Abstract
Hypertension is an important modifiable cardiovascular risk factor and a leading cause of death throughout Asia. Effective prevention and control of hypertension in the region remain a significant challenge despite the availability of several regional and international guidelines. Out‐of‐office measurement of blood pressure (BP), including home BP monitoring (HBPM), is an important hypertension management tool. Home BP is better than office BP for predicting cardiovascular risk and HBPM should be considered for all patients with office BP ≥ 130/85 mm Hg. It is important that HBPM is undertaken using a validated device and patients are educated about how to perform HBPM correctly. During antihypertensive therapy, monitoring of home BP control and variability is essential, especially in the morning. This is because HBPM can facilitate the choice of individualized optimal therapy. The evidence and practice points in this document are based on the Hypertension Cardiovascular Outcome Prevention and Evidence (HOPE) Asia Network expert panel consensus recommendations for HBPM in Asia.
Keywords: blood pressure control, clinical practice, guidelines, home blood pressure monitoring, hypertension, Pfizer
1. INTRODUCTION
Hypertension is one of the major modifiable risk factors for cardiovascular disease. It represents an important public health issue, particularly in South East Asia, where the disease kills nearly 1.5 million people each year.1 This is likely due, at least in part, to absent or poor disease management, with rates of uncontrolled hypertension as high as 70%‐95% in South Asia.2
Although several countries or regions in Asia have local guidelines for the diagnosis and management of hypertension,3, 4, 5, 6, 7, 8 effective prevention and control of hypertension remain a significant challenge in the region. A number of potential barriers could contribute to this problem, including cultural norms that promote unhealthy behaviors and misconceptions about hypertension, high rates of cigarette smoking, healthcare disparities, high out‐of‐pocket treatment costs, and poor adherence to treatment.9 It is also possible that the volume of information prevents busy clinicians from identifying the most important points for their own clinical practice.
Out‐of‐office measurement of blood pressure (BP), including ambulatory and home BP monitoring (ABPM and HBPM, respectively), is recognized internationally as an important tool to facilitate effective detection and management of hypertension, and to monitor BP variability.5, 10, 11, 12, 13 Deficits in knowledge about out‐of‐office BP measurement and gaps in clinical practice among general practitioners and specialists have recently been identified in Singapore.14 This is likely to reflect the situation elsewhere in Asia, highlighting the need for accessible, key evidence‐based information for physicians.
The Hypertension Cardiovascular Outcome Prevention and Evidence (HOPE) Asia Network, recently studied the current evidence of HBPM15 and developed a set of expert panel consensus recommendations for HBPM in Asia.16 Here, we provide the key messages and practice points (Figure 1) that can be easily implemented in clinical practice.
Figure 1.
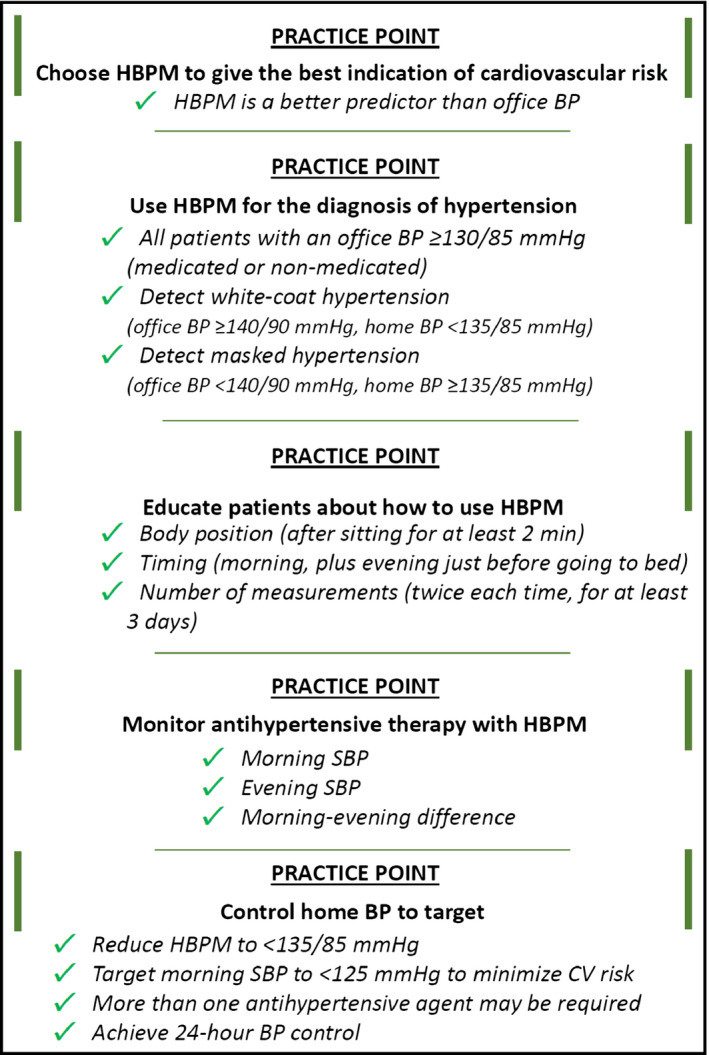
Practice points
2. WHY IS HOME BP MANAGEMENT SO IMPORTANT?
It has been recognized that one‐off, irregular measurements of BP at office visits may not provide the most realistic representation of a patient's BP during normal activities of daily living.11, 17 Home BP measurements are important for detecting “white‐coat” hypertension (office BP ≥ 140/90 mm Hg but home BP < 135/85 mm Hg) and “masked” hypertension (office BP < 140/90 mm Hg but home BP ≥ 135/85).17 HBPM also allows quantification and monitoring of blood pressure variability (BPV), something that is increasingly being recognized as playing an important role in overall cardiovascular risk.18
High systolic BP (SBP) measured using HBPM has been shown to significantly increase the risk of major cardiovascular events. The Home Blood Pressure Measurement With Olmesartan‐Naive Patients to Establish Standard Target Blood Pressure (HONEST) study was a large‐scale prospective observational trial that included 21 591 patients treated with olmestartan‐based BP‐lowering therapy for 2 years in Japan.19 The risk of a major cardiovascular event was significantly increased when morning, evening, or averaged morning and evening home BP was ≥145 mm Hg and when office SBP was ≥150 mm Hg (Figure 2).19 In addition, patients with masked hypertension and a high morning SBP were at high risk of cardiovascular events even when office SBP was normal.19 Another analysis of HONEST study data showed that morning home SBP ≥ 155 mm Hg was associated with a > 6‐fold increase in the risk of developing coronary artery disease (hazard ratio [HR] 6.24, 95% confidence interval [CI] 2.82‐13.84).20 The risk associated with an office SBP of ≥160 mm Hg was also significant, but substantially lower in comparison (HR 3.51; 95% CI: 1.71‐7.20).20 The results of another study from Japan showed that the addition of morning home SBP improved the ability to predict incident stroke, over and above traditional risk factors.21 Other studies conducted in Europe have also documented improved prediction of cardiovascular risk using home‐based measurement of BP compared with office BP measurements.22, 23
Figure 2.
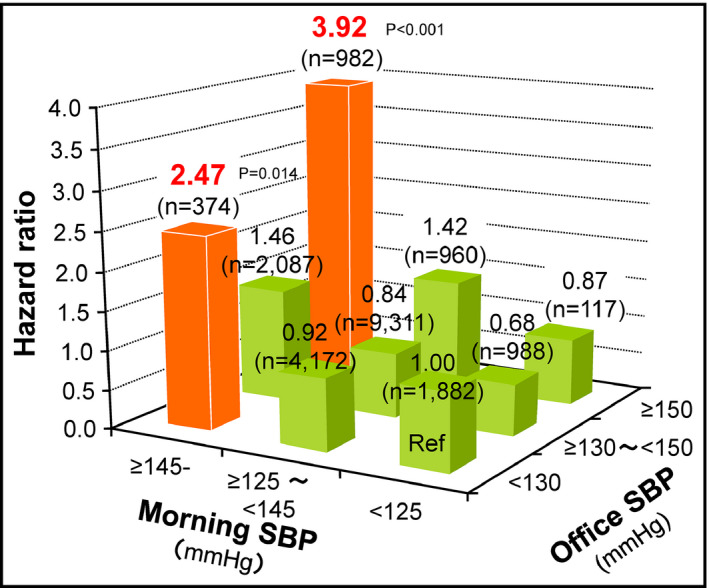
On‐treatment home and office systolic blood pressure and risk of cardiovascular events in medicated patients with hypertension, adjusted for sex, age, family history of cardiovascular disease, dyslipidemia, diabetes mellitus, chronic kidney disease, history of cardiovascular disease, and smoking status (HONEST study).20 SBP, systolic blood pressure
In Asia, due to the local lifestyle, measurement of evening home BP before dinner is uncommon, and measurement of home BP in the evening just before going to bed is recommended in the Japanese guidelines5 and the Chinese guidance document.24 However, measurements of evening home BP taken at this time are strongly influenced by recent food and alcohol consumption, and by evening behavior (eg, bathing).25 In contrast, morning BP measurements have better reproducibility than both evening home BP and office BP assessments. Asian patients with hypertension have been shown to have an exaggerated morning BP surge, which is a risk factor for stroke26 and higher morning BP levels than Westerners.27, 28
Taken together, the above data highlight the importance of monitoring and controlling home BP, especially morning home BP in Asians, for reducing the risk of cardiovascular events. The data also emphasize the superiority of HBPM over office BP measurements for effective cardiovascular risk management.
3. WHO NEEDS HOME BP MONITORING?
Home BP monitoring provides useful additional information to office BP measurements for the diagnosis and monitoring of hypertension in all patients, medicated or non‐medicated. For hypertension diagnosis, HBPM is particularly useful for the detection of possible white coat or masked hypertension.17 In the majority of patients receiving antihypertensive therapy, HBPM helps to inform treatment decisions, monitor the effectiveness of antihypertensive therapy, support dose adjustments, provide information about treatment adherence, evaluate BP control and BPV, and identify drug‐resistant hypertension.29 Home BP measurements are particularly valuable in high‐risk patients with additional cardiovascular risk factors, including obesity, metabolic syndrome, diabetes mellitus, chronic kidney disease, obstructive sleep apnea syndrome, organ damage, and/or a history of cardiovascular disease.
4. HOW AND WHEN SHOULD HOME BP BE MEASURED?
A validated brachial BP measuring oscillometric device should be used for measuring home BP.5, 6, 17, 24 Where and when this is not feasible, the device of choice should be calibrated every 6‐12 months.
It is recommended that home BP measurements be taken in the seated position (feet flat on the floor, with the back and arm supported) after 2 minutes of rest, preferably with a delay of at least 30 minutes after exercise, smoking, or caffeine/alcohol consumption.16 Morning BP measurements should be taken within 1 hour of waking, after urination, before breakfast, and prior to taking any antihypertensive medication. Evening BP measurements should be taken before going to bed.16 Patients need to take at least 2 BP readings each time, with a 1‐minute interval between measurements.16 The average of at least 2 BP measurements over at least 3 days (preferably 7 days) should be calculated separately for morning and evening values.16
It is important to provide all patients using HBPM with good information and training about the above requirements for home BP measurement. This should include a practical demonstration, written information to take away, and details about where to find additional support if required.29
5. HOW ARE HOME BP READINGS ASSESSED?
Home BP monitoring is an accurate adjunct for diagnosing hypertension when a validated device is used and the measurement is performed correctly.16, 30 When using HBPM, patients are taking their BP at a similar time(s) and under similar conditions each day, which means that HBPM should have good reproducibility.31 Another advantage of HBPM is the ability to collect information about BP over long periods of time,31 making this the preferred method for evaluating BPV according to the Japanese hypertension guidelines.5
Important measures captured during HBPM and their definitions are shown in Table. The morning‐evening difference in BP is important because this has been associated with left ventricular hypertrophy and cardiac remodeling, and is an independent risk factor for cardiovascular disease and stroke.32, 33, 34, 35
Table 1.
Summary of key home blood pressure monitoring metrics
| Measure | Definition |
|---|---|
| Morning SBP | Average of 2 consecutive values taken each morning over several days (at least 3) |
| Maximum morning SBP | Maximum of the average of 2 consecutive values taken each morning over several (≥3) days |
| Day‐by‐day morning SBP variability | Standard deviation of morning values taken over several days (at least 3 d) |
| Morning/evening difference | Morning SBP minus evening SBP |
| Home morning BP surgea | Morning SBP minus sleep SBPa |
| Orthostatic morning SBP change | Standing morning SBP minus sitting morning SBP |
BP, blood pressure; SBP, systolic blood pressure.
Can only be determined using nocturnal home BP monitoring.36
In situations where patients have taken >2 measurements at a particular recording time because the first 2 values were markedly different, it might be most appropriate to only include the last 2 measurements when calculating the average value.29 It is also suggested that recordings obtained on the first day of HBPM be discarded and not included in average calculations.29 It is important to remember that HBPM‐derived BP values should be increased by 5/5 mm Hg to give an indication of the comparable reading in an office setting (ie, home BP of 135/85 mm Hg is equivalent to a reading of 140/90 mm Hg in the clinic).29
6. WHAT ARE THE BEST WAYS TO CONTROL HOME BP?
The beneficial effects of antihypertensive therapy appear to be related primarily to the lowering of BP, rather than the specific agent used.37 Calcium channel blockers (CCBs), angiotensin converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs) are the most widely used antihypertensive agents. Factors to take into account in initial drug choice include patient age, comorbid conditions and/or end‐organ damage, potential drug interactions, likelihood of adherence, cost, and patient preference. In clinical practice, morning home BP‐guided titration of antihypertensive drugs is the first step to achieving good 24‐hour BP control, which consists of 3 main components: lowering 24‐hour BP; keeping normal circadian rhythm (dipper‐type); and suppressing exaggerated BPV, especially for morning surge.38
For patients with an exaggerated morning BP surge, a long‐acting agent is required. The most suitable agent might be a long‐acting CCB; a long‐acting ACE inhibitor or ARB could also be useful. If morning SBP cannot be lowered to <135 mm Hg, bedtime dosing of these agents, or an alpha blocker, could also be considered. When nocturnal hypertension is a problem (ie, patients classified as “riser” or “non‐dipper”), diuretics may be useful, usually in combination with an ACE inhibitor or ARB. Bedtime (or evening) dosing of an ARB, CCB, or alpha blocker could also be appropriate.39, 40, 41
A reasonable proportion of patients with hypertension, and particularly those with comorbidities, will not achieve BP targets with single‐agent therapy.42 Most will need a combination of ≥ 2 antihypertensive agents to lower BP to target levels.43 Effective combination therapies include thiazide or thiazide‐type diuretics with an ARB, ACE inhibitor, or CCB, or a CCB with an ARB or ACE inhibitor.10, 44 For second‐line therapy it might be useful to consider BPV parameters when choosing the most appropriate therapy.45 The combination of a CCB and an ARB is superior to the CCB+ diuretic combination for reducing uncontrolled nocturnal hypertension.28 However, the latter is more effective in patients with isolated systolic hypertension.
Guidelines recommend that BP assessed using HBPM be lowered to <135/85 mm Hg for patients aged <80 years and <145/85 mm Hg for those aged ≥80 years5, 10, 11, 16 Tight BP control targeting a home SBP of <125 mm Hg may be beneficial in high‐risk Asian patients with hypertension, particularly those with diabetes mellitus, chronic kidney disease, and/or cardiovascular disease.16 Based on the results of the HONEST study,20 a 3‐tier approach to controlling home SBP is recommended, in which the initial target for morning SBP should be to <145 mm Hg (even for patients with controlled office BP), then the home morning SBP target should be <135 mm Hg (as recommended in most guidelines), with further reduction to 125 mm Hg to minimize cardiovascular risk as much as possible (Figure 3).38 However, in the real world setting, when implementing morning home BP‐guided therapy in very elderly patients (age > 80 years), the clinician needs to pay careful attention to patient tolerance of therapy, frailty, orthostatic hypotension, and acute kidney injury, especially in the hot summer season.
Figure 3.

Three‐step strategy for morning blood pressure targets (mm Hg) with home blood pressure monitoring during antihypertensive treatment
Incorporation of HBPM into routine management of patients with hypertension has been shown to reduce both systolic and diastolic BP to a greater extent compared with usual care.46, 47, 48 Improvements in BP control have been documented when patients used HBPM,47, 48 and antihypertensive medication adherence is also better.49 In the first trial assessing cardiovascular outcomes in hypertensive patients whose antihypertensive treatment was guided by the results of HBPM, BP levels achieved were generally lower than those in trials where treatment was adjusted based on office BP.50
7. CONCLUSIONS
HBPM plays an important role in hypertension management. It can facilitate the diagnosis of hypertension, especially white‐coat and masked hypertension, and improve control of BP during antihypertensive therapy. In addition, home BP measurements provide better prediction of cardiovascular risk than office BP, and controlling morning home BP makes an important contribution to the prevention of hypertension‐related organ damage and cardiovascular events, especially in Asia. Implementation of the practice points provided should help clinicians incorporate HBPM into their everyday practice and help improve patient outcomes.
STATEMENT OF FINANCIAL DISCLOSURE
K Kario has received research grants from A&D Co., Bayer Yakuhin, Boehringer Ingelheim, Daiichi Sankyo, EA Pharma, Fukuda Denshi, Medtronic, Mitsubishi Tanabe Pharma Corporation, Mochida Pharmaceutical Co., Omron Healthcare, Otsuka, Takeda, and Teijin Pharma Co.; and honoraria from Daiichi Sankyo, Omron Healthcare, and Takeda. S Park has received research grants and honoraria from Pfizer. S Siddique has received honoraria from Bayer, GlaxoSmithKline, Pfizer, ICI, and Servier; and travel, accommodation and conference registration support from Atco Pharmaceutical, Highnoon Laboratories, Horizon Pharma, ICI, and Pfizer. YC Chia has received honoraria and sponsorship to attend conferences and CME seminars from Abbott, Bayer, Boehringer Ingelheim, GlaxoSmithKline, Menarini, Merck Sharp & Dohme, Novartis, Orient Europharma, Pfizer, and Sanofi; and a research grant from Pfizer. CH Chen has received honoraria as a member of a speaker's bureau for Pfizer. R Divinagracia has received honoraria as a member of speakers’ bureaus for Bayer, Novartis, and Pfizer. J Sison has received honoraria from Pfizer, AstraZeneca, Boehringer Ingelheim and Novartis. GP Sogunuru has received a research grant related to hypertension monitoring and treatment from Pfizer. JC Tay has received advisory board and consultant honoraria from Pfizer. JG Wang has received research grants from Bayer, Pfizer, and Phillips; and lecture and consulting fees from Bayer, Daiichi‐Sankyo, Merck Sharp & Dohme, Pfizer, Sanofi, and Servier. L Wong has received honoraria from Bristol‐Myers Squibb and Pfizer. Y Zhang has received research grants from Bayer, Novartis, and Shuanghe; and lecture fees from Bayer, Daiichi Sankyo, Novartis, Pfizer, Sanofi, Servier, and Takeda. All other authors report no potential conflicts of interest in relation to this article.
Writing and editorial support was provided by Nicola Ryan, independent medical writer; this support was funded by Pfizer.
Kario K, Park S, Buranakitjaroen P, et al. Guidance on home blood pressure monitoring: A statement of the HOPE Asia Network. J Clin Hypertens. 2018;20:456–461. 10.1111/jch.13216
This study was done on Behalf of the Hypertension Cardiovascular Outcome Prevention and Evidence (HOPE) Asia Network.
REFERENCES
- 1. World Health Organisation . Hypertension fact sheet. http://www.searo.who.int/entity/noncommunicable_diseases/media/non_communicable_diseases_hypertension_fs.pdf?ua=1. Accessed June 7, 2017.
- 2. Gupta R. SSA 02‐3 Trend in hypertension epidemiology in south Asia. J Hypertens. 2016;34(Suppl 1):e2. [Google Scholar]
- 3. Chiang CE, Wang TD, Ueng KC, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015;78:1‐47. [DOI] [PubMed] [Google Scholar]
- 4. Liu LS. Writing Group of Chinese Guidelines for the Management of H [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:579‐615. [PubMed] [Google Scholar]
- 5. Shimamoto K, Ando K, Fujita T, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253‐390. [DOI] [PubMed] [Google Scholar]
- 6. Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension: part III‐hypertension in special situations. Clin Hypertens. 2015;21:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension. Part II‐treatments of hypertension. Clin Hypertens. 2015;21:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shin J, Park JB, Kim KI, et al. 2013 Korean Society of Hypertension guidelines for the management of hypertension: part I‐epidemiology and diagnosis of hypertension. Clin Hypertens. 2015;21:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Castillo R. SSA 03‐1 prevalence and management of hypertension in Southeast Asia. J Hypertens. 2016;34(Suppl 1):e4. [Google Scholar]
- 10. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC practice guidelines for the management of arterial hypertension. Blood Press. 2014;23:3‐16. [DOI] [PubMed] [Google Scholar]
- 11. National Institute for Health and Care Excellence . Hypertension: clinical management of primary hypertension in adults (update). Clinical guideline 127. (2011) https://www.nice.org.uk/guidance/cg127/chapter/1-guidance. Accessed December 25, 2016.
- 12. Kario K. Evidence and Perspectives on the 24‐hour Management of Hypertension: hemodynamic Biomarker‐Initiated ‘Anticipation Medicine’ for Zero Cardiovascular Event. Prog Cardiovasc Dis. 2016;59:262‐281. [DOI] [PubMed] [Google Scholar]
- 13. Kario K, Tomitani N, Kanegae H, et al. Development of a new ICT‐based multisensor blood pressure monitoring system for use in hemodyanmic biomarker‐initiated anticipation medicine for cardiovascular disease. The National IMPACT Program Project. Prog Cardiovasc Dis. 2017;60:435‐449. [DOI] [PubMed] [Google Scholar]
- 14. Setia S, Subramaniam K, Teo BW, Tay JC. Ambulatory and home blood pressure monitoring: gaps between clinical guidelines and clinical practice in Singapore. Int J Gen Med. 2017;10:189‐197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chia Y‐C, Buranakitjaroen P, Chen C‐H, et al. Current status of home blood pressure monitoring in Asia ‐ statement from the HOPE Asia Network. J Clin Hypertens (Greenwich). 2017;19:1192‐1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Park S, Buranakitjaroen P, Chen C‐H, et al. Expert panel consensus recommendations for home blood pressure monitoring in Asia: the HOPE Asia Network. J Hum Hypertens 2017. [in press]. [DOI] [PubMed] [Google Scholar]
- 17. Parati G, Stergiou G, O'Brien E, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359‐1366. [DOI] [PubMed] [Google Scholar]
- 18. Stevens SL, Wood S, Koshiaris C, et al. Blood pressure variability and cardiovascular disease: systematic review and meta‐analysis. BMJ. 2016;354:i4098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kario K, Saito I, Kushiro T, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large‐scale prospective, real‐world observational study. Hypertension. 2014;64:989‐996. [DOI] [PubMed] [Google Scholar]
- 20. Kario K, Saito I, Kushiro T, et al. Morning home blood pressure is a strong predictor of coronary artery disease: the HONEST study. J Am Coll Cardiol. 2016;67:1519‐1527. [DOI] [PubMed] [Google Scholar]
- 21. Hoshide S, Yano Y, Haimoto H, et al. Morning and evening home blood pressure and risks of incident stroke and coronary artery disease in the Japanese general practice population: the Japan Morning Surge‐Home Blood Pressure Study. Hypertension. 2016;68:54‐61. [DOI] [PubMed] [Google Scholar]
- 22. Niiranen TJ, Hanninen MR, Johansson J, Reunanen A, Jula AM. Home‐measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure: the Finn‐Home study. Hypertension. 2010;55:1346‐1351. [DOI] [PubMed] [Google Scholar]
- 23. Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self‐measurement in elderly treated hypertensive patients. JAMA. 2004;291:1342‐1349. [DOI] [PubMed] [Google Scholar]
- 24. Wang JG. Chinese hypertension guidelines. Pulse (Basel). 2015;3:14‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fujiwara T, Hoshide S, Nishizawa M, Matsuo T, Kario K. Difference in evening home blood pressure between before dinner and at bedtime in Japanese elderly hypertensive patients. J Clin Hypertens (Greenwich). 2017;19:731‐739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401‐1406. [DOI] [PubMed] [Google Scholar]
- 27. Hoshide S, Kario K, de la Sierra A, et al. Ethnic differences in the degree of morning blood pressure surge and in its determinants between Japanese and European hypertensive subjects: data from the ARTEMIS study. Hypertension. 2015;66:750‐756. [DOI] [PubMed] [Google Scholar]
- 28. Kario K, Bhatt DL, Brar S, Bakris GL. Differences in dynamic blood pressure variability between Japanese and American treatment‐resistant hypertensive populations. Circulation J. 2017;81:948‐957. [DOI] [PubMed] [Google Scholar]
- 29. British Hypertension Society . Home blood pressure monitoring protocol. http://www.bhsoc.org/files/4414/1088/8031/Protocol.pdf. Accessed 7 Jun 2017.
- 30. Imai Y, Otsuka K, Kawano Y, et al. Japanese society of hypertension (JSH) guidelines for self‐monitoring of blood pressure at home. Hypertens Res. 2003;26:771‐782. [DOI] [PubMed] [Google Scholar]
- 31. Imai Y, Obara T, Asamaya K, Ohkubo T. The reason why home blood pressure measurements are preferred over clinic or ambulatory blood pressure in Japan. Hypertens Res. 2013;36:661‐672. [DOI] [PubMed] [Google Scholar]
- 32. Johansson JK, Niiranen TJ, Puukka PJ, Jula AM. Prognostic value of the variability in home‐measured blood pressure and heart rate: the Finn‐Home Study. Hypertension. 2012;59:212‐218. [DOI] [PubMed] [Google Scholar]
- 33. Matsui Y, Eguchi K, Shibasaki S, Ishikawa J, Shimada K, Kario K. Morning hypertension assessed by home monitoring is a strong predictor of concentric left ventricular hypertrophy in patients with untreated hypertension. J Clin Hypertens (Greenwich). 2010;12:776‐783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Matsui Y, Eguchi K, Shibasaki S, et al. Association between the morning‐evening difference in home blood pressure and cardiac damage in untreated hypertensive patients. J Hypertens. 2009;27:712‐720. [DOI] [PubMed] [Google Scholar]
- 35. Shibuya Y, Ikeda T, Gomi T. Morning rise of blood pressure assessed by home blood pressure monitoring is associated with left ventricular hypertrophy in hypertensive patients receiving long‐term antihypertensive medication. Hypertens Res. 2007;30:903‐911. [DOI] [PubMed] [Google Scholar]
- 36. Kario K, Hoshide S, Haimoto H, et al. Sleep blood pressure self‐measured at home as a novel determinant of organ damage: Japan Morning Surge Home Blood Pressure (J‐HOP) study. J Clin Hypertens (Greenwich). 2015;17:340‐348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 4. Effects of various classes of antihypertensive drugs‐overview and meta‐analyses. J Hypertens. 2015;33:195‐211. [DOI] [PubMed] [Google Scholar]
- 38. Kario K. Essential Manual of 24‐Hour Blood Pressure Management from Morning To Nocturnal Hypertension. London, UK: Wiley‐Blackwell; 2015:1‐138. [Google Scholar]
- 39. Kario K, Hoshide S, Shimizu M, et al. Effect of dosing time of angiotensin II receptor blockade titrated by self‐measured blood pressure recordings on cardiorenal protection in hypertensives: the Japan Morning Surge‐Target Organ Protection (J‐TOP) study. J Hypertens. 2010;28:1574‐1583. [DOI] [PubMed] [Google Scholar]
- 40. Kario K, Matsui Y, Shibasaki S, et al. An alpha‐adrenergic blocker titrated by self‐measured blood pressure recordings lowered blood pressure and microalbuminuria in patients with morning hypertension: the Japan Morning Surge‐1 Study. J Hypertens. 2008;26:1257‐1265. [DOI] [PubMed] [Google Scholar]
- 41. Mizuno H, Hoshide S, Tomitani N, Kario K. Comparison of ambulatory blood pressure‐lowering effects of higher doses of different calcium antagonists in uncontrolled hypertension: the Calcium Antagonist Controlled‐Release High‐Dose Therapy in Uncontrolled Refractory Hypertensive Patients (CARILLON) Study. Blood Press. 2017;26:284‐293. [DOI] [PubMed] [Google Scholar]
- 42. Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988‐2000. JAMA. 2003;290:199‐206. [DOI] [PubMed] [Google Scholar]
- 43. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507‐520. [DOI] [PubMed] [Google Scholar]
- 44. PROGRESS Collaborative Group . Randomised trial of a perindopril‐based blood‐pressure‐lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033‐1041. [DOI] [PubMed] [Google Scholar]
- 45. Kario K. Proposal of RAS‐diuretic vs. RAS‐calcium antagonist strategies in high‐risk hypertension: insight from the 24‐hour ambulatory blood pressure profile and central pressure. J Am Soc Hypertens. 2010;4:215‐218. [DOI] [PubMed] [Google Scholar]
- 46. Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta‐analysis. Hypertension. 2011;57:29‐38. [DOI] [PubMed] [Google Scholar]
- 47. Bray EP, Holder R, Mant J, McManus RJ. Does self‐monitoring reduce blood pressure? Meta‐analysis with meta‐regression of randomized controlled trials. Ann Med. 2010;42:371‐386. [DOI] [PubMed] [Google Scholar]
- 48. Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta‐analysis of randomised trials. BMJ. 2004;329:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ogedegbe GO, Boutin‐Foster C, Wells MT, et al. A randomized controlled trial of positive‐affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med. 2012;172:322‐326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Asayama K, Ohkubo T, Metoki H, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self‐measured home blood pressure. Hypertens Res. 2012;35:1102‐1110. [DOI] [PubMed] [Google Scholar]


