Drug therapy for hyperlipidemia1 and hypertension2 has significantly contributed to the reduction of coronary heart disease (CHD). However, the burden of CHD remains high, as indicated from a recent report by the American Heart Association (AHA) statistical analysis.3 For the reduction of CHD, other means in addition to drug therapy, such as healthy lifestyle with a low‐risk diet and exercise, are as effective in the prevention of CHD.4, 5, 6, 7, 8, 9, 10, 11, 12, 13 However, despite the fact that these lifestyle changes are beneficial, inexpensive, and safe, very few people practice these modifications.13 In this study, data collected from 12,744 participants in the Atherosclerosis Risk in Communities (ARIC) study cohort, aged 45 to 64 years, only 0.1% had practiced ideal cardiovascular health and 17.4% had practiced intermediate cardiovascular health, whereas 82.5% had practiced poor cardiovascular health as defined by the AHA.14 The beneficial cardiovascular effects of a healthy low‐risk diet and exercise were also demonstrated by a recent prospective, population‐based study.13 This study showed that the combination of a low‐risk diet and exercise among 20,721 men aged 49 to 75 years free of CHD at onset who were followed for 11 years could prevent 80% (95% confidence interval [CI], 34%–93%) of primary myocardial infarction (MI).
Definition of Ideal Health Profile
Several studies have variably defined an ideal health profile as being associated with decreased cardiovascular risk based on the presence of low‐risk factors and behaviors.4, 5, 6, 7, 8, 9, 10, 11, 12, 13 Based on these factors, the AHA has classified persons in poor, intermediate, and ideal health9 (Table I). All studies that have demonstrated a beneficial cardiovascular effect have used 4 or 5 of these low‐risk factors and life behaviors. The most common included a healthy diet, lack of smoking, leisure‐time physical activity, moderate alcohol intake, normal body weight, and normal cholesterol and blood pressure (BP) levels as being compatible with an ideal health status. The beneficial CHD and cardiovascular disease (CVD) effects of the ideal health status are listed in Table II. However, the presence of any one of these five low‐risk factors contributes significantly to the reduction of CHD (Figure). In addition, the beneficial cardiovascular effects of low‐risk factors are independent of age, race, sex, and ethnicity.4–13
The study by Knoops and colleagues4 of 1507 men and 832 women aged 70 to 90 years from several European countries showed the beneficial effects of low‐risk factors. In these patients, the combination of the Mediterranean diet with physical activity, moderate alcohol consumption, and lack of smoking resulted in a significant decrease in CHD (hazard ratio [HR], 0.27; 95% CI, 0.14–0.53) and CVD (HR, 0.33; 95% CI, 0.22–0.47). In addition, beneficial effects were noted in those with fewer low‐risk factors (1–3).
A study by Daviglus and colleagues5 in 7302 women aged 18 to 39 years from the Chicago Heart Association Detection Project in Industry showed that a low‐risk group with normal BP, serum cholesterol, normal blood sugar, normal body mass index (BMI), and lack of cigarette smoking was associated with a significant decrease in CHD and CVD. After 31 years of follow‐up, these patients had a significantly lower incidence of CHD (HR, 0.13; 95% CI, 0.04–0.45) and CVD (HR, 0.20; 95% CI, 0.09–0.43) compared with the group with fewer low‐risk factors. However, incidence of CHD and CVD were also lower in patients with two or more low‐risk factors.
A study by Chiuve and colleagues6 of 42,847 men aged 40 to 75 years from the Health Professionals Follow‐up Study showed a significant reduction in the incidence of CHD (relative risk, 0.13; 95% CI, 0.09–0.19) after 16 years of follow‐up for those who had five low‐risk factors compared with men who were at low risk with no low‐risk lifestyle factors. These five factors included absence of smoking, BMI <25 kg/m2, moderate to vigorous physical activity ≥30 min/d, moderate alcohol consumption, and the top 40% of healthy diet score. However, significant reductions were noted for those who had more than one low‐risk factor.
A study by Odegaard and colleagues7 of 44,056 Chinese men and women aged 45 to 74 years free of diabetes mellitus (DM) and CVD at baseline and living a healthy lifestyle had significantly lower onset of CVD (HR, 0.24; 95% CI, 0.17–0.34) after a mean follow‐up period of 12 years. These patients had the presence of six low‐risk factors, which included healthy diet (upper 60% of healthy score), physical activity (≥2 h/wk), alcohol intake (>2 drinks per day), lack of smoking (never smoked), BMI (18.5–21.5 kg/m2 for <65 years and 18.5–24.5 kg/m2 for ≥65 years), and sleep of 6 to 8 hours a day. For those with the presence of one, two, three, four low‐risk factors, the HR (95% CI) were 0.60 (0.45–0.84), 0.50 (0.38–0.67), 0.40 (0.30–0.53), and 0.32 (.24–0.43), respectively.
A study by Eguchi and colleagues8 of 18,747 men and 24,263 women aged 40 to 79 years without a history of stroke or CHD at baseline and followed for 16.5 years showed that those in the highest score of low‐risk factors (7–8) had the lowest incidence of CHD. The HRs for men and women were 0.35 (95% CI, 0.25–0.49) and 0.24 (95% CI, 0.16–0.36), respectively, compared with men and women with health scores 0 to 2.
A study by Carlsson and colleagues10 of 2039 Swedish men and 2193 Swedish women aged 60 years was a prospective cohort study that showed after 11 years of follow‐up, those patients who followed a healthy lifestyle had a significant reduction in the incidence of CVD. The HRs, (95% CI) for CVD for men and women with six or seven low‐risk factors were 0.39 (0.25–0.61) and 0.44 (0.26–0.75), respectively, after adjustment for education and BMI. The low‐risk factors that were researched included, nonsmoking, alcohol intake 0.6 g/d to 30 g/d, moderate physical activity once per week, low intake of processed meats, weekly intake of fish, and daily intake of fruit and vegetables. The HRs (95% CI) for all‐cause mortality for healthy men and women were 0.35 (0.23–0.54) and 0.25 (0.15–0.44), respectively.
A prospective cohort study by Akesson and colleagues12 was performed in 24,444 Swedish postmenopausal women free of DM and CVD at baseline who were followed for 6.2 years. In women with a healthy lifestyle that included a low‐risk diet (high intake of fruits and vegetables), moderate alcohol intake (≥5 g/d), moderate physical activity (4–5 h/wk), lack of smoking, and normal BP, cholesterol, and BMI, the incidence of first MI was decreased by 92% (95% CI, 72%–98%) compared with women without any low‐risk factors. The relative risk for the primary MI in women with at least five low‐risk factors was 0.22 (95% CI, 0.07–0.70). The incidence of primary MI was considerably higher in women with two to four low‐risk factors.
A recent population‐based prospective study by Akesson and colleagues13 included 20,721 Swedish men aged 45 to 75 years. After 11 years of follow‐up, the men who had at least five low‐risk factors had a relative risk for primary MI of 0.14 (95% CI, 0.04–0.43) compared with those with no low‐risk factors. This is consistent with an 80% decrease in the incidence of primary MI or the prevention of four of five primary MIs. The low‐risk factors that were included were previously reported15 and included a healthy diet (top quintile of recommended food score), moderate alcohol consumption (10–30 g/d), lack of smoking, physical activity (walking/bicycling ≥40 min/d), and no abdominal obesity (waist circumference <95 cm). Unfortunately, only 1% of the men met these criteria. However, a decrease in the incidence of primary MI was seen proportionally, with the number of low‐risk factors present (Figure). This study also showed that men with one high‐risk factor benefited from following a healthy lifestyle.
Figure 1.
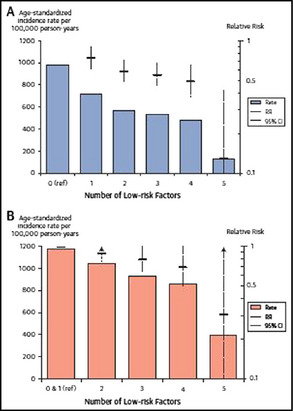
Incidence of myocardial infarction (MI) with the addition of any low‐risk factor. This figure shows the progressive reduction in the incidence of MI with the progressive addition of low‐risk factors in patients without high‐risk factors at baseline (A). This figure shows the progressive reduction in the incidence of MI with the progressive addition of low‐risk factors in patients with one high‐risk factor at baseline (B). The progressive addition of low‐risk factors had similar preventive effects for MI in both the healthy and high‐risk patients. CI indicates confidence interval. Adapted from Akesson and colleagues.13
Discussion
In the prospective study by Akesson and colleagues13 of 20,721 healthy men who practiced a healthy lifestyle, 86% had a risk reduction of primary MI. This translates to avoidance of four of five primary heart attacks. Even patients with a healthy diet and moderate alcohol consumption had a 35% reduction in primary MI. Similar findings have been previously reported by other investigators.4, 5, 6, 7, 8, 10, 13 These studies included low‐risk factors similar to those recommended by the AHA minus the alcohol intake (Table 1). The present study used low‐risk factors by the Recommended Food Score.14 The value of a healthy lifestyle on cardiovascular risk reduction has been recognized by the AHA, which has set national goals for cardiovascular health promotion and disease reduction through the year 2020 and beyond.11 Although simple, safe, and inexpensive lifestyles have been proven to significantly decrease the incidence of CHD and CVD, people prefer to practice unhealthy lifestyles, which are the cause for the high prevalence of CVDs. It is time to prioritize these most basic and fundamental behaviors to reduce the health and economic burden of cardiometabolic diseases.16, 17 The AHA has explicitly highlighted diet, physical activity, and lack of smoking as crucial to its agenda for promoting cardiovascular health independent of BP, blood cholesterol, blood glucose, and obesity levels.11 Therefore, we believe that a healthy lifestyle should be taught and promoted from a very young age through older age. This responsibility rests with the family, schools, and primary care physicians as well as cardiovascular specialists. The benefits of healthy lifestyle are greater if they are started in young persons.18
Table 1.
Definition of Low‐Risk Cardiovascular Factors by the American Heart Association Strategic Impact Goals Committee
| Metric | Level of Cardiovascular Health | ||
|---|---|---|---|
| Poor | Intermediate | Ideal | |
| Smoking | Current smoker | Quit smoking <12 months | Never smoker or quit ≥12 months |
| Diet a | Diet score=0 or 1 | Diet score=2 or 3 | Diet score=4 or 5 |
| Physical activity b | No activity | 1–49 min/wk moderate intensity | ≥150 min/wk moderate intensity |
| Body weight | BMI ≥30 kg/m2 | BMI 25–29.9 kg/m2 | BMI <25 kg/m2 |
| Glucose/DM | FBG ≥126 mg/dL | FBG 100–125 mg/dL | FBG <100 mg/dL |
| Cholesterol | TC ≥240 mg/dL or treated >200 mg/dL | TC 200–239 mg/dL or treated <200 mg/dL | TC <200 mg/dL |
| BP | Treated >140/90 mm Hg or SBP ≥140 or DBP ≥90 mm Hg | 120–139/80–89 or treated <140/<90 mm Hg | <120/80 mm Hg |
Abbreviations: BMI, body mass index; BP, blood pressure; DM, diabetes mellitus; DBP, diastolic blood pressure; FBG, fasting blood glucose; SBP, systolic blood pressure; TC, total cholesterol. aDiet score (scale=0–5) calculated as one point for each five components, including ≥4.5 fruits/vegetables per day, ≥2 3.5 oz servings fish per week, <1500 mg/d sodium, ≤450 kcal/wk (36 oz/wk of sweets/sugar sweetened beverages, and ≥3 servings per day of whole grains (1 oz equivalent servings). bLeisure‐time physical activity.
Table 2.
Studies Showing the Beneficial Effects of a Healthy Lifestyle on the Incidence of CHD and CVD
| Author | Patients, No. | Age, y | Follow‐Up, y | CHD, HR (95% CI) | CVD, HR (95% CI) |
|---|---|---|---|---|---|
| Knoops4 | 2339 M+W | 70–90 | 10 | 0.27 (0.14–0.53) | 0.33 (0.22–0.47) |
| Daviglus5 | 7302 W | 18–39 | 31 | 0.13 (0.04–0.45) | 0.20 (0.09–0.43) |
| Chiuve6 | 4287 M | 40–75 | 16 | 0.13 (0.09–0.19) | – |
| Odegaard7 | 44,056 M+W | 45–74 | 11 | 0.23 (0.14–0.37) | 0.24 (0.17–0.34) |
| Eguchi8 | 43,010 M+W | 40–79 | 17 | M: 0.19 (0.07–0.70) | 0.35 (0.25–0.49) |
| W: 0.20 (0.09–0.47) | 0.24 (0.16–0.36) | ||||
| Carlsson10 | 4232 M+W | 60 | 11 | – | M: 0.39 (0.25–0.49) |
| W: 0.44 (0.26–0.75) | |||||
| Akesson11 | 24,444 W | 59 | 6 | 0.22 (0.09–0.70) | – |
| Akesson14 | 20,721 M | 45–79 | 11 | 0.14 (0.04–0.43) | – |
Abbreviations: CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio; M, men; W, women.
Disclosures
The authors disclose no conflicts of interest and that no funds were received for the preparation of this manuscript.
References
- 1. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol lowering treatment: prospective meta‐analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–1278. [DOI] [PubMed] [Google Scholar]
- 2. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta‐analysis 0f 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics‐2014 update. A report from the American Heart Association. Circulation. 2014;129:399–410. [DOI] [PubMed] [Google Scholar]
- 4. Knoops KT, de Groot LC, Kromhout D, et al. Mediterranean diet, lifestyle factors, and 10‐year mortality in elderly European men and women. The HALE Project. JAMA. 2004;292:1433–1439. [DOI] [PubMed] [Google Scholar]
- 5. Daviglus ML, Stamler J, Pizada A, et al. Favorable cardiovascular risk profile in young women and long‐term risk of cardiovascular and all‐cause mortality. JAMA. 2004;292:1588–1592. [DOI] [PubMed] [Google Scholar]
- 6. Chiuve SE, McCullough ML, Sacks FM, Rimm EB. Healthy lifestyle factors in the primary prevention of coronary heart disease among men. Benefits of users and nonusers of lipid‐lowering and antihypertensive medications. Circulation. 2006;114:160–167. [DOI] [PubMed] [Google Scholar]
- 7. Odegaard AO, Koh WP, Gross MD, et al. Combined lifestyle factors and cardiovascular disease mortality in Chinese men and women. The Singapore Chinese Health Study. Circulation. 2011;124:2847–2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Eguchi E, Iso H, Tanabe N, et al. Healthy lifestyle behaviours and cardiovascular mortality among Japanese men and women. The Japan Collaborative Cohort Study. Eur Heart J. 2012;33:467–477. [DOI] [PubMed] [Google Scholar]
- 9. Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulation system among adults in the United States. Circulation. 2012;125:987–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Carlsson AC, Wandell PE, Gigante B, et al. Seven modifiable lifestyle factors predict reduced risk for ischemic cardiovascular disease and all‐cause mortality regardless of body mass index: a cohort study. Int J Cardiol. 2013;168:946–952. [DOI] [PubMed] [Google Scholar]
- 11. Lloyd‐Jones DM, Hong Y, Labarthe D, on behalf of the American Heart Association Strategic Planning Task Force Statistics Committee . Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 12. Akesson A, Weismayer C, Newby PK, Wolk A. A combined effect of low‐risk dietary and lifestyle behaviours in primary prevention of myocardial infarction in women. Arch Intern Med. 2007;167:2122–2127. [DOI] [PubMed] [Google Scholar]
- 13. Akesson A, Larsson SC, Discacciati A, Wolk A. Low risk and lifestyle habits in the primary prevention of myocardial infarction in men. A population‐based prospective cohort study. J Am Coll Cardiol. 2014;64:1299–1306. [DOI] [PubMed] [Google Scholar]
- 14. Folsom AR, Yatsuya H, Nettleton JA, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Michels KB, Wolk A. A prospective study of variety of healthy foods and mortality in women. Int J Epidemiol. 2002;31:847–854. [DOI] [PubMed] [Google Scholar]
- 16. Mozaffarian D. Achieving cardiovascular health, a bleak outlook or tremendous potential? J Am Coll Cardiol. 2011;57:1697–1699. [DOI] [PubMed] [Google Scholar]
- 17. Mozaffarian D. The promise of lifestyle for cardiovascular health. Time for implementation. J Am Coll Cardiol. 2014;64:1307–1309. [DOI] [PubMed] [Google Scholar]
- 18. Laitinen TT, Pahkala K, Magnussen CG, et al. Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood. The Cardiovascular Risk in Young Finns Study. Circulation. 2012;125:1971–1978. [DOI] [PubMed] [Google Scholar]


