Abstract
Purpose
To describe the utilization trends of a dedicated ophthalmology emergency department (ED) in Boston, Massachusetts.
Methods
The medical records of 500 randomly selected patients who presented at the Massachusetts Eye and Ear (MEE) Emergency Department (ED) from January 2015 to March 2016 were reviewed retrospectively. Data were analyzed using the Pearson χ2 test and multiple logistic regression. The primary study outcome measure was whether a patient’s visit was emergent or nonemergent. Emergent or nonemergent conditions were classified based on the diagnosis and treatment required at follow-up appointments. Nonemergent diagnoses were classified as conditions that could have been seen as an outpatient without negative consequences for vision.
Results
Of the 500 cases, 252 were males and 248 were females. The median age was 45 years (range, 2–101 years). The most common diagnoses were posterior vitreous detachment (8.6%), corneal abrasion (8.4%), dry eye syndrome (7%), and viral conjunctivitis (5.4%). Of the total, 92.6% of patients originated from within Massachusetts. The majority of patients were self-referred (78.6%) or referred from another hospital (12.8%). Nonemergent visits accounted for 49.4% of patients seen. Compared to patients who presented with duration of symptoms for ≥1 week, patients who presented with symptoms of <1 week were more likely to present with an emergent condition (8.8% vs 41.8%). Referrals from an outside ophthalmologist or hospital were predictive of emergent patient visits (OR, resp., 1.971 [95% CI, 0.478–3.462; P = 0.01]; 1.040 [95% CI, 0.462–1.616; P < 0.001]).
Conclusions
In our study, nonemergent patient visits comprised nearly half of all ophthalmology ED visits. Emergent visits were associated with acute symptoms and referrals from outside healthcare providers.
Emergency departments (EDs) in the United States have seen a considerable rise in visits during the first two decades of the 21st century, with a 25% increase from 2001 to 2009.1 Previous studies have attributed this rise in visits to an increase in ED utilization for nonurgent conditions, with lack of access to primary care services as the cause of approximately one-third of nonurgent ED visits.2 A 2013 systematic review showed that 37% of all general ED visits among adults were deemed nonurgent.3 Eye-specific emergency departments are far more rare than general EDs, with only five dedicated ophthalmology EDs currently in the United States. Despite being specialty-specific EDs, these eye EDs experience high patient volumes, which, in our case, have continued to rise annually.
A few studies have been performed to characterize the nature of ophthalmology-specific ED visits and their corresponding urgency. Bascom Palmer Eye Institute in Miami, Florida, conducted a prospective cohort study from 2010 to 2014 and found a significant percentage of nonurgent visits, with 35.8% of new patient visits to its ophthalmology-specific ED deemed as nonemergent.4 In addition, a study of eye-related ED visits in general EDs found that 44.3% of patients presenting with ocular problems had nonemergent conditions.5
Massachusetts Eye and Ear (MEE), associated with Harvard Medical School in Boston, Massachusetts, houses one of the five dedicated ophthalmology EDs in the United States, providing patient care 24-hours per day, 7 days per week, year-round. Massachusetts is a unique location to examine ED visits, given the distinct health insurance coverage of MassHealth, a combined Medicaid and state children’s health insurance program that is a critical part of the health care safety net for the state. MassHealth provides health care coverage to approximately 1.9 million of Massachusetts’s 6.8 million residents.6 No studies to date have evaluated the utilization trends for ophthalmology EDs in the Northeast of the United States.
In this study, we describe utilization trends of the MEE ophthalmology-specific Emergency Department (ED) from January 2015 to March 2016. The specific aims of this investigation were as follows: (1) to characterize the most common diagnoses and types of services rendered in the ED (2) to determine the percentage of emergency visits representing true emergent ophthalmic conditions; (3) and to determine which variables, including patient demographics or insurance status, were associated with higher ED utilization.
Subjects and Methods
This is a retrospective case series of patients who presented to MEE ED. The study protocol was approved by the MEE Institutional Review Board and was performed in compliance with the US Health Insurance Portability and Accountability Act of 1996 and adhering to the tenets of the Declaration of Helsinki.
There were a total of 16,406 encounters at the ED from January 2015 to March 2016. In order to generate a random sampling of cases, the encounters were first populated chronologically, and one encounter was selected at a set interval of every 32nd encounter, such that a total of 500 visits were included for review. The following demographic and clinical examination findings were recorded: date of visit, day of week, time of visit, patient age and sex, city of residence, where patient was referred from, insurance status, duration of symptoms, and final diagnosis or diagnoses, additional imaging, prescription given, intervention performed, and whether or not an on-call specialist was required. Emergent or nonemergent conditions were classified based on the diagnosis and treatment required at the ED visit and/or follow-up appointments. Nonemergent diagnoses were classified as conditions that could have been seen on an outpatient basis in 72 hours without negative consequences for vision. Six types of insurance statuses were analyzed for this study: (1) self-pay (uninsured); (2) Medicaid; (3) Medicare; (4) commercial insurance: health maintenance organization (HMO) or preferred provider organization (PPO); (5) MassHealth; and (6) other. Secondary insurance status was not included in the analysis, and patients with secondary insurance in addition to Medicare were placed in the Medicare category.
The primary outcome measure of the study was whether or not a patient’s diagnosis was emergent. All data analyses were performed using Stata software version 12.0. Pearson χ2 tests were performed for frequency comparisons of categorical variables, and multiple logistic regression was performed to determine factors associated with emergent diagnoses. All analyses were 2-tailed, with P values of ≤0.05 considered significant.
Results
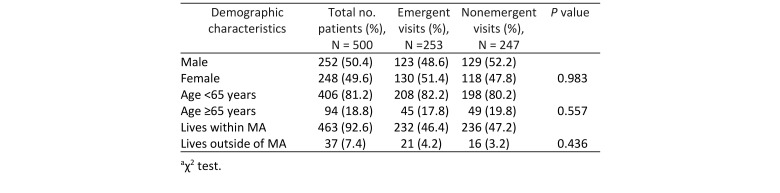
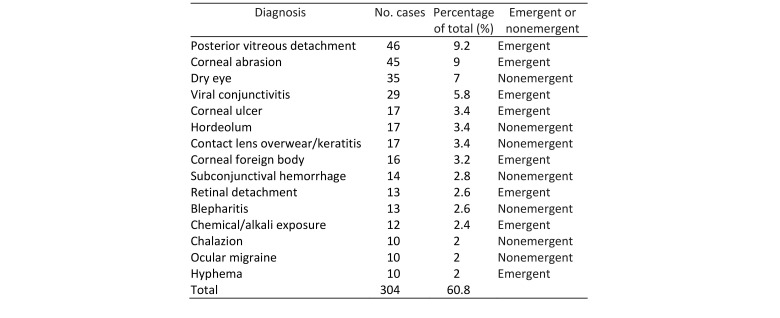
Of the 500 patients, 252 (50.4%) were males, and there was no statistically significant difference between female and male patients who presented with emergent diagnoses (Table 2). The mean and median age of patients included in the study were 45 years and 46 years, respectively, with a range of 2-101 years. Of the 500 patient encounters reviewed during the study period, 253 (50.6%) were classified as emergent. Most patients arriving at our ED fall into one of about 20 common diagnoses. Because of the large volume of patients, cases of usual diseases present in measurable numbers. There were 113 unique final diagnoses reported, with the 15 most common diagnoses being posterior vitreous detachment, corneal abrasion, dry eye, viral conjunctivitis, corneal ulcer, hordeolum, contact lens overwear/keratitis, corneal foreign body, subconjunctival hemorrhage, retinal detachment, blepharitis, chemical/alkali exposure, chalazion, ocular migraine, and hyphema, respectively (Table 1).
Table 2.
Demographic characteristics of patients seen in the ED
Table 1.
Most common diagnoses seen in the Mass Eye and Ear Emergency Department (ED)
Of the 500 patients, 406 (81.2%) were <65 years of age, and there was no significant difference between patients older or younger than 65 in terms of presenting with emergent diagnoses. Logistic regression of age as a continuous variable demonstrated that age was not predictive of the urgency of a patient’s condition (OR, 0.0026; P = 0.56). There was also no significant difference between in-state and out-of-state residency with respect to presenting with an emergent condition (Table 2).
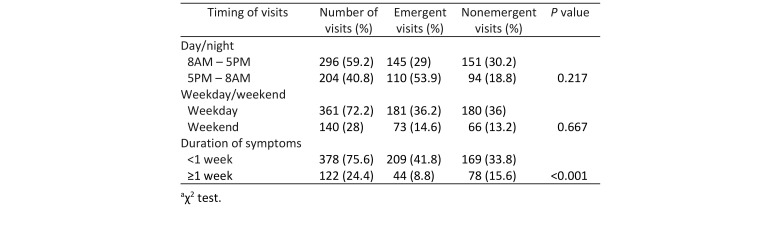
There was no statistically significant difference in presenting with an emergent condition between patients arriving outside of business hours (5 PM to 8 AM) and those who arrived during business hours (8 AM to 5 PM) or between patients presenting on weekdays as compared to the weekend (Table 3). Patients who experienced symptoms for <1 week were more likely to present with an emergent ophthalmic condition than those with symptoms for ≥1 week (209 vs 169 [P < 0.001]; Table 3).
Table 3.
Timing of visits to the ED
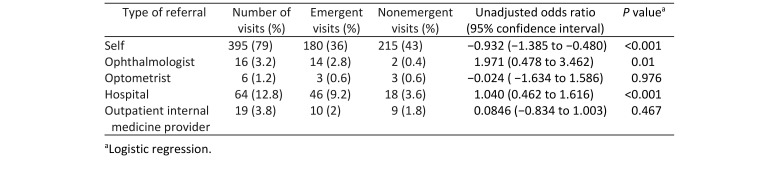
The majority of patients had no formal referral but were self-referred (395 patients [79%]; Table 4). A χ2 test comparing emergent rates among all five referral types demonstrated that there are differences in rates of emergent conditions among all five referral types. Logistic regression showed that patients who were referred by ophthalmologists or hospitals were more likely to present with an emergent ophthalmic condition (OR, resp., 1.971 [95% CI, 0.478–3.462; P = 0.01]; 1.040 [95% CI, 0.462–1.616; P < 0.001]). By contrast, patients who were self-referred were more likely to present with a nonemergent condition (P < 0.001) See Table 4.
Table 4.
Types of referral
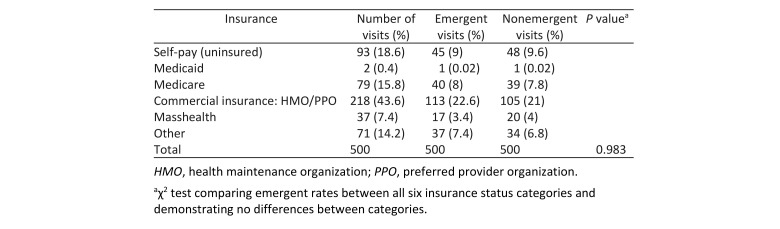
The greatest number of patients fell into the commercial insurance category (218 patients, or 43.6%). There was no significant association with patient insurance status and their odds of presenting with an emergent condition (Table 5).
Table 5.
Insurance status of patient visits
A multiple logistic regression that included sex, age, time of visit (day/night, weekday/weeknight), insurance status, and referral source showed that duration of symptoms and referral were independent predictors of presenting with an emergent condition, P values <0.001 for both variables.
Discussion
This study found that 49.4% of patient visits to the ED were classified as nonemergent. This result is similar to the findings of previous studies from international ophthalmology-specific EDs, which found that nonemergent conditions compromised 50%–70% of all visits.7,8 The high percentage of nonemergent visits may be attributed to the general discomfort of ED physicians and primary care physicians (PCPs) in performing eye examinations and thus the greater likelihood of patients being referred to dedicated ophthalmology EDs.9
The most common presenting diagnoses in our study were posterior vitreous detachment, corneal abrasion, dry eye syndrome, viral conjunctivitis, corneal ulcer, hordeolum, and contact lens overwear/keratitis, akin to similar studies in the literature.4,10–12
As expected and shown in a previous report by Sridhar et al, patients with a shorter duration of symptoms were more likely to present with an emergent condition.4 Emergent conditions are more likely to have sudden onset of symptoms, such as retinal detachment causing floaters, or to be very painful, such as corneal abrasions. Onset of symptoms and pain level were likely factors driving patients with emergent conditions to seek care at the ED at an earlier time compared to patients with nonemergent conditions. Our study showed no difference in urgency of conditions between patients presenting during the day versus at night as well as between patients presenting on weekdays versus weekends. Because of the typically high levels of anxiety patients feel with vision loss or other eye disorders, the actual urgency of the diagnosis may be discordant with patient perception of the problem.
The majority of ED visits were self-referral (79%). Our study showed that there was a significant difference in urgency of conditions between the different types of referrals. Patients referred from ophthalmologists and hospitals were more likely to present with an emergent condition compared with referrals from self, optometrists, or outpatient providers. Hospitals may have an established protocol regarding the urgency of an ophthalmic condition and which ones require referral to an ophthalmologist.13 Only 6 patients in our study were referred from optometrists, which makes it difficult to draw conclusions about their referral process.
Commercial insurance was the most common type of insurance, accounting for 43.6% of ED visits. Self-pay patients comprised 18.6% of visits, which is lower than the 28.8% reported by Sridhar et al and 26.2% by Witmer et al for Florida eye emergency visits as a whole.4,14 We found no difference in the urgency of diagnoses across different types of insurance. Given the unique availability of MassHealth insurance serving as a safety net for patients in Massachusetts, it is expected that the MEE ED would have fewer self-pay patients compared to other states. It is possible that the insurance coverage that MassHealth provides increases patients’ access to PCPs and that these patients may seek care from PCPs more often than from ophthalmology-specific EDs.
A major strength of our study is that diagnoses could be characterized as emergent or nonemergent by consulting both ED visit as well as follow-up appointment notes. Thus, the evaluation of urgency of diagnoses was not confined by subjective opinions of the initial treating physician. Limitations of this study include its retrospective nature and relatively small size. In addition, the time frame of 1.5 years is relatively short compared with previous studies, such as Sridhar et al, who include a 30-day period each year over a 5-year time frame.4 To obtain a representative sample of patients, we randomly selected patients from each month during the study period.
In conclusion, we found that approximately half of all ED visits were nonemergent. Independent factors predictive of emergent visits were duration of symptoms as well as referral from an outside ophthalmologist or hospital. Our findings suggest that improved access to ophthalmologists’ offices may provide more cost-effective care for approximately half of ED visits. The Wilmer Eye Institute of Johns Hopkins Hospital has improved such access by implementing the Same-Day project in 2015, in which all ophthalmology clinic locations created same-day appointment slots for at least 1 practitioner.15 The project, which is ongoing, did not require hiring of additional personnel to accommodate patients.15 A retrospective quality improvement analysis of the Same-Day project found that a patient with a nonemergent eye concern would save $782 in charges and 5.75 hours in visit duration by choosing the same-day outpatient care rather than an emergency department visit. Major eye centers, such as MEE, could implement a similar project with the goal of saving money and time.15
References
- 1.Pines JM, Mullins PM, Cooper JK, Feng LB, Roth KE. National trends in emergency department use, care patterns, and quality of care of older adults in the United States. J Am Geriatr Soc. 2013;61:12–7. doi: 10.1111/jgs.12072. [DOI] [PubMed] [Google Scholar]
- 2.Afilalo J, Marinovich A, Afilalo M, et al. Nonurgent emergency department patient characteristics and barriers to primary care. Acad Emerg Med. 2004;11:1302–10. doi: 10.1197/j.aem.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 3.Uscher-Pines L, Pines J, Kellerman A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19:47–59. [PMC free article] [PubMed] [Google Scholar]
- 4.Sridhar J, Isom RF, Schiffman JC, et al. Utilization of ophthalmology-specific emergency department services. Semin Ophthalmol. 2018;33:185–90. doi: 10.1080/08820538.2016.1188129. [DOI] [PubMed] [Google Scholar]
- 5.Channa R, Zafar S, Canner J, Haring R, Schneider E, Friedman D. Epidemiology of eye-related emergency department visits. JAMA Ophthalmol. 2016;134:312–9. doi: 10.1001/jamaophthalmol.2015.5778. [DOI] [PubMed] [Google Scholar]
- 6.Massachusetts Medicaid Policy Institute MassHealth: The Basic FACTS AND TRENDS. https://bluecrossmafoundation.org/sites/default/files/download/publication/MassHealthBasics_Chartpack_FY2015_FINAL_1.pdf. Accessed May 25, 2018.
- 7.Fenton S, Jackson E, Fenton M. An audit of the ophthalmic division of the accident and emergency department at the royal Victoria Eye and Ear Hospital, Dublin. Ir Med J. 2001;94:265–6. [PubMed] [Google Scholar]
- 8.Carvalho Rde S, José NK. Ophthalmology emergency room at the University of São Paulo General Hospital: a tertiary hospital providing primary and secondary level care. Clinics (Sao Paulo) 2007;62:301–8. doi: 10.1590/s1807-59322007000300015. [DOI] [PubMed] [Google Scholar]
- 9.Tan MM, Driscoll PA, Marsden JE. Management of eye emergencies in the accident and emergency department by senior house officers: a national survey. J Accid Emerg Med. 1997;14:157–8. doi: 10.1136/emj.14.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Price M, Phillips CI. A general practitioner in an ophthalmology accident and emergency department. Br Med J. 1976;2(6034):509–11. doi: 10.1136/bmj.2.6034.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vernon SA. Analysis of all new cases seen in a busy regional center ophthalmic casualty department during a 24-week period. J R Soc Med. 1983;76:279–82. doi: 10.1177/014107688307600408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones NP, Hayward JM, Khaw PT, Claoué CM, Elkington AR. Function of an ophthalmic “accident and emergency” department: results of a six-month survey. Br Med J (Clin Res Ed) 1986;292(6514):188–90. doi: 10.1136/bmj.292.6514.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davey CJ, Green C, Elliott DB. Assessment of referrals to the hospital eye service by optometrists and GPs in Bradford and Airedale. Ophthalmic Physiol Opt. 2011;31:23–8. doi: 10.1111/j.1475-1313.2010.00797.x. [DOI] [PubMed] [Google Scholar]
- 14.Witmer MT, Margo CE. Analysis of ophthalmology work-force and delivery of emergency department eye care in Florida. Arch Ophthalmol. 2009;127:1522–7. doi: 10.1001/archophthalmol.2009.269. [DOI] [PubMed] [Google Scholar]
- 15.Singman EL, Smith K, Mehta R, et al. Cost and visit duration of same-day access at an academic ophthalmology department vs emergency department. JAMA Ophthalmol. 2019;137(7):729–35. doi: 10.1001/jamaophthalmol.2019.0864. [DOI] [PMC free article] [PubMed] [Google Scholar]