Abstract
Electronic health record data were analyzed to estimate the number of statin‐eligible adults with the 2013 American College of Cardiology/American Heart Association cholesterol guidelines not taking statin therapy and the impact of recommended statin therapy on 10‐year atherosclerotic cardiovascular disease (ASCVD10) events. Adults aged 21 to 80 years in an outpatient network with ≥1 clinic visit(s) from January 2011 to June 2014 with data to calculate ASCVD10 were eligible. Moderate‐intensity statin therapy was assumed to lower low‐density lipoprotein cholesterol by 30% and high‐intensity therapy was assumed to reduce low‐density lipoprotein cholesterol by 50%. ASCVD events were assumed to decline 22% for each 39 mg/dL decline in low‐density lipoprotein cholesterol. Among 411,768 adults, 260,434 (63.2%) were not taking statins and 103,478 (39.7%) were eligible for a statin, including 79,069 (76.4%) patients with hypertension. Estimated ASCVD10 events were 18,781 without and 13,328 with statin therapy, a 29.0% relative and 5.3% absolute risk reduction with a number needed to treat of 19. The 2013 cholesterol guidelines are a relatively efficient approach to reducing ASCVD in untreated, statin‐eligible adults who often have concomitant hypertension.
Hypercholesterolemia is a major, modifiable risk factor for atherosclerotic cardiovascular disease (ASCVD) events.1, 2 Statins are evidence‐based first‐line therapy for primary and secondary prevention of ASCVD.1, 2 The 2013 American College of Cardiology/American Heart Association (ACC/AHA) cholesterol guidelines would treat approximately 12.8 million more adults for hypercholesterolemia than those proposed by the Third Report of the Adult Treatment Panel III (ATP III) of the National Cholesterol Education Program (NCEP) guideline, based on extrapolations from a representative sample of the US population.3 This observation suggests that population cardiovascular health could be significantly improved by implementing the 2013 guidelines.2
Cardiovascular health is critically important in the United States, where the population is aging and with increasing proportions of racially and ethnically diverse groups with greater cardiometabolic risk.4, 5 These population and demographic changes are projected to increase costs for cardiovascular care in the United States from $460 billion in 2010 to $1.1 trillion by 2030 in constant 2008 dollars.6 In the United States, the Southeast has higher rates of cardiovascular mortality than other regions of the country. Within the Southeast, South Carolina led the nation in stroke mortality in all but one decade from the 1930s through the 1990s.7 In 1995, South Carolina was 50th among US states and the District of Columbia in age‐adjusted cardiovascular mortality. Between 1995 and 2011, South Carolina had a larger improvement in cardiovascular mortality rank than other southeastern States, rising from 50th to 34th.8
To explore the potential for preventing even more cardiovascular events, data were analyzed from diverse, community‐based practice settings across South Carolina. The proportion of statin‐eligible adults was estimated for individuals not currently taking statin therapy using both the updated NCEP/ATP III and 2013 cholesterol guidelines.3, 4, 9 The reduction in ASCVD events was also calculated using the 10‐year ASCVD risk (ASCVD10) calculator included in the newer guideline and the number needed to treat (NNT) over 10 years to prevent an ASCVD event was estimated.
Methods
Patients
This study used electronic health record system data of patients seen at approximately 350 clinical sites in the Care Coordination Institute Quality Improvement Network.10 Each clinical group signed an approved Business Associate Agreement, which addresses provisions of the Health Insurance Portability and Accountability Act and the HiTech 2009 amendment. The authorized agreement permits use of de‐identified data for research. In addition, the analysis for this report was approved by the Office of Human Research Protection, University of South Carolina School of Medicine, Greenville, South Carolina.
Inclusion and Exclusion Criteria
The primary analysis included adults aged 21 to 80 years with a minimum of one valid blood pressure (BP) measurement, lipid profile, and medication for any disease state as well as cigarette smoking, cardiovascular disease, and diabetes status, between January 1, 2011, and June 30, 2014. Exclusion criteria were limited to failure to meet any inclusion criteria, congestive heart failure, and estimated glomerular filtration rate <15 mL/1.73 m2/min, ie, stage 5 chronic kidney disease (CKD).
Operational Definitions
BP at the last (most recent) visit was used to calculate ASCVD10 risk and to assess hypertension control. A valid BP was defined as a systolic BP of 60 mm Hg to 300 mm Hg, a diastolic BP of 30 mm Hg to 240 mm Hg, and systolic BP greater than diastolic BP. The BP value included was the mean of values recorded for that visit or the single value if only one was recorded. BP control was defined as <140/<90 mm Hg for all patients, including those with diabetes mellitus and CKD as well as patients 60 years and older.
Lipoprotein Cholesterol Values
Low‐density lipoprotein cholesterol (LDL‐C) was calculated as total cholesterol − [high‐density lipoprotein cholesterol (HDL‐C) + triglycerides / 5].11 If triglycerides were >400 mg/dL, then LDL‐C was not calculated.11 A valid LDL‐C value was defined by a range of 20 mg/dL to 700 mg/dL. Non–HDL‐C was calculated as total cholesterol − HDL‐C. A valid HDL‐C value was defined by values of 2 mg/dL to 140 mg/dL.
Defining Statin‐Eligible Adults
Statin eligibility was defined for ATP III by: (1) coronary heart disease (CHD) and CHD risk equivalents and included adults with diabetes,12 ie, assigned 10‐year CHD risk >20%, and LDL‐C ≥100 mg/dL; and (2) combination of calculated 10‐year CHD risk and LDL‐C in four groups: (a) risk >20% and LDL‐C ≥100 mg/dL, (b) risk 10% to 20% and LDL C ≥130 mg/dL or (c) two or more major risk factors, 10‐year risk <10% ,and LDL‐C ≥160 mg/dL; and (d) <10%, 0 to 1 risk factors, and LDL‐C ≥190 mg/dL (Table S1).3, 9.
For the 2013 ACC/AHA cholesterol guidelines,3 statin eligibility was defined by:
IA (1=benefit>>>risk; A=multiple randomized clinical trials or meta‐analyses), which includes all adults with (1) clinical ASCVD and 75 years or younger, (2) diabetes and aged 40 to 75 years and LDL‐C ≥70 mg/dL, and (3) adults without diabetes and ASCVD10 risk ≥7.5%.
IB (B=single randomized trial or nonrandomized studies), which includes adults 21 years and older with LDL‐C ≥190 mg/dL.
IIaB (IIA=benefit≫risk) level recommendations, which includes: (1) clinical ASCVD in patients older than 75 years (IIaB). The ATP III guideline update noted that evidence provided “strong justification for intensive LDL‐lowering therapy in adults 65 to 80 years old with established CVD.9 (2) Adults without diabetes, aged 40 to 75 years, with ASCVD10 risk ≥5% to <7.5% and LDL‐C 70 mg/dL to 189 mg/dL. Adults with diabetes were subdivided into individuals with ASCVD risk ≥7.5% (IA) and <7.5% (1A).3, 4 Moderate‐intensity statin therapy received a 1A recommendation for all eligible adults with diabetes. High‐intensity statin therapy received a IIaB recommendation for the subset with ASCVD10 ≥7.5%.
Estimating ASCVD10 Reduction With Statin Therapy
Two assumptions were used. First, ASCVD events would decline 22% for each 39 mg/dL reduction in LDL‐C based on the Cholesterol Treatment Trialists' colloboration.13 Second, LDL‐C would decline 30% with moderate‐ and 50% with high‐intensity statin therapy. The estimates are conservative given a reported decline of LDL‐C of 30% to <50% with moderate‐intensity and ≥50% with high‐intensity statin therapy.3
For patients with clinical ASCVD in whom ASCVD10 was not calculated, a risk of 34.5% was assigned. The estimate was based on evidence that adults with clinical CHD have a 26% 10‐year risk of another CHD event and that patients with vascular CHD risk equivalent status have a 10‐year CHD risk of ≥20%.14, 15, 16, 17 Using a conservative approach, the 26% and 20% 10‐year CHD event rates in patients with clinical ASCVD were averaged. We assumed the risk for any ASCVD event including CHD was 50% greater than the risk for CHD alone, ie, 23%×1.5=34.5%. This assumption is also conservative, since there are approximately 795,000 strokes and 735,000 myocardial infarctions reported in the United States annually.18, 19
Data Reporting and Analysis
Descriptive statistics including mean and standard deviation were generated for adults with and without hypertension and for the various group of statin‐eligible adults by the ATP III and/or 2013 cholesterol guideline as well as those who were ineligible for statin therapy by either guideline. The t test was applied for continuous variables and χ2 test was used for categorical variables. SAS Enterprise Guide 7.1 (SAS Institute Inc, Cary, NC) was used for all analyses. Two‐sided P values <.05 were accepted as significant.
Results
Among 1,497,564 adults aged 21 to 80 years seen between January 1, 2011, and June 30, 2014, a total of 1,085,796 (72.5%) were excluded for various reasons, leaving 411,768 adults (27.5%) for analysis (Figure). The distribution of adults prescribed statins and statin eligibility among adults not prescribed statins are depicted separately for nonhypertensive and hypertensive subsets.
Figure 1.
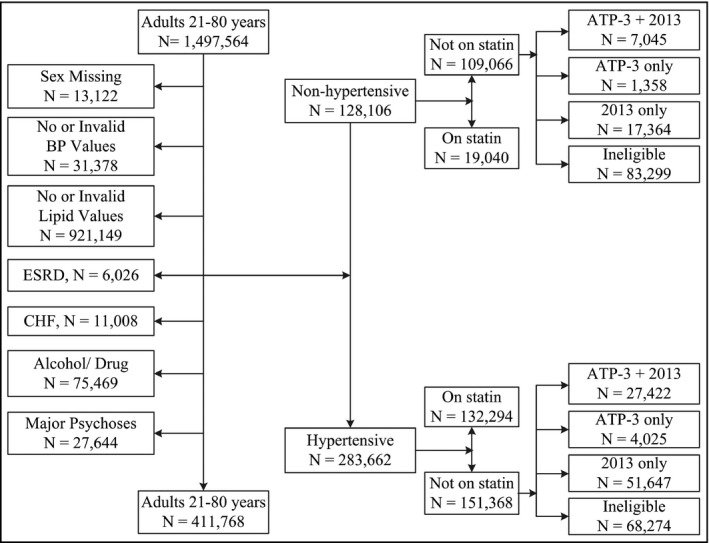
The process is shown for deriving the study sample of statin‐eligible nonhypertensive and hypertensive adults aged 21 to 80 years from the subset of 428,802 with sufficient clinical data to assess atherosclerotic cardiovascular disease risk. BP indicates blood pressure; ESRD, end‐stage renal disease; CHF, congestive heart failure; ATP‐3, Third Report of the Adult Treatment Panel III.
In both the nonhypertensive and hypertensive groups, adults taking statins were older and more likely to be men but had clinically comparable body mass indices (Table 1) to their peer group not taking statins. However, differences were statistically significant given the large sample size. In the nonhypertensive group, total cholesterol, LDL‐C, and triglycerides were higher among adults taking statins, whereas the reverse was true for adults with hypertension except for HDL‐C. Diabetes mellitus, cigarette smoking, stage 3 to 4 CKD, 10‐year CHD risk and risk equivalent status, and ASCVD10 risk were greater in adults with hypertension. Within the nonhypertensive and hypertensive groups, most of these same variables were higher in adults prescribed statins than those not prescribed statins with the exception of cigarette smoking in the nonhypertensive group.
Table 1.
Characteristics of Adults With and Without Hypertension by Statin Prescription Status
| Nonhypertensive Adult | P Value | Hypertensive Adult | P Value | |||
|---|---|---|---|---|---|---|
| Taking Statin | Not Taking Statin | Taking Statin | Not Taking Statin | |||
| No./% | 19,040/14.9 | 109,066/85.1 | 132,294/46.6 | 151,368/53.4 | ||
| Age, y | 56.7±11.8 | 45.3±13.8 | <.0001 | 62.2±11.0 | 54.9±13.8 | <.0001 |
| Men/women, % | 49.5/50.5 | 37.8/62.2 | <.0001 | 46.5/53.5 | 39.8/60.2 | <.0001 |
| Race, % | ||||||
| Black | 9.2 | 14.0 | <.0001 | 24.1 | 24.5 | <.0001 |
| White | 76.9 | 72.0 | 62.5 | 61.8 | ||
| Other, unknown | 13.8 | 14.0 | 13.4 | 13.7 | ||
| BMI, kg/m2 | 28.6±5.7 | 28.2±6.7 | <.0001 | 31.9±7.3 | 32.0±8.0 | <.0001 |
| Obese, % | 32.2 | 31.7 | .20 | 54.7 | 53.3 | <.0001 |
| SBP, mm Hg | 122.1±12.4 | 120.4±13.0 | <.0001 | 132.3±17.5 | 132.4±17.9 | .3 |
| DBP, mm Hg | 75.2±8.5 | 75.1±8.8 | .40 | 77.7±10.4 | 80.0±10.9 | <.0001 |
| Total cholesterol, mg/dL | 194.2±43.8 | 189.0±36.6 | <.0001 | 180±44.4 | 187.1±38.6 | <.0001 |
| HDL cholesterol, mg/dL | 51.8±17.7 | 53.0±19.2 | <.0001 | 48.3±17.0 | 50.0±18.8 | <.0001 |
| LDL cholesterol, mg/dL | 115.0±38.5 | 112.1±31.1 | <.0001 | 102.4±37.4 | 109.8±32.4 | <.0001 |
| Triglycerides, mg/dL | 128.6±72.6 | 114.6±71.7 | .009 | 137.6±75.8 | 130.3±75.5 | <.0001 |
| Diabetes mellitus, % | 11.3 | 4.8 | <.0001 | 40.7 | 21.3 | <.0001 |
| Glycated hemoglobin <8%, % | 76.1 | 68.7 | <.0001 | 73.1 | 73.7 | .1 |
| Cigarette smokers, % | 13.6 | 16.1 | <.0001 | 21.1 | 19.3 | <.0001 |
| Stage 3 or 4 CKD, % | 3.4 | 1.8 | <.0001 | 13.4 | 8.4 | <.0001 |
| CHD10, % | 5.0±5.0 | 3.0±3.9 | <.0001 | 8.6±7.5 | 6.3±6.7 | <.0001 |
| CHD10 >20%, % | 19.2 | 7.3 | <.0001 | 56.8 | 30.0 | <.0001 |
| CHD10 10%–20%, % | 15.2 | 7.5 | 14.9 | 14.4 | ||
| CHD10 <10%, % | 65.5 | 85.2 | 28.3 | 55.1 | ||
| ASCVD10, % | 10.3±12.1 | 6.0±12.8 | <.0001 | 21.6±15.1 | 14.3±15.8 | <.0001 |
| ASCVD, % | 8.5 | 2.4 | <.0001 | 24.3 | 9.6 | <.0001 |
| LDL ≥190 mg/dL, % | 3.7 | 1.3 | <.0001 | 1.9 | 1.3 | <.0001 |
| ⊕DM ASCVD10 ≥7.5%, % | 5.3 | 1.7 | <.0001 | 23.7 | 12.5 | <.0001 |
| ⊕DM ASCVD10 <7.5%, % | 4.6 | 2.8 | 5.2 | 5.1 | ||
| ∅DM ASCVD10 ≥7.5%, % | 25.3 | 14.2 | <.0001 | 27.4 | 29.4 | <.0001 |
| ∅DM ASCVD10 5.0%–7.4%, % | 10.9 | 6.5 | 5.6 | 7.9 | ||
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; ASCVD10, 10‐year risk of atherosclerotic cardiovascular disease; CHD, coronary heart disease; CHD10, 10‐year risk of coronary heart disease; CKD, chronic kidney disease; DBP, diastolic blood pressure; ⊕DM, diabetes mellitus; ∅DM, no diabetes mellitus; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; obese, body mass index (BMI) ≥30 kg/m2; SBP, systolic blood pressure. Data are expressed as mean±standard deviation.
Within the nonhypertensive group not taking statins (Table 2), percentages of statin‐eligible adults according to ATP III or the 2013 guideline or both are shown. Overall, 23.6% of nonhypertensive adults not prescribed a statin were eligible for statins according to one or both guidelines, with 22.4% eligible by the 2013 guidelines vs 7.7% by the ATP III guidelines (Figure, Table 2). Adults eligible for statin therapy by only ATP III and adults ineligible by either guideline were younger and had lower systolic BP values than statin‐eligible adults by both guidelines or by the 2013 guideline only. BP, total cholesterol, non–HDL‐C, and LDL‐C were lowest in those ineligible for either guideline and highest in those eligible for both. These lipid values were higher in those only eligible by ATP III than in ASCVD only. Diabetes and CHD risk equivalent status were more common among those who were eligible according to ATP III and both ATP III and 2013 guidelines than only those eligible according to the 2013 guidelines and least common in those ineligible by either guideline.
Table 2.
Statin Eligibility in Adults Without Hypertension Not Prescribed a Statin
| Eligibility | Not Taking a Statin | |||
|---|---|---|---|---|
| Eligible According to ATP III and 2013 Cholesterol Guidelines | Only Eligible According to ATP III Guideline | Only Eligible According to 2013 Cholesterol Guideline | Not Eligible According to Either Guideline | |
| No./% | 7045/6.5 | 1358/1.2 | 17,364/15.9 | 83,299/76.4 |
| Age, y | 55.1±11.2 | 39.9±17.1 | 60.7±9.1 | 41.4±12.0 |
| Men/women, % | 55.1/44.9 | 46.5/53.5 | 56.4/43.6 | 32.3/67.7 |
| Race, % | ||||
| Black | 1238 | 20.3 | 12.0 | 14.5 |
| White | 75.2 | 66.3 | 77.0 | 70.7 |
| Other, unknown | 12.5 | 13.3 | 11.0 | 14.8 |
| Obese, % | 40.0 | 48.9 | 30.5 | 31.0 |
| BMI, kg/m2 | 29.5±6.1 | 31.2±7.9 | 28.2±5.9 | 28.1±6.8 |
| SBP, mm Hg | 126.0±13.7 | 123.2±13.7 | 125.9±12.7 | 118.7±12.5 |
| DBP, mm Hg | 77.3±8.9 | 76.9±9.0 | 76.3±8.6 | 74.8±8.8 |
| Total cholesterol, mg/dL | 228.9±43.1 | 209.8±30.4 | 190.0±32.9 | 184.9±34.6 |
| HDL cholesterol, mg/dL | 47.2±17.6 | 45.1±15.9 | 50.5±21.2 | 54.2±18.9 |
| LDL cholesterol, mg/dL | 152.0±37.4 | 136.8±25.6 | 113.8±26.6 | 107.9±28.7 |
| Triglycerides, mg/dL | 148.3±78.7 | 139.4±78.9 | 132.1±82.0 | 107.7±66.9 |
| Diabetes mellitus, % | 26.2 | 62.7 | 7.0 | 1.6 |
| Glycated hemoglobin <8%, % | 71.9 | 56.2 | 75.1 | 65.9 |
| Cigarettes, % | 31.3 | 28.4 | 22.5 | 13.3 |
| CKD stage 3 or 4, % | 3.5 | 2.3 | 4.0 | 1.2 |
| CHD10, % | 9.4±7.1 | 5.2±6.8 | 6.8±4.3 | 1.7±2.0 |
| CHD10 >20%, % | 49.7 | 65.4 | 12.6 | 1.7 |
| CHD10 10%–20%, % | 30.5 | 15.6 | 27.4 | 1.2 |
| CHD10 <10%, % | 19.8 | 19.0 | 60.0 | 97.1 |
| ASCVD10, % | 17.4±13.9 | 10.1±18.5 | 12.8±10.6 | 3.5±12.0 |
| ASCVD | 23.3 | 0 | 6.5 | 0 |
| LDL ≥190 mg/dL, % | 19.6 | 0.0 | 0.0 | 0.0 |
| ⊕DM ASCVD10 ≥7.5%, % | 12.7 | 8.9 | 2.8 | 0.4 |
| ⊕DM ASCVD10 <7.5% | 11.2 | 53.8 | 3.2 | 1.2 |
| ∅DM ASCVD10 ≥7.5%, % | 29.2 | 13.9 | 52.9 | 4.9 |
| ∅DM ASCVD10 5% to <7.5%, % | 5.4 | 4.1 | 34.7 | 0.8 |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; ASCVD10, 10‐year risk of atherosclerotic cardiovascular disease; CHD, coronary heart disease; CHD10, 10‐year risk of coronary heart disease; CKD, chronic kidney disease; DBP, diastolic blood pressure; ⊕DM, diabetes mellitus; ∅DM, no diabetes mellitus; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; obese, body mass index (BMI) ≥30 kg/m2; SBP, systolic blood pressure. Data are expressed as mean±standard deviation.
Among adults with hypertension not prescribed a statin, 54.9% were eligible by one or both guidelines, with 52.2% eligible by the 2013 guideline and 20.8% by the ATP III guideline (Figure, Table 3). Adults eligible by both guidelines and the 2013 guideline only were older than those who were only eligible by ATP III and ineligible by both guidelines. The highest BMI values occurred in the ATP III only eligible group, which coincides with this group also having the highest diabetes prevalence. Systolic BP was lowest among adults who were statin ineligible by either guideline, whereas diastolic BP was clinically similar across all four groups. Total cholesterol, non–HDL‐C and LDL‐C, CHD risk equivalent status, and ASCVD10 risk were greater in statin‐eligible than statin‐ineligible adults.
Table 3.
Statin Eligibility in Hypertensive Adults Not Prescribed a Statin
| Eligibility | Not Taking a Statin | |||
|---|---|---|---|---|
| Eligible According to ATP III and 2013 Cholesterol Guidelines | Only Eligible According to ATP III Guideline | Only Eligible According to 2013 Cholesterol Guideline | Not Eligible According to Either | |
| No./% | 27,422/18.1 | 4025/2.7 | 51,647/34.1 | 68,274/45.1 |
| Age, y | 60.0±10.2 | 54.6±21.8 | 61.5±9.3 | 47.9±13.8 |
| Men/women, % | 48.6/51.4 | 39.5/60.5 | 45.3/54.7 | 32.1/67.9 |
| Race | ||||
| Black, % | 25.1 | 27.8 | 26.1 | 22.8 |
| White, % | 60.8 | 58.2 | 62.2 | 62.1 |
| Other, unknown, % | 14.0 | 14.0 | 11.6 | 15.1 |
| Obese, % | 58.2 | 57.0 | 51.8 | 53.4 |
| BMI, kg/m2 | 32.4±7.5 | 33.4±9.2 | 31.5±7.5 | 32.1±8.5 |
| SBP, mm Hg | 136.7±19.0 | 135.3±18.9 | 134.6±18.0 | 128.8±16.6 |
| DBP, mm Hg | 80.8±11.1 | 80.1±11.5 | 79.7±11.0 | 80.0±10.8 |
| Total cholesterol, mg/dL | 215.1±37.6 | 208.1±30.5 | 179.9±33.1 | 180.2±37.7 |
| HDL cholesterol, mg/dL | 46.9±16.4 | 45.5±15.3 | 50.3±19.4 | 51.4±19.7 |
| LDL cholesterol, mg/dL | 138.2±31.5 | 133.7±24.3 | 102.8±25.6 | 101.8±30.7 |
| Triglycerides, mg/dL | 150.0±77.7 | 144.1±78.0 | 131.9±76.5 | 120.0±71.6 |
| Diabetes mellitus, % | 45.7 | 54.0 | 21.3 | 9.7 |
| Glycated hemoglobin <8%, % | 72.4 | 69.8 | 76.4 | 72.6 |
| Cigarettes, % | 28.4 | 23.2 | 22.9 | 12.6 |
| CKD stage 3 or 4, % | 11.1 | 12.4 | 10.6 | 5.3 |
| 10‐y CHD, % | 11.8±8.2 | 11.1±10.5 | 7.5±5.4 | 3.5±5.1 |
| CHD10 >20% | 70.4 | 72.0 | 30.8 | 10.8 |
| CHD10 10%–20% | 23.2 | 15.7 | 22.4 | 5.8 |
| CHD10 <10% | 6.4 | 12.2 | 46.9 | 83.4 |
| ASCVD10, % | 23.4±13.9 | 23.0±22.5 | 17.2±12.6 | 7.8±15.5 |
| ASCVD, % | 24.8 | 0 | 15.0 | 0 |
| LDL ≥190 mg/dL, % | 7.0 | 0.0 | 0.0 | 0.0 |
| ⊕DM ASCVD10 ≥7.5%, % | 28.8 | 24.6 | 11.0 | 6.3 |
| ⊕DM ASCVD10 <7.5% | 8.2 | 29.4 | 3.9 | 3.4 |
| ∅DM ASCVD10 ≥7.5%, % | 28.8 | 32.7 | 50.9 | 13.1 |
| ∅DM ASCVD10 5% to <7.5%, % | 2.5 | 1.7 | 19.2 | 2.0 |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; ASCVD10, 10‐year risk of atherosclerotic cardiovascular disease; CHD, coronary heart disease; CHD10, 10‐year risk of coronary heart disease; CKD, chronic kidney disease; DBP, diastolic blood pressure; ⊕DM, diabetes mellitus; ∅DM, no diabetes mellitus; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; obese, body mass index (BMI) ≥30 kg/m2; SBP, systolic blood pressure. Data are expressed as mean±standard deviation.
ASCVD10 events without statin therapy and the relative and absolute reductions with statin therapy in adults without (Table 4) and with hypertension (Table 5) were estimated. Statin eligibility was defined according to the 2013 guideline and is exclusive and sequential beginning with adults having clinical ASCVD, LDL ≥190 mg/dL, diabetes, and no diabetes. Adults with and without diabetes were subdivided based on the ASCVD10 boundaries shown. The largest proportion of statin‐eligible individuals in the nonhypertensive and hypertensive groups was comprised of adults without diabetes who had absolute ASCVD10 risk ≥7.5% followed by individuals with clinical ASCVD. These same groups also contributed more than the other categories to absolute numbers of ASCVD10 events before and after statin therapy. The two groups with the smallest absolute risk reduction and largest NNTs are adults with diabetes and ASCVD10 <7.5% and adults without diabetes and ASCVD10 5% to 7.4%. Removing the two lowest risk groups increased absolute risk reduction and reduced the NNT to prevent a major ASCVD event.
Table 4.
Estimated Decline in ASCVD Events in Adults Without Hypertension Eligible For But Not Currently Taking Statin Therapy
| Nonhypertensive, No Statin Group | No. | Statin Intensity | ∅Statin ASCVD10, % | ∅Statin ASCVD10 | ASCVD10 ⊕Statin, No. | Change ASCVD10 Events | Relative ASCVD Reduction, % | Absolute ASCVD Reduction, % | Number Needed to Treat |
|---|---|---|---|---|---|---|---|---|---|
| ASCVD | 2666 | High | 34.5 | 920 | 653 | 267 | 28.9 | 10 | 10 |
| LDL ≥190 mg/dL | 1379 | High | 7.8 | 108 | 55 | 52 | 48.7 | 3.8 | 26 |
| ⊕DM ASCVD10 ≥7.5% | 1379 | High | 19.5 | 269 | 188 | 81 | 30.1 | 5.9 | 17 |
| ⊕DM ASCVD10 <7.5% | 1344 | Moderate | 3.6 | 48 | 39 | 9 | 18.8 | 0.7 | 143 |
| ∅DM ASCVD10 ≥7.5% | 11,241 | High | 15.3 | 1720 | 1169 | 551 | 32.0 | 4.9 | 20 |
| ∅DM ASCVD10 5%–7.4% | 6400 | Moderate | 6.1 | 390 | 307 | 83 | 20.8 | 1.3 | 77 |
| Total (All) | 24,409 | Moderate to high | 14.1 | 3442 | 2416 | 1025 | 29.8 | 4.2 | 24 |
| All minus ⊕DM <7.5%, ∅DM 5%–7.4% | 16,665 | High | 18.1 | 3016 | 2066 | 950 | 32.8 | 5.7 | 18 |
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; ASCVD10, 10‐year risk of atherosclerotic cardiovascular disease; ⊕DM, diabetes mellitus; ∅DM, no diabetes mellitus; LDL, low‐density lipoprotein.
Table 5.
Estimated Reduction in ASCVD10 Events in Hypertensive Adults Eligible For But Not Prescribed a Statin
| Hypertensive, No Statin Group | No. | Statin Intensity | ∅Statin ASCVD10, % | ∅Statin ASCVD10, No. | ⊕Statin ASCVD10, No. | ΔASCVD10 Events | Relative ASCVD Reduction | Absolute ASCVD Reduction | Number Needed to Treat |
|---|---|---|---|---|---|---|---|---|---|
| With ASCVD | 14,523 | High | 34.5 | 5010 | 3645 | 1365 | 27.1 | 9.4 | 11 |
| LDL ≥190 mg/dL | 1910 | High | 15.2 | 290 | 147 | 143 | 49 | 7.5 | 13 |
| ⊕DM ASCVD10 ≥7.5% | 13,603 | High | 24.6 | 3346 | 2367 | 979 | 29.2 | 7.2 | 14 |
| ⊕DM ASCVD10 <7.5% | 4226 | Moderate | 4.3 | 182 | 148 | 34 | 18.2 | 0.8 | 125 |
| ∅DM ASCVD10 ≥7.5% | 34,218 | High | 17.0 | 5817 | 4004 | 1814 | 31.1 | 5.3 | 19 |
| ∅DM ASCVD10 5%–7.4% | 10,589 | Moderate | 6.2 | 657 | 529 | 127 | 20.1 | 1.2 | 83 |
| Total (All) | 79,069 | Moderate to high | 20.3 | 15,339 | 10,912 | 4428 | 28.9 | 5.6 | 18 |
| All minus ⊕DM <7.5%, ∅DM 5–7.4% | 64,254 | High | 22.5 | 14,457 | 10,152 | 4305 | 30.3 | 6.7 | 15 |
Abbrevations: ASCVD, atherosclerotic cardiovascular disease; ASCVD10, 10‐year risk of atherosclerotic cardiovascular disease; ⊕DM, diabetes mellitus; ∅DM, no diabetes mellitus; LDL, low‐density lipoprotein.
Statin eligibility by ATP III or the 2013 guidelines was greater in adults aged 60 to 80 years than those 21 to 59 years, in hypertensive than nonhypertensive adults, and by the 2013 than the ATP III guideline (Figure S1). The greater proportion of statin eligibility with the 2013 than ATP III guideline was largely accounted for by differences in calculated risk levels that qualified for statin therapy.
Discussion
Statins are effective for primary and secondary ASCVD prevention in eligible adults.1, 2 The opportunity to prevent more ASCVDs is limited by statin‐eligible adults not prescribed a statin.3 This paper extends the previous report on statin eligibility nationally3 by estimating the number of ASCVD events that could be prevented by implementing the 2013 cholesterol guidelines. Nearly 40% of adults aged 21 to 80 years in our diverse, community‐based, practice network registry currently not prescribed a statin were statin eligible by the 2013 cholesterol guidelines. Prescribing an appropriate‐intensity statin was estimated to reduce the 10‐year risk of an ASCVD10 event by a relative 29.0% and an absolute 5.3% with a 10‐year estimated NNT of 19. Full implementation of the 2013 cholesterol guidelines emerges as a relatively efficient strategy for reducing ASCVD events in this clinic‐based population.
In our analysis, the majority of statin‐eligible adults currently not prescribed a statin had hypertension (76.4%). Among US adults aged 40 to 75 years, approximately 14.4 million adults who were ineligible for statins under the ATP III guideline were eligible by the 2013 guideline, which included 7.9 million (54.9%) with hypertension.3 The larger proportion of statin‐eligible adults with hypertension in our analysis than the previous report likely reflects differences between our clinic‐based and the National Health and Nutrition Examination Survey (NHANES) population–based sample. In our clinic‐based study, the proportion of adults with hypertension was greater than in the NHANES population–based sample.3 Moreover, adults with hypertension were more likely to have a lipid profile than adults without hypertension in our study (data not shown).
The potential value of statin therapy for reducing ASCVD events in adults with hypertension may be underrecognized. The majority of adults with hypertension have a concomitant lipid disorder.20 Antihypertensive therapy alone reduces the risk for CHD approximately 20% to 25%, whereas moderate‐intensity statin therapy decreases CHD events in adults with hypertension more than 35%.20, 21, 22 Stroke is reduced 35% to 40% with antihypertensive therapy and approximately 22% with statins.23, 24 Treatment of hypertension and hypercholesterolemia in adults with both risk factors provides greater protection against ASCVD than treatment of only one risk factor. Moreover, patients taking statin therapy are more likely to have controlled hypertension and less likely to have treatment‐resistant hypertension than their counterparts not receiving statins.25, 26 In this report, more than 70% of all adults with hypertension were either prescribed a statin (46.6%) or eligible for a statin (27.9%) by the 2013 cholesterol guidelines.
Our estimates of statin eligibility are higher than a prior estimate,3 which did not include adults without diabetes and ASCVD10 5% to 7.4% or adults aged 76 to 80 years. Both groups received a IIaB recommendation for statin therapy in the 2013 guidelines.2 While adults aged 40 to 75 years with diabetes and ASCVD10 <7.5% received a IA and adults aged 40 to 75 years without diabetes and ASCVD10 5% to 7.5% received a IIaB recommendation, absolute risk reduction and NNT were more favorable in the latter group (Table 4 and Table 5).
Removing the two groups with the lowest absolute benefit and highest NNTs, ie, adults with diabetes and ASCVD10 <7.5 and without diabetes and ASCVD10 5% to <7.5%, lowered the NNT from 24 to 18 for adults without hypertension and from 18 to 15 for adults with hypertension. When the two lowest risk groups were removed, 32% fewer adults without hypertension and 19% fewer adults with hypertension would receive statin therapy, yet 93% and 97%, respectively, of estimated ASCVD event prevention was retained.
The 2013 cholesterol guidelines included a favorable risk‐benefit analysis for each group in which statin therapy was recommended, ie, IA, IB, and IIaB. Given the proven benefits of statins and relative safety for reducing ASCVD, it is important to understand barriers to implementation of and adherence with the guideline at the healthcare system, clinician, and patient level. Health system barriers such as lack of discharge planning after hospitalization and lack of care coordination and continuity by multiple providers across institutions and community settings contribute to geographic variations in patient nonadherence.27, 28 Although recent studies reported considerable improvements in guideline implementation, common clinician barriers include lack of awareness or knowledge of guidelines, disagreement and uncertainty with recommendations, concerns about side effects, clinical inertia, and time.29, 30, 31 Suggested strategies for more effective guideline implementation include engaging transdisciplinary teams with guideline developers, implementation scientists, clinicians, other healthcare professionals, and patients to identify and mitigate barriers.31, 32 Further, some studies identified computerized reminders, guideline implementation planning checklists, and software applications and interface platforms as information support systems to improve physician performance and prescribing behaviors.33 Patient factors associated with adherence with statins are multifactorial and include sex, race/ethnicity, regimen complexity and cost, comorbidity status, healthcare utilization and access, trust, and provider‐patient communication.34, 35, 36 Adherence interventions that address multi‐level barriers have the potential to increase guideline use and improve patient outcomes.
Study Limitations
Limitations of this analysis include a regional, clinic‐based, rather than national, population‐based sample. Thus, extrapolation of these findings to all adults in the region or nation is limited. More than 60% of adults were excluded for missing or invalid lipid data, and individuals without hypertension were less likely than adults with hypertension to have a lipid profile. While missing data were common in this clinical dataset, >50% of NHANES participants are missing an LDL value.20 The missing data introduce potential additional bias with regard to identifying fewer statin‐eligible adults, especially without hypertension, but it reflects current practice in our quality improvement network. Estimates of LDL‐C reduction with moderate‐ and high‐intensity statin therapy were conservative. Yet, given physician resistance to prescribing and patient experience of adverse effects or other reasons for resistance to long‐term adherence with statin therapy, the predicted (vs actual) benefits of statin therapy on ASCVD events are likely overly optimistic. Our analytical data set did not include information on previous statin therapy among patients currently not prescribed statins in order to estimate the magnitude of potential statin intolerance. Despite the limitations noted, the intent is to raise awareness of the potential for ASCVD prevention with full implementation of the 2013 cholesterol guideline.
Conclusions
Among adults aged 21 to 80 years in a practice‐based setting and currently not prescribed a statin, almost 40% were eligible for statin therapy according to the 2013 cholesterol guidelines. Estimates suggest that treating 19 eligible adults with recommended intensity statin therapy for 10 years would prevent a major ASCVD event. Our findings suggest that further progress in reducing cardiovascular events regionally, attaining national goals for heart disease and stroke prevention, and potentially reducing the projected health financial burden of cardiovascular diseases would be facilitated by implementing the 2013 cholesterol guidelines in practice‐based settings.6, 20, 37
Funding
This research was supported in part by funding from the Centers for Disease Control through the South Carolina Department of Health and Environmental Control and from the Health Research Services Administration through the Medical University of South Carolina.
Supporting information
Table S1. Eligibility for treatment of hypercholesterolemia by the Third Report of the Adult Treatment Panel III (ATP III) (top) and the American College of Cardiology/American Heart Association (ACC/AHA) 2013 (bottom) cholesterol guidelines.
Figure S1. Statin eligibility by the Third Report of the Adult Treatment Panel III (ATP III) and the American College of Cardiology/American Heart Association 2013 cholesterol guidelines. Both are shown for nonhypertensive (top) and hypertensive (bottom) adults with both groups subdivided by age 21 to 59 years and 60 to 80 years.
Acknowledgments and disclosures
The authors appreciate the essential support provided by David Ramsey and Shaun Wagner for building and maintaining the Care Coordination Institute (CCI) clinical data repository and Lauren Henslee for logistical support with the publication. We are indebted to the physicians and staff in the clinics and health systems that participate in the CCI. Dr Egan has received royalties from UpToDate, research support from Medtronic and Quintiles, and income as a consultant from AstraZeneca and Medtronic. None of the other authors have anything to disclose.
J Clin Hypertens (Greenwich). 2016;18:663–671. DOI: 10.1111/jch.12727 © 2015 Wiley Periodicals, Inc.
References
- 1. Taylor F, Huffman MD, Macedo TH, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;(1):1–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 pt B):2889–2934. [DOI] [PubMed] [Google Scholar]
- 3. Pencina MJ, Navar‐Boggan AM, D'Agostino RB, et al. Application of new cholesterol guidelines to a population‐based sample. N Engl J Med. 2014;370:1422–1431. [DOI] [PubMed] [Google Scholar]
- 4. Passel J, Cohn D'V. U.S. Population Projections: 2005–2050. Washington, DC: Pew Research Center; 2008. [Google Scholar]
- 5. Egan BM. Opportunities for multidisciplinary ASH clinical hypertension specialists in an era of population health and accountable care: ASH leadership message. J Am Soc Hypertens. 2014;8:451–456. [DOI] [PubMed] [Google Scholar]
- 6. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States. A policy statement from the American Heart Association. Circulation. 2011;123:933–944. [DOI] [PubMed] [Google Scholar]
- 7. Perry HM, Roccella EJ. Conference report on stroke mortality in the Southeastern United States. Hypertension. 1998;31:1206–1215. [DOI] [PubMed] [Google Scholar]
- 8. Egan BM, Laken MA, Wagner CS, et al. Impacting population cardiovascular health through a community‐based practice network: update on an ASH‐supported collaborative. J Clin Hypertens (Greeenwich). 2011;13:543–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Grundy SM, Cleeman JI, Bairey CN, et al. Implications f or recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;110:227–239. [DOI] [PubMed] [Google Scholar]
- 10. Egan BM, Zhao Y, Li J, et al. Prevalence of optimal treatment regimens in patients with apparent treatment resistant hypertension in a community‐based practice network. Hypertension. 2013;62:691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low‐density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 12. American Diabetes Association . Standards of medical care in diabetes – 2014. Diabetes Care. 2014;37(suppl 1):S14–S80. [DOI] [PubMed] [Google Scholar]
- 13. Cholesterol Treatment Trialists' Collaboration . Efficacy and safety of more intensive lowering of LDL cholesterol: a meta‐analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Long‐Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group . Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–1357. [DOI] [PubMed] [Google Scholar]
- 15. Sacks FM, Pfeffer MA, Moye LA, et al; for the Cholesterol Recurrent Events Trial Investigators . The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–1009. [DOI] [PubMed] [Google Scholar]
- 16. Crouse JR III, Byington RP, Bond MG, et al. Pravastatin, lipids, and atherosclerosis in the carotid arteries (PLAC‐II). Am J Cardiol. 1995;75:455–459. [DOI] [PubMed] [Google Scholar]
- 17. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Final Report. NIH Publication No.02‐5215, September, 2002. [PubMed]
- 18. Stroke Facts. http://www.cdc.gov/stroke/facts.htm. Accessed May 28, 2015.
- 19. About Heart Disease and Stroke: Consequences & Costs. http://millionhearts.hhs.gov/abouthds/cost-consequences.html. Accessed May 28, 2015.
- 20. Egan BM, Li J, Qanungo S, Wolfman TE. Blood Pressure and cholesterol control in hypertensive hypercholesterolemic patients: a report from NHANES 1988–2010. Circulation. 2013;128:29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Downs JR, Clearfield M, Weis S, et al; for the AFCAPS/TexCAPS Research Group . Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels. JAMA. 1998;279:1615–1622. [DOI] [PubMed] [Google Scholar]
- 22. Sever PS, Dahlöf B, Poulter NR, et al; ASCOT Investigators . Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower‐than‐average cholesterol concentrations, in the Anglo‐Scandinavian Cardiac Outcomes Trial‐Lipid Lowering Arm (ASCOT‐LLA): a multicentre randomised controlled trial. Lancet. 2003;361:1149–1158. [DOI] [PubMed] [Google Scholar]
- 23. Lackland DT, Roccella EJ, Deutsch AF, et al. Factors influencing the decline in stroke mortality. Stroke. 2014;45:315–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2013;(1):CD004816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States 1999–2012: progress toward healthy people 2020 goals. Circulation. 2014;30:1692–1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gupta AK, Nasothimiou EG, Chang CL, et al. Baseline predictors of resistant hypertension in the Anglo‐Scandinavian Cardiac Outcome Trial (ASCOT): a risk score to identify those at high‐risk. J Hypertens. 2011;29:2004–2013. [DOI] [PubMed] [Google Scholar]
- 27. Fang G, Robinson JG, Lauffenburger J, et al. Prevalent but moderate variation across small geographic regions in patient nonadherence to evidence‐based preventive therapies in older adults after acute myocardial infarction. Med Care. 2014;52:185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sengstock D, Vaitkevicius P, Salama A, Mentzer RM. Under‐prescribing and non‐adherence to medications after coronary bypass surgery in older adults: strategies to improve adherence. Drugs Aging. 2012;29:93–103. [DOI] [PubMed] [Google Scholar]
- 29. Deedwania P. Gaps in guideline implementation: a cause for concern, time for action. J Am Coll Cardiol. 2015;65:278–280. [DOI] [PubMed] [Google Scholar]
- 30. Erhardt LR. Barriers to effective implementation of guideline recommendations. Am J Med. 2005;118:36S–41S. [DOI] [PubMed] [Google Scholar]
- 31. Pronovost PJ. Enhancing physicians' use of clinical guidelines. JAMA. 2013;310:2501–2502. [DOI] [PubMed] [Google Scholar]
- 32. Martin SS, Abd TT, Jones SR, et al. 2013 ACC/AHA cholesterol treatment guideline. J Am Coll Cardiol. 2014;63:2674–2678. [DOI] [PubMed] [Google Scholar]
- 33. Martens JD, van der Weijden T, Winken RAG, et al. Feasibility and acceptability of a computerised system with automated reminders for prescribing behaviour in primary care. Int J Med Inform. 2008;77:199–207. [DOI] [PubMed] [Google Scholar]
- 34. Chakraborty S. Part I: the role of trust in patient noncompliance: a qualitative case study of users of statins for the chronic treatment of high‐cholesterol in New York City. J Risk Res. 2013;16:97–112. [Google Scholar]
- 35. Cheetham TC, Niu F, Green K, et al. Primary nonadherence to statin medications in a managed are organization. J Manag Care Pharm. 2013;19:367–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lewey J, Shrank WH, Bowry ADK, et al. Gender and racial disparities in adherence to statin therapy: a meta‐analysis. Am Heart J. 2013;165:665–678. [DOI] [PubMed] [Google Scholar]
- 37. Healthy People 2020 Objectives. http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx. Accessed May 28, 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Eligibility for treatment of hypercholesterolemia by the Third Report of the Adult Treatment Panel III (ATP III) (top) and the American College of Cardiology/American Heart Association (ACC/AHA) 2013 (bottom) cholesterol guidelines.
Figure S1. Statin eligibility by the Third Report of the Adult Treatment Panel III (ATP III) and the American College of Cardiology/American Heart Association 2013 cholesterol guidelines. Both are shown for nonhypertensive (top) and hypertensive (bottom) adults with both groups subdivided by age 21 to 59 years and 60 to 80 years.


