Abstract
Population assessment of effective blood pressure (BP) control is fundamental for reducing the global burden of hypertension, especially in low‐ and middle‐income countries. The authors evaluated the effectiveness of BP control and determined independent predictors associated with effective control among patients with hypertension on drug treatment in a large cross‐sectional study performed in two metropolitan areas in Brazil's southeast region. A total of 43 647 patients taking antihypertensive treatment were identified. Less than half of the patients (40.9%) had controlled BP (systolic BP <140 mm Hg and diastolic BP <90 mm Hg). Independent predictors of BP control were age, eating fruit daily, physical activity, previous cardiovascular disease, male sex, diabetes mellitus, ethnicity, and obesity. Simple variables associated with BP control may be utilized for knowledge translation strategies aiming to reduce the burden of hypertension.
Keywords: cardiovascular disease, hypertension, observational study, primary prevention, risk factors
1. INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of mortality worldwide.1 About 80% of the global burden of CVD death occurs in low‐ and middle‐income countries.2 Therefore, primary and secondary CVD prevention is of increasing priority for these countries.
Primary risk factors for a first cardiovascular event include age, sex, tobacco use, arterial hypertension, dyslipidemia, diabetes mellitus, obesity, and physical inactivity.3 Hypertension is one of the leading preventable causes of cardiovascular morbidity and mortality.1 Despite the availability of effective antihypertensive treatment and guidelines, there are large asymmetries in both detection and control of hypertension across the world.4
The prevalence of uncontrolled hypertension varies between countries. In the United States, data from the National Health and Nutrition Examination Survey (NHANES) 2003–2010 indicated that 53.5% of individuals did not have controlled blood pressure (BP) at the 140/90 mm Hg threshold.5 In Europe, data from the EURIKA (European Study on Cardiovascular Risk Prevention and Management in Daily Practice) showed that 51.6% of the general population had uncontrolled hypertension.6 Brazil's population is about 206 million people, 84% of whom live in urban areas.7 National data estimate that the prevalence of referred hypertension is 22.7% among Brazilian adults,8 indicating that there are approximately 36 million people with hypertension who are aware of their condition. In addition, data from the PURE (Prospective Ural Rural Epidemiology) study estimated the prevalence of hypertension to be about 40% of the Brazilian population aged 30 to 70 years.4 Although epidemiological studies have been published, predictors of BP control among patients with hypertension who have access to Brazilian public health care are poorly understood.
The aim of the current analysis was to evaluate BP control rates and to identify independent predictors associated with effective BP control among patients with hypertension under pharmacological therapy.
2. METHODS
2.1. Study design and participants
The First Cardiovascular Risk Assessment Sao Paulo and Campinas was a large cross‐sectional study performed in two metropolitan areas in Brazil's southeast region (Figure 1). The metropolitan areas of Sao Paulo and Campinas are among the most developed in the country, with a degree of urbanization of 99.0% and 97.4%, and a Human Development Index of 0.794 and 0.792 (national average of 0.727), respectively.9 Data collection was performed over 3 weeks in July 2009 at 500 public primary care units. The initiative was supported locally by the Cardiology Society of Sao Paulo, Health Secretary of the cities of Sao Paulo and Campinas, and Sao Paulo State Health Secretary, enabling data collection in almost all primary healthcare units of both cities. The study protocol was approved by the appropriate clinical research ethics committee (Institute Dante Pazzanese of Cardiology, protocol No. 4639).
Figure 1.

Geographic regions represented in this study: metropolitan regions of Sao Paulo and Campinas
For practical reasons, a nonprobabilistic selection of sites and participants was used. The goal was not to sample strictly proportionally, but instead to assure socioeconomic diversity and include all subregions in Sao Paulo and Campinas that utilize the primary public healthcare system (Supporting Information: Maps of Socioeconomic Diversity by the Human Development Index in the metropolitan regions of Sao Paulo and Campinas). Units in which it was possible to collect large quantities of data at a low cost were chosen. Included participants were consecutively selected from the general population living near primary healthcare units. In the present analysis, we included only patients 18 years and older, with a previous diagnosis of hypertension (by a physician), who were receiving antihypertensive medication for at least 4 weeks and had available BP measurement data (n = 43 647) (Figure 2).
Figure 2.
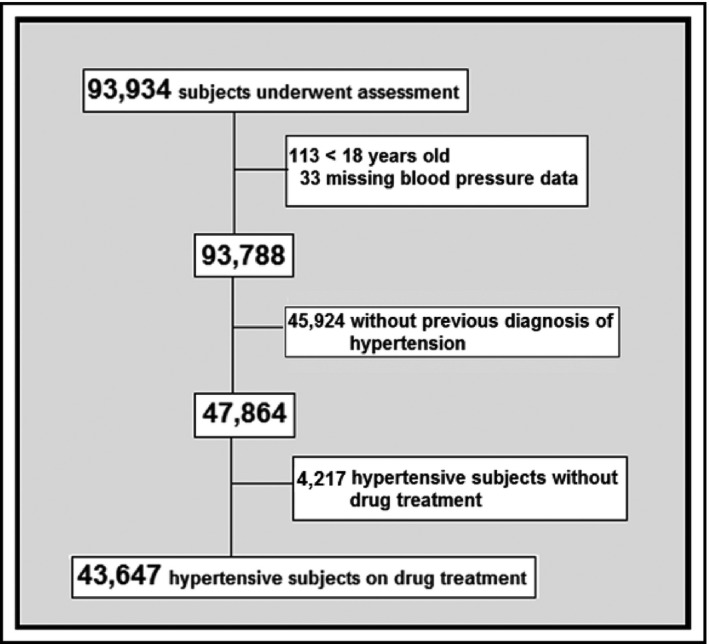
Enrollment of patients
2.2. Assessment of CVD risk factors
Demographics and further key information were obtained from patient interviews. All physicians, nurses, and healthcare workers were trained through a customized video on how to apply the electronic case report form and BP measurement.
BP was measured by either physicians, nurses, or healthcare workers trained according to the most recent Brazilian Cardiology Society recommendation.10 All participants had their systolic BP (SBP)/diastolic BP (DBP) measured in a sitting position after at least 5 minutes of rest. BP measurements were performed using conventional sphygmomanometers or validated automated devices, with appropriately sized cuffs. A single BP measurement was performed, and this was used for the analysis. Ethnicity was assessed as self‐declared white, black (African‐Brazilian), mixed race (combined European, native, and African ancestry), Asian‐Brazilian, or indigenous (Indigenous‐Brazilian). In these analyses, prevalent diabetes mellitus was defined on the basis of self‐reported medication use for glycemic control.11, 12, 13 Body mass index was calculated (kg/m2). Smokers were defined as individuals who had smoked tobacco in the previous 12 months; former smokers were those who had stopped smoking for over a year. Previous CVD was defined on the basis of self‐reported medical diagnosis and was considered if individuals self‐reported any history of myocardial infarction, stenting, angioplasty, coronary artery bypass graft, or nontraumatic lower limb amputation.11, 12, 13 Individuals were considered physically active if they were regularly involved in moderate physical activity for at least 180 minutes per week.13 Fruit and vegetable intake was assessed by self‐reported daily intake of at least one portion of each.13
2.3. Hypertension definition and control
For this analysis, patients with hypertension were defined as having had a previous diagnosis of hypertension by a physician and being on antihypertensive medication. Although several guidelines are available,10, 14, 15, 16, 17 controlled BP was defined as <140/90 mm Hg. An analysis was also performed according to the 2014 Evidence‐Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8), considering controlled hypertension in adults older than 60 years, with a target BP of <150 × 90 mm Hg and a target DBP of <90 mm Hg among patients younger than 60 years.16
2.4. Statistical analysis
Data are presented as mean and standard deviation (SD) for continuous variables, and as frequency and percentage for categorical variables. Intergroup comparison (controlled vs uncontrolled BP) was performed using Student t test for normally distributed continuous variables, Mann‐Whitney U test for continuous variables without normal distribution, and chi‐square or Fisher exact test for categorical variables. Factors associated with controlled hypertension were assessed using univariate and subsequently multivariate logistic regression models. Only variables statistically significantly associated (P < .05) were included in the final multivariate model. An association study was performed in the overall population of patients with hypertension (n = 43 647), and another was conducted after dividing participants into two groups by sex: men (n = 13 456) and women (n = 30 191). Statistical analyses were performed using SPSS version 19 (IBM).
3. RESULTS
Of the 93 934 participants in the First Cardiovascular Risk Assessment Sao Paulo and Campinas trial, 43 647 patients were included in the current study. These patients were 18 years or older, had a previous diagnosis of hypertension, and were on antihypertensive drugs. Mean participant age was 58.6 years, 30.8% were men, 24.8% had diabetes mellitus, 11.8% were current smokers, and 35.2% had a history of CVD (Table 1).
Table 1.
Patient characteristics and hypertension status of 43 647 patients with hypertension on treatment
| Total (N=43 647) | Controlled(n=17 835) | Uncontrolled(N=25 812) | |
|---|---|---|---|
| Age, mean (SD), y | 58.6 (10.5) | 58.2 (10.6) | 58.9 (10.5) |
| ≥60 y, % | 48.1 | 46.4 | 49.3 |
| Men, % | 30.8 | 26.5 | 33.8 |
| Declared ethnicity, % | |||
| White | 54.2 | 55.2 | 53.4 |
| Mixed | 31.0 | 30.4 | 31.3 |
| Black | 12.1 | 11.5 | 12.5 |
| Other | 2.7 | 2.9 | 2.8 |
| SBP, mean (SD), mm Hg | 136.7 (20.1) | 119.8 (9.3) | 148.3 (17.2) |
| DBP, mean (SD), mm Hg | 84.9 (12.2) | 75.5 (6.5) | 91.3 (11.1) |
| BMI, mean (SD), kg/m2 | 29.5 (5.5) | 28.9 (5.2) | 29.9 (5.7) |
| BMI ≥30, % | 40.9 | 37.0 | 43.6 |
| Smoking status, % | |||
| Never | 64.3 | 64.6 | 64.2 |
| Current | 11.8 | 11.6 | 11.9 |
| Former | 23.9 | 23.8 | 23.9 |
| Diabetes mellitus, % | 24.8 | 22.3 | 26.5 |
| Previous CVD,a% | 35.2 | 36.5 | 30.1 |
| Moderate physical activity,b% | 31.5 | 33.6 | 30.1 |
| Daily fruit intake, % | 59.9 | 61.2 | 59.0 |
| Daily vegetable intake, % | 64.7 | 65.2 | 64.3 |
Abbreviations: BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure; SD, standard deviation.
Previous cardiovascular disease (CVD): previous myocardial infarction, stroke, coronary artery bypass surgery, coronary angioplasty.
Moderate physical activity: at least 180 minutes per week.
3.1. Control rate
In the primary analysis, it was observed that 17 835 (40.9%) had controlled BP levels, with a target SBP of <140 mm Hg and a DBP of <90 mm Hg. The mean SBP was 119.8 mm Hg (SD = 9.3) in the controlled group and 148.3 mm Hg (SD = 17.2) in the uncontrolled group. The mean DBP was 75.5 mm Hg (SD = 6.5) in the controlled group and 91.3 mm Hg (SD = 11.0) in the uncontrolled group.
Among 25 812 patients with hypertension on treatment but without BP control, it was observed that 42.5% had SBP of ≥160 mm Hg and/or DBP of ≥100 mm Hg. Considering the BP targets according to JNC 8,16 20 732 (47.5%) patients with hypertension on treatment had controlled BP.
3.2. Predictors of hypertension control
To investigate factors associated with controlled hypertension, an initial univariate analysis was performed to compare patients with and without controlled hypertension who were receiving antihypertensive medication. Smoking status (odds ratio [OR], 1.03; 95% confidence interval [CI], 0.97–1.10) and eating vegetables daily (OR, 1.04; 95% CI, 1.00–1.08) were not significantly associated with controlled hypertension (Table 2).
Table 2.
Predictors of blood pressure control in 43 647 patients with hypertension on treatment—univariate analysis
| OR | 95% CI | P value | |
|---|---|---|---|
| Men | 0.71 | 0.68–0.74 | <.001 |
| Age <60 y | 1.13 | 1.08–1.17 | <.001 |
| Ethnicitya | |||
| Mixed | 0.94 | 0.90–0.98 | <.001 |
| Black | 0.89 | 0.83–0.94 | <.001 |
| Others | 1.02 | 0.90–1.15 | .163 |
| Obesityb | 0.76 | 0.73–0.79 | <.001 |
| Diabetes mellitus | 0.79 | 0.76–0.83 | <.001 |
| Previous CVDc | 1.10 | 1.05–1.14 | <.001 |
| Current smokerd | 1.03 | 0.97–1.10 | .082 |
| Moderate physical activitye | 1.17 | 1.13–1.22 | <.001 |
| Daily fruit intake | 1.10 | 1.05–1.14 | <.001 |
| Daily vegetable intake | 1.04 | 1.00–1.08 | .059 |
Abbreviations: BP, blood pressure; CI, confidence interval; OR, odds ratio.
Compared with white ethnicity.
Obesity: body mass index (BMI) ≥30 (reference group BMI <30).
Previous cardiovascular disease (CVD): previous myocardial infarction, stroke, coronary artery bypass surgery, coronary angioplasty.
Current smoker: reference group never smoker.
Moderate physical activity: at least 180 minutes per week.
In the multivariate analysis considering all participants, being younger than 60 years, having a history of CVD, eating fruit daily, and moderate‐intensity physical activity were significantly positively associated with controlled BP (Table 3). Male sex, obesity, black or mixed race ethnicity (white ethnicity as reference), and diabetes mellitus were negatively associated with hypertension control (Table 3).
Table 3.
Independent predictors of BP control in 43 647 patients with hypertension on treatment—multivariate analysis
| OR | 95% CI | P value | |
|---|---|---|---|
| Men | 0.68 | 0.66–0.72 | <.001 |
| Age <60 y | 1.14 | 1.09–1.18 | <.001 |
| Declared ethnicitya | |||
| Mixed | 0.92 | 0.87–0.97 | <.001 |
| Black | 0.88 | 0.83–0.94 | <.001 |
| Obesityb | 0.73 | 0.70–0.76 | <.001 |
| Diabetes mellitus | 0.83 | 0.80–0.87 | <.001 |
| Previous CVDc | 1.09 | 1.04–1.13 | <.001 |
| Moderate physical activityd | 1.18 | 1.13–1.23 | <.001 |
| Daily fruit intake | 1.05 | 1.01–1.10 | .01 |
Abbreviations: BP, blood pressure; CI, confidence interval; OR, odds ratio.
Compared with white ethnicity.
Obesity: body mass index (BMI) ≥30 (reference group BMI <30).
Previous cardiovascular disease (CVD): previous myocardial infarction, stroke, coronary artery bypass surgery, coronary angioplasty.
Moderate physical activity: at least 180 minutes per week.
3.3. Predictors of hypertension control by sex
Among the 30 191 women with hypertension undergoing drug treatment, smoking status (OR, 1.06; 95% CI, 0.99–1.13), previous CVD (OR, 1.04; 95% CI, 0.99–1.10), and eating vegetables daily (OR, 0.99; 95% CI, 0.94–1.04) were not significantly associated with controlled hypertension in the univariate analysis (Table 4).
Table 4.
Predictors of BP control among 30 191 women with hypertension on drug treatment—univariate and multivariate analysis
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age <60 y | 1.17 | 1.12–1.22 | <0.001 | 1.19 | 1.14–1.25 | <0.001 |
| Declared ethnicitya | ||||||
| Mixed | 0.93 | 0.88–0.98 | 0.005 | 0.91 | 0.87–0.96 | 0.001 |
| Black | 0.88 | 0.82–0.95 | <0.001 | 0.89 | 0.83–0.96 | 0.001 |
| Obesityb | 0.73 | 0.70–0.77 | <0.001 | 0.74 | 0.71–0.78 | <0.001 |
| Current smokerc | 1.06 | 0.99–1.13 | 0.135 | ‐ | ‐ | ‐ |
| Diabetes mellitus | 0.77 | 0.73–0.81 | <0.001 | 0.81 | 0.77–0.86 | <0.001 |
| Previous CVDd | 1.04 | 0.99–1.10 | 0.068 | ‐ | ‐ | ‐ |
| Moderate physical activitye | 1.20 | 1.14–1.26 | <0.001 | 1.21 | 1.15–1.27 | <0.001 |
| Daily fruit intake | 1.06 | 1.01–1.11 | 0.017 | 0.97 | 0.93–1.02 | 0.28 |
| Daily vegetable intake | 0.99 | 0.94–1.04 | 0.756 | ‐ | ‐ | ‐ |
Abbreviations: BP, blood pressure; CI, confidence interval; OR, odds ratio.
Compared with white ethnicity.
Obesity: body mass index (BMI) ≥30 (reference group BMI <30).
Current smoker: reference group never smoker.
Previous cardiovascular disease (CVD): previous myocardial infarction, stroke, coronary artery bypass surgery, coronary angioplasty.
Moderate physical activity: at least 180 minutes per week.
In the multivariate analysis, women aged younger than 60 years and moderate‐intensity physical activity were statistically significantly positively associated with controlled BP (Table 4). Obesity, black or mixed race ethnicity (white ethnicity as reference), and diabetes mellitus were negatively associated with hypertension control.
Different from findings among the female group, even without a statistically significant difference, fewer men younger than 60 years had BP control than those older than 60 years (34.6% vs 35.7%, respectively). Smoking status (OR, 0.96; 95% CI, 0.86–1.07), eating fruit daily (OR, 1.06; 95% CI, 0.99–1.14), and eating vegetables daily (OR, 1.03; 95% CI, 0.96–1.11) were not significantly associated with controlled hypertension in the male population (Table 5).
Table 5.
Predictors of BP control among 13 456 men with hypertension on treatment—univariate and multivariate analysis
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age <60 y | 0.95 | 0.89–1.02 | 0.192 | ‐ | ‐ | ‐ |
| Declared ethnicitya | ||||||
| Mixed | 0.94 | 0.87–1.02 | 0.160 | ‐ | ‐ | ‐ |
| Black | 0.87 | 0.78–0.99 | 0.026 | 0.87 | 0.75–0.98 | .019 |
| Obesityb | 0.70 | 0.65–0.76 | <0.001 | 0.71 | 0.66–0.77 | <.001 |
| Current smokerc | 0.96 | 0.86–1.07 | 0.199 | ‐ | ‐ | ‐ |
| Diabetes mellitus | 0.89 | 0.82–0.96 | 0.003 | 0.89 | 0.82–0.97 | .010 |
| Previous CVDd | 1.18 | 1.10–1.28 | <0.001 | 1.19 | 1.10–1.28 | <.001 |
| Moderate physical activitye | 1.17 | 1.09–1.27 | <0.001 | 1.16 | 1.07–1.24 | <.001 |
| Daily fruit intake | 1.06 | 0.99–1.14 | 0.096 | ‐ | ‐ | ‐ |
| Daily vegetable intake | 1.03 | 0.96–1.11 | 0.391 | ‐ | ‐ | ‐ |
Abbreviations: BP, blood pressure; CI, confidence interval; OR, odds ratio.
Compared with white ethnicity.
Obesity: body mass index (BMI) ≥30 (reference group BMI <30).
Current smoker: reference group never smoker.
Previous cardiovascular disease (CVD): previous myocardial infarction, stroke, coronary artery bypass surgery, coronary angioplasty.
Moderate physical activity: at least 180 minutes per week.
In the multivariate analysis, among the male group, previous CVD and moderate‐intensity physical activity were significantly positively associated with controlled BP (Table 5). Obesity, black ethnicity (white ethnicity as reference), and diabetes mellitus were negatively associated with hypertension control (Table 5).
4. DISCUSSION
This study included 43 647 patients with hypertension under drug treatment followed at primary healthcare units in the cities of Sao Paulo and Campinas in Brazil. Less than half of the patients with treated hypertension had controlled BP. Epidemiological studies on BP control rates in Brazil, either by city or region, showed rates ranging from 10% to 57.6%.18
The control rate in this study was higher than that found by Muxfeldt and colleagues,19 which analyzed BP control in 1699 patients with hypertension at a tertiary hospital in Rio de Janeiro, where only 27% of patients had BP <140 × 90 mm Hg. This difference can be partly explained by the fact that tertiary hospital clinics are referral centers for patients who are more resistant to hypertension control. Piccini and associates20 interviewed 12 324 participants in a population‐based epidemiological study from 100 municipalities and identified 2004 (16.3%) patients with hypertension. Of these, 57.6% had controlled BP. The differences in the control rate found among these studies may be due to the fact that the latter only included patients between the ages of 20 and 59 years. Persons older than 60 years were excluded, and this age category is associated with BP that is more difficult to achieve effective control, especially among women. Nobre and colleagues21 included 2810 patients with hypertension in the private Brazilian healthcare system from 291 different centers in four regions across the country. The study found a BP control rate of 53.3%.21 This rate was higher than that found in the public health system, suggesting that access and affordability of hypertension treatment along with better education and socioeconomic status might explain this finding.
A control rate of 46.5% was found in the NHANES 2003–2010 population in the United States. However, this rate refers to the percentage of patients with hypertension who have BP <140 × 90 mm Hg of all patients diagnosed with hypertension, including those who were unaware or were not using antihypertensive drug therapy. When only the hypertension control rate in those using antihypertensive drug treatment is considered, NHANES had a higher control rate than that of the current study, with 66% of treated patients with controlled BP.5 A European study showed a similar control rate to that found in the current study but it was still higher than the rate we found. Of the 5220 patients with hypertension under treatment in the EURIKA study, 48.4% had controlled BP.6
The low rate of BP control found in the Sao Paulo and Campinas populations is a major public health problem, since there is a confirmed clear association between hypertension and CVD, in addition to a high prevalence of hypertension in the general population. Over 40% of patients with hypertension who had uncontrolled BP showed BP levels of ≥160 × 100 mm Hg. This observation is even more alarming in light of the recent results of SPRINT (Systolic Blood Pressure Intervention Trial), which showed that targeting an SBP of 120 mm Hg showed better results in reduction of clinically relevant outcomes than the SBP goal of 140 mm Hg in high‐risk patients without diabetes mellitus.22
In our primary analysis of the entire population (n = 43 647), eight predictors associated with BP control were identified in multivariate analysis and three of these are considered modifiable. Age younger than 60 years, history of CVD, daily intake of fruit, and regular physical activity were independent factors associated with a higher odds of BP control (SBP <140 mm Hg and DBP <90 mm Hg). Male sex, black or mixed ethnicity, having diabetes mellitus, and obesity were associated with uncontrolled BP.
Older age (>60 years) and obesity are two factors that are consolidated in the literature as predictors of reduced BP control.6, 23, 24, 25, 26 However, when the association analysis was performed according to sex, it was observed that only younger age in women (<60 years) was associated with better BP control. In contrast, in men, there was a lower percentage of younger patients with controlled BP, although this difference was not statistically significant. This finding is compatible with that found by Daugherty and colleagues.27 These researchers identified that the difference between BP control rates between men and women depended on the age group analyzed. The lowest rates of control were identified in older women and younger men.27
The question of sex as a predictor of BP control is controversial. Studies have shown conflicting results, identifying male sex as a predictor of better or worse control, or not even as a statistically significant predictor. Cushman and colleagues23 analyzed data from 33 357 patients with hypertension who participated in ALLHAT (Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial), and found that male sex was associated with a 10% (OR, 1.10; 95% CI, 1.03–1.18 [P < .05]) higher odds of having controlled BP in the third year of follow‐up compared with women. This finding was confirmed by Borghi and colleagues,6 who evaluated predictors of poor BP control in 2691 patients with hypertension in the EURIKA study. Ong and colleagues28 analyzed data from 3475 treated participants with hypertension in NHANES 1999–2004 and concluded that despite the prevalence of uncontrolled hypertension being higher among women (55.9% vs 50.8%), this difference was not statistically significant (P = .06). In our study, the multivariate analysis showed that men had 32% lower odds of having controlled BP. This finding aligns with those of other studies.24, 26, 29, 30 As a variable, sex is intrinsically associated with other behavior (eg, increased demand for health care, differing rates of adherence to treatment, and alcohol consumption) and factors (eg, abdominal obesity, metabolic syndrome) that could be associated with BP control. These variables were not uniformly analyzed in all studies and may explain these contradictory results.
The association between hypertension and diabetes mellitus is known to increase cardiovascular risk, requiring more intensive BP control. However, it was observed that among patients with diabetes mellitus and hypertension included in our study, about one third had BP <140 × 90 mm Hg. The association of diabetes mellitus and poor BP control was also identified in the ALLHAT population.23
This study identifies three important modifiable factors associated with BP control: obesity, regular moderate physical activity, and daily consumption of fruit. Patients with hypertension who performed moderate‐intensity physical activity were 18% more likely to have controlled BP compared with those categorized as sedentary. Although already established in the literature in a clinical trial scenario,31 to the best of our knowledge, this was the first epidemiological study to demonstrate an independent association between regular engagement in physical activity and BP control. Similarly, there are few epidemiological studies where fruit intake was evaluated as an independent factor for BP control. Despite being the weakest independent association with BP control, when all participants were analyzed, it was observed that patients with hypertension who reported daily consumption of fruit were more likely to have controlled BP.
Despite tobacco being confirmed as a classic risk factor for CVD, no significant association was found between tobacco and BP control in our study. Similar results have been found in ALLHAT and in a Lebanese study.23, 24 Finally, history of CVD was associated with higher odds of having controlled BP, consistent with results from ALLHAT.23
5. LIMITATIONS AND STRENGTHS
This cross‐sectional study included the highest number of patients with hypertension under treatment in Brazil, with over 40 000 patients included. Three modifiable independent predictors of BP control were identified, which may be useful in guiding the implementation of efficient population knowledge translation strategies: obesity, sedentary lifestyle, and eating habits. Nevertheless, some study limitations should be considered. Our study was performed in two of the most developed metropolitan areas of Brazil, with a level of urbanization of more than 95%. Thus, it was not representative of rural areas, nor representative of the whole country, especially in regions with less social development, where access to the healthcare system is challenging. We did not evaluate some predictors that may be associated with BP control rates, such as alcohol consumption, adherence to medication, sodium intake, educational level, and economic status. We also have no information on the amount or number of antihypertensive drugs used by patients. The study was also limited by the fact that only one BP measurement was taken. Handler and colleagues32 concluded that the results of NHANES 1999–2008 supported the fact that in patients with and those without hypertension who had a normal BP value on the first BP measurement, a single measurement is appropriate because <10% of patients would be reclassified as having prehypertension and <0.5% as having hypertension. However, at least 18.2% of those with above‐normal initial BP are often reclassified to lower categories and require a second measurement.32
6. CONCLUSIONS
Fewer than half of the patients with hypertension in our study had controlled BP levels. Considering all patients with hypertension under drug treatment, three modifiable factors (regular moderate exercise, obesity, and fruit intake) were independently associated with BP control. This finding should be utilized to build nationwide knowledge translation strategies to improve BP control and to reduce the burden of hypertension.
CONFLICT OF INTEREST
All authors report no specific funding in relation to this research and have no conflicts of interest to disclose.
Supporting information
Costa Filho FF, Timerman A, Saraiva JFK, et al. Independent predictors of effective blood pressure control in patients with hypertension on drug treatment in Brazil. J Clin Hypertens. 2018;20:125–132. 10.1111/jch.13139
REFERENCES
- 1. GBD 2015 Mortality and Causes of Death Collaborators . Global, regional, and national life expectancy, all‐cause mortality, and cause‐specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459‐1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chockalingam A, Balaguer‐Vintro I, Achutti A, et al. Impending global pandemic of cardiovascular diseases: challenges and opportunities for the prevention and control of cardiovascular diseases in developing countries and economies in transition (World Heart Federation). Can J Cardiol. 2000;16:227‐229. [PubMed] [Google Scholar]
- 3. Perk J, De Backer G, Gohlke H, et al. European guidelines on cardiovascular disease prevention in clinical practice (version 2012): the fifth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33:1635‐1701. [DOI] [PubMed] [Google Scholar]
- 4. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high‐, middle‐, and low‐income countries. JAMA. 2013;310:959‐968. [DOI] [PubMed] [Google Scholar]
- 5. US Centers for Disease Control and Prevention . Vital signs: awareness and treatment of uncontrolled hypertension among adults—United States, 2003–2010. MMWR Morb Mortal Wkly Rep. 2012;61:703‐709. [PubMed] [Google Scholar]
- 6. Borghi C, Tubachb F, De Backer G, et al. Lack of control of hypertension in primary cardiovascular disease prevention in Europe: results from the EURIKA study. Int J Cardiol. 2016;218:83‐88. [DOI] [PubMed] [Google Scholar]
- 7. Instituto Brasileiro de Geografia e Estatística – IBGE . Projeções e estimativas da população do Brasil e das Unidades da Federação [on‐line]. http://www.ibge.gov.br/apps/populacao/projecao/index.html. Accessed February 26, 2017.
- 8. Andrade SS, Malta DC, Iser BM, Sampaio PC, de Moura L. Prevalence of self‐reported arterial hypertension in Brazilian capitals in 2011 and analysis of its trends in the period between 2006 and 2011. Rev Bras Epidemiol. 2014;17(suppl 1):215‐226. [DOI] [PubMed] [Google Scholar]
- 9. Human development atlas in the Brazilian metropolitan regions. Brasilia: United Nations Development Programme (UNDP), IPEA, FJP; 2014.
- 10. Sociedade Brasileira de Cardiologia/Sociedade Brasileira de Hipertensão/Sociedade Brasileira de Nefrologia . VI Brazilian guidelines on hypertension. Arq Bras Cardiol. 2010;95(suppl 1):1‐51. [PubMed] [Google Scholar]
- 11. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159‐174. [PubMed] [Google Scholar]
- 12. Oksanen T, Kivimäki M, Pentti J, Virtanen M, Klaukka T, Vahtera J. Self‐report as an indicator of incident disease. Ann Epidemiol. 2010;20:547‐554. [DOI] [PubMed] [Google Scholar]
- 13. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet. 2004;364:937‐952. [DOI] [PubMed] [Google Scholar]
- 14. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560‐2572. [DOI] [PubMed] [Google Scholar]
- 15. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. J Hypertens. 2013;31:1281‐1357. [DOI] [PubMed] [Google Scholar]
- 16. James PA, Oparil S, Carter BL, et al. 2014 Evidence‐based guideline for the management of high blood pressure in adults report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507‐520. [DOI] [PubMed] [Google Scholar]
- 17. Malachias MV, Souza WK, Plavnik FL, et al. 7th Brazilian guideline of arterial hypertension. Arq Bras Cardiol. 2016;107(suppl 3):1‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pinho NA, Pierin AM. Hypertension control in Brazilian publications. Arq Bras Cardiol. 2013;101:e65‐e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Muxfeldt ES, Nogueira AR, Salles GF, Bloch KV. Demographic and clinical characteristics of hypertensive patients in the internal medicine outpatient clinic of a university hospital in Rio de Janeiro. Sao Paulo Med J. 2004;122:87‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Piccini RX, Facchini LA, Tomasi E, et al. Promotion, prevention and arterial hypertension care in Brazil. Rev Saude Publica. 2012;46:543‐550. [DOI] [PubMed] [Google Scholar]
- 21. Nobre F, Ribeiro AB, Mion D Jr. Control of arterial pressure in patients undergoing anti‐hypertensive treatment in Brazil: Controlar Brazil. Arq Bras Cardiol. 2010;94:663‐670. [DOI] [PubMed] [Google Scholar]
- 22. The SPRINT Research Group . A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103‐2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4:393‐404. [DOI] [PubMed] [Google Scholar]
- 24. Farah R, Zeidan RK, Chahine MN, et al. Predictors of uncontrolled blood pressure in treated hypertensive individuals: first population‐based study in Lebanon. J Clin Hypertens (Greenwich). 2016;18:871‐877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kanungo S, Mahapatra T, Bhowmik K, et al. Patterns and predictors of undiagnosed and uncontrolled hypertension: observations from a poor‐resource setting. J Hum Hypertens. 2017;31:56‐65. [DOI] [PubMed] [Google Scholar]
- 26. Girerd X, Hanon O, Pannier B, Mourad JJ, Vaïsse B. Determinants of controlled hypertension in patients treated with antihypertensive drugs in France: the French League Against Hypertension Survey (FLAHS 2015). Ann Cardiol Angeiol (Paris). 2016;65:219‐222. [DOI] [PubMed] [Google Scholar]
- 27. Daugherty SL, Masoudi FA, Ellis JL, et al. Age dependent gender differences in hypertension management. J Hypertens. 2011;29:1005‐1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ong KL, Tso AW, Lam KS, Cheung BM. Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension. 2008;51:1142‐1148. [DOI] [PubMed] [Google Scholar]
- 29. Sarganas G, Neuhauser HK. The persisting gender gap in hypertension management and control in Germany: 1998 and 2008–2011. Hypertens Res. 2016;39:457‐466. [DOI] [PubMed] [Google Scholar]
- 30. Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479‐486. [DOI] [PubMed] [Google Scholar]
- 31. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta‐analysis. J Am Heart Assoc. 2013;2:e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Handler J, Zhao Y, Egan BM. Impact of the number of blood pressure measurements on blood pressure classification in US adults: NHANES 1999–2008. J Clin Hypertens (Greenwich). 2012;14:751‐759. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


