Abstract
Visits with nonprimary care providers such as optometrists may be missed opportunities for the detection of high blood pressure (BP). For this study, normotensive adults with at least 12 months of health plan membership on January 1, 2009 (n=1,075,522) were followed‐up for high BP through March 14, 2011. Of 111,996 patients with a BP measurement ≥140/90 mm Hg, 82.7% were measured during primary care visits and 17.3% during nonprimary care visits. Individuals with a BP ≥140/90 mm Hg measured during nonprimary care visits were older and more likely to be male and non‐Hispanic white. The proportion of patients with follow‐up and false‐positives were comparable between primary and nonprimary care. The main nonprimary care specialty to identify a first BP ≥140/90 mm Hg was ophthalmology/optometry with 24.5% of all patients. Results suggest that expanding screening for hypertension to nonprimary care settings may improve the detection of hypertension.
Hypertension affects an estimated 68 million adults (29%) in the United States and is one of the leading risk factors for cardiovascular and renal diseases.1, 2 Because it is modifiable and has very high prevalence, recognition and treatment of hypertension are important.3 Therefore, screening for high blood pressure (BP) is recommended for all adults and is a critical component in the prevention of cardiovascular disease.3
In most health‐care settings, screening, detection, and treatment for hypertension is routinely conducted in primary care.4, 5 Because hypertension is mostly asymptomatic, patients who do not proactively seek medical attention from their primary care providers may be unrecognized.
For this reason, expanding screening for hypertension to nonprimary care settings, such as optometry, orthopedics, or urology, may improve hypertension recognition and control. Integrated health‐care delivery systems have proven to be effective in increasing hypertension control by utilizing comprehensive decision support tools, such as BP measurement flag alerts when completing patient care checklists during all types of medical visits, into electronic health record (EHR) systems.6 However, the effectiveness of these tools depends on their efficiency in recognizing patients with hypertension.6, 7
The primary goal of the present study was to identify the prevalence and characteristics of patients identified with high BP in nonprimary care compared with primary care visits. The secondary goals were to investigate whether patients with an initial high BP had at least one other BP measurement within 3 months, and to examine the proportion of false‐positives after an initial elevated BP reading during nonprimary care visits compared with primary care visits.
Patients and Methods
Study Setting
This study was conducted at Kaiser Permanente Southern California (KPSC), the largest health‐care provider and integrated health‐care delivery system in Southern California. In 2009, KPSC provided health‐care services to more than 2.2 million adult members. Detailed demographic characteristics of the KPSC membership population are described elsewhere.8 Members receive care in medical offices and hospitals managed by KPSC. A comprehensive EHR system, HealthConnect, was implemented region‐wide by 2007. A system‐level, multifaceted quality improvement program for hypertension care was developed and implemented to include a comprehensive hypertension registry, use of evidence‐based clinical care guidelines that were integrated into the EHR system, a best practice reminder feature, staff performance metrics, medical assistant visits for BP measurements, and automated voice message reminders or reminder postcards to either make an appointment or walk in for a follow‐up BP in the primary or nurses care clinic, which is described in detail elsewhere.6, 7 During the study period from January 1, 2009, to March 14, 2011, screening for high BP was conducted during all patient visits in primary and nonprimary care offices. The study protocol was reviewed and approved by the institutional review board of KPSC. Informed consent was waived.
Study Design and Population
For this longitudinal study, eligible participants were normotensive members (BP <140/90 mm Hg), older than 18 years, and enrolled in a KPSC health plan for at least 12 months on January 1, 2009. A gap in health‐care coverage of <3 months in the year prior to January 1, 2009, was allowed (Figure). We identified 2,144,436 adult KPSC members on January 1, 2009, and excluded members with a history of elevated BP (≥140/90 mm Hg) during an outpatient visit, an inpatient or outpatient diagnosis code for hypertension (International Classification of Disease, Ninth Revision [ICD‐9] 401‐405 or 362.11), or a prescription for an antihypertensive medication within 24 months prior to January 1, 2009 (n=1,013,794). In addition, we excluded patients with missing BP information (n=2914), patients whose only BP measurements were from a visit indicating fever defined as body temperature ≥101.4 F (n=701), or those with BP measured in preparation for a surgery or pain management (n=3145). Lastly, patients who were pregnant during the study period (n=48,139) and patients with missing sex information (n=28) and missing visit specialty information (n=193) were also excluded. The analytical cohort of this study included 1,075,522 members who were normotensive on January 1, 2009, and eligible for follow‐up.
Figure 1.
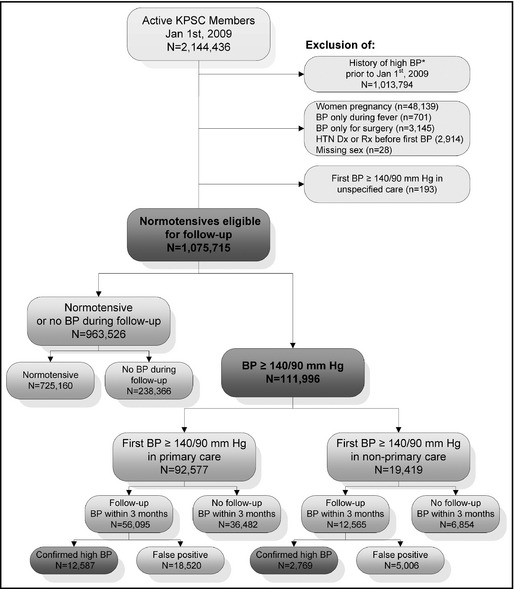
Study flow chart. *History of high blood pressure (BP) is defined as any outpatient visits with a BP ≥140/90 mm Hg, any inpatient or outpatient diagnosis (Dx) code for hypertension (HTN) defined as International Classification of Disease, Ninth Revision (ICD ‐9 401‐405 or 362.1), or any prescription (Rx) for an antihypertensive medication within 24 months prior to January 1, 2009. KPSC indicates Kaiser Permanente Southern California.
BP Measurement
BP was measured routinely at the beginning of almost every primary and nonprimary outpatient visit. The BP measurement was triggered by an alert for the nurses and medical assistants as part of a standard protocol for all outpatient visits. Nurses and medical assistants were trained according to a standard KPSC protocol using automated sphygmomanometer digital devices (Welch Allyn Connex series; Welch Allyn Inc, Skaneateles Falls, NY), which are the preferred BP measurement devices at KPSC. In some cases, wall‐mounted aneroid sphygmomanometers (Welch Allyn Inc) were used. As indicated by protocol, in cases in which BP was elevated (≥140/90 mm Hg), a second measurement was obtained. At KPSC, all staff members measuring BP were certified in BP measurement during their initial staff orientation and recertified annually––this included primary and nonprimary care staff. Staff must successfully pass a certification process that includes knowledge of preparing patients for measuring BP, selecting correct cuff size, and using standard techniques for BP measurement. In addition to the training, staff is observed by a certified trainer measuring BP to verify their competency. However, the intensity of this training may vary by medical center, and deviations of the preferred measurement method may have occurred.
Primary and Secondary Study Outcomes
The primary study outcome was an initial BP ≥140/90 mm Hg during a primary or nonprimary care outpatient visit. Among those with a BP ≥140/90 mm Hg during follow‐up, a secondary outcome of BP follow‐up within 3 months of the initial elevated BP was analyzed. We classified those patients as having (1) confirmed high BP if they had another BP ≥140/90 mm Hg within 3 months or (2) false‐positives if they had normal BP after their initial BP ≥140/90 mm Hg (Figure).
Cohort Follow‐Up
All patients were followed through March 14, 2011. Patients with BP ≥140/90 mm Hg were additionally followed through June 30, 2013, through regular linkage of information extracted from the EHR. For the primary outcome analysis, follow‐up time was calculated from January 1, 2009 (baseline), until the first occurrence of one of the following events: BP ≥140/90 mm Hg, end of KPSC health‐care coverage, death, or the end of follow‐up in March 14, 2011. For the secondary outcome analysis among patients with a BP ≥140/90 mm Hg, we calculated the follow‐up time from the date of the first elevated BP until one of the following events: occurrence of an additional BP measurement, end of KPSC health‐care coverage, death, or the end of follow‐up in June 30, 2013.
Classification of Specialty Care vs Primary Care Visits
Visits were classified as primary care visits when they occurred with providers in family care, cardiology, endocrinology, internal medicine (without infectious disease care), obstetrics and gynecology, or pediatrics. In KPSC, obstetrics and gynecology visits are considered primary care visits because they follow similar standard‐of‐care protocols. Visits were defined as nonprimary care (specialty) visits when they occurred in settings specific to allergology and immunology, dermatology, gastroenterology with hepatology, hematology, infectious disease care, mental health including social services and addiction medicine, neurology, occupational medicine, ophthalmology and optometry, pain management, and physical medicine including podiatry, pulmonology, rheumatology, urology, and others. Visits to the emergency department, urgent care, pain management, and visits with the primary purpose of surgical preparation were not included.
Statistical Analysis
Summary statistics were calculated for sociodemographic characteristics, Framingham risk score,9 chronic disease status (diabetes, cardiovascular disease, chronic kidney disease), and smoking status at baseline on January 1, 2009. Percentages were calculated for categorical variables and differences in characteristics were assessed using chi‐square tests.
We examined the associations of a high BP in nonprimary care vs primary care after adjusting for demographic characteristics and baseline risk factors (diabetes, cardiovascular disease risk calculated as Framingham 10‐year risk score, coronary artery disease, chronic kidney disease, and smoking), using log‐binomial regression models to estimate the relative risk (RR) and corresponding 95% confidence intervals (CIs). For individuals with a BP ≥140/90 mm Hg, the same models were used to examine the association of having a follow‐up BP within 3 months after the initial BP ≥140/90 mm Hg. For individuals with a BP ≥140/90 mm Hg and at least one follow‐up visit, the association of having normal BP during follow‐up visits (false‐positives) by demographic characteristics and baseline risk factors was examined. In order to detect the possible interactions between demographic characteristics and baseline risk factors on high BP identified in a nonprimary care contact, we used two log‐binomial regression models: (a) the multivariable model stratified by age, sex, race, body mass index (BMI; weight in kg/height in m2), and baseline risk factors; (b) additionally including two‐way interaction terms into the model. RRs and CIs were calculated. All analyses were performed using SAS statistical software version 9.3 (SAS Institute Inc, Cary, NC).
Results
The mean (standard deviation [SD]) ages at baseline and at end of follow‐up for the primary outcome were 39.7 (13.9) and 41.5 (14.0) years, respectively. The total cohort (n=1,075,522) was nearly equally representative of both men (48.6%) and women (51.4%). The majority of the patients (91.7%) were younger than 60 years. A large proportion of the cohort belonged to racial/ethnic minorities with 33.1% Hispanics, 6.5% blacks, and 8.4% Asian/Pacific Islander (Table 1). The total cohort (N=1,075,522) had 4,903,200 office visits, of which 3,996,190 were primary care visits, 901,275 nonprimary care visits, and 5735 visits of unknown specialty (ratio primary to nonprimary care visits 4.4:1).
Table 1.
Baseline Demographic and Clinical Characteristics of Patients With a Blood Pressure (BP) ≥140/90 mm Hg Documented During a Primary Care Visit and a Nonprimary Visit Compared With Patients Who Were Normotensive or Had No BP Measurement Taken During the Study Period
| Variable | Total | BP <140/90 mm Hg or no BP | First BP ≥140/90 mm Hg | |
|---|---|---|---|---|
| Primary Care | Nonprimary Care | |||
| Total | 1,075,522 | 963,526 | 92,577 | 19,419 |
| Sex | ||||
| Men | 48.6 | 48.0 | 52.7 | 57.3 |
| Women | 51.4 | 52.0 | 47.3 | 42.7 |
| Age group, y | ||||
| 18–29 | 27.4 | 29.0 | 14.0 | 9.4 |
| 30–39 | 23.2 | 23.8 | 19.1 | 12.9 |
| 40–49 | 24.5 | 24.2 | 27.9 | 23.2 |
| 50–59 | 16.6 | 15.7 | 24.0 | 28.2 |
| ≥60 | 8.3 | 7.3 | 14.9 | 26.3 |
| Race/ethnicity | ||||
| Non‐Hispanic white | 29.3 | 28.3 | 36.6 | 46.7 |
| Hispanic | 33.1 | 33.3 | 31.9 | 25.6 |
| African American | 6.5 | 6.3 | 8.5 | 7.8 |
| Asian/Pacific Islander | 8.4 | 8.4 | 8.1 | 8.3 |
| Other/unknown | 22.7 | 23.7 | 14.9 | 11.5 |
| Body mass index, kg/m2 | ||||
| Missing | 22.7 | 25.3 | 0.5 | 1.7 |
| <18.5 | 1.2 | 1.2 | 0.7 | 1.0 |
| 18.5–24.9 | 26.8 | 27.6 | 19.8 | 24.4 |
| 25.0–29.9 | 28 | 27.1 | 35.7 | 38.5 |
| 30.0–34.9 | 13.8 | 12.6 | 24.8 | 22 |
| 35.0–39.9 | 4.9 | 4.3 | 11 | 8.2 |
| ≥40 | 2.4 | 1.9 | 7.5 | 4.3 |
| Framingham 10‐year risk scorea ≥20% | 4.7 | 3.3 | 15.7 | 19.4 |
| Diabetes, % | 1.5 | 1.4 | 2.7 | 2.3 |
| Chronic kidney disease, % | 0.2 | 0.2 | 0.3 | 0.7 |
| Coronary artery disease, % | 0.2 | 0.2 | 0.4 | 0.7 |
| Ever smoked, % | 19.4 | 18.9 | 22.5 | 28.3 |
Data are expressed as percentage or mean±standard deviation. aBased on D'Agostino et al9
During 1,673,193 person‐years of follow‐up (mean follow‐up, 1.6 years; SD, 0.8), we documented 111,996 patients with a BP ≥140/90 mm Hg, of which 1736 had a BP ≥180/110 mm Hg. Patients with high BP were older, more likely to be male, to have a Framingham risk score ≥20% or chronic health conditions, and more likely to smoke when compared with patients who were normotensive (Table 1). About 55% of patients in all groups had a primary care visit within 12 months prior to their first BP, or first elevated BP, or 12 months prior to study baseline for those without BP during follow‐up. An initial BP ≥140/90 mm Hg was confirmed within 3 months in 15,356 patients.
Of 111,996 patients with a BP ≥140/90 mm Hg, 92,577 (82.7%) were measured during primary care visits and 19,419 (17.3%) patients during nonprimary care visits (ratio of primary care to nonprimary care, 4.8:1). Of 15,356 patients with confirmed high BP, 12,587 (82.0%) were measured during primary care visits and 2769 (18.0%) patients during nonprimary care visits (ratio of primary care to nonprimary care, 4.5:1).
Patients with a BP ≥140/90 mm Hg measured during nonprimary care visits were older and more likely to be male and non‐Hispanic white and less likely to be obese (defined as a BMI ≥30 kg/m2), but more likely to smoke or have a Framingham risk score ≥20% (Table 1). Among patients with a BP ≥140/90 mm Hg measured during primary care visits, 36.2%, 13.8%, 15.6%, and 34.4%, respectively, did not have a BP 0 to 3 months, 3 to 6 months, 6 to 12 months, and more than 12 months before the BP ≥140/90 mm Hg compared with 66.9%, 10.4%, 9.1%, and 13.6%, respectively, with a BP ≥140/90 mm Hg measured during nonprimary care visits (P<.0001). The main nonprimary care specialties to identify a first BP ≥140/90 mm Hg were ophthalmology/optometry with 24.5%, neurology with 19.0%, and dermatology with 13.1% (Table 2). In comparison, 21.2% of nonprimary care visits in participants with normal BP occurred in ophthalmology/optometry, 20.9% in neurology, and 13.2% in dermatology.
Table 2.
Distribution of Patients With a First Blood Pressure ≥140/90 mm Hg During Follow‐Up and Their Visits by Corresponding Health‐Care Setting
| Health‐Care Setting | Patients With a First Blood Pressure ≥140/90 mm Hg |
|---|---|
| All visits | 111,996 (100) |
| Primary care visits | 92,577 (82.7) |
| Family practice | 67,614 (73.0) |
| Cardiology, endocrinology, internal medicine | 21,335 (23.1) |
| Obstetrics and gynecology | 3593 (3.9) |
| Pediatricsa | 35 (0.1) |
| Nonprimary care visits | 19,419 (17.3) |
| Ophthalmology/optometry | 4757 (24.5) |
| Neurology | 3694 (19.0) |
| Dermatology | 2546 (13.1) |
| Gastroenterology and hepatology | 2252 (11.6) |
| Occupational medicine | 1484 (7.6) |
| Urology | 1323 (6.8) |
| Physical medicine/podiatry | 1177 (6.1) |
| Mental health, social services, and addiction medicine | 712 (3.7) |
| Rheumatology | 435 (2.2) |
| Allergology/immunology | 338 (1.7) |
| Other nonprimary care visits | 257 (1.3) |
| Pulmonary disease | 239 (1.2) |
| Infectious diseases | 205 (1.1) |
Values are expressed as number (percentage). aMembers transitioning into adulthood can continue to see their pediatrician in special cases after turning 18 years of age.
Of 1736 patients with a BP ≥180/110 mm Hg, 1497 (86.2%) were measured during primary care visits and 239 (13.8%) patients during nonprimary care visits (ratio of primary care to nonprimary care, 6.3:1). Among patients with a BP ≥180/110 mm Hg measured during primary care visits, 12.5%, 3.6%, 5.5%, and 78.4%, respectively, did not have a BP 0 to 3 months, 3 to 6 months, 6 to 12 months, and more than 12 months before the BP ≥180/110 mm Hg compared with 31.0%, 7.1%, 4.2%, and 57.7%, respectively, with a BP ≥180/110 mm Hg measured during nonprimary care visits (P<.0001). The main nonprimary care specialties to identify a first BP ≥180/110 mm Hg were ophthalmology/optometry with 47.3% and neurology with 11.7%, followed by dermatology with 9.2%. In comparison, 26.1% of nonprimary care visits in participants with normal BP occurred in ophthalmology/optometry, 14.2% in neurology, and 9.8% in dermatology (data not shown).
In multivariable analyses, patients with a first BP ≥140/90 mm Hg during nonprimary care visits were more likely to be male, older, and non‐Hispanic whites compared with patients with a first BP ≥140/90 mm Hg during primary care visits (Table 3). They also had a lower BMI and were more likely to smoke and have chronic kidney disease but less likely to have diabetes. The RRs were essentially the same when restricting to individuals with first BP ≥140/90 mm Hg who had a subsequent follow‐up BP ≥140/90 mm Hg (confirmed high BP).
Table 3.
Relative Risks for Detection of a First BP ≥140/90 mm Hg During Nonprimary Care Visits Compared With Primary Care Visits by Patient Demographics
| Variables | First BP ≥140/90 mm Hg | ||
|---|---|---|---|
| All | Confirmed High BP | False Positivesa | |
| Sex | |||
| Male | Reference | Reference | Reference |
| Female | 0.78 (0.76, 0.81) | 0.84 (0.78, 0.90) | 1.06 (1.04, 1.07) |
| Age at baseline, y | 1.19 (1.18, 1.20) | 1.12 (1.09, 1.15) | 0.97 (0.97, 0.98) |
| Race/ethnicity | |||
| Non‐Hispanic white | Reference | Reference | Reference |
| Hispanic | 0.80 (0.77, 0.82) | 0.89 (0.81, 0.96) | 1.02 (1.01, 1.03) |
| African American | 0.88 (0.84, 0.92) | 0.84 (0.74, 0.95) | 0.97 (0.95, 0.99) |
| Asian/Pacific Islander | 0.87 (0.83, 0.91) | 0.92 (0.81, 1.04) | 1.00 (0.98, 1.02) |
| Other/unknown | 0.70 (0.67, 0.74) | 0.66 (0.58, 0.76) | 1.00 (0.98, 1.02) |
| BMI at baseline, kg2/m2 | 0.91 (0.90, 0.92) | 0.90 (0.87, 0.92) | 0.98 (0.97, 0.98) |
| Smoking status | |||
| No | Reference | Reference | Reference |
| Yes | 1.18 (1.15, 1.22) | 1.24 (1.15, 1.34) | 1.03 (1.01, 1.04) |
| Diabetes | |||
| No | |||
| Yes | 0.84 (0.77, 0.91) | 0.91 (0.73, 1.14) | 1.06 (1.03, 1.09) |
| Chronic kidney disease | |||
| No | Reference | Reference | Reference |
| Yes | 1.38 (1.21, 1.57) | 1.2 (0.81, 1.76) | 1.06 (0.99, 1.14) |
| Coronary artery disease | |||
| No | Reference | Reference | Reference |
| Yes | 1.02 (0.89, 1.17) | 1.06 (0.7, 1.59) | 1.12 (1.06, 1.18) |
False‐positives are defined as patients with a BP ≥140/90 mm Hg who had normal BP during follow‐up.
The demographic characteristics of patients with a first BP ≥140/90 mm Hg measured during a nonprimary care visit varied by specialty (Table 4). Patients identified during an ophthalmology or optometry visit tended to be older and less likely to have a primary care visit within the past 12 months compared with those from other specialties. Patients identified at urology visit were more likely to be male, patients identified in physical medicine were more likely to be female, and patients from occupational medicine were more likely to be from a racial/ethnic minority but less likely to have a primary care visit within the past 12 months compared with other specialties.
Table 4.
Demographics of Patients With a Detected Blood Pressure ≥140/90 mm Hg During the Most Frequently Represented Nonprimary Care Visits
| Variables | Ophthalmology/Optometry | Neurology | Dermatology | Gastroenterology/Hepatology | Occupational Medicine | Urology | Physical Medicine/Podiatry |
|---|---|---|---|---|---|---|---|
| Total | 4757 | 3694 | 2546 | 2252 | 1484 | 1323 | 1177 |
| Sex | |||||||
| Men | 53.9 | 57.6 | 59.3 | 55.3 | 54.8 | 86.5 | 52.6 |
| Women | 46.1 | 42.4 | 40.7 | 44.7 | 45.2 | 13.5 | 47.4 |
| Age group, y | |||||||
| 18–29 | 6.7 | 12.2 | 9.1 | 4.2 | 11.6 | 8.8 | 6.5 |
| 30–39 | 8.4 | 14.8 | 11.5 | 7.7 | 21.4 | 15.3 | 16.4 |
| 40–49 | 20.2 | 24.3 | 20.9 | 20.7 | 31.9 | 21 | 27.9 |
| 50–59 | 26.5 | 27.6 | 30.1 | 37.5 | 25.3 | 26.3 | 29.2 |
| ≥60 | 38.2 | 21.1 | 28.4 | 29.9 | 9.8 | 28.5 | 20 |
| Race/ethnicity | |||||||
| Non‐Hispanic white | 41.3 | 49.2 | 58.1 | 49.3 | 32.1 | 44.3 | 50.6 |
| Hispanic | 26.5 | 27.4 | 16.9 | 22.7 | 35.6 | 29.6 | 21.3 |
| African American | 7.4 | 8.1 | 3.8 | 8.6 | 10.4 | 9.4 | 9.3 |
| Asian/Pacific Islander | 11.3 | 7.1 | 6 | 9.3 | 9.3 | 5.9 | 6.8 |
| Other/unknown | 13.5 | 8.2 | 15.2 | 10 | 12.6 | 10.9 | 12 |
| Body mass index, kg/m2 | |||||||
| Missing | 5.1 | 0.2 | 1.1 | 0.1 | 0.9 | 0.8 | 0.3 |
| <18.5 | 1 | 0.8 | 0.7 | 1.2 | 0.6 | 0.5 | 0.3 |
| 18.5–24.9 | 25.1 | 22.3 | 26 | 29 | 20.6 | 20.3 | 22.1 |
| 25.0–29.9 | 37.7 | 38.2 | 39.9 | 36.5 | 35.6 | 46 | 41.3 |
| 30.0–34.9 | 20.1 | 23.4 | 21.4 | 23.1 | 26 | 21.8 | 23 |
| 35.0–39.9 | 7.3 | 9.6 | 6.7 | 7.3 | 10.4 | 7.9 | 8.8 |
| ≥40 | 3.7 | 5.5 | 4.1 | 2.7 | 5.8 | 2.7 | 4.2 |
| Framingham 10‐year risk score ≥20% | 23.5 | 14.8 | 20.4 | 23 | 11.4 | 31.8 | 16 |
| Diabetes, % | 3 | 2 | 1.4 | 2.7 | 2.3 | 2.2 | 2.1 |
| Chronic kidney disease, % | 0.5 | 0.6 | 0.6 | 0.8 | 0.4 | 0.8 | 0.8 |
| Coronary artery disease | 0.8 | 0.6 | 0.7 | 0.9 | 0.5 | 1 | 0.8 |
| Ever smoked | 23.3 | 28.4 | 28.2 | 30.5 | 23 | 30.1 | 37.5 |
The follow‐up after a first elevated BP was marginally higher in patients identified in nonprimary care than in primary care (Table 5). Among patients with a first BP ≥140/90 mm Hg measured during a primary care visit (n=92,577), 60.6% (n=56,095) of individuals had a follow‐up BP within 3 months of the first high BP, 22.9% (n=21,228) after 3 months or more, and 16.5% (n=15,254) did not have a follow‐up BP. Among individuals with a first BP ≥140/90 mm Hg measured during a nonprimary care visit (n=19,419), 64.7% (n=12,565) of individuals had a follow‐up BP within 3 months of the first high BP, 22.6% (n=4389) after 3 months or more, and 12.7% (n=2495) did not have a follow‐up BP measurement (follow‐up within 3 months for primary vs nonprimary care; P<.001). The average time between a specialty care visit and the next primary care visit was 97 days (SD, 116 days) in individuals with a first high BP in primary care, 117 days (SD, 134 days) in individuals with a first high BP in nonprimary care, and 119 days (SD, 131 days) in individuals with normal or no BP (P<.0001).
Table 5.
Distribution of Patients With a First Blood Pressure (BP) ≥140/90 mm Hg and Who Received Follow‐Up Attention Within 3 Months of Initial High BP and Those Identified as False‐Positive by Corresponding Health‐Care Setting
| Health‐Care Setting | Frequency, % | ||
|---|---|---|---|
| BP ≥140/90 mm Hg | Follow‐up Within 3 moa | False‐Positivesa | |
| All visits | 111,996 | ||
| Primary care visits | 92,577 | 56,095 (60.6) | 18,520 (33.0) |
| Family practice | 67,614 | 40,703 (60.2) | 13,542 (33.3) |
| Cardiology, endocrinology, internal medicine | 21,335 | 12,999 (60.9) | 4,038 (31.1) |
| Obstetrics and gynecology | 3593 | 2372 (66.0) | 933 (39.3) |
| Pediatricsb | 35 | 21 (60.0) | 7 (33.3) |
| Nonprimary care visits | 19,419 | 12,565 (64.7) | 5006 (39.8) |
| Ophthalmology/optometry | 4757 | 2874 (60.4) | 971 (33.8) |
| Neurology | 3694 | 2673 (72.4) | 1216 (45.5) |
| Dermatology | 2546 | 1473 (57.9) | 522 (35.4) |
| Gastroenterology and hepatology | 2252 | 1239 (55.0) | 480 (38.7) |
| Occupational medicine | 1484 | 1130 (76.1) | 486 (43.0) |
| Urology | 1323 | 817 (61.8) | 316 (38.7) |
| Physical medicine/podiatry | 1177 | 807 (68.6) | 348 (43.1) |
| Mental health, social services, and addiction medicine | 712 | 517 (72.6) | 215 (41.6) |
| Rheumatology | 435 | 308 (70.8) | 141 (45.8) |
| Allergology/immunology | 338 | 214 (63.3) | 83 (38.8) |
| Other nonprimary care visits | 257 | 192 (74.7) | 95 (49.5) |
| Pulmonary disease | 239 | 173 (72.4) | 76 (43.9) |
| Infectious diseases | 205 | 148 (72.2) | 57 (38.5) |
Percentage based on the column “First BP ≥140/90 mm Hg” as 100%.
Members transitioning into adulthood can continue to see their pediatrician in special cases after turning 18 years of age.
The proportion of false‐positives, defined as individuals with an initial BP ≥140/90 mm Hg who had a follow‐up visit with a normal BP within 3 months, was essentially the same for patients identified in primary or nonprimary care, with 81.4% of false‐positives (n=5006) identified during a nonprimary care visit and 79.8% of false‐positives (n=18,520) identified during a primary visit (Table 5). False‐positives were most frequent in individuals identified during visits in other specialty care, rheumatology, and neurology fields.
Discussion
In this large population‐based study within a managed care setting, 17% of all patients with an initial high BP were identified during nonprimary care visits. Patients with an initial high BP during nonprimary care were older and more likely to be non‐Hispanic white and male, to smoke, and to have chronic kidney disease but less likely to be obese compared with those with an initial high BP during a primary care visit. After an initial high BP, follow‐up within 3 months was slightly better in patients identified during nonprimary care compared with those during primary care visits while the proportion of patients who had normal BP during follow‐up (false‐positives) was comparable.
Interventions to improve control of BP in patients with hypertension require successful identification as the first step.4 Differences in health‐care service utilization and type of care providers may affect the recognition, diagnosis, and awareness of hypertension. Hypertensive individuals with a routine place of care demonstrate a higher awareness of hypertension than those without a routine place of care (85% vs 66%).10 The standard point of care for hypertension diagnosis is primary care,4, 5 but some patients may not have regular visits with their primary care providers because of the asymptomatic nature of the condition, and thus continue for years without being diagnosed or treated.11 However, some of these patients may interact with specialty care providers. In 1994, Harris reported 40% of optometry patients had not had a complete physical examination in more than 5 years and speculated that optometrists might treat vision problems of hypertensive patients while ignoring high BP, which might, in turn, have affected the health of the eye.12 For patients with psoriasis who have a higher cardiovascular risk, screening for high BP and other cardiovascular risk factors is recommended, but dermatologists rarely screen for these risk factors.13 Based on 2005–2009 data from the National Ambulatory Medical Care Survey, only 2.6% of patients with psoriasis and 6.1% of patients without psoriasis were screened for high BP compared with 89.9% of patients with psoriasis and 60.8% of patients without psoriasis.13 However, that study does not provide information on the proportion of patients who were identified with high BP in different specialties. Nonprimary care may, therefore, be missing the opportunity to identify patients with increased BP as suggested by the significant proportion of patients (17%) in the present study who were identified as having high BP during nonprimary care visits, especially during ophthalmology/optometry and neurology visits.
On the other hand, false‐positives are a concern because of the time and resource costs for both patients and health‐care systems in making additional and perhaps unnecessary appointments when an elevated BP is found. Our study suggests that many patients (82%) identified with an initial high BP––in primary care as well as in nonprimary care––cannot be confirmed as patients with high BP in subsequent visits. The proportion of false‐positives was comparable between primary and nonprimary care, suggesting that identifying patients with high BP in this setting did not increase the proportion of false‐positives. However, it will increase the absolute number of false‐positives––patients who require follow‐up and do not have hypertension.
To minimize false‐positives, the identification of high BP in nonprimary care required the training of staff in nonprimary care in using standard techniques for BP measurement. At KPSC, all staff members measuring BP were certified in BP measurement during their initial staff orientation and recertified annually––this includes primary and nonprimary care staff.
Study Limitations
As a potential limitation, the present study was conducted observing a system‐wide change and does not include control clinics in which BP measurements in nonprimary care were rolled out at a different point in time. We do not know when a high BP would have been detected without BP measurements in nonprimary care. Hence, our ability to assess the magnitude of the potential benefit of expanding screening for hypertension to nonprimary care settings is limited. Since many patients with high BP measured during a nonprimary care visit (13.6% of patients ≥140/90 mm Hg and 57.7% of patients ≥180/110 mm Hg) did not have BP assessed within the past 12 months on record, expanding screening for hypertension to nonprimary care settings may improve early hypertension recognition and control, especially for patients with very high BP. The average time between a specialty care visit and the next primary care visit was more than 5 months, indicating that a significant amount of time may have passed until the next opportunity to measure BP.
Patients with high BP identified in nonprimary care differed in their demographics and characteristics from those identified in primary care. Patients identified in nonprimary care were generally older and more likely to be non‐Hispanic white and male, to smoke, and to have chronic kidney disease, but were less likely to be obese compared with those identified in primary care settings. The differences in demographics observed in our study suggest that expanding screening for hypertension to nonprimary care settings may also help identify patients who would have been missed otherwise.
Detection of high BP requires an adequate follow‐up by primary care physicians to determine whether hypertension is present and whether further action such as surveillance or treatment is required. It is of concern that patients with a first high BP in nonprimary care may have lower follow‐up rates than those with a first high BP in primary care. The present study was performed within an integrated health‐care delivery system after conducting a system‐level, multifaceted quality improvement program for hypertension that included comprehensive decision support tools embedded in the EHR system such as BP measurement flag alerts when completing patient care checklists during all types of medical visits.6 The program also included follow‐up with patients with high BP using reminder phone calls managed centrally.7 Patients detected in nonprimary care also received help to schedule a follow‐up appointment at the time of their visit. Consequently, the proportion of patients with high BP with a follow‐up visit was overall relatively high (>60%) and comparable between primary care and nonprimary care.
The quality of BP measurements made in nonprimary care visits are a concern but can be addressed by regular training of staff responsible for BP measurements. The proportion of false‐positives defined as individuals with an initial high BP and normal BP during follow‐up visits was essentially the same for primary and nonprimary care. However, some nonprimary care specialties such as gastroenterology and hepatology showed slightly higher proportions of false‐positives, which may be explained by the nature of the conditions leading to the specialty care visit.
Conclusions
The present study suggests that expanding screening for hypertension to nonprimary care settings may improve the detection of hypertension and can contribute to hypertension control. However, the approach requires an effective system to ensure appropriate follow‐up if high BP is detected. The benefit may be highest for older, non‐Hispanic white, and male patients and those with very high BP.
Disclosures
This research was supported by Kaiser Permanente Direct Community Benefit Funds. There are no other conflicts of interest to disclose.
Acknowledgments
None.
J Clin Hypertens (Greenwich). 2015;17:431–439. DOI: 10.1111/jch.12517. © 2015 Wiley Periodicals, Inc.
References
- 1. Centers for Disease Control and Prevention (CDC) . Vital signs: prevalence, treatment, and control of hypertension–United States, 1999‐2002 and 2005‐2008. MMWR Morb Mortal Wkly Rep. 2011;60:103–108. [PubMed] [Google Scholar]
- 2. Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. [DOI] [PubMed] [Google Scholar]
- 3. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 4. Glynn LG, Murphy AW, Smith SM, et al. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010:CD005182. [DOI] [PubMed] [Google Scholar]
- 5. McManus RJ, Mant J. Management of blood pressure in primary care. BMJ. 2009;338:b940. [DOI] [PubMed] [Google Scholar]
- 6. Sim JJ, Handler J, Jacobsen SJ, Kanter MH. Systemic implementation strategies to improve hypertension: the Kaiser Permanente Southern California experience. Can J Cardiol. 2014;30:544–552. [DOI] [PubMed] [Google Scholar]
- 7. Harrison TN, Ho TS, Handler J, et al. A randomized controlled trial of an automated telephone intervention to improve blood pressure control. J Clin Hypertens (Greenwich). 2013;15:650–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Koebnick C, Langer‐Gould AM, Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16:37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. D'Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–753. [DOI] [PubMed] [Google Scholar]
- 10. Angell SY, Garg RK, Gwynn RC, et al. Prevalence, awareness, treatment, and predictors of control of hypertension in New York City. Circ Cardiovasc Qual Outcomes. 2008;1:46–53. [DOI] [PubMed] [Google Scholar]
- 11. Trilling JS, Froom J. The urgent need to improve hypertension care. Arch Fam Med. 2000;9:794–801. [DOI] [PubMed] [Google Scholar]
- 12. Harris MG, Gan CM, Revelli EJ, et al. Blood pressure measurement by eye care practicioners. J Am Optom Assoc. 1994;65:512–516. [PubMed] [Google Scholar]
- 13. Alamdari HS, Gustafson CJ, Davis SA, et al. Psoriasis and cardiovascular screening rates in the United States. J Drugs Dermatol. 2013;12:e14–e19. [PubMed] [Google Scholar]


