Abstract
Estimates of blood pressure (BP) control in real life are not systematically collected in Italy. We evaluated trends in systolic/diastolic BP levels, as well as prevalence, awareness, treatment, and control rates of hypertension among adult individuals visiting open checkpoints during the 2004 to 2014 annual editions of World Hypertension Day. Hypertension was defined as BP level ≥140/90 mm Hg or use of antihypertensive medication, whereas BP control was defined as BP level <140/90 mm Hg. We included 10,051 individuals (53.2% female, age 56.2±16.8 years, body mass index 25.7±7.6 kg/m2, systolic/diastolic BP 131.9±18.6/79.1±10.5 mm Hg). Hypertension prevalence and treatment were substantially unchanged, whereas awareness appears to increase over time. Controlled hypertension in diagnosed treated patients increased from 50.0% in 2004–2010 to 55.5% in 2011–2012 towards 57.6% in 2013–2014. This analysis provides real‐life snapshots of hypertension over the years in the occasion of World Hypertension Day, showing increased awareness and improved control rates among treated hypertensive patients attending open checkpoints during 2004 to 2014 in Italy.
Hypertension is a major modifiable risk factor that significantly and independently increases the risk of developing major cardiovascular complications.1 On the other hand, effective treatment for hypertension substantially reduces the risk of developing such complications.2 Despite these benefits, overall rates of blood pressure (BP) control are still reported to be largely unsatisfactory worldwide, thus contributing to a persistently high burden of hypertension‐related diseases.3, 4
Systematic and periodical evaluations of BP levels and control have been applied in various countries other than Italy, in order to estimate the effectiveness of both national and local interventions aimed at improving patients' awareness and physicians' clinical management of hypertension.5, 6, 7, 8, 9, 10 These surveys have also been recently applied in Italy, and confirmed that BP control among treated hypertensive patients is poorly achieved, ranging from 30% to 40% in most recent surveys.11, 12 Although generated from a large sample of patients with hypertension at high or very high cardiovascular risk, these analyses were derived from specific cohorts of hypertensive outpatients or select individuals from local urban or rural areas and, thus, they cannot be extrapolated to the whole national territory.11, 12 On the other hand, data on BP levels and control rates recorded in the general adult population were limited to a relatively small sample of individuals involved in the Progetto CUORE of the Italian Ministry of Health, which was accomplished in 2004.13
World Hypertension Day is a worldwide initiative of the International Society of Hypertension (ISH), World Hypertension League (WHL), and various national societies to focus population and media attention on the problem of hypertension and the consequences of uncontrolled high BP levels. During these 1‐day events, open checkpoints are made available to people in public spaces or hospital areas to measure BP levels and check other hypertension‐related clinical data for free. This provides a unique opportunity to access the “man in the street” and obtain real‐life data on hypertension awareness and control.
On the basis of these considerations, the primary aim of the present analysis was to evaluate trends in systolic/diastolic BP levels, as well as prevalence, awareness, treatment, and control rates of hypertension from 2004 to 2014 among adult individuals who had their BP measured in open checkpoints during the annual edition of World Hypertension Day in Italy. Although the methodology of the analysis does not allow any rigorous estimates on the clinical management of hypertension, these data may be useful for evaluating the effectiveness of educational interventions addressed to the general population with the principal aim to improve hypertension awareness and control at national levels.
Methods
Methodology of the Survey
This analysis was designed to evaluate the prevalence, awareness, treatment, and control of hypertension in Italy from 2004 to 2014. Data were collected during subsequent editions of World Hypertension Day, held every year during the month of May. This educational event, which was locally supported by the Italian Society of Hypertension (SIIA) and broadly promoted by the ISH and WHL in different European countries, generated a large number of data on hypertension prevalence and control in a real‐life setting.
Study Population
Involved individuals were engaged from the general population living throughout the whole national territory in Italy. Participation in the survey was free. Checkpoints for BP measurements were open for people who requested to have their BP measured, and individuals who were included in the survey did not receive any compensation for their participation.
BP Measurements
BP measurements were predominantly performed during the morning (from 8 am to 2 pm) in two different settings: (1) hospital open points, supported by local hypertension units, and outpatient clinics, which were open for medical consultations; and (2) public spaces, from external areas supported by the Italian Red Cross and located in large urban areas (including central squares, main streets, shopping centers, public institutions, and organizations).
BP levels were measured by either physicians, trained nurses, or nonmedical volunteers, according to the currently available recommendations for BP measurements.14, 15 In particular, all individuals had their systolic/diastolic BP measured in the sitting position and after a few minutes of rest. Once the participant was in a comfortable position, BP measurement was manually started and systolic and diastolic BP levels (and heart rate) were recorded.14, 15
BP measurements were performed using conventional sphygmomanometer devices or automated validated devices.
Hypertension Definition and Control
Hypertension was generally defined as systolic/diastolic BP levels >140/90 mm Hg or presence of antihypertensive medications at the time of the BP assessment.16
Although different guidelines have been available during the years,17, 18 BP control was uniformly regarded as having a BP value <140/90 mm Hg, as stated in the most recent set of European guidelines.16
Case Report Form
All data were reported into a case report form (CRF). The CRF included the following items: (1) demographic and anthropometric data (age, sex, height, and weight); (2) cardiovascular risk factors (family history of hypertension, smoking habits, hypercholesterolemia, diabetes); (3) questions for testing hypertension awareness (“Do you know your last blood pressure levels?”) and treatment (“Do you assume any antihypertensive medication?”); and (4) measured systolic and diastolic BP levels (and heart rate).
Additional information was collected in some select points and during certain years on the basis of the personal intentions of local referring physicians, as they were not mandatory. This information included the presence of concomitant clinical conditions (coronary artery disease, previous stroke, atrial fibrillation, chronic kidney disease), as well as number and type of antihypertensive drugs. Data on hypertension‐related organ damage were not collected, with the exception of values of pulse pressure, which were calculated by the difference between systolic and diastolic BP levels.
No personal information was requested to individuals included in the present study and all CRFs were anonymously completed on site and then delivered to the national committee per mail.
Data Analysis
Hypertension prevalence, awareness, and treatment were calculated in the overall sample, whereas control of hypertension was calculated among treated hypertensive patients. Average systolic/diastolic BP levels were estimated both in the overall population sample and in different subgroups or time periods.
Statistical Analysis
Continuous variables were expressed as mean±standard deviation (SD), while dichotomous variables were expressed as proportions among either overall population or specific subgroups of hypertensive patients, when appropriate. All data were recorded in a computerized spreadsheet (Microsoft Excel; Microsoft Corp, Redmond, WA), then statistical analyses were performed. Normal distribution of data was assessed using histograms and Kolmogorov‐Smirnov test. Differences between continuous variables were assessed using univariate analysis of variance. Categorical variables were compared among groups by the chi‐square test. All tests were two‐sided, and a P value of <.05 was considered statistically significant. All calculations were generated using SPSS version 15.0 (SPSS Inc, Chicago, IL).
Results
General characteristics of the study population are reported in Table 1. A total sample of 10,051 individuals (53% female, mean age 56.2±16.8 years, mean body mass index 25.7±7.6 kg/m2) was considered in the present analysis, among whom 3155 (31.0%) were included in the 2004–2010 period, 3795 (37.8%) in the 2011–2012 period, and 3141 (31.3%) in the 2013–2014 period. Overall BP levels were measured predominantly in hospital areas (75.8%) compared with public spaces (24.2%).
Table 1.
Distribution, Anthropometric Characteristics, and Cardiovascular Risk Factors in the Overall Sample and in Different Time Periods
| Parameters | Overall | Period 2004–2010 | Period 2011–2012 | Period 2013–2014 | P Value |
|---|---|---|---|---|---|
| Individuals | 10,051 (100.0) | 3115 (31.0) | 3795 (37.8) | 3141 (31.3) | |
| In‐hospital points (hypertension units) | 76,178 (75.8) | 2313 (74.3) | 3222 (84.9) | 2083 (66.3) | <.001 |
| Out‐of‐hospital areas (Italian Red Cross) | 2433 (24.2) | 802 (25.7) | 573 (15.1) | 1058 (33.7) | <.001 |
| Anthropometric parameters | |||||
| Age, y | 56.2±16.8 | 55.9±16.8 | 56.2±16.7 | 56.4±16.8 | .005 |
| Female sex | 5349 (53.2) | 1597 (51.3) | 2014 (53.1) | 1738 (55.3) | .005 |
| Height, cm | 167.0±8.7 | – | 166.5±8.4 | 167.5±8.9 | .736 |
| Weight, kg | 71.8±20.2 | – | 71.7±12.9 | 71.9±26.6 | .007 |
| BMI, kg/m2 | 25.7±7.61 | – | 25.8±4.3 | 25.7±10.3 | .643 |
| Cardiovascular risk factors | |||||
| Family history of hypertension | 3840 (46.6) | 1139 (49.2) | 1329 (45.6) | 1172 (44.9) | .003 |
| Smoking | 1982 (23.1) | 652 (24.0) | 801 (24.8) | 529 (20.3) | <.001 |
| Hypercholesterolemia | 2275 (26.6) | 702 (25.8) | 882 (27.3) | 691 (26.5) | .419 |
| Diabetes | 858 (10.0) | 225 (8.3) | 405 (4.7) | 228 (8.7) | <.001 |
| Previous CHD | 194/1627 (11.9) | – | 159 (17.3) | 35 (5.0) | <.001 |
| Previous stroke | 157/1627 (9.6) | – | 141 (15.3) | 16 (2.3) | <.001 |
| Atrial fibrillation | 63/1131 (5.6) | – | 38 (6.8) | 25 (4.4) | .083 |
| CKD | 53/754 (7.0) | – | 35 (10.0) | 18 (4.5) | .003 |
Abbreviations: BMI, body mass index; CHD, coronary artery disease; CKD, chronic kidney disease. Continuous variables are reported as mean±standard deviation, whereas dichotomous variables are reported as absolute number (percentage).
Both age and female proportions of involved individuals increased over time (P<.005 for both comparisons), whereas no significant differences were observed for anthropometric variables, when available. Family history of hypertension (P=.003) and smoking habits (P<.001) decreased over time, whereas hypercholesterolemia and diabetes did not significantly change during the observational period, being reported in about 27% and 10% of the overall population sample, respectively. Prevalence of comorbidities, including previous myocardial infarction, stroke, atrial fibrillation, and chronic kidney disease, was higher during the 2011–2012 period than that reported during the 2013–2014 period, although these data were collected in a relatively small number of centers.
BP Levels and Thresholds
Overall mean systolic/diastolic BP levels were within the high‐normal range for systolic BP and below the normal range for diastolic BP (average values 131.9±18.6/79.1±10.5 mm Hg; Table 2). A slight increase in both systolic BP and pulse pressure levels was reported in the last two time periods compared with the first one, whereas no significant changes were observed with regard to diastolic BP levels and heart rate. In addition, proportions of individuals with normal systolic, diastolic, and systolic/diastolic BP levels all increased over time.
Table 2.
Systolic/Diastolic BP Levels, Pulse Pressure, and Heart Rate in the Overall Sample and in Different Time Periods
| Parameters | Overall | Period 2004–2010 | Period 2011–2012 | Period 2013–2014 |
|---|---|---|---|---|
| Systolic BP, mm Hg | 131.9±18.6 | 131.1±19.1 | 132.6±17.9a | 131.8±18.8b |
| Diastolic BP, mm Hg | 79.1±10.5 | 79.2±11.0 | 79.3±10.2 | 78.8±10.5 |
| Pulse pressure, mm Hg | 52.8±15.2 | 52.0±15.4 | 53.3±15.0b | 53.0±15.4c |
| Heart rate, beats per min | 74.3±10.3 | 78.7±9.0 | 74.2±9.6a | 74.2±11.0a |
| Systolic BP <140 mm Hg | 6559 (65.3) | 1954 (62.7) | 2488 (65.6) | 2117 (67.4) |
| Diastolic BP <90 mm Hg | 8126 (80.9) | 2382 (76.5) | 3115 (82.1) | 2629 (83.8) |
| Systolic/diastolic BP <140/90 mm Hg | 6035 (60.0) | 1747 (56.1) | 2308 (60.8) | 1980 (63.0) |
Abbreviation: BP, blood pressure. Continuous variables are reported as mean±standard deviation, whereas dichotomous variables are reported as absolute number (percentage) among groups. a P<.005, b P<.001, and c P<.05 vs period 2004–2010.
Figure 1.
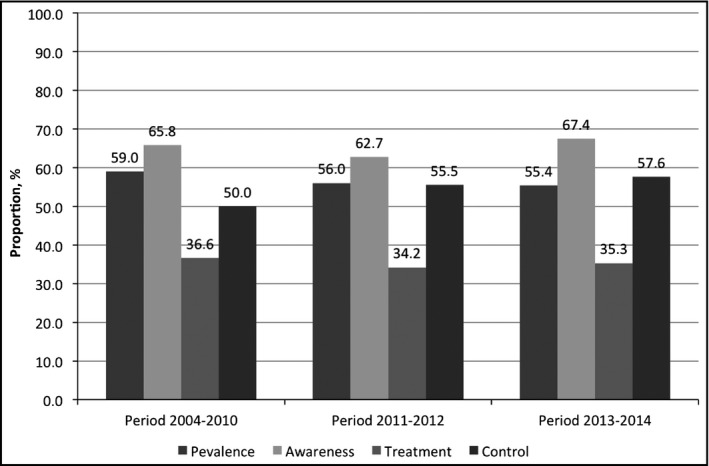
Prevalence, awareness, treatment, and control rates during the different time periods. Blood pressure control rates have been calculated among treated hypertensive individuals.
Hypertension Prevalence, Awareness, Treatment, and Control
In the overall population sample, hypertension prevalence and treatment did not significantly change, whereas awareness and control increased over time (Figure). In particular, awareness of hypertension increased from 65.8% to 67.4% (P<.001 for trend). At the same time, BP control in diagnosed and treated hypertensive patients increased from 50.0% in 2004–2010 to 55.5% in 2011–2012 toward 57.6% in 2013–2014 (P<.001 for trend).
Discussion
Previous surveys performed in Italy between 2000 and 2011 reported that BP control among treated hypertensive patients was approximately around 30%.19 Recent randomized clinical trials reported that extended use of rational and effective antihypertensive therapies allows the achievement of controlled hypertension close to 70% to 80%.20, 21 On the basis of these findings, several interventions have been promoted and applied in Italy over the past few years in order to improve BP control rates among treated hypertensive patients and to reach the proportions of 70% of treated controlled hypertension by 2015.22 Similar interventions aimed at improving awareness and treatment of hypertension has been promoted by the ISH and WHL, mostly throughout the annual organization of World Hypertension Day.23 A fundamental step shared by all these educational and clinical interventions is represented by the systematic assessment of BP levels in the general population. This large number of data can be used to provide a rough estimation of hypertension awareness and control in various countries in a setting of real life.
In this view, we analyzed for the first time temporal trends of BP levels and control rates in a relatively large sample of adult individuals from the general population involved in subsequent editions of World Hypertension Day. With the well‐known limitations of this descriptive approach, our findings confirmed the large prevalence and relatively poor treatment of hypertension in a real‐life setting. In fact, hypertension generally occurred in more than half of the involved individuals and was treated in about one third of the same population.
These findings were consistent with those reported in previous studies performed in Italy,19 as well as in other European countries.24, 25 Indeed, these data may suggest a more extensive and systematic adoption of educational programs and support for physicians involved in the clinical management of hypertension. In fact, we reported a slight but relevant increase of hypertension awareness during the observational period, particularly during the past 2 years. This may at least in part suggest that educational interventions adopted by the National Ministry of Health and different scientific societies have generated a higher level of attention on high BP assessment and control among the general population in Italy.
We also reported a progressive increase in BP control rates among diagnosed and treated hypertensive patients. Although we cannot provide a potential explanation for these findings, since we cannot address the pharmacologic therapies adopted in treated hypertensive patients, these findings are very encouraging. The achievement of about 60% of treated controlled hypertensive patients in a setting of the general population may, indeed, promote the adoption of further educational and pharmacologic interventions to achieve the so‐called “Objective 70%” by 2015.22
Potential Limitations
The present study is based on a descriptive survey; as such, it can only report trends of the selected clinical parameters, without focusing on the diagnostic and therapeutic management of hypertension in Italy. Since the individuals included in the subsequent editions of the survey may vary over the years, any comparison among different time periods should be considered with caution. Another potential bias is related to self‐selection of participants who decided to have their BP measured in open checkpoints during subsequent editions of World Hypertension Day. Involved individuals may be considered or not as people from the general population during their typical workday, simply by the fact that they decided to stop their activity to have their BP measured. Thus, the accuracy of measuring BP levels and control cannot be compared with that obtained with 24‐hour ambulatory BP monitoring. However, the same limitations can also be applied to 24‐hour ambulatory BP monitoring, which indeed may alter the typical workday, for example by applying and removing the device in the hospital clinics, as well as by limiting the routine work or family activities as a result of repeated BP measurements during the day and nighttime periods. In our opinion, this different information on BP levels and control derived from either “street BP” or “24‐hour BP” should be not viewed as opposite, but as potentially alternative and integrated tools, both providing useful clinical information for improving hypertension awareness and control. In addition, the different methodologies applied for measuring BP levels during the different time periods should always be taken into consideration when interpreting the data derived from the present analysis. Comparing single readings with the auscultatory method in an early phase with the oscillomertric method in a later phase might partly explain the progressive reduction in BP levels and the derived conclusion on the occurrence of better BP control over time. The use of different techniques for measuring BP levels, as well as the different number of BP measurements over time strictly reflected the routine practice recommended at the time of the different observations. In addition, the educational nature of the World Hypertension Day initiative did not include the need for standardized BP measurements, similar to those performed in hypertension units. It should also be noted, however, that the predominant involvement of hospital points as well as the large effort adopted by local volunteers by national scientific societies of hypertension represented two major guarantees of having accurate BP measurements. Information on comorbidities and markers of organ damage were not systematically collected, thus proper individual global cardiovascular risk stratification cannot be applied to the whole population sample. Data on antihypertensive drug therapies (both drug classes and use of monotherapy vs combination therapies) were not reported in the CRF, since they were out of the intention of the survey. Consequently, we cannot provide rates of BP control according to type and intensity of antihypertensive therapy. Finally, our analysis did not take into consideration the whole population sample of the corresponding areas or macro‐areas, so that our results may not fully represent the BP levels and control rates of the whole national territory.
Conclusions
Although prevalence and treatment of hypertension did not change over time, this survey reported increased awareness and control among treated hypertensive patients in a real‐life setting. Our study also demonstrated the importance of an educational intervention aimed at improving knowledge and control of hypertension at both national and local levels, thus promoting further interventions and actions in the future to reduce the burden of hypertension worldwide.
Sources of Funding
None.
Disclosure
No conflict of interest about the work reported in this paper has been declared by any of the authors.
Endorsement
This work has been endorsed by the Italian Society of Hypertension (SIIA).
Acknowledgments
The authors wish to thank all of the hypertension centers and their referring physicians who provided data for the present analysis. The authors also wish to thank the Croce Rossa Italiana (Italian Red Cross) for providing external support for blood pressure measurements during the subsequent Italian editions of World Hypertension Day.
J Clin Hypertens (Greenwich). 2016;18 551–556. DOI: 10.1111/jch.12711. © 2015 Wiley Periodicals, Inc.
References
- 1. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 2. Turnbull F. Effects of different blood‐pressure‐lowering regimens on major cardiovascular events: results of prospectively designed overviews of randomised trials. Lancet. 2003;362:1527–1535. [DOI] [PubMed] [Google Scholar]
- 3. Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. [DOI] [PubMed] [Google Scholar]
- 4. Danaei G, Finucane MM, Lin JK, et al. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country‐years and 5.4 million participants. Lancet. 2011;377:568–577. [DOI] [PubMed] [Google Scholar]
- 5. Sakhuja A, Textor SC, Taler SJ. Uncontrolled hypertension by the 2014 evidence‐based guideline: results from NHANES 2011–2012. J Hypertens. 2015;33:644–652. [DOI] [PubMed] [Google Scholar]
- 6. Whyte JL, Lapuerta P, L'Italien GJ, Franklin SS. The challenge of controlling systolic blood pressure: data from the national health and nutrition examination survey (NHANES III), 1988–1994. J Clin Hypertens (Greenwich). 2001;3:211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhao Y, Lu F, Sun H, et al. Trends in hypertension prevalence, awareness, treatment, and control rates in shandong province of china. J Clin Hypertens (Greenwich). 2012;14:637–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bromfield SG, Bowling CB, Tanner RM, et al. Trends in hypertension prevalence, awareness, treatment, and control among US adults 80 years and older, 1988–2010. J Clin Hypertens (Greenwich). 2014;16:270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. de Burgos‐Lunar C, Jimenez‐Garcia R, Salinero‐Fort MA, et al. Trends in hypertension prevalence, awareness, treatment and control in an adult type 2 diabetes Spanish population between 2003 and 2009. PLoS ONE. 2014;9:e86713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang J, Ning X, Yang L, et al. Trends of hypertension prevalence, awareness, treatment and control in rural areas of northern China during 1991–2011. J Hum Hypertens. 2014;28:25–31. [DOI] [PubMed] [Google Scholar]
- 11. Volpe M, Tocci G, Trimarco B, et al. Blood pressure control in Italy: results of recent surveys on hypertension. J Hypertens. 2007;25:1491–1498. [DOI] [PubMed] [Google Scholar]
- 12. Tocci G, Rosei EA, Ambrosioni E, et al. Blood pressure control in Italy: analysis of clinical data from 2005 to 2011 surveys on hypertension. J Hypertens. 2012;30:1065–1074. [DOI] [PubMed] [Google Scholar]
- 13. Palmieri L, Panico S, Vanuzzo D, et al. Evaluation of the global cardiovascular absolute risk: the Progetto Cuore individual score. Ann Ist Super Sanita. 2004;40:393–399. [PubMed] [Google Scholar]
- 14. O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension Working Group on Blood Pressure Management. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. [DOI] [PubMed] [Google Scholar]
- 15. Parati G, Omboni S, Palatini P, et al. Monitoring obotISoHWGoBP. Italian Society of Hypertension guidelines for conventional and automated blood pressure measurement in the office, at home and over 24 hours. High Blood Press Cardiovasc Prev. 2008;15:283–310. [DOI] [PubMed] [Google Scholar]
- 16. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–2219. [DOI] [PubMed] [Google Scholar]
- 17. European Society of Hypertension‐European Society of Cardiology Guidelines C . European Society of Hypertension‐European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;2003:1011–1053. [DOI] [PubMed] [Google Scholar]
- 18. Mancia G, De Backer G, Dominiczak A, et al. Hypertension E‐ETFotMoA. 2007 ESH‐ESC practice guidelines for the management of arterial hypertension: ESH‐ESC task force on the management of arterial hypertension. J Hypertens. 2007;25:1751–1762. [DOI] [PubMed] [Google Scholar]
- 19. Tocci G, Ferrucci A, Pontremoli R, et al. Blood pressure levels and control in Italy: comprehensive analysis of clinical data from 2000 to 2005 and 2005 to 2011 hypertension surveys. J Hum Hypertens. 2015 Feb 12. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 20. Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high‐risk patients. N Engl J Med. 2008;359:2417–2428. [DOI] [PubMed] [Google Scholar]
- 21. Oparil S, Melino M, Lee J, et al. Triple therapy with olmesartan medoxomil, amlodipine besylate, and hydrochlorothiazide in adult patients with hypertension: the trinity multicenter, randomized, double‐blind, 12‐week, parallel‐group study. Clin Ther. 2010;32:1252–1269. [DOI] [PubMed] [Google Scholar]
- 22. Volpe M. The changing role of hypertension societies: shifting gears in italy. High Blood Press Cardiovasc Prev. 2012;19:1–2. [DOI] [PubMed] [Google Scholar]
- 23. Campbell N, Touyz R, Lackland D, et al. Celebrate World Hypertension Day (WHD) on May 17, 2015, and contribute to improving awareness of hypertension. J Clin Hypertens (Greenwich). 2015;17:317–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bramlage P, Bohm M, Volpe M, et al. A global perspective on blood pressure treatment and control in a referred cohort of hypertensive patients. J Clin Hypertens (Greenwich). 2010;12:666–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dallongeville J, Banegas JR, Tubach F, et al. Survey of physicians' practices in the control of cardiovascular risk factors: the eurika study. Eur J Prev Cardiol. 2012;19:541–550. [DOI] [PubMed] [Google Scholar]


