The term white‐coat hypertension (WCH) refers to a condition characterized by an elevation of blood pressure (BP) in the office with normal ambulatory or home values. Previous studies have estimated a prevalence of this condition ranging from 15‐20% to 40‐50% of individuals with elevated office BP. A controversy currently exists on whether WCH is a benign phenomenon and how it should be best defined. Some studies suggest that patients with the condition have a risk of cardiovascular events similar to patients with normotension, whereas others document an increased rate of target organ damage and cardiovascular events.1 In some patients, WCH may deteriorate to persistent hypertension in the future, leading to the risk of cardiovascular events as a long‐term outcome. Individuals with high‐normal BP, additional cardiovascular risk factors (eg, obesity, metabolic syndrome, advanced age, and impaired glucose tolerance), and organ damage may be particularly susceptible to a poor prognosis in the presence of WCH. According to two recent meta‐analyses, WCH is associated with a slightly increased risk of cardiovascular events compared with normotension, although this risk is well below that seen in either persistent hypertension or masked hypertension. Briasoulis et al2 analyzed 14 studies with 29 100 participants and showed that individuals with WCH had higher rates of cardiovascular disease morbidity and mortality but not significantly different all‐cause mortality and stroke risk compared with patients with normotension. Huang et al3 analyzed 23 cohorts of 20 445 untreated individuals, 11 cohorts of 8656 treated individuals, and a mixed population including both treated and untreated patients (12 cohorts, 21 336 individuals) and concluded that WCH is associated with long‐term risk of cardiovascular disease and total mortality in untreated and mixed populations but not in treated patients. All of the studies included in these meta‐analyses based categorization of WCH either on ambulatory or home BP. In case of ambulatory BP, the most common definition of WCH was based on daytime BP only, thus excluding nighttime BP. However, many people have normotension during waking hours and hypertension during night sleep, and may thus be mistakenly classified as having WCH. Yet, there are few data comparing the prevalence and consequences of using daytime (awake), full 24‐hour, rather than nighttime (sleep), periods to define WCH. In fact, heterogeneity among recommendations from the different guidelines exists and there is currently controversy on which period of the day is most suitable for defining WCH (Table 1).
Table 1.
Current definitions of WCH according to major hypertension guidelines
| Guideline | Common term for defining WCH | Current definition | Unclear points |
|---|---|---|---|
| Europe4 | White‐coat (or isolated office) hypertension | Untreated individuals with elevated office BP (≥ 140/90 mm Hg), 24‐h BP < 130/80 mm Hg, awake BP < 135/85 mm Hg, and sleep BP < 120/70 mm Hg | The term white‐coat effect is used in both treated and untreated individuals |
| United States5 | WCH | Untreated individuals with office BP ≥ 130/80 mm Hg but <160/100 mm Hg and daytime BP < 130/80 mm Hg | In treated individuals the term white‐coat effect is used |
| Canada6 | WCH | Untreated individuals with elevated office BP (≥ 140/90 mm Hg), 24‐h BP < 130/80 mm Hg, and awake BP < 135/85 mm Hg | Nighttime BP not included in the categorization. No mention of treated individuals |
| United Kingdom7 | WCH | Elevated clinic BP (≥140/90 mm Hg) and daytime BP < 135/85 mm Hg | The term white‐coat effect is used in both treated and untreated individuals |
| Latin America8 | WCH | Patients with hypertensive values in the office and normal values with ABPM | No mention of which period of the 24 h is suitable for categorization |
| Australia9 | White‐coat (or isolated clinic) hypertension | Untreated individuals with elevated office BP (≥ 140/90 mm Hg) and daytime BP < 135/85 mm Hg | No mention of treated patients |
| Japan10 | WCH | Untreated individuals with elevated office BP (≥ 140/90 mm Hg) and 24‐h BP < 130/80 mm Hg | The condition is defined as WCH under treatment in patients receiving treatment |
ABPM, ambulatory blood pressure monitoring; BP, blood pressure; WCH, white‐coat hypertension.
The article by Anstey et al,11 published in the present issue of the Journal of Clinical Hypertension, may help yield further evidence to unravel the dispute. In their study, based on a relatively large sample of black individuals in the community‐based prospective cohort Jackson Heart Study, the authors showed that the prevalence of WCH may substantially vary according to the periods of the 24 hours used for classification. When only the daytime period was selected (average BP < 135/85 mm Hg with office systolic BP ≥ 140 or office diastolic BP ≥ 90 mm Hg), 29.6% of patients were categorized as having WCH. When daytime and 24‐hour averages (BP < 130/80 mm Hg) were used, a 21.1% prevalence rate of WCH was found. The lowest prevalence rate of WCH (10.6%) was observed when daytime, 24‐hour, and nighttime (BP < 120/70 mm Hg) average BPs were considered together. The present study confirms previous observations from two large studies, namely that the lowest prevalence of WCH is found when the calculation includes daytime, nighttime, and 24‐hour average BP (Table 2). In untreated patients in the Spanish Registry and in the International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes (IDACO) consortium, the prevalence of WCH when considering normal values for all 24‐hour daytime and nighttime BPs was 26.1% and 6.3%, respectively; values much lower than 41.3% and 9.1% of the prevalence based on inclusion of daytime BP only.12, 13
Table 2.
Prevalence of WCH according to different setting thresholds in three cohort studies
| Study | Patients, No. | Ethnicity (%) | WCH defined on daytime BP only, % | WCH defined on 24‐h BP only, % | WCH defined on daytime, nighttime, and 24‐h BP, % |
|---|---|---|---|---|---|
| Spanish Registry12 | 33 855 Untreated patients | White (100) | 41.3 | 35.2 | 26.1 |
| 53 451 Treated patients | White (100) | 45.8 | 38.9 | 27.2 | |
| IDACO13 | 2449 Untreated patients | White (75.3) | 9.1 | 10.7 | 6.3 |
| Jackson Heart Study14 | 199 Untreated or treated patients | Black (100) | 29.6 | 21.1a | 10.6 |
IDACO, International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes; WCH, white‐coat hypertension.
24‐Hour plus daytime blood pressure (BP).
These results support the concept that the definition of WCH must always include night sleep since BP in this period is a potent predictor of outcomes. This is particularly true for blacks, an ethnic group with a high prevalence of hypertension during sleep, as shown in a previous publication by the same authors of the Jackson Heart Study.14 If nocturnal sleep BP is not included in the definition of WCH, overdiagnosis of the condition may occur instead of correctly labeling patients as having sustained hypertension.
The hypothesis that a working definition of WCH should include all normal BPs over the 24‐hour, day and night period is sustained by the results of the Jackson Heart Study related to cardiac organ damage. The new finding provided by the study is that left ventricular mass index (LVMI) was significantly higher in patients with WCH than in those with normotension, but only when the condition was defined according to daytime values (80.6 ± 22.1 vs 72.7 ± 17.9 g/m2, P = 0.003). Conversely, the difference was much smaller and not statistically significant when the definition also included nighttime and 24‐hour BPs (76.0 ± 14.1 g/m2, P = 0.400 vs normotension). Furthermore, the prevalence of left ventricular hypertrophy (LVH) was similar between patients with normotension and those with WCH calculated from all ambulatory periods (7.0% vs 4.8%, P = 0.700) and lesser than that observed in those with WCH categorized by daytime BP only (10.2%). These results are also in line with those of the Spanish Registry and the IDACO consortium.12, 13 In the Spanish Registry, the proportion of patients with LVH in the WCH group based on normal values of all ambulatory periods was 1.4%, and similar to that found in the normotensive group (1.3%), whereas the prevalence of LVH ranged between 1.9% and 2.0% in the other two WCH groups. In multivariate analyses of the IDACO consortium, the hazard ratio for a cardiovascular event associated with WCH compared with normotension progressively weakened when considering daytime only (1.38; P = 0.033) to 24‐hour plus daytime plus nighttime (1.16; P = 0.410).
Some additional aspects of the Jackson Heart Study deserve to be discussed. The fact that 47.3% of patients with sustained normotension and 66.7% of those with WCH used antihypertensive medications may pose a problem for correct data interpretation. The authors decided not to evaluate treated and untreated patients separately. Although after adjustment for various confounding factors, including antihypertensive medication use, the mean LVMI was only 0.4 g/m2 larger than the unadjusted one, it is well known that both the prevalence and long‐term cardiovascular consequences of WCH may differ in untreated and treated patients. In the Spanish Registry, the prevalence of WCH estimated by using daytime BP only or 24‐hour BP only was 41.3% and 35.2% in untreated and 45.8% and 38.9% in treated patients, respectively (Table 2).12 The difference in the proportion of patients with WCH was smaller between untreated and treated patients when all ambulatory periods were considered for the categorization (26.1% vs 27.2%). In a pooled data analysis of the International Database of Home Blood Pressure in Relation to Cardiovascular Outcome (IDHOCO) consortium including five population studies and 6458 participants and based on home BP monitoring, Stergiou et al15 showed that among untreated patients, cardiovascular risk was high in those with WCH compared with individuals with normotension (hazard ratio [HR], 1.42; 95% confidence interval [CI], 1.06–1.91 [P = 0.001]), whereas, among treated patients, the cardiovascular risk did not differ between the two groups (HR, 1.16; 95% CI, 0.79–1.72 [P = 0.45]). In a recent publication of the Spanish Registry including 63 910 patients,16 the proportion of patients with WCH was larger in treated patients (17.3% vs 10.4% untreated). However, the risk for cardiovascular mortality and all‐cause death during 4.7 years of follow‐up was negligible as compared with patients with normotension for white‐coat (treated) uncontrolled hypertension (HR, 1.04; 95% CI, 0.65–1.66 [P = 0.860] and HR, 1.06; 95% CI, 0.82–1.37 [P = 0.660], respectively), but not for untreated patients (HR, 1.96; 95% CI, 1.22–3.15 [P = 0.005] and HR, 1.79; 95% CI, 1.38–2.32 [P < 0.001]). These large cohort studies suggest that WCH is associated with different risk in untreated and treated individuals, probably because the latter receive effective treatment during the 24 hours. Consequently, WCH should be managed appropriately according to the treatment status of the patient. In the Jackson Heart Study, a separate analysis according to treatment was not provided, as a result of the small sample size.
The inclusion of nighttime BP in the definition of WCH, as appropriately included in the study by Anstey et al, is crucial to the optimal stratification of patient risk. This is strengthened by a comparison with LVMI results of a meta‐analysis of 2493 patients with normotension and 1705 untreated patients with WCH. In the individuals with WCH included in the meta‐analysis, the mean LVMI was much larger (95.7 ± 1.8 g/m2) than that observed in the same group included in the Jackson Heart Study (76.0 ± 14.1 g/m2).17 Furthermore, the difference in LVMI between the WCH and the normotension groups was much larger in the meta‐analysis (+7.6 g/m2 vs +3.3 g/m2 in the Jackson Heart Study). However, in the meta‐analysis by Cuspidi et al,17 the majority of studies categorized WCH using daytime BP only and did not specifically include nighttime BP (Figure 1).
Figure 1.
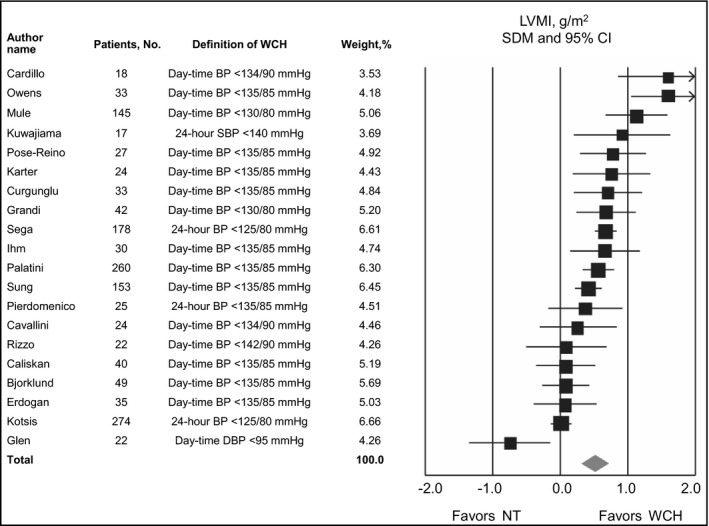
Standardized difference in mean (SDM) and 95% confidence interval (CI) of left ventricular mass index (LVMI) in a meta‐analysis. NT, normotension; WCH, white‐coat hypertension. (Redrawn with permission from Cuspidi et al.17)
Although some methodological aspects of the Jackson Heart Study (eg, inclusion of a mixed cohort of untreated and treated patients, small sample size of patients with WCH, specific ethnic group, and relatively low cardiovascular risk) may be open to criticism, there is no question that the data from the Jackson Heart Study confirm that when WCH is defined according to normal daytime, nighttime and 24‐hour BPs, the level of cardiac organ damage is low and does not differ from that of a normotensive counterpart.
These results support the view that the most accurate definition of WCH requires setting thresholds simultaneously to 24‐hour, daytime, and nighttime BP, because this allows identification of truly low‐risk patients with WCH. This more precise classification does not exclude that patients may have a cardiovascular risk that is in the intermediate position between normotension and sustained hypertension and does not exclude that they deserve proper attention. Using other definitions of WCH, which do not include BP during night sleep, may have different impacts and consequences on screening and treatment of hypertension, including delaying treatment or inappropriately managing patients who have sustained hypertension.
CONFLICT OF INTEREST
The author has no conflicts of interest to disclose.
REFERENCES
- 1. Abolbashari M. White coat hypertension and cardiovascular diseases: innocent or guilty. Curr Cardiol Rep. 2018;20 (4):25. [DOI] [PubMed] [Google Scholar]
- 2. Briasoulis A, Androulakis E, Palla M, Papageorgiou N, Tousoulis D. White‐coat hypertension and cardiovascular events: a meta‐analysis. J Hypertens. 2016;34 (4):593‐599. [DOI] [PubMed] [Google Scholar]
- 3. Huang Y, Huang W, Mai W, et al. White‐coat hypertension is a risk factor for cardiovascular diseases and total mortality. J Hypertens. 2017;35(4):677‐688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. O'Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31(9):1731‐1768. [DOI] [PubMed] [Google Scholar]
- 5. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13‐e115. [DOI] [PubMed] [Google Scholar]
- 6. Nerenberg KA, Zarnke KB, Leung AA, et al. Hypertension Canada's 2018 Guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34(5):506‐525. [DOI] [PubMed] [Google Scholar]
- 7. National Clinical Guideline Centre (UK) . Hypertension: The Clinical Management of Primary Hypertension in Adults: Update of Clinical Guidelines 18 and 34 [Internet]. London: Royal College of Physicians (UK); 2011. http://www.ncbi.nlm.nih.gov/books/NBK83274/. Accessed June 15, 2018. [PubMed] [Google Scholar]
- 8. Task Force of the Latin American Society of Hypertension . Guidelines on the management of arterial hypertension and related comorbidities in Latin America. J Hypertens. 2017;35(8):1529‐1545. [DOI] [PubMed] [Google Scholar]
- 9. Head GA, McGrath BP, Mihailidou AS, et al. Ambulatory blood pressure monitoring in Australia: 2011 consensus position statement. J Hypertens. 2012;30(2):253‐266. [DOI] [PubMed] [Google Scholar]
- 10. Shimamoto K, Ando K, Fujita T, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37(4):253‐390. [DOI] [PubMed] [Google Scholar]
- 11. Anstey DE, Colantonio LD, Yano Y, Booth JN, Muntner P. The importance of using 24‐hour and nighttime blood pressure for the identification of white coat hypertension: data from the Jackson Heart Study. J Clin Hypertens. 2018. 10.1111/jch.13330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. de la Sierra A, Vinyoles E, Banegas JR, et al. Prevalence and clinical characteristics of white‐coat hypertension based on different definition criteria in untreated and treated patients. J Hypertens. 2017;35(12):2388‐2394. [DOI] [PubMed] [Google Scholar]
- 13. Asayama K, Thijs L, Li Y, et al. Setting thresholds to varying blood pressure monitoring intervals differentially affects risk estimates associated with white‐coat and masked hypertension in the population. Hypertension. 2014;64(5):935‐942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thomas SJ, Booth JN 3rd, Bromfield SG, et al. Clinic and ambulatory blood pressure in a population‐based sample of African Americans: the Jackson Heart Study. J Am Soc Hypertens 2017;11(4):204‐212.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stergiou GS, Asayama K, Thijs L, et al. Prognosis of white‐coat and masked hypertension: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertension. 2014;63(4):675‐682. [DOI] [PubMed] [Google Scholar]
- 16. Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship between clinic and ambulatory blood‐pressure measurements and mortality. N Engl J Med. 2018;378(16):1509‐1520. [DOI] [PubMed] [Google Scholar]
- 17. Cuspidi C, Rescaldani M, Tadic M, Sala C, Grassi G, Mancia G. White‐coat hypertension, as defined by ambulatory blood pressure monitoring, and subclinical cardiac organ damage: a meta‐analysis. J Hypertens. 2015;33(1):24‐32. [DOI] [PubMed] [Google Scholar]


