Abstract
The National Heart, Lung, and Blood Institute recommends that children older than 3 years seen in the medical setting have their blood pressure (BP) measured. The authors aimed to determine whether BPs are measured at well‐child visits and whether elevated readings are recognized. A retrospective chart review of 3‐ to 18‐year‐old children seen for well‐child visits was performed. Age, sex, weight, height, BP, extremity measured, and type of intervention were collected. BP was measured in 777 of 805 patients (97%). BP was elevated in 158 patients (20%). A total of 95 patients (60%) did not receive any intervention. Not recognizing elevated BP was associated with increased daily patient load (17.9±6.5 vs 12.6±5.5, P=.001). Higher body mass index was associated with elevated BP (P=.0008) but was not associated with improved recognition. Findings show that BP is almost always measured at well‐child visits but is not being measured appropriately, and general pediatric clinics are not consistently following BP management recommendations.
The prevalence of elevated blood pressure (BP) (≥90th percentile for age, height, and sex) in the general pediatric population has been estimated to be between 3.5% and 19.2%1, 2. Elevated BP in childhood has been linked to future development of hypertension,3, 4 metabolic syndrome,5, 6 atherosclerosis,7 and cardiovascular disease.8, 9 Given the serious long‐term consequences of elevated BP in childhood, its prompt recognition, evaluation, and treatment is of the utmost importance.
The National Heart, Lung, and Blood Institute recommends that children older than 3 years, seen in the medical setting, have BP measured. Each measurement should be obtained in the right arm using an appropriately sized cuff, by auscultation. The cuff should have an inflatable bladder width that is at least 40% of the arm circumference at the midway point between the olecranon and the acromion, and the bladder length should cover 80% to 100% of the circumference of the arm. BP cuff sizes may be labeled as infant, pediatric, small adult, adult, and large adult. These descriptions are not always accurate and can be misleading to providers. If the measurement is obtained by an oscillometric device and is elevated, it should be repeated by auscultation. Elevated BP values should be confirmed on three separate occasions before a diagnosis of hypertension is made.10
Despite these guidelines, the recognition and evaluation of elevated BP readings is significantly lacking in the pediatric population. A recent study in children showed that only 20.8% of patients with elevated BP underwent repeat measurement within 1 month, and it was not significantly better in patients with obesity or stage 2 systolic elevation.11 Another demonstrated that 71% of physicians measure BP during a visit only if the child has risk factors for hypertension. Furthermore, they do not regularly compare the reading with reference tables, and their ability to classify the reading without using reference data is significantly limited.12 Physician clinic time per visit may be a limiting factor as physicians have reported for other disease states.13
We aimed to evaluate whether BPs are measured in the appropriate arm at well‐child visits, and whether elevated BPs are recognized and acted on appropriately. In addition, we aimed to evaluate whether physician workload as demonstrated by outpatient volume may play a role in lack of recognition of elevated BP.
Methods
After obtaining institutional review board approval at each site, the study was conducted in two primary care pediatric clinics at two quarternary care centers (Akron Children's Hospital Physician's Clinic [ACHPC] and Rush Pediatric Primary Care Center [RPPCC]) in the Midwest. Two sites over different dates were chosen because of the primary investigator changing institutions. A retrospective chart review was performed including 3‐ to 18‐year‐old children, seen for well‐child visits, with no documented concomitant medical conditions or medications known to affect BP. Patient age, sex, weight, height, BP reading, extremity measured, type of intervention, and number of patients seen by each provider on the given day were collected. Body mass index (BMI) was calculated from the height and weight obtained.
The data at ACHPC were collected from visits on two separate randomly chosen dates (7/14/10 and 8/27/10). The first day encompassed 16 offices with 41 providers, and the second day included 17 offices with 38 providers. The data at RPPCC were collected from visits on consecutive dates ranging from 7/2/12 to 11/7/12. This was performed at a single site with 59 providers. BP values at both centers were measured by medical assistants using an oscillometric device. RPPCC used the EpicCare electronic health record (Epic Systems Corp, Verona, WI), which automatically provided BP percentiles. ACHPC used the Allscripts electronic health record (Allscripts Healthcare Solutions, Inc., Chicago, IL), which did not provide BP percentiles.
The “intervention” was categorized into the following categories: none needed; needed and did not occur; rechecked at same visit, still elevated, and no further follow‐up; rechecked at same visit and normal; rechecked and elevated so follow‐up was planned; not rechecked but follow‐up was planned; and labs or imaging were performed. BP percentiles were calculated per the tables in the National Heart, Lung, and Blood Institute guidelines for both systolic BP (SBP) and diastolic BP (DBP). Each component of the reading was categorized as normal (<90th percentile), prehypertension (90–95th percentile or >120/80 mm Hg and <95th percentile), stage 1 hypertension (95th–99th percentile + 5 mm Hg), or stage 2 hypertension (>99th percentile + 5 mm Hg). Based on this, an overall categorization for the reading was determined. Statistical analysis was performed using JMP, version 12.1 (SAS Institute Inc., Cary, NC). Descriptive statistics were used to categorize the data. Chi‐square and Fisher exact tests were performed to assess differences in center for distribution of sex, arm measured, BP readings, and type of intervention. Mann‐Whitney U test was performed to compare demographic data between centers and to determine whether patient load or BMI affected recognition and evaluation of elevated BP. A Kruskal‐Wallis test was performed to determine whether the stage of hypertension was associated with a higher BMI.
Results
A total of 805 children were seen in the participating clinics. Four hundred and five children and 400 children were seen in the ACHPC and RPPCC clinics for well‐child visits, respectively, during the specified time frame. The demographics of the study population are shown in Table 1. Of note, there were no significant demographic differences between the populations.
Table 1.
Patient Demographics and BP Measurement Data
| ACHPC | RPPCC | All Patients | P Value | |
|---|---|---|---|---|
| Total patients, No. | 405 | 400 | 805 | |
| Age, y | 8.7±4.3 | 8.3±4.1 | 8.5±4.2 | .18 |
| Height, cm | 133.0±25.6 | 132.2±24.9 | 132.6±25.3 | .67 |
| Weight, kg | 36.9±21.5 | 37.6±22.0 | 37.2±21.7 | .72 |
| BMI, kg/m2 | 19.0±4.8 | 19.6±5.3 | 19.3±5.0 | .26 |
| Sex, m/f/u | 196/207/2 | 200/200 | 396/407/2 | .49 |
| BP taken | 393/405 | 384/400 | 777/805 | .42 |
| Arm, left/right/upper | 286/106/13a | 112/38/250 | 398/144/234 | <.0001 |
Abbreviations: ACHPC, Akron Children's Hospital Physician's Clinic; BMI, body mass index; f, female; m, male; RPPCC, Rush Pediatric Primary Care Center; u, unknown. aOne patient had blood pressure (BP) taken in the left leg. Values are expressed as mean±standard deviation where applicable.
BP measurements were not documented in 28 (3%) children. Of the 777 patients who had recorded BP, two did not have height documented, so the BP percentile could not be calculated. For the remaining patients, the measured BPs according to category separated for systolic and diastolic elevation are shown in Table 2. There were differences in the distribution of measured BP between the ACHPC and RPPCC groups for SBP (P=.02) but not for DBP (P=.07). Elevated BP was associated with a higher BMI (Table 3) (P=.0008). The measured BPs classified by highest category for systolic or diastolic BP are shown in Table 4. There was not a significant difference in distribution between centers (P=.35). Of those children who had BP values and height obtained, 617 (80%) were normal, with elevation in 158 patients. The type of intervention, if any, for patients with elevated BP measurements are shown in Figure. Ninety‐five (60%) of the 158 patients with elevated BP readings did not receive any further intervention. Of these, 58 patients had a reading that was classified as prehypertension, 34 as stage 1 hypertension, and three as stage 2 hypertension. Twenty‐four patients (15%) had their BP rechecked, and it remained elevated. Six of these had a reading that was classified as prehypertension, 15 as stage 1 hypertension, and three as stage 2 hypertension.
Table 2.
Distribution of BP Category by SBP and DBP
| ACHPC | RPPCC | All Patients | |
|---|---|---|---|
| Total patients, No. | 392 | 383 | 775 |
| Normal, SBP/DBP | 315/374 | 328/348 | 643/722 |
| Prehypertension, SBP/DBP | 43/12 | 23/21 | 66/33 |
| Stage 1, SBP/DBP | 33/5 | 27/12 | 60/17 |
| Stage 2, SBP/DBP | 1/1 | 5/2 | 6/3 |
Abbreviations: ACHPC, Akron Children's Hospital Physician's Clinic; BP, blood pressure; DBP, diastolic blood pressure; RPPCC, Rush Pediatric Primary Care Center. Statistically significant difference in distribution of systolic blood pressure (SBP) (P=.02) between centers.
Table 3.
Mean BMI by BP Category
| BMI, kg/m2 | |
|---|---|
| Normal | 18.9±4.5 |
| Prehypertension | 20.9±5.7 |
| Stage 1 | 21.6±7.1 |
| Stage 2 | 21.1±4.8 |
Values expressed as mean±standard deviation where applicable. Statistically significant difference in body mass index (BMI) by blood pressure (BP) category (P=.0008).
Table 4.
Distribution of BP Category by Highest Category
| ACHPC | RPPCC | All Patients | |
|---|---|---|---|
| Total patients, No. | 392 | 383 | 775 |
| Normal | 308 | 309 | 617 |
| Prehypertension | 47 | 37 | 84 |
| Stage 1 | 35 | 31 | 66 |
| Stage 2 | 2 | 6 | 8 |
Abbreviations: ACHPC, Akron Children's Hospital Physician's Clinic; BP, blood pressure; RPPCC, Rush Pediatric Primary Care Center.
Figure 1.
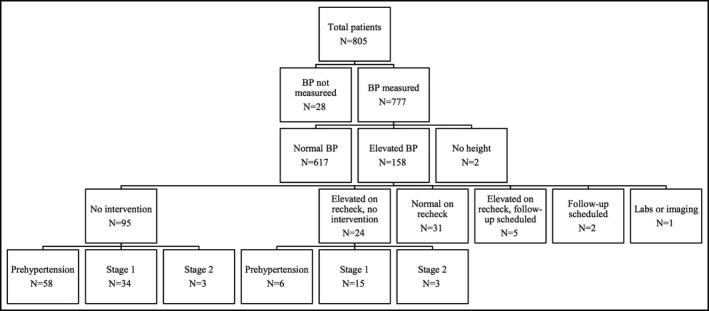
Flowchart depicting the distribution of blood pressures (BP) and intervention type.
The mean number of patients seen on a given day by providers who did not intervene for an elevated BP was 17.9±6.5 vs 12.6±5.5 for those who received some type of intervention (P=.001). A total of 9.5% of patients at ACHPC received an initial intervention after an elevated reading in comparison to 74.3% at RPPCC (P<.0001). The distribution by type of intervention is shown in Table 5. The BMI for patients who received an intervention was 21.7±6.3 vs 20.9±6.3 for those who did not receive an intervention (P=.30).
Table 5.
Distribution of Intervention by Center
| No. or No. (%) | ACHPC | RPPCC |
|---|---|---|
| Total patients | 84 | 74 |
| No intervention | 76 (91) | 19 (26) |
| Elevated on recheck, no intervention | 2 (2) | 22 (30) |
| Normal on recheck | 5 (6) | 26 (35) |
| Elevated on recheck, follow‐up scheduled | 1 (1) | 4 (5) |
| Follow‐up scheduled | 0 | 2 (3) |
| Labs or imaging | 0 | 1 (1) |
Statistically significant difference in distribution of intervention by center (P<.0001).
Discussion
As hypertension has been described as a “silent killer” and major contributor to cardiovascular disease, the identification of elevated BP becomes critical. Standardization of practice guidelines for the identification and management approach of hypertension in children were established in 2004 by an interdisciplinary group of experts.10 Our data show that primary care pediatric clinics measure BP regularly (97%) at well‐child visits. However, as others have shown,14, 15 they perform quite poorly with regard to recognizing and intervening upon elevated BP readings. In our study, 60% of patients with elevated BP values went unrecognized. If we include those patients who had their BP rechecked and remained elevated, then 75% of patients did not receive adequate intervention or follow‐up.
What is even more alarming is that BP is not being measured appropriately. BP was measured in the left arm of at least 49% of patients, and likely in more, given that the extremity measured was unknown in 29% of patients. Choosing the correct arm to measure is a relatively simple and easy task. Therefore, if the correct arm is not being measured in at least half of the patients, it can be surmised that the appropriate cuff may not be utilized either. While recognizing an elevated reading is important, making the measurement appropriately is equally as crucial. It is imperative that the entire medical team be educated on the importance of BP readings and how they should be measured.
Several factors play a role in the under‐recognition of an elevated BP reading. General pediatricians, who do not frequently diagnose or manage hypertension, may require more education on the topic. Bijlsma and colleagues12 demonstrated that pediatricians are not aware of how prehypertension or hypertension are defined and often do not use BP reference tables. Additionally, general providers do a poor job of properly classifying a reading or estimating the BP percentile, and they often underestimate the percentile.12 BP reference tables are complex and require the use of multiple variables, including sex, age, and height. Ascertaining a BP percentile can be a time‐consuming task, which may contribute to their lack of use. Our data demonstrated that there was significantly better recognition of elevated BP readings at RPPCC, which may be attributable to the electronic health record's capability to automatically provide the BP percentile. Additionally, the medical assistants at RPPCC often automatically rechecked the BP if it was elevated, which likely contributes to the large percentage of patients having their BP rechecked (70%). There was still a significant portion of patients (35%) who's BP remained elevated and who did not undergo further intervention. Adequate training of medical assistants, nursing staff, and any other medical professionals is imperative as well. Other methods that may improve recognition include a simplified screening table16 or a simple screening tool such as BP to height ratio17 that could be used to determine whether the reference tables need to be used. Further, some electronic health record systems have the capability of alerting the provider if a patient's BP is elevated. This type of “alert” can be an adjuvant tool.
It has also been shown that predictors of under‐recognition include systolic BP <120 mm Hg or diastolic BP <80 mm Hg, decreasing BMI, male sex, older age, lack of family history of cardiovascular disease, and negative medical history.18 Our data did not show improved recognition of elevated BP readings in patients with higher BMI. However, we were unable to calculate the BMI percentile, which is likely a more accurate manner to assess this association. In the aforementioned study, patient load was not associated with under‐recognition. Conversely, 34% of practitioners who were surveyed felt time constraints were a barrier to identification of elevated BPs. In our results, we found that physicians with a higher daily patient load were less likely to recognize an elevated BP reading (P=.0001).
Study Limitations
There are several limitations to this study. We were unable to assess the cuff sizes used to measure BP and how this may have impacted the measurements. Additionally, the study was performed at two centers with clinics that may be structured differently and have different parameter fields within the medical record systems. The electronic medical records were different at both institutions. The biggest and most impactful difference is likely the ability of the medical record system to provide the BP percentile. Therefore, the combined data are somewhat heterogeneous. With regard to the group of patients who had their BP rechecked, we cannot determine which member of the medical team recognized the elevated BP and rechecked it (physician, nurse, or medical assistant).
Conclusions
Our findings suggest that BPs are not being measured appropriately, and that general pediatric clinics are not consistently following management recommendations made by the Fourth Report, despite these recommendations being released several years prior.10 Possible reasons may include not referring to normative BP tables, lack of awareness of guidelines, and/or possible provider fatigue. Future interventions should focus on provider education and the use of automated electronic notifications in electronic medical records to alert providers to abnormal BPs.
Conflicts of Interest
Dr Chand is an employee and shareholder at Abbvie.
J Clin Hypertens (Greenwich). 2016;18:1230–1234. DOI: 10.1111/jch.12915. © 2016 Wiley Periodicals, Inc.
References
- 1. Rosner B, Cook NR, Daniels S, Falkner B. Childhood blood pressure trends and risk factors for high blood pressure: the NHANES experience 1988‐2008. Hypertension. 2013;62:247–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Freedman DS, Goodman A, Contreras OA, et al. Secular trends in BMI and blood pressure among children and adolescents: the Bogalusa Heart study. Pediatrics. 2012;130:e159–e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mahoney LT, Clarke WR, Burns TL, Lauer RM. Childhood predictors of high blood pressure. Am J Hypertens. 1991;4:608S–610S. [DOI] [PubMed] [Google Scholar]
- 4. Bao W, Threefoot SA, Srinivasan SR, Berenson GS. Essential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart study. Am J Hypertens. 1995;8:657–665. [DOI] [PubMed] [Google Scholar]
- 5. Sun SS, Grave GD, Siervogel RM, et al. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–246. [DOI] [PubMed] [Google Scholar]
- 6. Burns TL, Letuchy EM, Paulos R, Witt J. Childhood predictors of the metabolic syndrome in middle‐aged adults: the Muscatine study. J Pediatr. 2009;155:S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Berenson GS, Srinivasan SR, Bao W, et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart study. N Engl J Med. 1998;338:1650–1656. [DOI] [PubMed] [Google Scholar]
- 8. Li S, Chen W, Srinivasan SR, Berenson GS. Childhood blood pressure as a predictor of arterial stiffness in young adults: the Bogalusa Heart Study. Hypertension. 2004;43:541–546. [DOI] [PubMed] [Google Scholar]
- 9. McNiece KL, Gupta‐Malhotra M, Samuels J, et al. Left ventricular hypertrophy in hypertensive adolescents: analysis of risk by 2004 National High Blood Pressure Education Program Working Group staging criteria. Hypertension. 2007;50:392–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents . The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 suppl 4th report):555–576. [PubMed] [Google Scholar]
- 11. Daley MF, Sinaiko AR, Reifler LM, et al. Patterns of care and persistence after incident elevated blood pressure. Pediatrics. 2013;132:e349–e355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bijlsma MW, Blufpand HN, Kaspers GJ, Bökenkamp A. Why pediatricians fail to diagnose hypertension: a multicenter survey. J Pediatr. 2014;164:173.e7–177. e177. [DOI] [PubMed] [Google Scholar]
- 13. Olson AL, Kelleher KJ, Kemper KJ, et al. Primary care pediatricians’ roles and perceived responsibilities in the identification and management of depression in children and adolescents. Ambul Pediatr. 2001;1:91–98. [DOI] [PubMed] [Google Scholar]
- 14. Hansen ML, Gunn PW, Kaelber DC. Underdiagnosis of hypertension in children and adolescents. JAMA. 2007;298:874–879. [DOI] [PubMed] [Google Scholar]
- 15. Beacher DR, Chang SZ, Rosen JS, et al. Recognition of elevated blood pressure in an outpatient pediatric tertiary care setting. J Pediatr. 2015;166:1233.e1231–1239. e1231. [DOI] [PubMed] [Google Scholar]
- 16. Mitchell CK, Theriot JA, Sayat JG, et al. A simplified table improves the recognition of paediatric hypertension. J Paediatr Child Health. 2011;47:22–26. [DOI] [PubMed] [Google Scholar]
- 17. Outdili Z, Marti‐Soler H, Simonetti GD, et al. Performance of blood pressure‐to‐height ratio at a single screening visit for the identification of hypertension in children. J Hypertens 2014;32:1068–1074. discussion 1074. [DOI] [PubMed] [Google Scholar]
- 18. Brady TM, Solomon BS, Neu AM, et al. Patient‐, provider‐, and clinic‐level predictors of unrecognized elevated blood pressure in children. Pediatrics. 2010;125:e1286–e1293. [DOI] [PubMed] [Google Scholar]


