In this issue of the Journal, Banegas and colleagues publish results from a cross‐sectional study from Spain in 1047 individuals 60 years and older who had casual blood pressure (BP) measurements and 24‐hour ambulatory BP measurement (ABPM) performed under standardized conditions.1
ABPM Reveals Many Secrets
The results can be summarized as follows: First, regarding the prevalence of hypertension, the data show that, in patients aged 60 years or more, the prevalence of hypertension is greatly overestimated when BP status is assessed with casual BP instead of ABPM. Specifically, 7%, or one in 15 patients diagnosed as being hypertensive according to casual BP, would be considered normotensive when ABPM is used, suggesting a considerable overdiagnosis when clinic BP is used alone. Extrapolating this figure to the elderly Spanish population means that some 700,000 people diagnosed as hypertensive with casual BP measurement would no longer be considered to be hypertensive with ABPM. The majority (51%) of the patients diagnosed as hypertensive with casual BP had white‐coat hypertension, which was eliminated with ABPM.
Second, the Spanish study results have important implications for treatment. In Spain, some 700,000 elderly subjects would be spared medication if ABPM, instead of casual BP, was performed. On the other hand, the percentage of patients considered eligible for treatment increased by 6% with ABPM, which amounts to some 350,000 elderly patients. In this instance, casual BP is masking hypertension, which only becomes apparent with ABPM. In other words, the patients who were spared treatment were partly offset by those who would receive treatment, but this occurrence has to be viewed from the perspective of drug treatment being prescribed appropriately.
Third, the use of ABPM resulted in a marked reclassification of patients. In untreated patients, 39% were hypertensive using casual BP but only 19% were hypertensive with ABPM, and these patients would have been reclassified as normal with ABPM. Similarly, in treated patients, 48% were hypertensive using casual BP, but only 24% were hypertensive with ABPM, meaning that half of these patients would be reclassified as normal with ABPM. Likewise, 6% of untreated participants had normal BP according to casual BP but would be reclassified as being hypertensive with ABPM, and 8% of treated patients who were normotensive with casual BP would be reclassified as being hypertensive with ABPM.
Fourth, BP control was influenced by the method of measurement. There was a considerable gap between the percentages of hypertensive patients at BP goal with ambulatory vs casual BP. Among patients eligible for treatment, only 37% were controlled with casual BP, whereas this figure rose to 54% with ABPM. Although, this indicates that if ABPM is used to asses BP in the community, the degree of BP control appears much better than with casual BP (simply because multiple BP measurements provide a more accurate assessment). The daunting reality is that only half of all patients were within the normal range for both casual BP and ABPM and less than half of patients with elevated casual BP and ABPM were receiving antihypertensive medication.
In conclusion, the telling messages from the Spanish study are that, compared with casual BP measurement, ABPM led to a reduction in the proportion of older patients recommended for hypertension treatment and a substantial increase in the proportion of those whose hypertension was controlled. ABPM would reduce misdiagnosis, ensure that the right people are treated with BP‐lowering drugs, and reduce the number of patients treated for hypertension. All of this means that ABPM can save money and the extra costs of providing the technique would be more than offset by cost savings from better targeted treatment.
We have analyzed data from the Dublin Outcome Study2 to illustrate just how misleading clinic BP measurement is compared with ABPM. It can be seen from Figure 1 that when office BP is within the narrow range of 150 mm Hg to 152 mm Hg for systolic BP and 88 mm Hg to 95 mm Hg for diastolic BP there are no less than six diagnostic patterns of BP with ABPM, none of which could be suspected from the office BP. In Figure 2, patients with normal clinic BP (130/70 mm Hg) had four hypertensive profiles that were masked by normal office BP. The hypertensive profiles revealed by ABPM in the illustrated instance demand very different management strategies to those that would be implemented on the basis of clinic BP.
Figure 1.
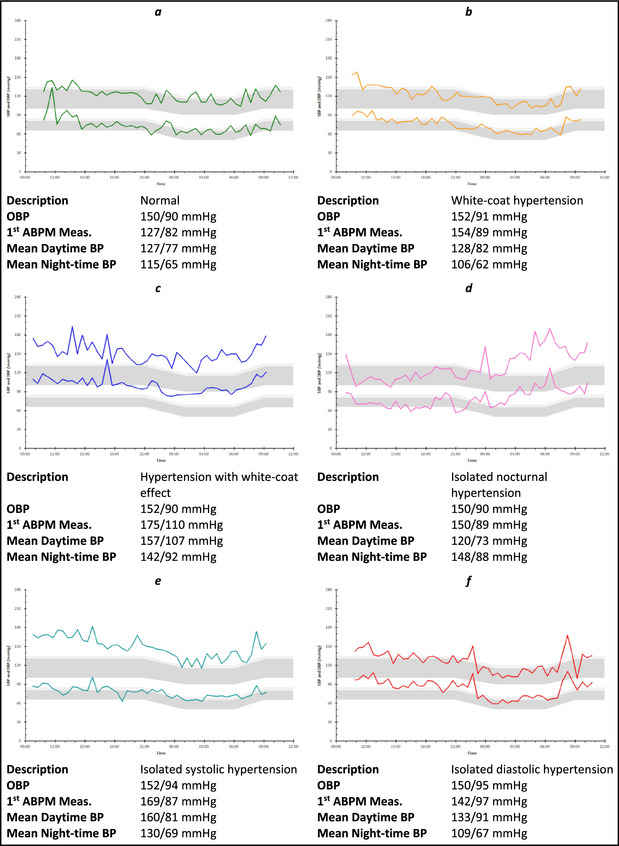
Examples of ambulatory blood pressure (BP) monitoring (ABPM) measurements where office BP was 150 mm Hg to 152 mm Hg systolic BP (SBP) and 88 mm Hg to 95 mm Hg diastolic BP (DBP). OBP indicates office BP.
Figure 2.
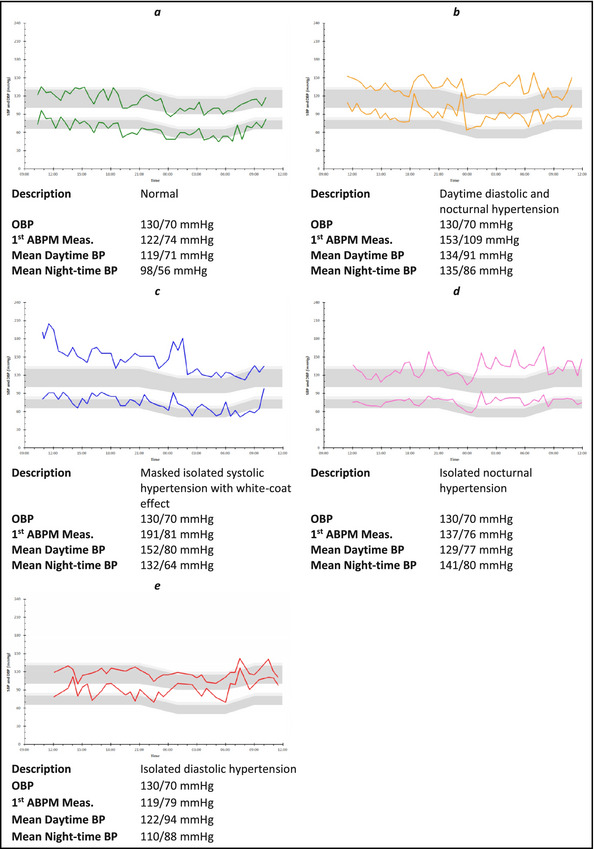
Examples of ambulatory blood pressure (BP) monitoring (ABPM) measurements where office BPs were all 130/70 mm Hg. OBP indicates office BP.
One is left wondering why it is that the technique of 24‐hour ABPM is not as available to all patients with hypertension (or suspected hypertension), as is electrocardiography to patients with chest pain.
Guideline Recommendations
Numerous guidelines and recommendations from international authorities have emphasized time and time again that diagnostic and management decisions for patients with hypertension should be based on ABPM rather than clinic measurement of BP.3, 4, 5, 6 Most notable among these has been the recommendation from the National Institute for Health and Care Excellence (NICE), which states unequivocally that ABPM should be offered to anyone who has ever had a BP ≥140/90 mm Hg.7 Moreover, it has been shown that ABPM is more cost‐effective than clinic BP or home BP measurement.8 Yet, despite all these recommendations, the technique is not available routinely, which begs two questions.
First, why is it that expensive magnetic resonance imaging of the brain is available to anyone who has had a bang on the head but ABPM is denied in patients with elevated BP? Second, what are the consequences of failing to provide the technique to such patients?
Why is ABPM Not Readily Available?
The answer to this question involves a combination of circumstances. First and foremost there is the apathy of the medical profession in recognizing the overwhelming scientific evidence for the routine use of ABPM. This negligence has been excused under various guises, such as there being insufficient evidence or the procedure is too expensive or too difficult to implement in routine practice. Added to this, there has been remarkable lack of innovative impetus from manufacturers of ABPM devices to apply modern technology to making the devices more acceptable by, for example, having the pump incorporated into the inflating cuff, so as to facilitate patient comfort by removing the need to wear a device on the waist. Also, there has been excessive reliance on the provision of the technique by doctors, be it in primary care or through specialist clinics. Recently, we showed that pharmacists could provide every bit as good an ABPM service as doctors and often at a fraction of the cost.9 Finally, there has been abject failure by health‐care providers in most countries to reimburse ABPM and, where reimbursement is provided, it has been paltry.6
Consequences of Failing to Provide ABPM
The consequences of not making ABPM available to all patients with hypertension are illustrated by the Spanish study,1 among many others.2, 3, 4, 5, 6 Patients with white‐coat hypertension are overtreated, patients with masked hypertension are undertreated, and patients with threatening profiles, such as nocturnal hypertension, are simply not identified. All of this adds greatly to the cost of health care to say nothing of the burden of cardiovascular illness that could be prevented if ABPM was readily available. There is then the elephant in the room, namely the potential for medicolegal redress by patients denied ABPM, which has not often been discussed.1, 4 Take, for example, a patient with hypertension who develops a stroke but whose treatment was based on clinic BP and in whom it was subsequently shown with ABPM that BP elevation was more severe than was apparent from clinic BP (masked hypertension) together with elevation of nocturnal BP (a well‐documented risk for cardiovascular events), which, of course, cannot be detected without performing ABPM. Does such a patient not have a reasonable case? To the best of my knowledge there have not been medicolegal consequences for failure to provide a technique that is recommended by all international societies, but let us put our house in order before we are forced to do so.
References
- 1. Banegas JR, de la Cruz JJ, Graciani A, et al. Impact of ambulatory blood pressure monitoring on reclassification of hypertension prevalence and control in older people in Spain. J Clin Hypertens (Greenwich). 2015;17:453–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality. The Dublin outcome study. Hypertension. 2005;46:156–161. [DOI] [PubMed] [Google Scholar]
- 3. O'Brien E. 24‐hour ambulatory blood pressure measurement in clinical practice and research: a critical review of a technique in need of implementation. J Int Med. 2011;269:478–495. [DOI] [PubMed] [Google Scholar]
- 4. O'Brien E. First Thomas Pickering memorial lecture: ambulatory blood pressure measurement is essential for the management of hypertension. J Clin Hypertens (Greenwich). 2012;12:836–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. O'Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1767. [DOI] [PubMed] [Google Scholar]
- 6. Turner JR, Viera AJ, Shimbo D. Ambulatory blood pressure monitoring in clinical practice: a review. Am J Med. 2015;128:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. National Institute for Health and Clinical Excellence (NICE) . Hypertension. The clinical management of primary hypertension in adults. Clinical Guideline 127. 2011. www.nice.org.uk/guidance/CG127
- 8. Lovibond K, Jowett S, Barton P, et al. Cost‐effectiveness of options for the diagnosis of high blood pressure in primary care: a modeling study. Lancet. 2011;378:1219–1230. [DOI] [PubMed] [Google Scholar]
- 9. James K, Dolan E, O'Brien E. Making ambulatory blood pressure monitoring accessible in pharmacies. Blood Press Monit. 2014;19:134–139. [DOI] [PubMed] [Google Scholar]


