To the Editor:
We report a case of baroreceptor dysfunction after percutaneous angioplasty for renal artery stenosis (RAS). A 77‐year‐old woman with a history of coronary artery disease, treatment‐resistant hypertension, and left ventricular hypertrophy presented with pulmonary edema and hypertensive emergency with a supine blood pressure (BP) of 250/120 mm Hg and heart rate of 95 beats per minute and a standing BP of 235/115 mm Hg and heart rate of 90 beats per minute. A fundoscopic examination revealed only moderate signs of retinopathy.
The patient was treated with intravenous sodium nitroprusside and intravenous furosemide. After discontinuation of nitroprusside and aggressive diuresis, the patient continued to have episodes of elevated supine BP of 180 to 200/95 to 105 mm Hg and standing BP 170 to 200/85 to 100 mm Hg despite maximum tolerated doses of oral antihypertensive therapy, including chlorthalidone, amlodipine, carvedilol, spironolactone, hydralazine, and isosorbide dinitrate. After the addition of lisinopril 20 mg/d, her supine BP declined to 120/50 mm Hg and her serum creatinine increased from 0.7 mg/dL to 1.8 mg/dL. Results from renal computed tomographic angiography showed dense atherosclerotic calcifications at the renal artery origins with severe right RAS and moderate to severe left RAS. The right kidney was small, measuring 7.6 cm in the long axis, and the left kidney was 10 cm (Figure a and b). We treated the patient with percutaneous angioplasty of severe ostial left RAS with a bare‐metal stent under distal protection. Renal function returned to the baseline normal range after revascularization.
Figure 1.
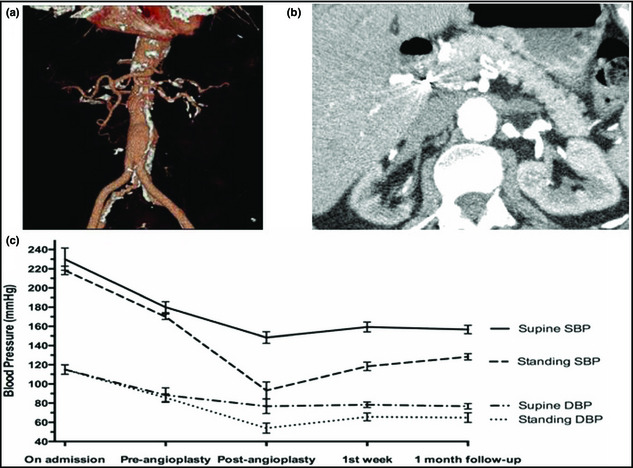
Computed tomographic angiography showing severe bilateral renal artery stenosis (a and b) and supine and standing blood pressure trends on admission, pre‐angioplasty on antihypertensive treatment, immediately after post‐angioplasty, 1 week on nonpharmacologic and pharmacologic treatment for orthostatic hypotension, and 1 month later at the outpatient follow‐up visit (c). SBP indicates systolic blood pressure; DBP, diastolic blood pressure.
After the procedure, the patient developed marked symptomatic orthostatic hypotension with a standing BP of 80 to 110/50 to 60 mm Hg with a heart rate of 85 to 90 beats per minute, and supine hypertension of 140 to 160/70 to 85 mm Hg with a heart rate of 75 to 85 beats per minute. All antihypertensive medications were discontinued and the patient was treated with hydration, sodium tablets, compression stockings, and the addition of fludrocortisone. The Valsalva ratio (R‐R interval recorded during Valsalva maneuver for 20 seconds and immediately afterwards for 5 minutes and calculated as maximal R‐R interval divided by minimal R‐R interval) was 1.3. After the implementation of pharmacologic and nonpharmacologic measures, BP variability decreased and her symptoms improved. At the outpatient follow‐up visits, her symptoms had substantially subsided. Eventually, oral mineralocorticosteroids were discontinued. The trends of orthostatic BP changes are depicted in Figure c.
Studies conducted in experimental animals showed an impairment of baroreflex control in renovascular hypertension caused by angiotensin II.1, 2 Gao and colleagues3 suggested that patients with renovascular hypertension exhibit some degree of autonomic dysfunction, encompassing both the sympathetic and parasympathetic systems. Interestingly, the cardiac baroreceptor reflex sensitivity increased 1 year following renal angioplasty in a subset of patients who were cured or improved regarding hypertension.3
Our case suggests that impaired capability to reflexively buffer spontaneous BP fluctuations in a patient with long‐standing renovascular hypertension resulted in orthostatic hypotension and supine hypertension. Orthostatic changes persisted after discontinuation of antihypertensive medication and rehydration. BP instability and orthostatic changes can occasionally be unmasked by treatment of renovascular hypertension with percutaneous angioplasty and stenting.
References
- 1. Lumbers ER, McCloskey DI, Potter EK. Inhibition by angiotensin II of baroreceptor‐evoked activity in cardiac vagal efferent nerves in dog. J Physiol. 1979;294:69–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Heesch CM, Carey LA. Acute resetting of arterial baroreflex in hypertensive rats. Am J Physiol. 1987;253:H974–H979. [DOI] [PubMed] [Google Scholar]
- 3. Gao SA, Johansson M, Rundqvist B, et al. Reduced spontaneous baroreceptor sensitivity in patients with renovascular hypertension. J Hypertens. 2002;20:111–116. [DOI] [PubMed] [Google Scholar]


