Abstract
Masked hypertension (MH), the presence of normal office blood pressure (BP) with elevated ambulatory pressure, has been shown to correlate with organ damage. Population‐based studies from Europe and Asia estimate a prevalence of 8.5% to 15.8%. Two small studies in African Americans estimate a prevalence >40%. Therefore, the authors utilized ambulatory BP monitoring (ABPM) to identify the prevalence of MH in our African American population. Pressure was recorded every 30 minutes while awake and every 60 minutes while asleep. Patients with 24‐hour average BP ≥135/85 mm Hg, awake average BP ≥140/90 mm Hg, or asleep average BP ≥125/75 mm Hg had MH. Seventy‐three participates had valid data. The mean age of the patients was 49.8 years, mean body mass index was 31.1, and 39 patients (53%) were women. Thirty‐three patients (45.2%) had MH. Patients with MH had higher clinic systolic BP and trended toward higher BMI values. The authors corroborated the high prevalence of MH in African Americans. ABPM is critical to diagnose hypertension in African Americans, particularly in those with high‐normal clinic pressure and obesity.
Hypertension has been defined by several medical societies as an in‐office systolic blood pressure (SBP) >140 mm Hg or diastolic blood pressure >90 mm Hg.1, 2 Traditionally, hypertension is diagnosed based on office blood pressure (BP) measurements with the average measurement of two or more readings taken at each of three or more visits during a span of weeks to months to represent the actual BP. The development of techniques to measure BP outside the physician's office with either home or 24‐hour ambulatory BP monitoring (ABPM) has made BP characterization more complex. Individuals may have sustained hypertension (BP elevated in both settings), sustained normotension (BP controlled in both settings), white‐coat hypertension (BP elevated in the office but normal outside of the office), or masked hypertension (BP normal in the office but elevated throughout the day).3
The clinical entity “masked hypertension” was first named and described by Pickering and colleagues in 2002.4 Patients with masked hypertension are at increased risk for adverse cardiovascular events at a level similar to patients with documented hypertension.5 In fact, 24‐hour BPs have been shown to correlate better with end‐organ damage than traditional office measurements and better predict progression to end‐stage renal disease.6
Several population‐based studies have reported the prevalence of masked hypertension to be between 8.5% and 15.8%.7, 8, 9, 10 These studies were conducted in European countries and Japan, thus they may not reflect the prevalence of masked hypertension in American populations. One New York study involving employed adults reported a prevalence of 15.2%.11 Two small studies examining African Americans (n=38 and n=50) reported a prevalence of 46% and 58%.12, 13 In our present study we sought to determine the prevalence of masked hypertension in an African American population attending an urban ambulatory internal medicine clinic in southeast Michigan.
Methods
Study Population
We enrolled African Americans aged 18 to 85 years attending a primary care ambulatory internal medicine clinic in southeast Michigan between February 2012 and June 2014. Patients must have had at least two prior clinic visits. Patients had to be normotensive (BP <140/90 mm Hg) based on office BP measurements taken on each of three consecutive office visits prior to enrollment. Patients with a previous diagnosis of hypertension or taking medication that affected BP such as angiotensin‐converting enzyme inhibitors, angiotensin receptor blockers, diuretics, calcium channel blockers, α‐blockers, or β‐blockers were excluded. Demographic and clinical data were collected prospectively. Written informed consent was obtained from all participants before enrollment. The study protocol was approved by the St. John Providence institutional review board.
Study Design
Patients underwent 24‐hour ABPM using a noninvasive BP monitor (Oscar 2; SunTech Medical, Morrisville, NC) starting at the time of enrollment. BP was measured every 30 minutes in patients while awake and every 60 minutes while asleep. Patients were provided a diary to record their activity and emotional status during each measurement. To be included in the analysis each patient had to have at least 80% valid BP measurements. Individual measurements were considered invalid if there was artifact or cuff timeout error. BP recordings were then analyzed using computer analysis software. Mean 24‐hour, awake, and asleep BPs were calculated. Patients with average 24‐hour BP ≥135/85 mm Hg, awake average ≥140/90 mm Hg, or asleep average ≥125/75 mm Hg were considered to have masked hypertension. Patients found to have masked hypertension were compared with those who were confirmed to have normotension. Statistical tests were performed using SPSS v11.5.1 (IBM, Armonk, NY).
Results
Patient demographics are summarized in Table 1. Of 101 patients enrolled, 73 had valid data. The mean age was 49.8 (±13) years, 39 (53%) were women, mean body mass index was 31.1 (±6.6), average sleep duration was 6.25 (±1.5) hours per night, and mean BP measured in the clinic was 120/76 (±10.4/7.3) mm Hg. Overall, there were few medical comorbidities; 3 (4%) had diabetes mellitus, 7 (10%) had dyslipidemia, and 7 (10%) had known obstructive sleep apnea. Sixteen (22%) used tobacco products, 5 (7%) admitted to daily alcohol use, and 4 (5%) admitted to marijuana use. The total population averaged 1.2 (±1.4) fast‐food meals per week (range 0–5) and 0.98 (±1.2) cups of coffee per day (range 0–6). In total, 46 (63%) participants knew of a first‐degree relative with hypertension.
Table 1.
Study Demographics
| Age,y | 49.8 (±13) |
| Women, No. (%) | 39 (53) |
| Body mass index | 31.1 (±6.6) |
| Clinic pressure,mmHg | 120/76 (±10.4/7.3) |
| Diabetes mellitus, No. (%) | 3 (4) |
| Dyslipidemia, No. (%) | 7 (10) |
| Obstructive sleep apnea, No. (%) | 7 (10) |
| Family history of hypertension, No. (%) | 46 (63) |
| Tobacco use, No. (%) | 16 (22) |
| Daily alcohol use, No. (%) | 5 (7) |
| Marijuana use, No. (%) | 4 (5) |
| Sleep duration, h per night | 6.25 (±1.5) |
| Fast food intake, meals per wk | 1.2 (±1.4) |
| Coffee consumption, cups per d | 0.98 (±1.2) |
Masked hypertension was present in 33 (45.2%) patients. Table 2 compares patients with masked hypertension with those with confirmed normotension. There was no significant difference in age, sex, presence of diabetes mellitus, dyslipidemia, or obstructive sleep apnea; tobacco, alcohol, or coffee use; number of fast‐food meals per week; or family history of hypertension. Patients with masked hypertension had a higher average SBP in the clinic (124 mm Hg vs 118 mm Hg, P=.02) and tended to have a higher BMI (32.6 vs 29.9, P=.10).
Table 2.
Characteristics of Patients With Masked Hypertension Compared With Those With Confirmed Normotension
| Masked Hypertension (n=33) | Confirmed Normotension (n=40) | P Value | |
|---|---|---|---|
| Mean clinic systolic pressure, mmHg | 124 (±10.2) | 118 (±10.5) | .02 |
| Mean clinic diastolic pressure, mmHg | 77 (±6.7) | 75 (±7.8) | NS |
| Age, y | 50.8 (±12.4) | 49.1 (±14.1) | NS |
| Women, No. (%) | 17 (52) | 22 (55) | NS |
| Body mass index | 32.6 (±7.7) | 29.9 (±5.5) | .10 |
| Diabetes mellitus, No. (%) | 1 (3) | 2 (5) | NS |
| Dyslipidemia, No. (%) | 5 (15) | 2 (5) | NS |
| Obstructive sleep apnea, No. (%) | 4 (12) | 3 (8) | NS |
| Family history of hypertension, No. (%) | 20 (61) | 26 (65) | NS |
| Tobacco use, No. (%) | 9 (27) | 7 (18) | NS |
| Alcohol use, No. (%) | 3 (9) | 2 (5) | NS |
| Coffee consumption | 1.20 (±1.2) | 0.81 (±1.0) | NS |
| Fast food intake, meals per wk | 1.1 (±1.3) | 1.3 (±1.4) | NS |
Abbreviation: NS, not significant.
Of the patients found to have masked hypertension, 16 (48%) met all criteria (daytime BP ≥140/90 mm Hg, nighttime BP ≥125/75 mm Hg, or 24‐hour BP ≥135/85 mm Hg); eight (24%) met two of the criteria, mostly daytime and 24‐hour BPs; six (18%) were nondippers, as they met only the nighttime BP; and three (9%) met only the daytime or 24‐hour BP criteria (Figure).
Figure 1.
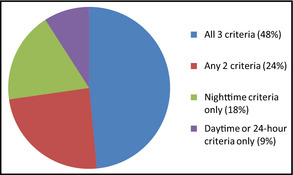
Distribution of ambulatory blood pressure criteria met by patients with masked hypertension.
Discussion
In the largest study to date conducted in African Americans, we have identified a prevalence of masked hypertension of 45.2% in our study population. This is significantly higher than what has been identified in prior population‐based studies conducted in Europe and Asia (prevalence 8.5%–15.8%). There have been few population‐based estimates of masked hypertension conducted in the United States. A study of adult employees conducted in New York reported a prevalence of 15.2%.11 This high prevalence in African Americans corroborates the findings of two previous small studies (n=38 and n=50) that enrolled only African Americans in Philadelphia.
Patients found to have masked hypertension had significantly higher SBPs than true normotensive patients (mean 124 mm Hg vs 118 mm Hg, P=.02), which is consistent with prior reports.11, 14, 15, 16 In our study, patients with masked hypertension had, on average, a larger BMI then normotensive patients (32.6 vs 29.9, P=.10). While this finding did not reach statistical significance, previous studies have identified an association between obesity and masked hypertension.15, 16, 17 While several studies have identified an association between smoking and/or daily alcohol use and masked hypertension,18, 19 we did not find an association with either. The rate of smoking was higher in our masked hypertension group (27%) than the normotensive group (18%) but this difference did not reach significance (P=.32). The overall smoking rate in our study population was 22%, which is slightly higher than the reported national rate of 18%, and likely reflects the local population.20
Patients with masked hypertension have been shown to have both a cardiovascular event and mortality rate similar to patients with sustained hypertension.5, 21 The presence of masked hypertension is associated with markers of impaired vasodilatation and endothelial dysfunction, which are early manifestations of coronary artery disease.22, 23 Thus, if our findings are representative of the general African American population, then nearly half of the African Americans who are believed to not have hypertension by office‐based measurements actually carry a cardiovascular risk comparable to those with sustained hypertension. These patients can only be identified by obtaining out‐of‐office BP measures with ambulatory or home BP monitoring. Additionally, only ambulatory monitoring will identify patients with isolated nocturnal hypertension (nondippers), which accounted for 18% of our masked hypertension population. Screening with ABPM to detect masked hypertension in untreated individuals is supported in European guidelines.24 In the United States, several professional societies have advocated for increased use and reimbursement for ABPM, although not specifically for the detection of masked hypertension.25
There is currently a lack of evidence on the best approach for detecting masked hypertension. Certainly, patients with end‐organ damage (eg, left ventricular hypertrophy and proteinuria) should be screened with 24‐hour ABPM. Ideally, these patients should be identified and treated before the development of organ damage. Patients with risk factors (eg, high‐normal SBP, obesity, smokers) should be screened, as suggested by Peacock and colleagues26 In that case, a majority of patients would qualify for screening yet we would still potentially miss many patients who truly have masked hypertension. If 45% of African Americans truly have masked hypertension, the case can be made for universal screening with ABPM in this population.
There is also a paucity of evidence to guide therapy in patients with masked hypertension. Given that these patients are at increased risk for progression to sustained hypertension,27 one approach is to closely monitor these individuals and treat once overt hypertension develops. An alternate approach would be to lower the ambulatory pressure and monitor with serial ABPM studies. Currently, we lack evidence to demonstrate that active treatment of masked hypertension improves outcomes. To date, we are not aware of any randomized trials evaluating the treatment outcomes in patients with masked hypertension.
Study Limitations
We recognize several limitations to our current study. Our population was derived from an established clinic population and thus may not reflect the general population as a whole. Additionally, these findings need to be confirmed in other geographic regions across the country. We need multicenter population‐based studies. It is notable that our cutoff values for diagnosing masked hypertension are slightly higher (about 5 mm Hg) than the most recent recommendations.4 Using the lower threshold, we would reclassify six patients from normotension to masked hypertension. Therefore, it is possible that despite how common masked hypertension was in our population, we may have underestimated the true prevalence.
Conclusions
We identified masked hypertension in 45.2% of African Americans enrolled in our ambulatory internal medicine clinic. These results need to be confirmed with population‐based studies. Further research is needed to determine the role of treatment to protect this population, which has been shown to be at increased cardiovascular risk.
Acknowledgments and disclosures
This project was funded by the research committee at Providence Hospital and Medical Center. The authors declare no conflict of interest.
J Clin Hypertens (Greenwich). 2014;16:801–804. © 2014 Wiley Periodicals, Inc.
References
- 1. O'Brien E, Asmar R, Beilin L, et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure. J Hypertens. 2005;23:697. [DOI] [PubMed] [Google Scholar]
- 2. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014;16:14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Angeli F, Reboldi G, Verdecchia P. Masked hypertension: evaluation, prognosis, and treatment. Am J Hypertens. 2010;23:941–948. [DOI] [PubMed] [Google Scholar]
- 4. Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40:795–796. [DOI] [PubMed] [Google Scholar]
- 5. Stergiou GS, Asayama K, Thijs L, et al. Prognosis of white‐coat and masked hypertension: International Database of Home Blood Pressure in Relation to Cardiovascular Outcome. Hypertension. 2014;63:675–682. [DOI] [PubMed] [Google Scholar]
- 6. Bobrie G, Clerson P, Menard J, et al. Masked hypertension: a systemic review. J Hypertens. 2008;26:1715. [DOI] [PubMed] [Google Scholar]
- 7. Imai Y, Tsuji I, Nagai K, et al. Ambulatory blood pressure monitoring in evaluating the prevalence of hypertension in adults in Ohasama, a rural Japanese community. Hypertens Res. 1996;19:207. [DOI] [PubMed] [Google Scholar]
- 8. Sega R, Trocino G, Lanzarotti A, et al. Alterations in cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population (Pressione Arteriose Monitorate e Loro Associazioni {PAMELA} study). Circulation. 2001;104:1385. [DOI] [PubMed] [Google Scholar]
- 9. Bjorklund K, Lind L, Zethelius B, et al. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation. 2003;107:1297. [DOI] [PubMed] [Google Scholar]
- 10. Alwan H, Pruijm M, Ponte B, et al. Epidemiology of masked and white‐coat hypertension: the family‐based SKIPOGH Study. PLoS One. 2014;9:e92522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shimbo D, Newman JD, Schwarz JE. Masked hypertension and prehypertension: diagnosis overlap and interrelationships with left ventricular mass: the Masked Hypertension Study. Am J Hypertens. 2012;25:664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Veerabhadrappa P, Diaz KM, Feairheller DL, et al. Enhanced blood pressure variability in a high cardiovascular risk group of African American. J Am Soc Hypertens. 2010;4:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Veerabhadrappa P, Diaz KM, Feairheller DL, et al. Endothelial‐dependent flow‐mediated dilation in African American with masked‐hypertension. Am J Hypertens. 2011;24:1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cacciolati C, Hanon O, Alperovitch A, et al. Masked hypertension in the elderly: cross‐sectional analysis of a population‐based sample. Am J Hypertens. 2011;24:674–680. [DOI] [PubMed] [Google Scholar]
- 15. Hanninen MR, Niiranen TJ, Puukka PJ, et al. Determinants of masked hypertension in the general population: the Finn‐Home study. J Hypertens. 2011;28:1880–1888. [DOI] [PubMed] [Google Scholar]
- 16. Obara T, Ohkubo T, Funahashi J, et al. Isolated uncontrolled hypertension at home and in the office amoung treated hypertensive patients from the J‐HOME study. J Hypertens. 2005;23:1653–1660. [DOI] [PubMed] [Google Scholar]
- 17. Wang GL, Li Y, Staessen JA, et al. Anthropometric and lifestyle factors associated with white‐coat, masked, and sustained hypertension in a Chinese population. J Hypertens. 2007;25:2396–2405. [DOI] [PubMed] [Google Scholar]
- 18. Verberk WJ, Kessels AGH, de Leeuw PW. Prevalence, cause, and consequences of masked hypertension: a meta‐analysis. Am J Hypertens. 2008;21:969–975. [DOI] [PubMed] [Google Scholar]
- 19. Ishikawa J, Kario K, Eguchi K, et al. Regular alcohol drinking is a determinant of masked morning hypertension detected by home blood pressure monitoring in medicated hypertensive patients with well‐controlled clinic blood pressure: the Jichi Morning Hypertension Research (J‐MORE) study. Hypertens Res. 2006;29:679–686. [DOI] [PubMed] [Google Scholar]
- 20. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics‐2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white‐coat, masked and sustained hypertension versus true normotension: a meta‐analysis. J Hypertens. 2007;25:2193–2198. [DOI] [PubMed] [Google Scholar]
- 22. Kabutoya T, Hoshide S, Ogata Y, et al. Masked hypertension defined by home blood pressure monitoring is associated with impaired flow‐mediated vasodilatation in patients with cardiovascular risk factors. J Clin Hypertens (Greenwich). 2013;15:630–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Papadopoulos DP, Mourouzis I, Faselis C, et al. Masked hypertension and atherogenesis: the impact of apelin and relaxin plasma levels. J Clin Hypertens (Greenwich). 2013;15:333–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. O'Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1768. [DOI] [PubMed] [Google Scholar]
- 25. Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society of Hypertension, and the Preventive Cardiovascular Nurses’ Association. Hypertension. 2008;52:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Peacock J, Diaz KM, Viera AJ, et al. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates, and future directions. J Hum Hypertens. 2014;28:521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mancia G, Bombelli M, Facchetti R, et al. Long‐term risk of sustained hypertension in white‐coat or masked hypertension. Hypertension. 2009;54:226–232. [DOI] [PubMed] [Google Scholar]


