Abstract
Antihypertensive drug adherence (ADA) is a mainstay in blood pressure control. Education through mobile phone short message system (SMS) text messaging could improve ADA. The authors conducted a randomized study involving 314 patients with hypertension with <6 months of antihypertensive treatment from the Preventive Health Program of 12 different primary care centers in Santiago, Chile. Patients were randomly assigned to receive or not receive SMS related to ADA and healthy lifestyle. Adherence was assessed by the self‐reported four‐item scale Morisky‐Green‐Levine questionnaire at baseline and after 6 months of follow‐up, with four of four positive questions classified as good adherence. Group comparison for adherence was performed by means of a logistic regression model, adjusting by baseline adherence, age older than 60 years, and sex. A total of 163 patients were randomized to receive and 151 to not receive SMS. After 6 months of follow‐up, ADA in the non‐SMS group decreased from 59.3% to 51.4% (P=.1). By contrast, adherence increased from 49% to 62.3% (P=.01) in the SMS group. Text messaging intervention improved ADA (risk ratio, 1.3; 95% confidence interval, 1.0–1.6 [P<.05]). At 6‐month follow‐up, text messaging resulted in an increase in reporting ADA in this hypertensive Latino population. This approach could become an effective tool to overcome poor medication adherence in the community.
Keywords: hypertension, medication adherence, patient compliance, text messaging
1. INTRODUCTION
Hypertension is a major public health problem worldwide. In 2010, hypertension was the leading risk factor responsible for approximately 9.4 million deaths across the globe. Moreover, recent data estimate that people with hypertension have a lifetime risk of overall cardiovascular disease at 30 years of age of 63% compared with 46% for those with normal blood pressure (BP).1, 2
According to data from the World Health Organization, the prevalence of global hypertension is approximately 40% and BP control rates are suboptimal, even in developed countries.3 A leading cause of poor BP control is the lack of adherence to antihypertensive drug therapy. Studies have shown that adherence rates to antihypertensive drugs ranged from 34% to 78% at 1 year.4 In Switzerland, a study with electronic monitoring has shown that about half of the patients who were prescribed an antihypertensive drug had stopped taking it within 1 year.5 Moreover, data from the United Kingdom have revealed a drug discontinuation rate of approximately 20% at 6 months among patients with newly diagnosed hypertension in general practice.6
Among the barriers to achieving good adherence, forgetfulness is a common factor reported by patients.7 Indeed, among patients with hypertension in the United States, it is the third most commonly reported barrier to adherence.8 Other barriers include lack of motivation to take pills and misunderstanding of the prescription.9 Thereby, as some studies have shown, a pivotal component of an adherence program is patient education and motivation.10 Therefore, strategies that remind patients about drug intake with the appropriate frequency, educate about medication, and also encourage behavioral change are attractive concepts for everyday clinical practice.
In Chile, the technology market has grown substantially in recent years. By 2010, statistics on cellular telephone usage reported 1.13 cellular phones per inhabitant.11 Therefore, the use of mobile phone short message service (SMS) text messaging could be an attractive and easy‐to‐use tool in modern medical practice. Text messaging can deliver simple and direct information and can be easily repeated to reinforce the information and potentially encourage behavioral changes in recipients.12 SMS technology has been used in several chronic diseases, such as supporting smoking cessation, obesity programs, and even risk factor modification, but there are limited data on its use in hypertensive populations.13, 14 In fact, in a recent meta‐analysis assessing the effect of SMS on medication adherence in chronic diseases, only one hypertension study was included.15
This study aimed to evaluate whether the effect of a mobile phone text messaging intervention vs no text messaging (control) improves self‐reported antihypertensive drug adherence in patients with hypertension recruited through primary care offices in Santiago, Chile.
2. METHODS
2.1. Eligibility and recruitment
This study was a prospective, multicenter, randomized, controlled study performed in patients with arterial hypertension treated in primary care clinics. Patients were recruited from 12 different primary care centers in Santiago, Chile, located in different geographic and socioeconomic areas. The primary outcome of the study was antihypertensive therapy adherence.
Patients included in the study were those: (1) with a confirmed medical diagnosis of arterial hypertension based on JNC 7 (Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure) criteria16; (2) who have been given their first antihypertensive medication prescription during the previous 1 to 6 months; (3) aged 30 to 80 years; and (4) who owned a mobile phone with access to SMS text messaging. Exclusion criteria included history of myocardial infarction, stroke, heart failure, and/or renal failure on dialysis, as well as inability to receive SMS text messages secondary to mental disabilities and/or patients who were unable to read.
During a period of 6 months, all patients who had been seen in the Preventive Health Program at the selected primary care centers and fulfilled the study criteria were invited to participate in the study by their primary care physicians (PCPs). If a patient declared no interest to participate, the patient was not incorporated in the list by the physician. Sequential listings of eligible patients with their phone numbers were delivered by the PCPs to the Chilean Society Foundation. Foundation staff phoned to invite the patient to a visit (baseline) at the medical center, calling sequentially by the list number. If the patient declared no interest in going to the visit, their name was deleted from the list. The selection procedure attempted to have no bias. It was a competitive enrollment. Study enrollment took place from October 2012 through August 2013, and the last study visit was conducted in January 2014. The baseline and follow‐up visits were conducted at primary care offices by members of the study team. The referring PCP was not present for those visits. Antihypertensive medications were provided to all patients free of cost by their respective primary care centers. Prescription modification was performed exclusively by their physicians, as hypertension control was not an outcome measured during this study.
At the baseline visit, after signing an informed consent, each patient completed a survey that collected demographics, cardiovascular risk factors, hypertensive medication(s), and dietary habits, as well as a health‐related quality‐of‐life questionnaire (EQ‐5D).17 Education level—an indicator of socioeconomic status in Chile—was ascertained by asking the years of formal education and the highest qualification received. Educational level was divided into three categories: primary education, defined as primary school or less (0–8 years); secondary education, defined as secondary school level (9–12 years); and high or superior education, defined as university or technical level (≥13 years). Antihypertensive medication adherence was measured using the validated Spanish version of the Morisky‐Green‐Levine (MGL) questionnaire.18, 19 Only patients who responded positively to the four questions were considered adherent. BP was measured with a validated electronic device (Omron HEM‐742, Omron Healthcare) using JNC 7 guidelines.16, 20 The inflation mechanism of the device was activated to perform three consecutive measurements with a 2‐minute interval between each.
2.2. Randomization
Patients were randomized to receive or not receive SMS text messages. Randomization was conducted by members of the study's coordinating center who were blinded to patient characteristics. All PCPs and the principal investigator were blinded to the intervention allocation. Patients were only seen at the baseline and 6‐month visits, thus they did not inform their physicians and nurses about whether they were receiving messages.
2.3. Text‐messaging
Text messages were developed by the principal investigator, the nurse‐study coordinator, a psychologist, and a cardiologist of the study's coordinating center using social‐cognitive theory data.21, 22 Text messages contained educational information about healthy diet, salt intake, antihypertensive medication schedule, and the importance of medication intake and adherence, among others. The main educational goal was to improve medication adherence through behavioral changes. Text messages were sent every 12±2 days during the 6‐month follow‐up period and limited to 160 characters (Table 1). All SMS were sent by an external agency, StepTherapy Chile (www.s-th.cl), a Chilean specialized agency focused on patient engagement programs. As part of this program, this agency made confirmation phone calls to ensure that the messages had been received every 4 weeks. No information was given except confirmation of SMS receipt.
Table 1.
List of mobile phone short message service text messages (translated into English) and the day the message was sent
| Content of message | Day | |
|---|---|---|
| 1 | Remember to take the medication prescribed by your doctor following the recommended dose and schedule. Do not stop any tablet! | 2 |
| 2 | Blood pressure drugs act through different mechanisms. If you suspend a tablet, you will lose the action and can raise blood pressure | 14 |
| 3 | If you have a medication prescribed at night, remember to take it! The drug′s effect lasts some hours and if you forget this dose, blood pressure can rise | 26 |
| 4 | Remember that salt raises blood pressure. Decrease your intake of high‐sodium products such as sausages, canned goods, and instant soups | 38 |
| 5 | Remember that your doctor knows your particular case and knows what you need to lower blood pressure. Take what you have been prescribed | 50 |
| 6 | How much blood pressure medicine do you have left? If you have only a few pills for this week, plan to obtain your medicine timely | 62 |
| 7 | Promptly take the medications your doctor prescribed, strictly following the schedule and doses indicated | 74 |
| 8 | If you feel that your blood pressure medicine causes you inconvenience, tell your doctor immediately for a change. Do not decide to change it by yourself | 86 |
| 9 | Do not stop treatment even if your blood pressure has returned to normal, or if you feel better, except on the advice of your doctor | 98 |
| 10 | Stress affects hypertension. Take space and moments of tranquility, and do not forget to take your medications at the time and dose indicated | 110 |
| 11 | If you forget to take the morning medicine, do so as soon as possible. To avoid forgetfulness, leave it near your toothbrush or your breakfast cup | 122 |
| 12 | If you must take medication during working hours, program your cell phone alarm to remind you when appropriate | 134 |
| 13 | Have you tried eating bread without salt? If you do not like it, at least try to get the salt shaker off the table. That′s already an improvement. | 146 |
| 14 | If this week you have taken all your medications at the correct time and dose, congratulations! | 158 |
| 15 | By controlling blood pressure, you add years to your life. Remember to take your medications to control it. We want to take care of you! | 170 |
2.4. Follow‐up
At the end of 6 months, patients were contacted for a final visit to complete a survey including dietary habits, antihypertensive therapy, and the MGL adherence questionnaire. BP was measured during this site visit. If a patient could not attend the final visit in person, blind staff conducted the survey over the phone. In this case, the BP could not be registered.
The protocol was approved by the regional ethics committee. All patients provided written informed consent prior to the first visit.
2.5. Sample size determination
Determination of sample size was done assuming an adherence rate of 50% at 6 months according to international data.5, 23 Sample size was calculated with unilateral test of two proportions to obtain a statistical power of 80% with a confidence level of 95% (1‐α) to detect a 15% difference between the effectiveness of the intervention (assuming an adherence rate of 55% in the control group, 70% in the intervention group, and a loss rate of 20%). The adjusted sample size was 160 patients per group.
2.6. Statistical analysis
Statistical analysis was performed using R software version 3.3.1.24 Values are presented as mean±SD for continuous variables and as percentages for discrete variables. Fisher exact test and McNemar test were used for categorical variables association. Group comparison for adherence at the end of the follow‐up period was performed by means of a logistic regression model, adjusted for baseline adherence, age older than 60 years, and sex, considering adherence at the second control as a dichotomous response. The effect of text messaging was assessed based on including an interaction term for treatment. Confidence intervals for adjusted risk ratios were calculated based on bootstrap replications.25, 26
3. RESULTS
Of the 605 patients with hypertension referred for recruitment, 314 were enrolled between October 2012 and August 2013. Patient disposition is illustrated in Figure 1. Of the study population, 64% were women, 67% had a primary or secondary educational level, and the mean age was 60±10 years. Table 2 provides baseline characteristics of the study population. Mean time on antihypertensive medication was 4±1 months, and mean drug pill number was 2.1 per day. The most frequently prescribed antihypertensive medications were angiotensin receptor antagonists (48%) and angiotensin‐converting enzyme inhibitors (39%).
Figure 1.
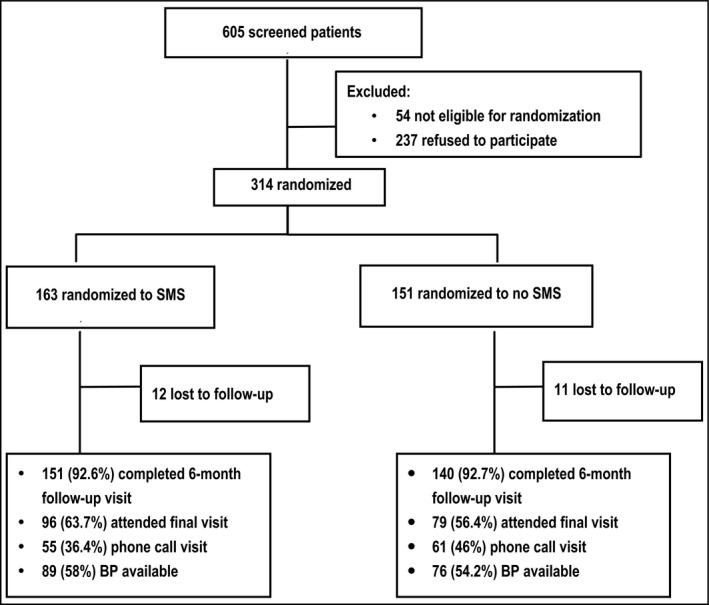
Study flow chart. BP indicates blood pressure; SMS, short message service
Table 2.
Study population baseline characteristics
| Characteristic | Non‐SMS/control group (n=151) | SMS group (n=163) | P value |
|---|---|---|---|
| Women, % | 63.6 | 65.6 | .7 |
| Age, y | 59.9±10.7 | 60.7±10.4 | .6 |
| Age range, y, % | .8 | ||
| 30–40 | 4.6 | 3.7 | |
| 41–50 | 17.9 | 16.0 | |
| 51–60 | 24.5 | 23.9 | |
| 61–70 | 37.7 | 41.7 | |
| 71 or older | 15.2 | 14.7 | |
| Educational level, % | .6 | ||
| Primary | 27.0 | 27.5 | |
| Secondary | 43.2 | 37.5 | |
| Superior | 29.7 | 35.0 | |
| Technical | 20.9 | 23.8 | |
| University | 8.8 | 11.2 | |
| Diabetes mellitus, % | 26.5 | 22.2 | .4 |
| Dyslipidemia, % | 41.6 | 48.5 | .3 |
| Current smoker, % | 17.2 | 19.6 | .7 |
| Systolic BP, mm Hg | 140.0±18.1 | 142.4±19.6 | .5 |
| Diastolic BP, mm Hg | 78.6±11.2 | 80.6±12.4 | .4 |
| No. of pills prescribed | 2.1 | 2.0 | .4 |
| Antihypertensive medications, % | |||
| ACEIs | 39.3 | 39.7 | .7 |
| Calcium antagonists | 14.3 | 7.3 | .1 |
| ARBs | 51.4 | 44.4 | .2 |
| Diuretics | 32.9 | 27.2 | .3 |
| β‐Blockers | 9.3 | 13.2 | .2 |
Abbreviations: ACEIs, angiotensin‐converting enzyme inhibitors; ARBs, angiotensin receptor blockers; BP, blood pressure; SMS, short message system.
Data are presented as mean±SD unless otherwise indicated.
Education levels are defined as follows: primary (completed ≤8 years), senior (completed between 8 and 12 years), and superior (completed >12 years achieving a technical or university diploma).
Of the 314 patients, 163 patients were randomized to receive SMS intervention and 151 were randomized to no text messaging (ie, the control arm). There were no significant differences between the groups at baseline with respect to demographics and clinical characteristics (Table 2). During the study the healthcare exposure did not differ between groups, inasmuch as access to the PCP is not ruled by the patient but by an organizational chart.
After 6 months of follow‐up, 12 patients (7.3%) in the SMS text message arm and 11 patients (7.2%) in the control arm were lost to follow‐up. The 6‐month final visit was performed in 60% of the study population in person and in 40% of the patients by phone (without BP measurement).
3.1. Adherence to hypertensive drugs
Overall, baseline and follow‐up antihypertensive medication adherence rates were 54% and 57%, respectively. After 6 months, medication adherence decreased for the control group from 59.3% to 51.4%, although this difference was not statistically significant (P=.1). By contrast, adherence improved significantly in the SMS text message group from 49% to 62.3% (P=.01). The effect of SMS on antihypertensive treatment in the study population is shown in Figure 2C. The analysis of the patients with baseline adherence and nonadherence shows a significant increase in the baseline nonadherent group with SMS vs the non‐SMS intervention (Figure 2A,B).
Figure 2.
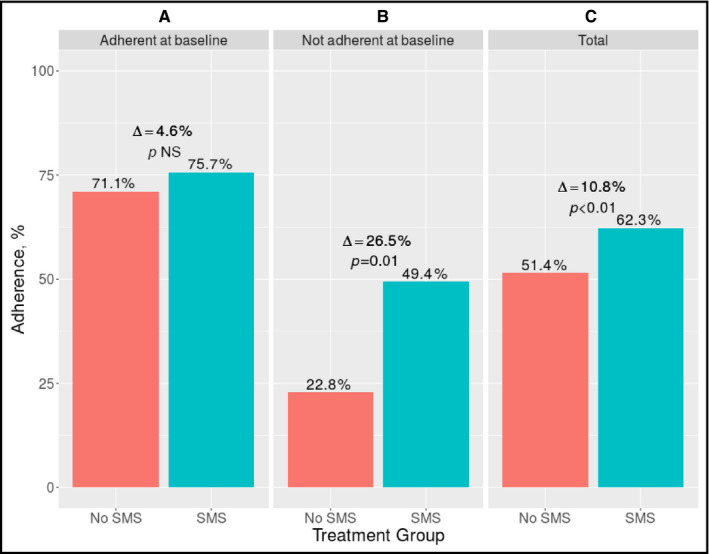
Effect of short message service (SMS) on adherence to antihypertensive treatment after 6 months. (A) Adherence rates in adherent baseline patients receiving SMS versus those with no SMS; (B) adherence rates in nonadherent baseline patients receiving SMS versus those with no SMS; (C) adherence rates in patients receiving SMS versus those with no SMS
The logistic regression model (risk ratio, 1.3; 95% confidence interval, 1.0–1.6 [P<.05]) showed that the SMS intervention improved antihypertensive medication adherence by 30% in the study population (Figure 3). Of note, a higher improvement in 6‐month medication adherence probability was observed in the baseline nonadherent subgroup (risk ratio, 2.3; 95% confidence interval, 1.4–4.4 [P<.001]).
Figure 3.
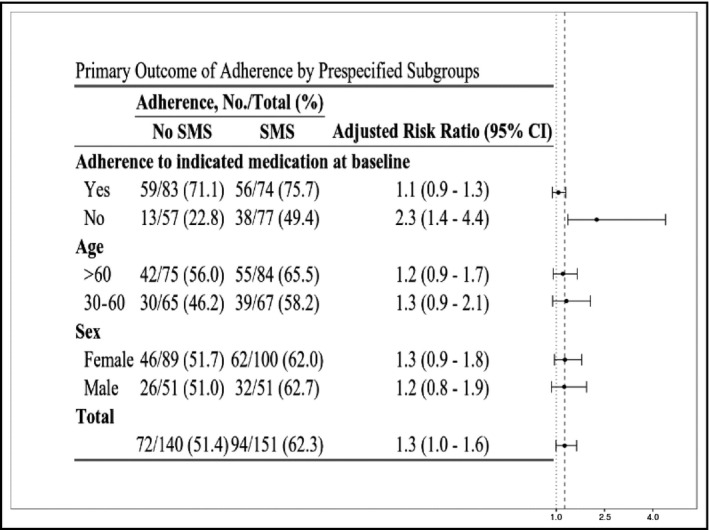
Adherence for the overall population and for prespecified subgroups. CI indicates confidence interval; SMS, short message system
Prespecified subgroup analyses by age (>60 years and between 30 and 60 years) and sex did not show significant differences for adherence rates in the SMS intervention group.
3.2. Blood pressure
Baseline mean BP was 142.7/81.1 mm Hg and 140/78.4 mm Hg in the SMS and non‐SMS groups, respectively. At the end of the study, BP data were available and reliable for 165 patients (57%). After the 6‐month follow‐up, mean BP was 134.6/77.5 mm Hg in the SMS group and 136.8/78.3 mm Hg in the non‐SMS group. While BP reduction was higher in the text‐messaging group, there was not enough power to make statistical comparisons.
4. DISCUSSION
Cellular phones are widely used around the world, and SMS has consequently been incorporated into daily life. Text messaging has been demonstrated to be a powerful tool to influence behavioral changes.27 The advantages of text messaging over other tools are considerable, including that it is widely available, relatively inexpensive, and confidential. The information can be sent at different set times and keeps the patient in contact with the medical team. It is reasonable, therefore, to believe that SMS could help with cardiovascular risk factors management. In fact, studies using SMS for smoking cessation and weight loss have reported successful results.28, 29, 30
A meta‐analysis has shown that mobile phone text messaging doubles the odds of medication adherence in chronic diseases.15 There are multiple studies evaluating the effects of SMS in chronic diseases such as asthma and diabetes mellitus, but there are limited and conflicting data on its use in patients with hypertension. For example, an interventional study with SMS conducted in Spain in patients with hypertension did not show positive results in drug adherence.31 The authors attributed their findings to an insufficient number of enrolled patients. Another study from Poland included SMS as well as other educational initiatives and reported a significant improvement in adherence to antihypertensive therapies.32 However, the design of this study was criticized because it included many educational tools, and it was therefore difficult to isolate the effect of SMS. Finally, the single‐blind randomized StAR (SMS‐Text Adherence Support) trial in South Africa compared unidirectional SMS, interactive SMS, and usual care in patients with hypertension and reported significant improvements in the availability of dispensed drugs (≥80% days covered with medication, a proxy for adherence) in both SMS groups compared with the usual care group.33
In Latin America, there are no data analyzing text messaging as a tool for improving medication adherence in the hypertensive population. In this regard, our results are the first to demonstrate that newer technologies, even in low‐intermediate socioeconomic groups, could be useful in the management of hypertension.
Mobile health studies have been performed in Latin America such as one validating text messages in behavioral change to prevent hypertension.34 Nevertheless, there are no data analyzing text messaging as a tool for improving medication adherence in the hypertensive population. In this regard, our results are the first to demonstrate that newer technologies, even in low‐intermediate socioeconomic Latino groups, could be useful in adherence to antihypertensive drugs. Latin America boasts a fast‐growing population of cell phones, and text messaging is an inexpensive and ready‐to‐use technology that could become an effective tool for our clinicians to overcome poor medication adherence in the real‐world community setting.
Indeed, knowledge of the main barriers (perceived by patients) to medication adherence is relevant and provides an opportunity for a medical team to develop approaches to address these barriers and potentially optimize adherence. For example, Egan and colleagues35 reported that pill intake forgetfulness was a main reason for inadequate adherence to antihypertensive therapy. A first report from a sample of our study population showed that forgetfulness was the primary reason for nonadherence.36 In addition, lack of understanding of the antihypertensive drug's benefits is important. Given these findings, it is possible that an SMS program that reinforces pill intake with text messaging and gives tips to avoid forgetting drug intake are a driver for the improvement in medication adherence in the intervention group. It is an achievement to convince patients of the benefits of having a routine in taking their medication. It is important to keep in mind that in our study, the SMS was not designed as a dose‐taking reminder and therefore the messages should have been daily.
Another explanation for our results is the behavioral change that was achieved by the text messaging. Behavioral changes are difficult to achieve in a population because they depend on beliefs, perceptions, social environment, and patient motivation.37 Given the current time constraints in clinical practice, it is difficult for a primary care doctor to properly communicate and motivate a patient to be adherent during a regular office visit. Education about the importance of adherence and lifestyle behaviors is ideally performed by a nurse. Unfortunately, physicians do not have nurses to assist them with these tasks in many Latin American countries. Therefore, the decision to take medication and be adherent depends primarily on a patient's beliefs and willingness to do so. Another challenge in encouraging adherence with antihypertensive medication is that the benefits of the medication are not readily perceived or recognized by patients, given the silent nature of the disease and its treatment. Therefore, text messages that focus on education about hypertension and the benefits of antihypertensive therapies could complement and facilitate the physician's job. Of note, the significant findings in patients identified as nonadherent at baseline reinforce the importance of the overall results and provide support that SMS could be an effective and easy‐to‐use intervention tool to use with nonadherent patients with hypertension in the community. In this regard, even though there was no significant difference between analyses of prespecified subgroups by age, it is highly probably that younger populations will benefit more, considering that at our baseline population analysis, younger age was associated with low adherence to antihypertensive treatment.36
5. STUDY LIMITATIONS AND STRENGTHS
Our study has some limitations: First, while our study showed significant improvement in antihypertensive medication adherence in the overall SMS group, it lacked statistical power to confirm the efficacy of this approach in the subgroup analyses by age and sex, likely attributable to the fact that the sample size calculation was based on the adherence behavior reported in a global hypertensive population. Second, the study was not powered to identify difference in BP or better control between the two arms. These outcomes would have required a 6‐month mandatory visit as a part of the study design. There was a considerable proportion of patients who conducted the final visit by phone, with no BP measurements. In addition, BP control is influenced by numerous variables, including physician inertia, salt consumption, and concomitant medications, among others. Third, we used the MGL questionnaire to assess medication adherence in this study; however, this tool is not considered to be as accurate as pill count or electronic devices to evaluate adherence. Because antihypertensive medication prescription and delivery was conducted by the primary care clinics and independently of the study's coordinating center, we did not consider pill count for this study. We did not use electronic devices to measure adherence because of the associated costs. Despite limited local data on the validation of the MGL questionnaire in our population, the Chilean Health Ministry promotes its use in patients with uncontrolled hypertension in the primary care setting.38 Moreover, published data support the utility of the MGL questionnaire for measuring adherence.39 Last, our study population incorporated few patients in the highest socioeconomic strata (approximately 10%). This is mainly because our patient population was derived from 12 primary care clinics in Santiago. Patients in the highest socioeconomic strata are not typically treated in primary care clinics, but rather in private clinics. Evidence suggests there is a lower risk of nonadherence to antihypertensive drugs among individuals with a higher socioeconomic status.40
The strengths of our study are the multicenter, randomized design and the fact that it was conducted in public primary care centers; therefore, the data represent real‐world findings. Moreover, it is the first study of an SMS intervention in a hypertensive population performed in Latin America.
6. CONCLUSIONS
This study demonstrated that an educational intervention using mobile text messaging significantly improves self‐reported antihypertensive medication adherence in a hypertensive population with <6 months of prescribed drug treatment. A potential implication of this study is the promotion of text messaging in a hypertensive population susceptible to low therapy compliance, either because of lack of education or motivation. Our data support the need for more robust studies in Latin America with more patients and complementary measures of medication adherence. Long‐term follow‐up studies using this type of intervention are necessary to evaluate whether the promising short‐term effects are maintained over time and associated with additional benefits. At the same time, with a public health perspective, this type of intervention must be evaluated with a cost‐effectiveness analysis. Future research should focus on the number and frequency of messages that achieve greater impact on this population and on the identification of the nonadherent patients with hypertension.
CONFLICTS OF INTEREST
Paola Varleta has received speaker fees for MSD and TEVA Pharmaceuticals, has participated in an advisory board of Boehringer Ingelheim, and has received an unrestrictive grant from TEVA Pharmaceuticals for a project in Ideal Cardiovascular Health in Women. Monica Acevedo has been a speaker for Novartis on sacubitril/valsartan and for Ferrer Pharmaceuticals on polypill, and has received an unrestrictive grant by TEVA Pharmaceuticals for a project in Cardiovascular Health in women. Carlos Akel has been speaker for SAVAL Pharmaceuticals. All other authors have no conflicts of interest to disclose.
This study was supported by the Foundation of the Chilean Society of Cardiology and by an unrestricted grant from Novartis.
ACKNOWLEDGMENTS
The authors would like to thank the following healthcare professionals: Hilda Hernández, MD; Patricia Neira, MD; Gloria Petit, MD; and Natalia Moya, RD. Editorial assistance was provided by Emily K Donovan.
Varleta P, Acevedo M, Akel C, et al. Mobile phone text messaging improves antihypertensive drug adherence in the community. J Clin Hypertens. 2017;19:1276–1284. 10.1111/jch.13098
REFERENCES
- 1. Lim SS, Vos T, Flaxman A, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990‐2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2224‐2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life‐years lost, and age‐specific associations in 1·25 million people. Lancet. 2014;383:1899‐1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mendis S, Puska P, Norrving B, eds. Global Atlas on Cardiovascular Disease Prevention and Control. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 4. Fitz‐Simon N, Bennett A, Feely J. A review of studies of adherence with antihypertensive drugs using prescription databases. Ther Clin Risk Manag. 2005;1:93‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336:1114‐1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Burke TA, Sturkenboom MC, Lu SE, Wentworth C, Lin Y, Rhoads GG. Discontinuation of antihypertensive drugs among newly diagnosed hypertensive patients in UK general practice. J Hypertens. 2006;24:1193‐1200. [DOI] [PubMed] [Google Scholar]
- 7. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487‐497. [DOI] [PubMed] [Google Scholar]
- 8. Tong X, Chu E, Fang J, Wall H, Ayala C. Nonadherence to antihypertensive medication among hypertensive adults in the United States—HealthStyles, 2010. J Clin Hypertens (Greenwich). 2016;18:892‐900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brown M, Bussell J. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86:304‐314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roumie CL, Elasy TA, Greevy R, et al. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med. 2006;145:165‐175. [DOI] [PubMed] [Google Scholar]
- 11. National Institute of Statistics . Telephone use in focus: information bulletin of the National Institute of Statistics. http://www.ine.cl/filenews/files/2010/diciembre/pdf/telefonia_web.pdf. Accessed November 29, 2016.
- 12. Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short‐message service. Am J Prev Med. 2009;36:165‐173. [DOI] [PubMed] [Google Scholar]
- 13. Free C, Phillips G, Galli L, et al. The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10:e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chow C, Redfern J, Hillis G, et al. Effect of lifestyle‐focused text messaging on risk factor modification in patients with coronary heart disease a randomized clinical trial. JAMA. 2015;314:1255‐1263. [DOI] [PubMed] [Google Scholar]
- 15. Thakkar J, Kurup R, Laba T, Santo K, Thiagalingam A, et al. Mobile telephone text messaging for medication adherence in chronic disease: a meta‐analysis. JAMA Intern Med. 2016;176:340‐349. [DOI] [PubMed] [Google Scholar]
- 16. Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA. 2003;289:2560‐2572. [DOI] [PubMed] [Google Scholar]
- 17. Herdman M, Badia X, Berra S. El EQ‐5D: una alternativa sencilla para la medición de la calidad de vida relacionada con la salud en atención primaria. Aten Primaria. 2001;28:425‐430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self‐reported measure of medication adherence. Med Care. 1986;24:67‐74. [DOI] [PubMed] [Google Scholar]
- 19. Val A, Amorós G, Martínez P, Fernández ML, León M. Estudio descriptivo del cumplimiento del tratamiento farmacológico antihipertensivo y validación del test Morisky y Green. Aten Primaria. 1992;10:767‐770. [PubMed] [Google Scholar]
- 20. Coleman A, Freeman P, Steel S, et al. Validation of the Omron MX3 plus oscillometric blood pressure monitoring device according to the European Society of Hypertension. Blood Press Monit. 2005;10:165‐168. [DOI] [PubMed] [Google Scholar]
- 21. Bandura A. Social cognitive theory. In: Rasta R, eds. Annals of Child Development, vol. 6. Greenwich, CT: JAI Press; 1989:1‐60. [Google Scholar]
- 22. Bandura A. Self‐efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191‐215. [DOI] [PubMed] [Google Scholar]
- 23. Sackett DL, Snow JC. The magnitude of adherence and nonadherence. In: Haynes RB, Taylor DW, Sackett DL, eds. Compliance in Health Care. Baltimore, MD: Johns Hopkins University Press; 1979:11. [Google Scholar]
- 24. R Core Team . R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. https://www.R-project.org/. Accessed January 23, 2017. [Google Scholar]
- 25. Canty A, Ripley B. boot: Bootstrap R (S‐Plus) Functions. R package version 1.3‐18: 2016.
- 26. Davison AC, Hinkley DV. Bootstrap Methods and Their Applications. Cambridge, MA: Cambridge University Press; 1997. [Google Scholar]
- 27. Cole‐Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010;32:56‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Free C, Knight R, Robertson S, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single‐blind, randomised trial. Lancet. 2011;378:49‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Whittaker R, Borland R, Bullen C, Lin RB, McRobbie H, Rodgers A. Mobile phone‐based interventions for smoking cessation. Cochrane Database Syst Rev. 2009;(4):CD006611. [DOI] [PubMed] [Google Scholar]
- 30. Haapala I, Barengo N, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: a 1‐year effectiveness study. Public Health Nutr. 2009;12:2382‐2391. [DOI] [PubMed] [Google Scholar]
- 31. Márquez E, dela Figuera M, Gil V, et al. [Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA‐Alert)]. Aten Primaria. 2004;34:399‐405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wizner B, Gaciong Z, Narkiewicz K, Szykula D, Grodzicki T. High risk patients benefit most from the SMS‐based intervention. J Hypertens. 2010;28(eSuppl):e329. [Google Scholar]
- 33. Bobrow K, Farmer AJ, Springer D, et al. Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS‐Text Adherence Support [StAR]): a single‐blind, randomized trial. Circulation. 2016;133:592‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Diez‐Canseco F, Zavala‐Loayza J, Beratarrechea A, et al. Design and multi‐country validation of text messages for an mhealth intervention for primary prevention of progression to hypertension in Latin America. JMIR Mhealth Uhealth. 2015;3:e19. 10.2196/mhealth.3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Egan BM, Lackland DT, Cutler NE. Awareness, knowledge, and attitudes of older Americans about high blood pressure: implications for health care policy, education, and research. Arch Intern Med. 2003;163:681‐687. [DOI] [PubMed] [Google Scholar]
- 36. Varleta P, Akel C, Acevedo M, et al. Assessment of adherence to antihypertensive therapy. Rev Med Chil. 2015;143:569‐576. [DOI] [PubMed] [Google Scholar]
- 37. Noar Z, Zimmerman R. Health behavioral theory and cumulative knowledge regarding health behaviors: are we moving to the right direction? Health Educ Res. 2005;20:275‐290. [DOI] [PubMed] [Google Scholar]
- 38. Chilean Health Minister (MINSAL) . Guía clínica hipertensión arterial primaria o esencial en personas de 15 años y más 2010. http://web.minsal.cl/portal/url/item/7220fdc4341c44a9e04001011f0113b9.pdf. Accessed November 28, 2016.
- 39. Castellano JM, Sanz G, Peñalvo JL, et al. A polypill strategy to improve adherence: results from the FOCUS project. J Am Coll Cardiol. 2014;64:2071‐2082. [DOI] [PubMed] [Google Scholar]
- 40. Alsabbagh W, Lemstra M, Eurich D, et al. Socioeconomic status and nonadherence to antihypertensive drugs: a systematic review and meta‐analysis. Value Health. 2014;17:288‐296. [DOI] [PubMed] [Google Scholar]


