Abstract
Accurate estimates of the prevalence rate of hypertension and determinants in Cameroon are crucial to inform efficient prevention and control policies. The authors carried out a cluster‐specific cross‐sectional survey in urban areas of the 10 regions of Cameroon to assess the prevalence and risk factors of hypertension in Cameroonian adults using the WHO STEPwise approach to Surveillance (STEPS). Sociodemographic data were collected and blood pressure and glycemia were measured using standardized methods. Participants were adults of both sexes aged 16 years or older. A total of 15,470 participants were surveyed. The age‐standardized prevalence rate of hypertension was 29.7%. The awareness rate was 14.1%. Independent correlates of hypertension included higher age, male sex, obesity, hyperglycemia, and living in the Savannah zone. The prevalence of hypertension is high in urban areas of Cameroon, with very low awareness. Prevention and control strategies should emphasize on improvement and vulgarization of population opportunistic screening and education.
Hypertension is the most frequent modifiable risk factor for cardiovascular disease (CVD) and death. Its global prevalence has been dramatically increasing for the past 2 decades.1 It is estimated that at least 1 billion adults have hypertension globally, a figure that is projected to expand to 1.5 billion by 2025, and that hypertension is associated with more than 9 million deaths annually.2, 3 Sub‐Saharan African countries along with other low‐ and low‐middle income countries are disproportionally affected by this epidemic of hypertension and consequential CVD, as they account for more than 80% of global deaths from CVD.3 According to the World Health Organization (WHO), in 2008 sub‐Saharan Africa had the highest prevalence of hypertension, with 46% of adults aged 25 and older affected in the region.3 However, there are concerns about the accuracy of such estimates of the prevalence of hypertension in sub‐Saharan Africa because they have usually been based on imputed calculations, which may be biased. Further assessments of hypertension prevalence using directly measured blood pressure (BP) and identification of potentially modifiable causes are therefore needed in the region.4
Cameroon, a low‐income country in Central Africa, has not been spared by the global epidemic of hypertension. Between 1994 and 2003, the 10‐year change showed that the prevalence of hypertension increased by two‐ to five‐fold in rural and urban Cameroonian men and women.5 The age‐adjusted prevalence rate of hypertension moved from 24.4% to 37.2% in men and from 20.1% to 37.5% in women. The hypertension prevalence rate of up to 47.5% was reported in a self‐selected urban population in Cameroon.6 This has been attributed to the rapid urbanization associated with the high rates of obesity, physical inactivity, diabetes, increased salt consumption, and tobacco use.7
The monitoring of the trends of hypertension and correlates is crucial to evaluate the effectiveness of interventions implemented to slow the rise in the disease occurrence. This nationwide survey aimed to determine the current prevalence rate of hypertension and its correlates in the Cameroonian population living in urban areas. This will help improve the effectiveness of current control strategies and plan for future cost‐effective interventions.
Methods
Ethical Considerations
This survey was approved by the national ethical review board of the Cameroon Ministry of Public Health, the results of which will help plan future interventions for the fight against the hypertension epidemic. They study was carried out in accordance with the Helsinki Declaration. Written informed consent was obtained from all the participants. All participants benefited from medical counselling and those who were diagnosed with hypertension and/or diabetes during the survey were referred for appropriate care in the nearest health facilities.
Study Design and Setting
This was a nationwide cluster‐specific cross‐sectional population‐based study carried out in the 10 regions of Cameroon in 2013. Cameroon is located in Central Africa, at the juncture of the Gulf of Guinea, slightly above the equator, covering an area of 472,442 km2, with a population of more than 19,406,100 inhabitants giving a population density of 41.08 inhabitants per square kilometer. The population is essentially young, with only about 57.5% of the national population aged 15 years and older, and about 52% lived in an urban area.8 There is varied ethnicity, with more than 240 tribes found in three main ethnic groups; Bantus in the south, Semi‐Bantus midway between the north and south, and Sudanese in the north. This varied ethnicity is distributed in four ecological zones. The Bantus is in the Forest and Littoral zone, the semi‐Bantus in the Grassland zone, and the Sudanese in the Savannah zone. At least 32.8% of the populations live on less than US$ 1 per day.8
Study Population
Adults of both sexes, aged 16 years and older, and permanent resident in the survey sights or for at least 1 month, or who intend to stay longer, and gave informed consent were included. Pregnant women were excluded. We collected data from 63 urban sites in the 10 administrative regions of Cameroon. These regions were grouped into three ecological zones: the Forest and Littoral zone including the Littoral, the Center, the South, and the East regions; the Grassland zone including the West, the North‐West, and the South‐West regions; and the Savannah zone including the Adamawa, the North, and the Far‐North regions.
Data Collection and Procedure
Participants were invited to take part in the study through messages on national television and radio, which cover all urban areas on the country. We enrolled all the potential participants who presented at the different recruitment sites and who were found eligible. Data were collected through designed questionnaires adapted from the WHO STEPwise approach to Surveillance (STEPS) in three steps.9 In step 1, we collected demographic data such as age, sex, and region. In step 2, we measured BPs using a standardized protocol with the participant in a seated position and after at least 10 minutes rest with a validated automated BP measuring device10 that were regularly calibrated to avoid erroneous measurements. The mean of two measures performed at least three minutes apart was used for all analyses. Height was measured with a calibrated stadiometer to the nearest 0.5 cm, weight in light clothes with a scale balanced to the nearest 0.1 kg. In step 3, we measured fasting blood glucose with a dry chemistry device. Medical personnel trained for this survey carried out all of the measurements.
Definitions
We defined hypertension according to World Health Organization recommendations11 as systolic BP (SBP) ≥140 mm Hg and diastolic BP (DBP) ≥90 mm Hg or a patient taking antihypertensive treatment. We defined diabetes mellitus as a fasting blood glucose >1.26 mg/dL or a patient taking antidiabetic treatment.12 Body mass index (BMI) was calculated as weight in kg/height2 in m2 and BMI‐based body habitus (in kg/m2) was classified as normal weight (BMI: 18.5–24.9), overweight (BMI: 25.0–29.9), mild or class I obesity (BMI: 30.0–34.9), moderate or class II obesity (BMI: 35.0–39.9), and severe or class III obesity (BMI: ≥40).13
Statistical Methods
Data collected on questionnaire were double‐checked and entered into an Excel datasheet and analyzed using the R version 3.0.0 software. Univariate analysis was performed for each variable. Levene's test and subsequently Student t test were used to compare the distribution of hypertension in men and women. Pearson's chi‐square test for independence was used to study the relationship of hypertension and region, age, sex, blood glucose level, and obesity. This was also used to study the relationship between obesity and sex. Logistic regression model was used to identify the potential correlates of hypertension. The prevalence rate of hypertension after age standardization was calculated as: number of existing cases divided by the population in question times 100. A P value <.05 was considered statistically significant.
Results
A total of 15,470 participants were included and 51.7% were men. Their age ranged from 16 to 94 years, with a mean of 42.7 (standard deviation: 14.2) years for both sexes. Participants from the Forest and Littoral zones were the most represented (65.9%). Hyperglycemia was present in 6.6% of participants, and 23.5% were obese, with mostly class I obesity (Table 1). The overall age‐standardized prevalence rate of hypertension was 29.7%. Among the 4800 participants with hypertension, 677 (14.1%) were aware of their status. Figures 1 and 2 present the distribution of SBP and DBP according to sex and age, respectively. Mean SBP and DBP significantly increased with age (all P values <.000) (Table 2). Men had significantly higher mean SBP than women (133.43 mm Hg vs 130.38 mm Hg, P<.05). There was no significant difference in the DBP between sexes (79.53 mm Hg vs 79.45 mm Hg, P=.427). In univariate logistic regression analyses, unadjusted correlates of hypertension included age, hyperglycemia, and abnormal weight (Table 3). In multivariate logistic regression analyses, living in the Savannah ecologic zone was associated with 1.26‐increased odds of having hypertension (P<.000) as compared with the Forest and Littoral zones. Age was highly associated with hypertension: compared with people younger than 40 years, those aged 40 to 49 years, 60 to 79 years, and 80 years and older were 3.26 times (95% confidence interval [CI], 2.997–3.538; P<.000), 6.38 times (95% CI, 5.685–7.168; P<.000), and 4.74 times (95% CI, 2.543–8.742; P<.000) more likely to have hypertension, respectively. Men were at higher risk for having hypertension (odds ratio [OR], 1.23; 95% CI, 2.543–8.742; P<.000). People with hyperglycemia were at a 2.83‐fold higher risk for having hypertension (95% CI, 2.461–3.251; P<.000). The odds of being hypertensive significantly increased with the severity of obesity (P<.000).
Table 1.
General Characteristics of the Study Population With Respect to Hypertension Status
| Variable | Total, (N=15,470) | Normotensive Individuals, (n=10,670), No. (%) | Hypertensive Individuals, (n=4800), No. (%) | Hypertension Prevalence, % | P Value |
|---|---|---|---|---|---|
| Zone | |||||
| Forest and littoral | 10,200 | 7049 (66.06) | 3151 (65.65) | 30.89 | .3587 |
| Grassland | 3272 | 2270 (21.27) | 1002 (20.88) | 30.62 | |
| Savannah | 1998 | 1351 (12.66) | 647 (13.48) | 32.38 | |
| Age, y | |||||
| <40 | 7170 | 6044 (56.64) | 1126 (23.46) | 15.70 | <.0000 |
| 40–59 | 6450 | 3796 (35.58) | 2654 (55.29) | 41.15 | |
| 60–79 | 1806 | 806 (7.55) | 1000 (20.83) | 55.37 | |
| ≥80 | 44 | 24 (0.22) | 20 (0.42) | 45.45 | |
| Sex | |||||
| Female | 7467 | 5168 (48.43) | 2299 (47.90) | 30.79 | .5463 |
| Male | 8003 | 5502 (51.57) | 2501 (52.10) | 31.25 | |
| Blood glucose | |||||
| Hyperglycemia | 1028 | 401 (3.76) | 627 (13.06) | 60.99 | <.0000 |
| Normoglycemia | 14,442 | 10,269 (96.24) | 4173 (86.94) | 28.89 | |
| Body mass index | |||||
| Normal weight | 6989 | 5369 (50.32) | 1620 (33.75) | 23.18 | <.0000 |
| Overweight | 4842 | 3215 (30.13) | 1627 (33.90) | 33.60 | |
| Class I obesity | 2438 | 1456 (13.65) | 982 (20.46) | 40.28 | |
| Class II obesity | 850 | 473 (4.43) | 377 (7.85) | 44.35 | |
| Class III obesity | 351 | 157 (1.47) | 194 (4.04) | 55.27 | |
Figure 1.
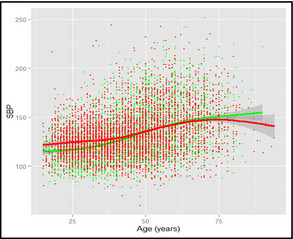
Evolution of mean systolic blood pressure with age while controlling for sex. Red curve = males; Green curve = females.
Figure 2.
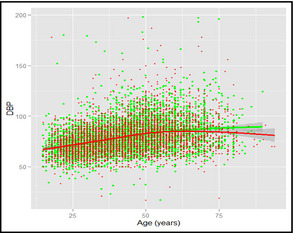
Evolution of mean diastolic blood pressure with age while controlling for sex. Red curve = males; Green curve = females.
Table 2.
Mean SBP and DBP According to Age and Sex
| Blood Pressure | Sex | Age Group, y | P Value | |||
|---|---|---|---|---|---|---|
| <40 | 40–59 | 60–79 | ≥80 | |||
| Mean SBP (SD) | Female | 120.87 (16.28) | 136.68 (24.08) | 149.12 (26.94) | 154.50 (33.30) | <.000 |
| Male | 126.97 (16.12) | 137.97 (24.19) | 148.02 (25.94) | 142.58 (18.84) | <.000 | |
| Mean DBP (SD) | Female | 75.08 (11.71) | 83.82 (15.05) | 87.64 (18.40) | 89.31 (17.08) | <.000 |
| Male | 75.54 (11.42) | 84.18 (15.61) | 85.82 (16.28) | 78.42 (9.76) | <.000 | |
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure; SD, standard deviation. Blood pressure values are expressed in mm Hg.
Table 3.
Unadjusted and Adjusted Correlates of Hypertension
| Variable | Unadjusted Correlates | Adjusted Correlates | ||||
|---|---|---|---|---|---|---|
| Odd Ratios | 95% CI | P Value | Odd Ratios | 95% CI | P Value | |
| Region (reference: forest and littoral) | ||||||
| Grassland | 0.99 | 0.906–1.075 | .772 | 1.01 | 0.923–1.111 | .788 |
| Savannah | 1.07 | 0.966–1.187 | .188 | 1.26 | 1.125–1.410 | <.000 |
| Age, y (reference: <40 y) | ||||||
| 40–59 | 3.75 | 3.463–4.069 | <.000 | 3.26 | 2.997–3.538 | <.000 |
| 60–79 | 6.66 | 5.953–7.455 | <.000 | 6.38 | 5.685–7.168 | <.000 |
| 80+ | 4.47 | 2.439–8.116 | <.000 | 4.74 | 2.543–8.742 | <.000 |
| Sex (reference: female) | ||||||
| Male | 1.02 | 0.954–1.094 | .535 | 1.23 | 1.142–1.331 | <.000 |
| Blood glucose (reference: normoglycemia) | ||||||
| Hyperglycemia | 3.85 | 3.379–4.386 | <.000 | 2.83 | 2.461–3.251 | <.000 |
| Body mass index (reference: normal weight) | ||||||
| Overweight | 1.68 | 1.546–1.820 | <.000 | 1.59 | 1.454–1.732 | <.000 |
| Class I obesity | 2.24 | 2.026–2.466 | <.000 | 2.07 | 1.863–2.309 | <.000 |
| Class II obesity | 2.64 | 2.281–3.057 | <.000 | 2.53 | 2.158–2.964 | <.000 |
| Class III obesity | 4.10 | 3.296–5.096 | <.000 | 4.11 | 3.255–5.197 | <.000 |
Discussion
This nationwide study presents the current age‐standardized prevalence rate of high BP and its correlates in urban areas of Cameroon. The prevalence rate of hypertension is very high, with the tendency of a steady rise toward a super epidemic in 20 years to come. This is associated with some known risk factors such as increasing age, male sex, high blood glucose levels, and higher BMI. More important, regions in the savannah ecological zones are identified as correlates of high BP.
The high prevalence rate of hypertension shown in this study has been suggested by evidence from previous studies in Cameroon since 1993, despite the heterogeneity in the methodologies and cutoff values used to define high BP. Cooper and colleagues14 reported an age‐standardized prevalence rate of 19.1% in 1993, Mbanya and colleagues15 reported a rate of 16.4% in 1998, Kamadjeu and colleagues16 reported a rate of 25.6% in 2006, Kengne and colleagues17 reported a rate of 20.8% in 2007, and Dzudie and colleagues6 reported a rate up to 47.5% in 2012 in a self‐selected urban population. The higher prevalence reported in this study is associated with a higher prevalence of some known risk factors reported by other authors.5, 6, 15, 16, 17, 18 Particularly, a recent study by Katte and colleagues19 showed a high prevalence of coincident diabetes and hypertension in a semi‐urban Cameroonian population, with age, sex, and adiposity as major determinants of hypertension.
Interestingly, a marked regional difference of the prevalence rate of hypertension was noted in the findings from Dzudie and colleagues.6 In this nationwide study, patients in the regions in the savannah ecological zone were more at risk for hypertension. This could be explained by a favorable environmental and genetic susceptibility to hypertension besides the known classical risk factors. This is suggested by the heterogeneous population and geographical situation of Cameroon.8 Compared with other African studies during the same timeframe, the 29.7% prevalence rate of hypertension in our study is higher than the 22.8% and 23.7% prevalence rates found in urban Nairobi (Kenya) and urban Tanzania20, 21 and the 30.6% and 28.8% rates found in urban Nigeria and Ghana, respectively,22, 23 and lower than the prevalence rates found in urban Namibia (38.0%),20 those in the town of Saint Louis in Senegal (46.6%),24 and those in the urban black population of Cape Town, South Africa (38.9%).25 Furthermore, the prevalence of hypertension in our study is lower than that found in urban areas of high‐income countries (36.4%), upper–middle‐income countries (45.2%), low–middle‐income countries (34.9%), low‐income countries (44.4%), as revealed by a recent multinational study.26 Our findings along with data from other sub‐Saharan African countries20, 21, 22, 23, 24, 25, 26 highlight the huge burden of hypertension in the region. Indeed, hypertension is a major contributor to the rising burden of CVD in sub‐Saharan Africa, which is expected to nearly double by the year 2030.27, 28 Concerted efforts are urgently needed towards prevention, early detection, and control of hypertension in the region.
Another striking finding of this study is the low awareness rate. Indeed, only 14.1% of hypertensive patients were aware of their status. This is lower than the 31.7% awareness rate found by Dzudie and colleagues6 in a self‐selected urban population. The common rule of halves in hypertension epidemiology suggests that about half of hypertensive populations are diagnosed, half of those diagnosed are treated, and half of those treated are controlled. Our finding shows that these estimates may be optimistic in many developing countries such as Cameroon.
This study has important implications. Since 2001, hypertension has been recognized as an emerging public health problem by the Cameroon Ministry of Public Health. This has led to the creation of the diabetes‐hypertension national control program with the objective of promoting equitable access to quality health services in order to reduce the morbidity and mortality associated with these conditions.7 This program is still embryonic, with limited access to cardiovascular care.29 The continuous increase in the prevalence of hypertension in Cameroon as shown by this and previous studies reveals that strategies implemented to control hypertension are inefficient. Therefore, there is an urgent need to reinforce the existing strategies and develop innovative approaches to tackle the burden of hypertension in the communities. This way, it is crucial to continuously raise awareness of hypertension and measures to prevent it in these populations, especially by encouraging the adoption of healthy lifestyles, and to improve and scale up population opportunistic screening of hypertension. Access to diagnosis and treatment should be improved, with an emphasis on the quality of health care provided, especially at the primary care level where poor management of hypertension is found.30
Study Limitations
This study has several limitations. Hypertension was defined based on a mean figure of repeated measurements at only one visit. In a community‐based survey for hypertension, this procedure is correct. However, as a true diagnosis of hypertension should be based on repeated measurements, with at least at one additional visit showing BP >140/90 mm Hg,31 the estimated prevalence of hypertension from this study may have been slightly overestimated. Participants' recruitment was biased on the fact that populations were informed using only radio and television in official languages (French and English), without involvement of local community leaders, and investigators did not visit households, rather, participants were surveyed in defined recruitment sites where there were invited. Furthermore, not all important risk factors were studied such as smoking habits, physical exercise, and salt consumption. Other risk factors that could only be diagnosed through a chemical panel were not studied. Thus, hypertension could not be fully characterized in this study. We did not assess treatment and control of hypertension. However, we report on a major outcome of hypertension: the prevalence rate of hypertension and some risk factors in a very large nationwide sample involving all the ecological zones and ethnic groups. This has provided valuable insights with baseline information for future intervention targets and in‐depth research. Further studies are needed to thoroughly determine the prevalence and determinants of hypertension in populations from both rural and urban areas of Cameroon.
Conclusions
According to this nationwide community‐based study, the prevalence of hypertension is estimated at 29.7% in urban areas of Cameroon, with a very low awareness rate (14.1%). In line with previous studies, this survey confirms an increasingly important burden of hypertension in Cameroon. Important risk factors of hypertension in our population include increasing age, male sex, high blood glucose levels, and obesity. Prevention and control strategies should emphasize improvement and increased population opportunistic screening of hypertension and education. Efforts to fight against obesity, diabetes, and other unhealthy lifestyle habits are also warranted.
Author Contributions
Study conception and design: SK. Data collection: SK, CNN. Statistical analysis and interpretation: SK, BF, JJNN, AMJ. Drafting: SK, AMJ, JJNN, APM. Critical discussion and manuscript revision: SK, AMJ, JJNN, APM, CNN, BF, GA, CN, WFTM. All the authors approved the final version of the manuscript.
Disclosures
The authors have declared that no competing interests exist.
This study was funded by Cameroon Ministry of Public Health, Department of Disease Control.
Acknowledgments
We are grateful to all the field investigators and all the individuals who volunteered to participate in this study.
J Clin Hypertens (Greenwich). 2015:819–824. DOI: 10.1111/jch.12604. © 2015 Wiley Periodicals, Inc.
References
- 1. Narayan KV, Ali MK, Koplan JP. Global non communicable diseases‐where worlds meet. N Engl J Med. 2010;363:1196–1198. [DOI] [PubMed] [Google Scholar]
- 2. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . A global brief on hypertension. WHO/DCO/WHD/2013.2. http://apps.who.int/iris/bitstream/10665/79059/1/WHO_DCO_WHD_2013.2_eng.pdf Accessed June 2, 2015.
- 4. Seligman BJ, Cullen MR, Horwitz RI. Aging, transition, and estimating the global burden of disease. PLoS One. 2011;6:e20264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Feuzeu L, Kengne AP, Balkau B, et al. Ten‐year change in blood pressure levels and prevalence of hypertension in urban and rural Cameroon. J Epidemiol Community Health. 2010;64:360–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dzudie A, Kengne AP, Muna WF, et al. Prevalence, awareness, treatment and control of hypertension in a self‐selected sub‐Saharan African urban population: a cross‐sectional study. BMJ Open. 2012;2:e001217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Echouffo‐Tcheugui JB, Kengne AP. Chronic non‐communicable diseases in Cameroon – burden, determinants and current policies. Global Health. 2011;7:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cameroon's National Institute of Statistics . Statistics year book 2010. Chapter 4: Characteristics of the population 2011: 39–52. http://www.statistics-cameroon.org/downloads/annuaire2010/chap4.pdf Accessed June 2, 2015.
- 9. Organisation Mondiale de la Santé . Le Manuel de Surveillance STEPS de L'OMS: L'approach STEPwise des Maladies Chroniques. Génève: Organisation Mondiale de la Santé; 2005. http://whqlibdoc.who.int/publications/2006/9789242593839_fre.pdf Accessed June 2, 2015. [Google Scholar]
- 10. OMRON . Clinical validations overview: OMRON blood pressure monitors June 2013. http://www.omron-healthcare.com/data/sitemanagement/media/Validation%20list%20June%202013.pdf Accessed June 2, 2015.
- 11. Guidelines Sub‐Committee . 1999 World Health Organization/International Society of Hypertension. Guidelines for the management of Hypertension. J Hypertens. 1999;17:151–183. [PubMed] [Google Scholar]
- 12. WHO‐IDF . Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. http://www.idf.org/webdata/docs/WHO_IDF_definition_diagnosis_of_diabetes.pdf. Accessed June 2, 2015.
- 13. WHO . Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation. WHO Technical Report Series 894. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 14. Cooper R, Rotimi C, Ataman S, et al. The prevalence of hypertension in seven populations of West African origin. Am J Public Health. 1997;87:160–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mbanya JC, Minkoulou EM, Salah JN, Balkau B. The prevalence of hypertension in rural and urban Cameroon. Int J Epidemiol. 1998;27:181–185. [DOI] [PubMed] [Google Scholar]
- 16. Kamadjeu RM, Edwards R, Atanga JS, et al. Prevalence, awareness, and management of hypertension in Cameroon: findings of the 2003 Cameroon Burden of Diabetes Baseline Survey. J Hum Hypertens. 2006;20:91–92. [DOI] [PubMed] [Google Scholar]
- 17. Kengne AP, Awah KP, Feuzeu L, Mbanya JC. The burden of high blood pressure and related risk factors in Urban sub‐Saharan Africa Africa: evidence from Douala in cameroon. Afr Health Sci. 2007;7:38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kamadjeu RM, Edwards R, Atanga JS, et al. Anthropometric measures and prevalence of obesity in the urban adult population of Cameroon: an update from the Cameroon Burden of Diabetes Baseline Survey. BMC Public Health. 2006;6:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Katte JC, Dzudie A, Sobngwi E, et al. Coincidence of diabetes mellitus and hypertension in a semi‐urban Cameroonian population: a cross‐sectional study. BMC Public Health. 2014;14:696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hendriks ME, Wit FW, Roos MT, et al. Hypertension in sub‐Saharan Africa: cross‐sectional surveys in four rural and urban communities. PLoS One. 2012;7:e32638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Joshi MD, Ayah R, Njau EK, et al. Prevalence of hypertension and associated cardiovascular risk factors in an urban slum in Nairobi, Kenya: a population‐based survey. BMC Public Health. 2014;14:1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Adeloye D, Basquill C, Aderemi AV, et al. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta‐analysis. J Hypertens. 2015;33:230–242. [DOI] [PubMed] [Google Scholar]
- 23. Awuah RB, Anarfi JK, Agyemang C, et al. Prevalence, awareness, treatment and control of hypertension in urban poor communities in Accra, Ghana. J Hypertens. 2014;32:1203–1210. [DOI] [PubMed] [Google Scholar]
- 24. Pessinaba S, Mbaye A, Yabeta GA, et al. Prevalence and determinants of hypertension and associated cardiovascular risk factors: data from from a population‐based, cross‐sectional survey in Saint Louis, Senegal. Cardiovasc J Afr. 2013;25:180–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Peer N, Steyn K, Lombard C, et al. A high burden of hypertension in the urban back population of Cape Town: the Cardiovascular Risk in Black South Africans (CRISBA) study. PLoS One. 2013;8:e78567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high‐, middle‐, and low‐income countries. JAMA. 2013;310:959–968. [DOI] [PubMed] [Google Scholar]
- 27. Kengne AP, Ntyintyane LM, Mayosi BM. A systematic overview of prospective cohort studies of cardiovascular disease in sub‐Saharan Africa. Cardiovasc J Afr. 2012;23:103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–619. [DOI] [PubMed] [Google Scholar]
- 29. Jingi AM, Noubiap JJ, Ewane OA, et al. Access to diagnostic tests and essential medicines for cardiovascular diseases and diabetes care: cost, availability and affordability on the west region of Cameroon. PLoS One. 2014;9:e111812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Noubiap JJ, Jingi AM, Veigne SW, et al. Approach to hypertension among primary care physicians in the west region of Cameroon: substantial room for improvement. Cardiovasc Diagn Ther. 2014;4:357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenw ich). 2014;16:14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]


