitudes, and behavior
Two thirds of the studies included in this review were conducted in high‐income countries, with the remaining 14 studies conducted in LMICs the majority in East and Southeast Asia and the Western Pacific region (n = 12).
The current review focused on the seven studies that evaluated the impact of interventions or policies to reduce salt intake (Table) and are appraised in detail below with risk of bias assessments included in Appendix S1. Three of the included studies were conducted in LMICs, two of which were large‐scale population studies: a repeated cross‐sectional study in Vietnam; and a cluster RCT in China; and the remaining study a RCT conducted in Indonesia. With the exception of an assessment of the effect of sodium targets on sodium content of packaged food products in the United States, the remaining studies were small‐scale community‐based feasibility or pilot intervention studies conducted in high‐income countries. These included an RCT conducted in a group of families in Japan, a pilot intervention study among restauranteurs and cooks in South Korea, and a mixed‐methods pilot feasibility study involving healthy adult volunteers from New Zealand. A summary of the additional 34 studies is provided in Appendix S1.
Table 1.
Characteristics of included “intervention” studies
| Study | Country | Study design | Study population | Intervention | Method of assessment | Results |
|---|---|---|---|---|---|---|
| Lofthouse et al (2016) | New Zealand | Mixed‐methods pilot study | 11 volunteers aged 18–65 y | Low‐salt diet education by dietitians over 4 wk |
One 24‐h urine collection A 2‐d nonconsecutive weighed diet record One 24‐h diet recall |
Baseline mean urinary sodium was 2342 mg/d and dietary sodium intake 3221 mg/d, shown to decrease on follow‐up by 18% and 53%, respectively. Substantial behavior changes were required to decrease sodium intake. |
| Do et al (2016) | Vietnam | Repeat cross‐sectional study | 509 baseline and 511 follow‐up participants aged 25–64 y living within the wards and communes of Viet Tri city | Communication for Behavioral Impact (COMBI) Intervention, conducted for 1 y (June 2013–June 2014) |
Spot urine samples Questionnaire Blood pressure |
A small but significant decrease in salt excretion was observed from baseline to follow‐up (8.48 g/d to 8.05 g/d) along with a large significant increase in favorable salt knowledge and behaviors. A statistically significant decrease was also observed for systolic and diastolic blood pressure. |
| Takada et al (2016) | Japan | Cluster, randomized controlled trial | 35 housewives aged 40 y or older (18 intervention, 17 control) and 33 family members aged 20 y or older (18 intervention, 17 control) | 2× cooking classes showcasing reduced‐salt cooking practices for intervention housewives. Controls received lectures on general healthy eating. |
Spot urine samples Blood pressure |
Following intervention there was a small increasein salt intake in the control group (10.00–10.3 g/d) compared with a reduction inthe intervention group (9.57–8.95 g/d), resulting in a mean difference between the groups of −1.19 g/d (P = .034). Changes in blood pressure were not significant. |
| Park et al (2016) | South Korea | Single‐arm pilot intervention using a pre‐post design | 49 restaurant owners or cooks in the business district of Seoul | Education, health examination, and counseling of restaurant personnel |
Questionnaire on salt KAB Urine dipstick tests |
Participants with lower estimated sodium intake reported more favorable sodium‐related KAB such as “it is necessary to use healthy cooking methods for customers.” |
| Irwan et al (2016) | Indonesia | Randomized controlled trial |
51 participants three groups: control (n = 17), salt reduction training (n = 17), and salt reduction and efficacy maintenance (n = 17). All aged <60 y with diagnosed or undiagnosed hypertension |
Two 90‐min educational training sessions over 2 d within 1 wk |
12‐item “knowledge of hypertension” questionnaire 7‐statement “attitudes towards self‐care” questionnaire Salinity checker of urinary sodium Salt meter assessment of salt in foods |
There was no significant decrease in urinary sodium between the two intervention groups and the control group; however, the intervention groups reported that they added less salt. No significant difference was observed for participants’ knowledge, yet self‐efficacy to decrease salt intake significantly increased in both intervention groups compared with the control group. |
| Li et al (2016) | China | Cluster randomized trial | 2380 adult participants from 120 villages in rural northern China (60 control villages and 60 intervention villages) | Community‐based sodium reduction program. Of the intervention villages, half received a subsidy on a salt substitute |
One 24‐h urine collection onfollow‐up Sodium to potassium ratio Questionnaire (KAB) Blood pressure |
Intervention group had a statistically significant lower sodium excretion than controls (by 5.5%, 237 mmol/d vs 251 mmol/d; P = .03). There was also a decline in the sodium to potassium ratio of 15%. There was no evident significant change in blood pressure. There was a higher uptake of salt substitute use in the villages with the subsidy compared with those without. |
| Curtis et al (2016) | United States | Repeat cross‐sectional study | National Salt Reduction Initiative (NSRI) packaged food database. 61 food categories, sales, sodium content, and serving size data in 2009, 2012, and 2014 with 6336, 6898, and 7396 products, respectively | 2009 sodium targets published, and companies were asked to publicly commit and meet the 2012 and 2014 targets |
Percentage of companies meetingtargets Percentage of products meetingtargets Change in sales‐weighted sodiumdensities overall and in specificfood categories |
A quarter of food categories met the 2012 target in 2014, with 3% meeting the 2014 targets. Overall, sales‐weighted mean sodium density decreased from 2009 to 2014 by 6.8% (P < .001). |
Abbreviation: KAB, knowledge, attitudes, and behaviors.
From the seven studies selected for full review, a high risk score in one or more domains, according to the risk of bias tools, was recorded for six studies (Figure 2). Three non‐RCT studies were at high risk of selection bias as a result of the sampling methods and representativeness of participants. One of the RCTs used a nonrandom method in the sequence generation process of selecting participants. Five studies were at high risk of performance bias because study personnel or participants were not blinded to knowledge of the intervention in RCTs or in non‐RCTs confounding variables were not controlled for, meaning that exposure to other factors apart from the intervention may affect the outcome. Two studies scored high risk of detection bias relating to blinding of the outcome assessment in the RCT study and reliability and validity of exposure and outcome assessment in the non‐RCT study, which may affect the outcome measurement as the outcome was likely influenced by lack of blinding and/or an unreliable measurement method. None of the studies were at risk of bias in the domains attrition or reporting bias.
Figure 2.

Risk of bias assessment of included “intervention” studies. N/A indicates not available; RCT, randomized controlled trial
Four of seven studies showed statistically significant decreases in the dietary salt intakes of study populations as a result of behavior interventions: one large repeated cross‐sectional population study15 two small community‐based studies (one that provided nutritional counseling in a University setting16 and another that provided cooking classes in a rural setting), and one large cluster randomized trial including a salt substitute combined with consumer education intervention.17 Of the remaining three studies, one found statistically significant decreases in mean sodium density of packaged food products following a national salt reduction initiative for voluntary, category‐specific sodium targets for packaged food. The other two studies found significant improvements in nutrition behaviors relating to salt intake after consumer education in a pilot study18 and a community‐based RCT.19 However, both showed nonsignificant decreases in actual salt intake. Both studies were conducted in samples of ≤50 community participants and aimed to improve knowledge, attitudes, and self‐care through education.
3.1. Studies evaluating the impact of salt reduction interventions
3.1.1. Behavioral interventions
Do HT, Santos JA, Trieu K, et al. Effectiveness of a Communication for Behavioral Impact (COMBI) intervention to reduce salt intake in a Vietnamese province based on estimations from spot urine samples. J Clin Hypertens (Greenwich). 2016;18:1135–1142.
Objective: To evaluate the effectiveness of the Communication for Behavioral Impact (COMBI)‐Eat Less Salt (ELS) intervention conducted in Viet Tri, Vietnam, for reducing salt intake with a view to scale up to a regional or national level. Specifically, to assess: (1) changes in salt intake; (2) changes in knowledge, attitudes, and behaviors regarding salt intake; and (3) changes in health outcomes including BP and prevalence of hypertension.
Design: Repeated cross‐sectional study.
Setting: Four wards and four communes among a total population of 80 000 in Viet Tri, Phu Tho Province, Vietnam.
Participants: A total of 509 (baseline) and 511 (follow‐up) adults (50% women) aged 25 to 64 years (mean age, 45 years) living within the wards and communes of Viet Tri city.
Intervention and duration: The COMBI‐ELS intervention was conducted between June 2013 and June 2014. Strategies included mass media communications, targeted primary school interventions, training for cooks community programs, and focus on high‐risk groups.
Outcomes: Sodium consumption estimated by spot urine samples using the INTERSALT equation; effects on knowledge, attitudes, and behaviors related to salt intake; and changes in health outcomes including blood pressure (BP).
Summary of results: The study reported a small statistically significant decrease in salt excretion from 8.48 g/d (3392 mg sodium) (SD 2.13) at baseline to 8.05 g/d (3220 mg sodium) (SD 2.11) at follow‐up (P = .001). In addition, there were large increases in the proportion of participants demonstrating positive changes in knowledge and behaviors between baseline and follow‐up including awareness of salt intake causing hypertension (43.61% to 86.3%), causing heart attack (5.5% to 17%), and leading to stroke (9.25% to 46.58%) (all P < .001). Furthermore, there were reductions in both systolic and diastolic BPs: net reduction in systolic BP of −5.93 mm Hg (95% confidence interval, −8.03 mm Hg to −3.83 mm Hg; P < .001) and diastolic BP of −4.86 mm Hg (95% confidence interval, −6.21 mm Hg to −3.51 mm Hg; P < .001). In addition, the proportion of respondents with hypertension was 26.13% at baseline and 21.14% at follow‐up, although this reduction was not statistically significant (P = .060).
Source of funding: Not reported.
Comments: This repeat cross‐sectional study evaluating the impact of behavior change interventions aimed at reducing salt intake found reductions in salt consumption, increased knowledge and behaviors on salt intake, and decreased systolic and diastolic BPs. While salt intake was estimated through spot urine samples, a subsample of 24‐hour urine at baseline and follow‐up was used to validate the spot samples. Mean daily sodium excretion was estimated using five different equations, although every equation underestimated the change in mean salt excretion compared with the 24‐hour measurement (9.43 g/d [3772 mg sodium] [SD 3.69] to 7.44 g/d [2976 mg sodium] [SD 4.09], P < .05). However, regardless of the equation used, there was a reduction in mean salt intake (P = .001) following the intervention. The random selection of participants, comparable characteristics between the baseline and follow‐up participants, and good urine completeness rates (>65% for both groups) were strengths of the study. Sources of bias inherent to the study design are discussed appropriately by the authors.
Lofthouse C, Te Morenga L, McLean R. Sodium reduction in New Zealand requires major behaviour change. Appetite. 2016;105:721–730.
Objective: To examine the feasibility of following a low‐sodium diet and its effects on other nutrients that influence cardiovascular risk and to identify the barriers and facilitators to adherence to a low‐sodium diet.
Design: Mixed‐methods pilot study.
Setting: Dietary counseling clinics in Dunedin, New Zealand.
Participants: Eleven healthy adult volunteers aged 18 to 65 years (7 men and 4 women; mean age, 39.2 ± 12.8 years) not already restricting their sodium intake and who were estimated to be consuming >5 g/d salt (sodium 2000 mg).
Intervention and duration: All participants received intensive low‐salt diet education delivered by a dietitian for 4 weeks and were instructed to follow a low‐sodium diet through one‐on‐one nutritional education sessions. In addition, guidance on using a salt substitute and training to use a smartphone application that helps to identify lower‐sodium food alternatives were provided. The intervention used behavior change theory for promoting participant self‐efficacy and by encouraging participants to set weekly goals.
Outcomes: Sodium and other nutrient intake and participants’ experiences of following a low‐sodium diet. Dietary intake was assessed via 2‐day (nonconsecutive days) weighed diet records, one 24‐hour dietary recall, and one 24‐hour urine sample at baseline and follow‐up. A 24‐hour diet record was conducted over the same period as 24‐hour urine collection. Sodium and potassium intake was assessed by 24‐hour urine sample. Information on sources of dietary sodium from dietary data was used to educate and inform participants during counseling sessions. A semistructured interview was conducted after the intervention to explore participants’ experiences and perceived barriers and facilitators in adhering to a low‐sodium diet.
Summary of results: At baseline, mean salt estimated from 24‐hour urinary sodium was 5.8 g/d (2342 mg sodium) and mean salt estimated from dietary recall was 8.0 g/d (3221 mg sodium) based on 2‐day weighed diet record and one 24‐hour recall. At follow‐up, mean urinary salt and mean dietary salt intakes were 18% and 53%, respectively, lower than baseline values (baseline 24‐hour urinary sodium 5.86 g/d salt [sodium 2342 mg] to follow‐up 24‐hour urinary sodium 4.77 g/d salt [sodium 1909 mg], P = .21). Thematic analysis showed that adherence to a low‐sodium diet required substantial changes to participants’ usual food purchasing and preparation habits.
Sources of funding: Department of Human Nutrition, University of Otago.
Comments: This 4‐week sodium reduction intervention was conducted in a clinical setting and recruited healthy adults. The aim was to provide intensive sodium reduction education to enable individuals to achieve and adhere to a low‐sodium diet meeting the World Health Organization's (WHO's) sodium recommendations. The short‐term intervention was based on individualized education and behavior change counseling to follow a low‐salt diet. Several different outcome assessment methods were used and provided reliable estimates of salt intake at baseline and follow‐up. However, the sample size was small and therefore not generalizable beyond the study population. In addition, use of volunteers who had high education levels and were highly motivated to follow a low‐sodium diet suggests that self‐reported barriers and facilitators to sodium reduction may not reflect the general population.
Irwan AM, Kato M, Kitaoka K, Ueno E, Tsujiguchi H, Shogenji M. Development of the salt‐reduction and efficacy‐maintenance program in Indonesia. Nurs Health Sci. 2016;18:519–532.
Objective: To examine the effects of a salt reduction and efficacy maintenance program in reducing and maintaining salt intake among older people with high BP in Indonesia. Specifically, to: (1) examine whether an educational intervention improved self‐care and self‐efficacy; and (2) determine whether maintenance meetings maintained self‐care and self‐efficacy. Expected outcomes included improvement and maintenance of hypertension knowledge, attitudes, self‐care practices, and self‐efficacy after the intervention.
Design: RCT.
Setting: Tammua subdistrict, Indonesia.
Participants: A total of 51 (n = 17 control; n = 17 salt reduction training [SRT] group; n = 17 salt reduction and efficacy maintenance [SREM] group) participants (28% women) younger than 60 years (mean, 66.5; SD 6.1) with systolic BP >120 mm Hg and diastolic BP >80 mm Hg or a diagnosis of hypertension within the past 6 months, and a monthly health checkup within 12 months living in two regions within the Tammua district.
Intervention and duration: The RCT was conducted between October 2014 and January 2015. Participants were assigned to one of three groups: a control group, which received usual care; an SRT group; and a salt reduction and efficacy maintenance group. Two 90‐minute educational training sessions were conducted over 2 days within 1 week and included both the SRT and SREM groups. Participants in the SREM group then attended a 90‐minute maintenance meeting 1 month after the SRT. The control group received no intervention, and usual care was provided to all participants.
Outcomes: All data were collected at baseline, 1 week following SRT, and 1 week following the SREM meeting. Self‐care knowledge was assessed using the 12‐item knowledge of hypertension index; attitudes towards self‐care were assessed using a seven‐statement questionnaire; salt consumption was measured with a salt meter to assess salt content in food; and urinary sodium was measured using a salinity checker previously validated in Japan. Self‐efficacy was measured using a general self‐efficacy scale consisting of 10 statements.
Summary of results: Urinary sodium showed a nonsignificant decrease compared with the control group after interventions for the SRT and SREM groups compared with baseline (8.6–7.2 g/d salt [sodium 3440–2880 mg] in the SRT group and 7.5–6.9 g/d salt [3000–2760 mg sodium] in the SREM group; all P ≥ .1). Salt content in food did not decrease after the SRT or SREM interventions compared with the control group (P ≥ .44 in SRT and P ≥ .35 in SREM). Both intervention groups reported a decrease in added salt compared with the control group (P ≤ .001). Knowledge after SRT training did not improve in the SRT group (P ≥ .05). Following the SREM intervention, knowledge, attitude scale, and self‐efficacy also did not improve (P ≥ .05). Self‐efficacy was improved after SRT and SREM interventions (all P ≤ .05) and was maintained after the maintenance intervention compared with the control group (both P≤.002).
Source of funding: Not reported.
Comments: This RCT evaluated the impact of training and maintenance interventions aimed at increasing knowledge and self‐care and maintaining a low‐salt diet. Salt intake was estimated from a salinity checker, which, while validated in Japan, does not appear to have been validated in an Indonesian population or against a gold standard 24‐hour urine sample, and the small sample size in all groups was likely to have affected the outcomes as a result of a lack of statistical power. Similarly, the qualitative data were captured during one SREM meeting and were not representative of all meetings; thus, they may be subject to self‐report bias. Furthermore, at baseline, urinary sodium was lower in the control group compared with the intervention groups (P < .05). The random selection of participants, comparable characteristics between the baseline and follow‐up participants, and good follow‐up rates (>75%) were strengths of the study. Sources of bias inherent to the sample size and analysis are discussed appropriately by the authors.
Park S, Lee H, Seo D, Oh KH, Hwang TG, Choi BY. Educating restaurant owners and cooks to lower their own sodium intake is a potential strategy for reducing the sodium contents of restaurant foods: a small‐scale pilot study in South Korea. Nutr Res Pract. 2016;10:635–640.
Objective: To evaluate the feasibility of a sodium reduction program to improve nutrition behaviors and psychosocial factors through nutrition education and to examine the health knowledge of restaurant owners and cooks with the aim of improving their nutrition behaviors and cooking methods at restaurants.
Design: Single‐arm pilot intervention using a pre‐post design.
Setting: Seoul, South Korea.
Participants: A total of 49 (35% women) restaurant owners and cooks aged 29 to 63 years (mean age, 48.5 years) from 30 independent restaurants.
Intervention and duration: Nutrition education, health examination and counseling, and a structured survey on key psychosocial and behavioral factors related to sodium intake and food preparation at restaurants. The intervention was conducted between October 2014 and February 2015 (5 months). Participants were categorized into high and low salt consumption groups using a spot urine dipstick with the cutoff correlating to an estimated 12 g/d salt (4800 mg sodium), which is approximately the average salt intake among the Korean adult population.
Outcomes: Change in nutrition behaviors related to sodium intake including perceptions of the importance of healthy eating (and low‐salt diet) and the influence on food preparation measured by self‐reported questionnaire.
Summary of results: A high proportion of participants (65%) were overweight or obese and 75% had elevated BP. Alcohol consumption and smoking were also common. There was more agreement that “it was necessary to use healthy cooking methods for customers” among the group with estimated lower salt intake (59% vs 19% in the highest salt intake group). Differences in behavioral factors related to salt intake did not reach statistical significance as a result of the small sample size. There was an increase in the number of participants indicating they were likely to reduce their salt intake as measured by the survey questionnaire administered before and after the intervention (composite score of 4: 2.63 ± 1.84 to 3.50 ± 1.56; P ≤ .007).
Source of funding: National Research Fund for the Republic of Korea and a research grant from Hallym University.
Comments: This study identified a high‐risk group of restaurant owners and cooks that could be a public health target given their own morbidity (65% overweight or obese) and the influence they have on the health of people who frequently consume food outside of their own home. The results demonstrated that people with lower dietary salt intake tend to place higher importance on healthy eating and making the food provided to consumers healthier. Results relating to participant salt intake and behaviors should be interpreted with caution as salt levels were measured by urine dipstick test (not 24‐hour urine collection). In addition, because of the small sample size and convenience sampling, the results are prone to selection bias, which affects the generalizability of the findings, and testing bias, which influences internal validity. These are discussed appropriately by the authors.
Takada T, Imamoto M, Fukuma S, et al. Effect of cooking classes for housewives on salt reduction in family members: a cluster randomized controlled trial. Public Health. 2016;140:144–150.
Objective: To assess the effect of cooking classes on the salt intake of housewives and family members.
Design: Cluster RCT.
Setting: Shirakawa, Japan.
Participants: A total of 35 housewives 40 years and older (18 in the intervention group and 17 in the control group) and 33 family members 20 years and older (18 in the intervention group and 15 in the control group).
Intervention: Two cooking classes (September and October 2015), 90‐minute duration each, comprised of instructions on salt‐reduced cooking and practical lessons for evaluating the amount of salt in a meal directly provided to the housewives. The housewives were then free to deliver the message to their family members. The control group received lectures on healthy lifestyle not covering topics related to salt reduction.
Outcomes: Outcomes were measured before and 2 months after the intervention. Difference in mean salt intake estimated from spot urine samples using the Tanaka equation, and difference in systolic and diastolic BP.
Summary of results: There was a slight increase in mean salt intake in the control group (from 10.00 to 10.30 g/d [4000–4200 mg sodium]), while there was a reduction in the intervention group (from 9.57 to 8.95 g/d [3828–3580 mg sodium]) from baseline to follow‐up. The mean difference between the two groups was −1.19 g/d (476 mg sodium) (95% confidence interval, −2.29 to −0.09; P = .034). Subgroup analyses of housewives and family members showed a similar pattern. Systolic and diastolic BPs increased in both groups from baseline to follow‐up, but the difference was not statistically significant.
Sources of funding: None declared.
Comments: This trial found that cooking classes focusing on salt reduction directed toward housewives resulted in a significant reduction in salt intake. These results, however, should be interpreted with caution as salt intake was assessed through spot urine samples rather than 24‐hour urine collection. There was insufficient information about the randomization process, and the participants were not blinded to the intervention. Overall, there was a good follow‐up rate, although it should be noted that there were higher follow‐up rates in the control group compared with the intervention group for both housewives and family members.
Li N, Yan LL, Niu W, et al. The effects of a community‐based sodium reduction program in rural China—a cluster‐randomized trial. PLoS One. 2016;11:e0166620.
Objective: To determine the effect of a community‐based sodium reduction program on salt consumption in rural northern China.
Design: Cluster‐randomized trial.
Setting: A total of 120 townships in rural northern china (two counties were selected from each province, and 12 townships from each county), with one village selected from each township.
Participants: An age‐ and sex‐stratified random sample of ≥20 consenting adults from each of the 120 villages (60 control, 60 intervention) (n = 2566).
Intervention and duration: Reduced sodium and added potassium salt substitute combined with community‐based health education focusing on sodium reduction. Half (30 of 60) of the intervention villages also received a price subsidy on the salt substitute. The intervention length was 18 months.
Outcomes: Sodium excretion measured by 24‐hour urine sample, sodium to potassium ratio, BP, and prevalence of hypertension. Knowledge and behavioral outcomes relating to salt and salt substitute were also recorded.
Summary of results: A total of 1903 individuals had a valid 24‐hour urine sample (975 and 928 from the intervention and control groups, respectively). Mean urinary salt excretion in the intervention group was 5.5% lower than the control group (13.6 ± 5.6 g/d [5451 ± 2231 mg sodium] vs 14.4 ± 5.4 g/d [5773 ± 2162 mg sodium] in the intervention and control groups, respectively; P = .03). The sodium to potassium ratio was also 15% lower in the intervention group compared with the control group (5.2 ± 3.1 intervention vs 6.1 ± 2.5 control, P < .001). There were no changes in BP.
Source of funding: Federal funds from the National Heart, Lung, and Blood Institute; National Institutes of Health; the Department of Health and Human Services; and the National Center for Chronic Disease Prevention and Health Promotion (CDC). Additional support was provided through the UnitedHealth Group.
Comments: Salt intake was reduced in a population where intake was previously estimated to be 14 g/d. It is likely that the lower sodium intake in the intervention group was predominantly attributable to the salt substitute given the corresponding change in the sodium to potassium ratio. The large‐scale intervention led to approximately 2000 individuals having evaluation data collected and the study used strict criteria for the collection of 24‐hour urine samples (gold standard measure). While the evaluation was useful for comparing control and intervention groups, there was no baseline salt intake data initially collected. Therefore, it is unknown whether salt intake levels differed in the villages at baseline. While sodium excretion decreased, there was no change in BP or the number of individuals with hypertension. This is possibly caused by the sample size providing insufficient power to detect changes in BP or the short intervention timeframe. Overall, this study shows that a salt substitute can decrease salt intake and that a price subsidy is effective in increasing uptake of the salt substitute.
3.1.2. Structural interventions to lower salt content in foods
Curtis CJ, Clapp J, Niederman SA, Ng SW, Angell SY. US food industry progress during the National Salt Reduction Initiative: 2009–2014. Am J Public Health. 2016;106:1815–1819.
Objective: To assess the US packaged food industry's progress towards meeting the National Salt Reduction Initiative (NSRI) targets and examine the change in overall sales‐weighted mean sodium density from 2009 to 2014.
Design: Repeated cross‐sectional survey of sales‐weighted mean sodium density values.
Setting: United States.
Data: The NSRI Packaged Food Database links sales and nutrition information for products that are in the top 80% of sales for each food category. The sample included 61 food categories with sales, sodium content, and serving size data in 2009 (n = 6336 products), 2012 (n = 6898 products), and 2014 (n = 7396).
Intervention: The NSRI is a national coalition led by New York City Department of Health and Mental Hygiene that engages the food industry to lower salt intake in the United States through targeted reductions in the food supply. In 2009, sodium targets for foods were published and companies were asked to publicly commit and meet the 2012 and 2014 targets.
Outcomes: Four measures were used to evaluate sodium reduction progress: (1) the percentage of food categories meeting 2012 and 2014 NSRI targets, (2) the percentage of products meeting 2012 and 2014 targets, (3) change in sales‐weighted mean sodium densities in specific food categories and meta‐categories, and (4) change in overall sales‐weighted mean sodium density.
Summary of results: In 2014, 26% of categories met the 2012 targets and 3% met the 2014 targets, compared with no categories meeting the targets in 2009. The percentage of products meeting the 2012 targets also significantly increased from 33% in 2009 to 42% in 2012 and 45% in 2015 (P < .001 for each). There was a significant decrease in sales‐weighted mean sodium density in 26 (43%) food categories. Overall, sales weighted mean sodium density significantly decreased by 6.8% (P < .001).
Sources of funding: Funding for the NSRI Packaged Food Database was supported in part through cooperative agreements with the Centers for Disease Control and Prevention. The authors were supported by the Department of Health and Mental Hygiene.
Comments: The inclusion of a large number of food products and the most commonly consumed foods (top 80% of sales for each food category) in the NSRI database indicates that the study findings are likely to be representative of the US food supply. Although Nutrition Fact Labels are an appropriate source for nutritional composition information, it should be noted that in the United States, the nutrition content on Nutrition Fact Labels can differ from actual nutrition content by up to 20%. A strength of the study was the use of sales‐weighted mean sodium densities, which provide information on the likely effects of the reductions on population salt intake. Overall, this study provides a useful assessment of the effects of the NSRI targets on the sodium content of the US food supply and demonstrates that the establishment of salt targets and a robust monitoring system are feasible.
4. DISCUSSION
Globally, countries are translating evidence on salt and health outcomes into policies and strategies to reduce population‐wide salt intake to prevent and control cardiovascular diseases.20 The Science of Salt periodic review initiative provides up‐to‐date critical appraisal of all studies published worldwide with the aim of building evidence on the relationship between dietary salt and health and the impact of strategies designed to achieve population dietary salt reduction.
This review (from September 2016 to February 2016) identified 41 studies that provided information related to the implementation of salt reduction strategies. However, only seven evaluated the impact of salt reduction strategies and therefore met inclusion criteria for critical appraisal.
Although the seven studies vary in quality, the process of critical appraisal and assessment of bias provides a clear evaluation of the strengths and limitations of each study and strengthens the evidence to support successful approaches to reducing dietary salt intake in different settings
Although improvements in nutrition behaviors as well as reductions in salt intake are reported across all seven studies, it is important to understand potential bias. Three studies evaluating the impact of nutrition education,16, 18, 19 including cooking low‐salt meals, scored high for the risk of selection bias because of the convenience sampling of their participants. Takada and colleagues21 used randomization to reduce the risk of selection bias in their small sample; however, because participants were not blinded to the intervention, the risk of performance bias was increased because of participant knowledge of which intervention was received, rather than the intervention itself affecting the outcome of the study. While two16, 17 of the six studies evaluating salt intake measured sodium excretion by 24‐hour urine samples, Irwan and colleagues19 estimated salt intake using a salinity checker that was not validated in the population studied nor against a gold standard 24‐hour urine sample, limiting the validity and reliability of the outcome measurement. Of the two studies using 24‐hour urinary sodium as an outcome measurement method, one had a more scientifically robust design: a cluster RCT by Li and colleagues.17 This study reliably reports a statistically significant decrease in salt intake among the study population and provides encouraging evidence that community‐based health education in addition to a low‐sodium salt substitute are effective in reducing dietary salt consumption.
Two of the four studies that showed a reduction in salt intake were conducted in LMICs (China and Vietnam), which is encouraging given the lack of evidence of effective salt reduction strategies in these settings. Three other studies in this review were conducted in East and Southeast Asia (Japan, South Korea, and Indonesia), which suggests an increased impetus to establish effective and acceptable salt reduction strategies in the Asia Pacific region
The WHO has been promoting the use of the SHAKE Technical Package for Salt Reduction22 in this region. While the formulation of a salt reduction strategy will differ in each setting, it is likely the main elements of the strategy will be a combination of actions targeting consumers, industry, and government in addition to strong leadership and political commitment. Key approaches set out by the SHAKE package include a set of evidence‐informed policy options and interventions to lower population salt consumption. In addition, the SHAKE package provides evidence of the efficacy of the recommended interventions and outlines the policies and interventions that have been effective in reducing population salt intake worldwide and would be well utilized in both high‐income as well as LMIC settings.
5. CONCLUSIONS
Controversy about dietary salt largely arises from low‐quality research including poorly established methods for measuring salt intake and short intervention durations, resulting in misleading research outcomes.23, 24, 25 Meta‐analyses of studies on salt and health outcomes using well‐established inclusion criteria, such as that by Aburto and colleagues,26 add value to the growing evidence base and should dispatch with paradoxical findings arising from poorly conducted research. In light of the ongoing challenges of establishing clear evidence of the harmful effect of excess salt intake on health outcomes, the Science of Salt regularly updated systematic and up‐to‐date review of studies is paramount to providing a balanced and objective assessment of the growing evidence and provides a valuable resource for researchers, clinicians, and policy makers involved in the implementation of salt reduction strategies. The recent discussions at the World Health Assembly in Geneva have strengthened the emphasis on the importance of salt reduction as a priority intervention to reduce noncommunicable diseases.27 The further evidence of effectiveness of interventions highlighted in this review can help to inform more sustained and effective program implementation.
CONFLICT OF INTEREST
JAS, KT, ST, CJ, BM, NC, and RM have no conflicts of interest to declare. JW is the Director of the WHO Collaborating Centre on Population Salt Reduction and is supported by a National Health and Medical Research Council/National Heart Foundation Career Development Fellowship on international strategies to reduce salt. JW receives funding from the WHO, VicHealth, and the Australian National Health and Medical Research Council of Australia for research on salt reduction. JW, KT, and JS were authors on the Do et al (2016) study and RM was an author on the Lofthouse et al (2016) study included in this review. NC is a paid consultant to Novartis Foundation on hypertension control in low‐resource settings, a paid consultant to Midway Corp for advice on BP measurement, and an unpaid member of World Action on Salt and Health.
Supporting information
Johnson C, Santos JA, McKenzie B, et al. The Science of Salt: A regularly updated systematic review of the implementation of salt reduction interventions (September 2016–February 2017). J Clin Hypertens. 2017;19:928–938. 10.1111/jch.13099
REFERENCES
- 1. Arcand J, Webster J, Johnson C, et al. Announcing “Up to Date in the Science of Sodium.” J Clin Hypertens (Greenwich). 2016;18:85‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Campbell NR, Appel LJ, Cappuccio FP, et al. A call for quality research on salt intake and health: from the World Hypertension League and supporting organizations. J Clin Hypertens (Greenwich). 2014;16:469‐471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Neal B, Land M, Woodward M. An update on the salt wars—genuine controversy, poor science, or vested interest? Curr Hypertens Rep. 2013;15:687‐693. [DOI] [PubMed] [Google Scholar]
- 4. Johnson C, Raj TS, Trudeau L, et al. The science of salt: a systematic review of clinical salt studies 2013 to 2014. J Clin Hypertens (Greenwich). 2015;17:401‐411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta‐analyses. BMJ. 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Canadian Institute for Health Research and Heart and Stroke Foundation . Science of Salt Weekly e‐newsletter. Hypertension Talk Website. Accessed May 6, 2017.
- 7. Trieu K, McLean R, Johnson C, et al. The science of salt: a regularly updated systematic review of the implementation of salt reduction interventions (November 2015 to February 2016). J Clin Hypertens (Greenwich). 2016;18:1194‐1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Trieu K, McLean R, Johnson C, et al. The science of salt: a regularly updated systematic review of the implementation of salt reduction interventions (June–October 2015). J Clin Hypertens (Greenwich). 2016;18:487‐494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Arcand J, Wong MM, Trieu K, et al. The science of salt: a regularly updated systematic review of salt and health outcomes (June and July 2015). J Clin Hypertens (Greenwich). 2016;18:371‐377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wong MM, Arcand J, Leung AA, et al. The science of salt: a regularly updated systematic review of salt and health outcomes (August to November 2015). J Clin Hypertens (Greenwich). 2016;18:1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Santos JA, Trieu K, Raj TS, et al. The science of salt: a regularly updated systematic review of the implementation of salt reduction interventions (March–August 2016). J Clin Hypertens (Greenwich). 2017;19:439‐451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Johnson C, Raj TS, Trieu K, et al. The science of salt: a systematic review of quality clinical salt outcome studies June 2014 to May 2015. J Clin Hypertens (Greenwich). 2016;18:832‐839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. The Cochrane Collaboration . Cochrane Handbook for Systematic Reviews of Interventions. West Sussex, UK: The Cochrane Collaboration; 2011. [Google Scholar]
- 14. McLaren L, Sumar N, Barberio AM, et al. Population‐level interventions in government jurisdictions for dietary sodium reduction. Cochrane Database Syst Rev. 2016;9:CD010166. [DOI] [PMC free article] [PubMed]
- 15. Do HT, Santos JA, Trieu K, et al. Effectiveness of a Communication for Behavioral Impact (COMBI) intervention to reduce salt intake in a Vietnamese Province based on estimations from spot urine samples. J Clin Hypertens (Greenwich). 2016;18:1135‐1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lofthouse C, Te Morenga L, McLean R. Sodium reduction in New Zealand requires major behaviour change. Appetite. 2016;105:721‐730. [DOI] [PubMed] [Google Scholar]
- 17. Li N, Yan LL, Niu W, et al. The effects of a community‐based sodium reduction program in rural China–a cluster‐randomized trial. PLoS ONE. 2016;11:e0166620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Park S, Lee H, Seo DI, Oh KH, Hwang TG, Choi BY. Educating restaurant owners and cooks to lower their own sodium intake is a potential strategy for reducing the sodium contents of restaurant foods: a small‐scale pilot study in South Korea. Nutr Res Pract. 2016;10:635‐640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Irwan AM, Kato M, Kitaoka K, Ueno E, Tsujiguchi H, Shogenji M. Development of the salt‐reduction and efficacy‐maintenance program in Indonesia. Nurs Health Sci. 2016;18:519‐532. [DOI] [PubMed] [Google Scholar]
- 20. Trieu K, Neal B, Hawkes C, et al. Salt reduction initiatives around the world—a systematic review of progress towards the global target. PLoS ONE. 2015;10:e0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Takada T, Imamoto M, Fukuma S, et al. Effect of cooking classes for housewives on salt reduction in family members: a cluster randomized controlled trial. Public Health. 2016;140:144‐150. [DOI] [PubMed] [Google Scholar]
- 22. World Health Organization . The SHAKE Technical Package for Salt Reduction. Geneva: Switzerland; 2016. [Google Scholar]
- 23. Stolarz‐Skrzypek K, Kuznetsova T, Thijs L, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305:1777‐1785. [DOI] [PubMed] [Google Scholar]
- 24. O'Donnell MJ, Yusuf S, Mente A, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306:2229‐2238. [DOI] [PubMed] [Google Scholar]
- 25. O'Donnell M, Mente A, Rangarajan S, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612‐623. [DOI] [PubMed] [Google Scholar]
- 26. Aburto NJ, Ziolkovska A, Hooper L, et al. Effect of lower sodium intake on health: systematic review and meta‐analyses. BMJ. 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. World Health Organization . Preparation for the third High‐level Meeting of the General Assembly on the Prevention and Control of Non‐communicable Diseases, to be held in 2018. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


