Abstract
Garlic supplements are thought to reduce blood pressure (BP). The authors performed a meta‐analysis to investigate garlic's effect on BP. Ovid Medline, Cochrane Library, and PubMed (1946 to November 2013) were used to search for randomized controlled trials. Seventeen trials were included. Pooled analysis showed that garlic intake caused a 3.75‐mm Hg reduction (95% confidence interval [CI], −5.04 to −2.45, I 2=30.7%; P<.001) in systolic BP and a 3.39‐mm Hg reduction (95% CI, −4.14 to −2.65, I 2=67%; P<.001) in diastolic BP compared with controls. Meta‐analysis of subgroups showed a significant reduction in systolic BP in hypertensive (−4.4 mm Hg; 95% CI, −7.37 to −1.42, I 2=0.0%; P=.004) but not normotensive patients. No significant reduction in diastolic BP was seen. After sensitivity analysis, heterogeneity disappeared and significant diastolic BP reduction (−2.68 mm Hg, 95% CI, −4.93 to −0.42, I 2=0.0%; P=.020) was shown in hypertensive patients. This meta‐analysis suggests that garlic supplements are superior to controls (placebo in most trails) in reducing BP, especially in hypertensive patients.
Worldwide, about 25% of adults have hypertension, and 7 million deaths per year may be contributed to hypertension.1 Effective measures must be taken to control blood pressure (BP) in hypertension patients. Antihypertensive medicine has been widely used, but its high cost has caused heavy economic burden to countries and individuals. In addition, side effects and complications often affect treatment adherence of hypertension patients. As a result, alternative or complementary therapy for hypertension is being explored.
Garlic is one of the most utilized supplements, with its antibacterial and antioxidant abilities mainly produced by allicin in garlic. In recent years, garlic has been thought to be effective in the treatment of hypertension. It is reported that allicin has angiotension II–inhibiting and vasodilating effects.2, 3, 4 Phenolic and steroidal compounds in garlic also have pharmacologic effects.5 Evidence from human trials suggests that garlic might be beneficial in the treatment of hypertension.6, 7, 8, 9, 10, 11 However, the results from several previous meta‐analysis were contradictory.12, 13, 14 In 1994, Silagy and colleagues13 included seven trials and found that garlic decreased BP in patients with mild hypertension. Ackermann and colleagues12 performed a meta‐analysis in 2001 to summarize the effects of garlic on several cardiovascular‐related factors and found no significant effects on BP. Ried and colleagues included 25 studies in a systematic review and found that garlic preparations were superior to placebo in reducing BP in individuals with hypertension.14 During the past few years, a number of human trials have been carried out, with new evidence; therefore, we conducted an updated meta‐analysis for the following purposes: (1) to update the evidence on the association between garlic intake and BP, and (2) to examine this association according to dosage and duration.
Materials and Methods
Search Strategy for Identification of Studies
We searched Ovid Medline, Cochrane Library, PubMed (January 1946 through November 2013) to identify randomized controlled trials (RCTs) that examined the effect of garlic on BP. We used the following terms: garlic AND blood pressure OR hypertension to identify intervention studies investigating the effect of garlic on BP. Reference of important articles were searched manually for possible relevant studies.
Inclusion/Exclusion Criteria
Studies were included if they met the following criteria: (1) The study investigated the association between intake of garlic and BP; (2) the studies included randomized controlled trials, reporting the following data: mean systolic and/or diastolic BP (SBP/DBP) and standard deviation (SD) or standard error; and (3) garlic was the only active intervention in the treatment group compared with a control group. Studies were excluded if they were not randomized or did not have a control arm, if they lacked enough data for statistical pooling, or if they did not report BP.
Data Extraction
Data were extracted independently by two researchers (H‐P.W. and J.Y.) according to the described selection criteria. Disagreement was resolved by discussion with the third person (X‐J.Y.). The following data were extracted from the studies: first author's name, publication year, study design, intervention method, study period, sample size, outcomes, method used to generate the randomization, level of blinding, and explanation for withdrawal or dropout.
Statistical Methods
The net changes were calculated as the difference between the baseline and final values of BP. If only SD for the baseline and final values were provided, SD for the net changes were imputed according to the method of Follmann using a correlation coefficient of 0.5. Overall effect size was expressed as weighted mean difference (WMD) with 95% confidence interval (CI) using Stata11 (StataCorp, College Station, TX). The heterogeneity between the studies was tested using the Q test at the P<.10 level of significance and quantified by the I² statistic, which describes the inconsistency across studies. In general, the random‐effects model was used in the presence of significant heterogeneity. In fact, heterogeneity always exists in varying degrees. Thus, results from random‐effects model, which would be more conservative (and hence more appropriate), were presented in our meta‐analysis. We performed a sensitivity analysis, in which a single trial was omitted each time and the effect size was recalculated to investigate its influence on the overall effect size. Potential publication bias was assessed using Begg's funnel plots and Egger's regression test. P<.05 was considered statistically significant, except where otherwise specified.
Result
Search Results
Based on our search strategy, we searched 245 potential relevant articles, 29 of which were retrieved for further assessment, and 12 were excluded for the reasons shown in Figure 1. As a result, 17 studies were included, and the characteristics of the included studies are listed in the Table. The detailed selection process is presented in Figure 1.
Figure 1.
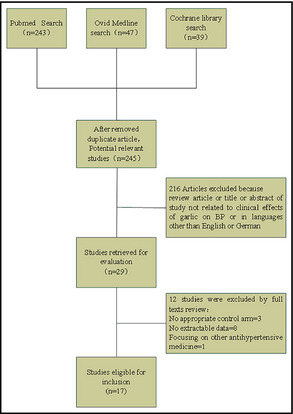
Flow diagram of search strategy and study selection. BP indicates blood pressure.
Table 1.
Charateristics of Trials Included in the Meta‐Analysis on the Effect of Garlic on BP
| Author, y | Trial Design | Patients, No. | BP | Interventional Method | Duration | Lacking Items Through Cochrane Checklist a | Total Points Quality Scale (maximum 9) a | BP Measurement (Lacking Items) | BP Measurement |
|---|---|---|---|---|---|---|---|---|---|
| Kandziora et al, 198823 | parallel | 40 | H | GP 600 mg/d+diuretic drug vs drug only | 12 wk | AC, PB, EB, D, ITT | 4 | DM, AH, RP | Supine and standing after 0, 2, 4, 8, and 12 wk; 2 measurements every visit |
| Auer et al, 199024 | Single‐blind parallel | 47 | H | GP 600 mg/d vs placebo | 12 wk | AC, EB, CG, D, ITT | 4 | DM, AH, RP, NR | BP measurements at office. Supine and standing at −2, 0, 4, 8, and 12 wk |
| Vorberg et al, 199025 | Single‐blind parallel | 40 | H+N | GP 900 mg/d vs placebo | 16 wk | AC, EB, CG, ITT | 5 | DM, AH, RP, NR | BP measurements at office. Supine and upright, before beginning, after washout, and at 2, 4, 8, 12, and 16 wk after baseline |
| Holzgartner et al, 199226 | Single‐blind parallel | 94 | H+N | GP 900 mg/d+lipid‐lowering drug vs lipid‐lowering drug | 12 wk | AC, EB, IT, ST | 5 | DM, AH, BP, RP, NR | BP measurement was not described |
| Jain et al, 199327 | Single‐blind parallel | 42 | N | GP 900 mg/d vs placebo | 12 wk | AC, EB, D, ITT | 5 | AH | Two sitting BP measurements were obtained after 10 minutes of rest in the clinic using an appropriate‐sized cuff, a conventional mercury sphygmomanometer, and standard recommended technique |
| Kiesewette et al, 199328 | Single‐blind parallel | 64 | H+N | GP 800 mg/d vs placebo | 12 wk | AC, EB, D, ITT | 5 | DM, AH, NR | BP was determined once a week according to the method of Riva Rocci, lying position after 10 min of rest |
| Saradeth et al, 199429 | Single‐blind parallel | 52 | N | GP 900 mg/d vs placebo | 15 wk | AC, EB, CG, D, ITT | 4 | DM, AH, BP, RP, NR | Resting BP was recorded using the traditional Riva Rocci method |
| Simons et al, 199530 | Single‐blind parallel | 30 | N | GP 900 mg/d vs placebo | 12 wk | AC, EB, CG, ITT | 5 | AH | BPs were measured after 5 min seated rest, used phase V diastolic, mean of two readings |
| Steiner et al, 199631 | Single‐blind parallel | 56 | H+N | AGE 2400 mg vs placebo | 12 wk | AC, EB, CG, D, ITT | 4 | BP, AH, RP, NR | BPs were monitored by manual measurement with sphygmomanometer |
| Adler et al, 19976 | Parallel | 23 | N | GP 900 mg/d vs placebo | 12 wk | AC, PB, EB, CG, ITT | 4 | DM, AH, RP, NR | Sitting BPs were taken at each visit by a digital BP monitor |
| Zhang et al, 200032 | Single‐blind parallel | 27 | N | GO 12.3 mg/d vs placebo | 12 wk | AC, EB, D, ITT | 6 | BP, AH | BPs were determined on the upper arm using a medical digital BP meter, 10–30 min in a quiet standardized environment, repeated low values were obtained. The means of the three lowest pulse rates plus associated systolic and diastolic BP values were utilized |
| William et al, 200533 | Double‐blind crossover | 30 | H+N | GP 600 mg/d vs placebo | 2 wk | AC EB ITT | 6 | DM, AH, BP, RP, NR | BP measurement was not described |
| Sobenin et al, 20097 | Double‐blind parallel | 50 | H | GP 600 mg/d vs placebo | 8 wk | AC EB ITT | 6 | DM AH RP | Morning BP, right and left arm, supine, sitting, standing every 4 wk |
| Ried et al, 20108 | Double‐blind parallel | 42 | H | AGE 960 mg vs placebo | 12 wk | EB | 8 | All reported | Office measurements by trained research nurse with automated sphygmomanometer while in the sitting position. The arm with higher reading was used. Mean of 3 readings at intervals of 30 s. Measurements at 0, 4, 8, and 12 wk |
| Ried et al, 20129 | Double‐blind parallel | 33 | H | AGE 960 mg vs placebo | 12 wk | EB | 8 | All reported | Office measurements by trained research nurse with automated sphygmomanometer. Sitting position. The arm with higher reading was used, mean of 3 readings at intervals of 30 s. Measurements at 0, 4, 8, and 12 wk |
| Nakasone et al, 201310, b | Double‐blind parallel | 40 | H | GP 300 mg/d vs placebo | 12 wk | AC | 8 | AH | Office measurements, automated sphygmomanometer. Sitting position. Left arm, repeated measurements at 2‐min intervals, until variance of 2 successive measurements ≤5 mm Hg. Mean values of 2 such measurements were then used. Measurements at 0, 4, 8, and 12 wk |
| Nakasone et al, 201310, b | Double‐blind parallel | 32 | N | GP 300 mg/d vs placebo | 12 wk | AC | 8 | AH | Office measurements, automated sphygmomanometer. Sitting position. Left arm, repeated measurements at 2‐min intervals, until variance of 2 successive measurements ≤5 mm Hg. Mean values of 2 such measurements were then used. Measurements at 0, 4, 8, and 12 wk |
| Ashraf et al, 201311 | Single‐blind parallel | 57 | H | GP 900 mg/d vs placebo | 24 wk | AC EB RB ITT D | 4 | DM, AH, BP, RP, NR | BP measurement was not described |
Abbreviations: AC, allocation concealment; AGE, aged garlic extract; AH, arm at heart level; BP, body position or blood pressure; CG, comparable groups; D, dropouts; DM, device mentioned; EB, evaluators blinded; GO, garlic oil; GP, garlic powder; H, hypertensive; H+N, hypertensive and normotensive; ITT, intention‐to‐treat analysis; N, normotensive; NR, number of reading; PB, patient blinding; RP, resting period; ST, same treatment of groups. aDutch Cochrane Centre: checklist for bias assessing of randomized controlled trials. bThis study included two separated randomized‐controlled trials involving hypertensive and normotensive patients.
Study Characteristics
Among the 17 trials, one included two separate random‐controlled trials10 that involved hypertensive patients and normotensive individuals, therefore this trial was counted as two trials. Therefore, our meta‐analysis included a total of 18 trials, seven of which comprised hypertensive individuals and six normotensive individuals, another five included both hypertensive and normotensive individuals. We evaluated measurements taken to test BP by five criteria: BP device, accuracy mentioned, body position reported, measurement with arm at heart level, rest period before measurement, and number of readings reported. The missing items are shown in the Table. Fourteen trials used garlic powder (mainly “kwai”), three trials used aged garlic extract, and another trial used garlic oil. One trial reported only DBP. Seventeen trials reported both SBP and DBP. Dosage of garlic powder ranged from 300 mg/d to 2400 mg/d and the duration of intervention ranged from 2 to 24 weeks. The total number of patients in the overall analysis for DBP was 799 and for SBP was 735.
Overall Analysis
Results showed a significant difference in favor of the garlic group, with garlic having a greater effect on reducing SBP by 3.75 mm Hg (95% CI, −5.04 to −2.45) compared with control (P<.001) (Figure 2). There was minor heterogeneity among the studies (I 2=30.7%, P=.111). Meta‐analysis of the effect of garlic on DBP also showed a significant difference between garlic and control groups, with the garlic group more effective in reducing DBP than placebo by 3.39 mm Hg (95% CI, −4.14 to −2.65; P<.001) (Figure 3); however, there was significant heterogeneity among the studies (I 2=67%, P=.000). The methodologic quality of trials can contribute to the heterogeneity across studies, so we evaluated methodologic quality of the selected trials using the nine quality criteria proposed by the Dutch Cochrane Centre in 2009 (Table). Trials that scored less than 5 were considered low quality and were then removed. We reanalyzed high‐quality trials and found that heterogeneity disappeared in both the SBP and DBP groups. Change in SBP was more obvious, with a reduction of 3.85 mm Hg (95% CI, −5.71 to −2.01, I 2=0.0%; P<.001) (Figure S1); the reduction in DBP was 1.59 mm Hg (95% CI, −2.91 to −0.26, I 2=8.4%; P=.019) (Figure S2).
Figure 2.
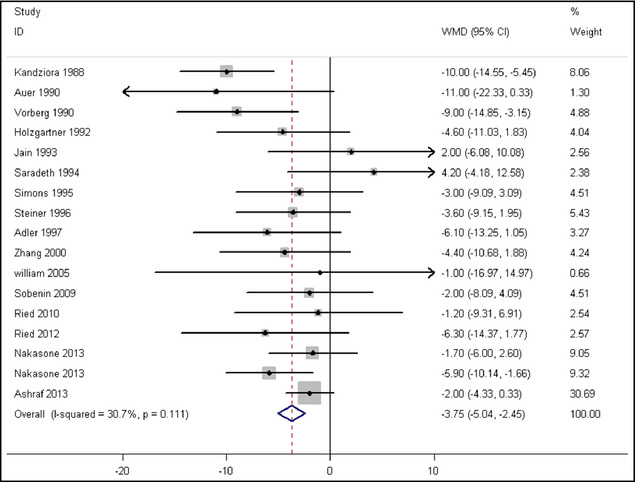
Effect of garlic on systolic blood pressure. WMD indicates weighted mean difference; CI, confidence interval; I‐squared, inconsistency.
Figure 3.
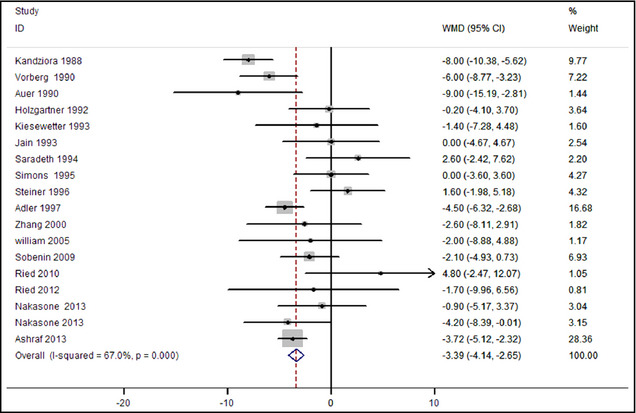
Effect of garlic on diastolic blood pressure. WMD indicates weighted mean difference; CI, confidence interval; I‐squared, inconsistency.
Subgroup and Sensitivity Analysis
To further explore the effect of garlic on BP, we conducted a subgroup analysis in the hypertensive and normotensive groups. To avoid confusion of results, trials in which BP were not recorded separately for hypertensive and normotensive people were excluded. Meta‐analysis by subgroup showed that in patients with hypertension, the mean reduction in SBP was 4.4 mm Hg (95% CI, −7.37 to −1.42, I 2=0.0%; P=.004) and there was no significant reduction for DBP, but there existed heterogeneity (I 2=32.3%) (Figures 4 and 5). We conducted a sensitivity analysis and found that one trial8 may generate heterogeneity; therefore, we removed this trial and the heterogeneity disappeared and the DBP reduction was 2.68 mm Hg (95% CI, −4.93 to −0.42, I 2=0.0%; P=.020) (Figure S3) in the garlic group. Subgroup analysis of studies in the normotensive group showed no significant difference on SBP and DBP between the garlic and placebo groups with no heterogeneity among studies.
Figure 4.
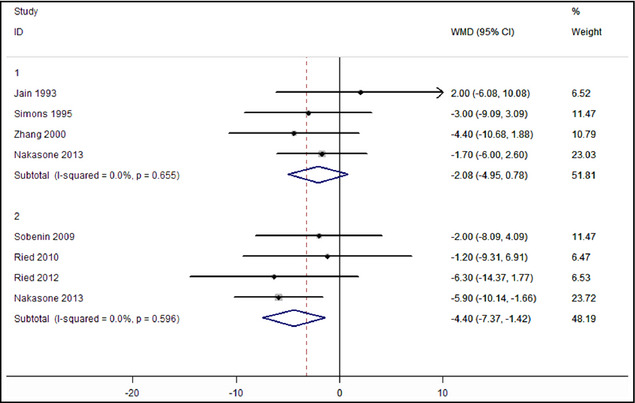
Subgroup analysis on the effect of garlic on systolic blood pressure. 1 indicates normotensive; 2, hypertensive; WMD, weighted mean difference; CI, confidence interval; I‐squared, inconsistency.
Figure 5.
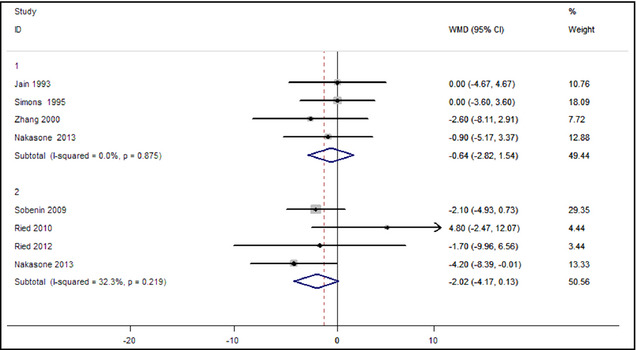
Subgroup analysis on the effect of garlic on diastolic blood pressure. 1 indicates normotensive; 2, hypertensive; WMD, weighted mean difference; CI, confidence interval; I‐squared, inconsistency.
Dose‐Response Relationship and Duration
There were two trials that investigated multiple levels of garlic intake. Garlic supplementation was presented at 240 mg, 480 mg, and 960 mg daily for 12 weeks in the first trial.9 The maximum antihypertensive effect of garlic was produced by 480 mg garlic at week 12. There was no obvious trend with increased dose at week 4 (Figure S4). In another trial,11 patients received garlic supplementation at the doses of 300 mg, 600 mg, 900 mg, 1200 mg, and 1500 mg per day for 24 weeks. BP was measured at week 0, week 12, and week 24. The SBP in the garlic group decreased more significantly with increased dose and duration (Figure S5). However, there were only two papers that aimed to study the dose‐response relationship and duration, and the garlic supplement used in the two trials were different. As a result, it was inappropriate to pool the data together, and only the dose and duration effect on SBP in the two trials were used.
Publication Bias
There was little evidence of publication bias with regard to garlic supplementation in relation to BP (including SBP and DBP), as indicated by the Begg rank correlation test (P>.05) and the Egger linear regression test (P>.05).
Discussion
Garlic has been used worldwide as traditional food, and has been considered to have therapeutic effects on some human diseases.15 At first, garlic was thought to be useful in decreasing serum cholesterol concentration.16 Recently, several studies have shown that garlic supplements can decrease BP.6, 7, 8, 9, 10, 11 However, the meta‐analysis by Ackermann and colleagues found that garlic had no significant effects on BP.12 Nine years later, another meta‐analysis showed that garlic preparations were superior to placebo in reducing BP in individuals with hypertension.14 Including some new trials, we performed an updated meta‐analysis and found that garlic supplements caused significant reduction in BP and that both SBP and DBP can be lowered at different degrees. However, heterogeneity existed among studies, especially in the DBP group. We re‐analyzed the data after exclusion of the low‐quality trials and no heterogeneity existed and the result still showed that both SBP and DBP were significantly decreased. To avoid confusion of results, studies that mixed hypertension and normotension participants together were excluded. Meta‐analysis of subgroups showed that garlic supplementation led to a significant fall in SBP in the hypertensive group but no significant decrease in the normotensive group. However, with regard to DBP, no significant change was shown in either the hypertensive or normotensive groups. Because of the heterogeneity in the DBP group, we conducted a sensitivity analysis and found that one trial8 may generate heterogeneity, and when this trial was removed, we re‐calculated the meta‐analysis and found that the heterogeneity disappeared and a significant DBP reduction was shown in the hypertensive group. Our findings were consistent with a previous meta‐analysis by Ried and colleagues in 2008.14 We believe our meta‐analysis has some advantages as it included new trials7, 8, 9, 10, 11 and evaluated the methodological quality of the selected trials using the nine quality criteria proposed by the Dutch Cochrane Centre in 2009 (Table). We reanalyzed the high‐quality trials after the low‐quality trials were removed and found that a significant reduction in both SBP and DBP still existed in the garlic‐treat group. Our study provides further support for garlic supplementation in hypertensive patients.
The mechanism of garlic's antihypertensive effect is still not clear. There are some hypotheses, however. Increased oxidative stress can induce endothelial dysfunction, and can eventually lead to hypertension.17, 18 Garlic contains several bioactive compounds, including allicin, which has antioxidant activity.19 Some studies showed that allicin could lower BP.20 Therefore, garlic supplements may ameliorate hypertension by its antioxidant effect. Garlic may elicit its antihypertensive effects by inhibition of angiotensin‐converting enzymes (ACEs). Sharifi and colleagues found that garlic and allicin could decrease ACE activity in a hypertensive rat model, and they also found that compared with the control group, a significant reduction in SBP was noted in rats treated with garlic.2 However, several dipeptides extracted from garlic have also been reported to inhibit ACE,21 and allicin may not be the only compound that has ACE inhibitory activity. Nonetheless, garlic can decrease BP by inhibiting ACE.
We also investigated the dose‐response relationship and duration in the trials. The dosage of garlic supplement in the hypertension groups was 600 mg or 900 mg in most of the studies. We cannot find a dose‐response relationship in the meta‐regression. Moreover, it is known that the dose‐response relationship from meta‐regression should be viewed as exploratory and could be prone to confounding.22 We tried to observe the dose‐effect relationship from trials with multiple levels of garlic intake. There were two trials that studied at least three levels of garlic intake. The first study by Ried and colleagues in 20129 was a double‐blind, randomized, placebo‐controlled trial comprising 79 participants with systolic hypertension in which 240 mg, 480 mg, and 960 mg daily garlic supplements were administered for 12 weeks. Change in SBP in the 240‐mg group was not significantly different from placebo. No obvious reduction was found in SBP in the 960‐mg group compared with the 480‐mg group. The maximum effect was produced by garlic in 480 mg. Possible reasons were as follows: (1) poorer compliance and less tolerability was reported in the 960‐mg group; (2) whether garlic in 480 mg has exerted its maximum effect was unknown, but other evidence suggests that this was unlikely. In Ashraf's study,11 hypertensive patients received garlic supplementation at the doses of 300 mg, 600 mg, 900 mg, 1200 mg, and 1500 mg per day for 24 weeks. Data were compared at week 12 and week 24. BP decreased with the increased intake of garlic, and the maximum effect was produced by 1500 mg of garlic at week 24. Unfortunately, the quality of the study was poor. Because the studies reported multiple dosages and the duration was limited, it was difficult for us to detect an association between the dosage and duration with BP change. More trials should be conducted to explore this relationship in the future.
Study Strengths and Limitations
Our meta‐analysis included several studies in which the patients were given hypotensive medicine, which may influence the hypotensive effect of garlic, but only patients who were already taking conventional antihypertensive medication and not planning to change the prescribed medication during the trial were included. In addition, heterogeneity was not reported after elimination of a low‐quality study.
The garlic supplements were not the same among the 17 trials. The supplements included garlic powder, aged garlic extract, and garlic oil, which may have different effects on BP. However, the active ingredients in the different garlic supplements is allicin, and, in our meta‐analysis, most trials used garlic powder in dosages ranging from 300 mg/d to 900 mg/d, providing 1.8 mg to 5.4 mg of allicin. In one trial, Zhang and colleagues used garlic oil, which is an allicin derivative produced by the steam‐distillation process. Three trials used aged garlic extract (Kyolic and Wakunaga of America Kyolic), which may contain 1% to 2% of allicin.
There might be issues related to the measurement of BP in these trials and this is crucial to the research question. In some papers, the method of BP taking were described in detail. In the trial by Ried and colleagues, for example, BP was tested by trained nurse, and the reported BP was the average of three times repeated measurements using standard techniques. However, in some trials, BPs were measured only once, and some papers did not describe the manner of BP testing (Table 1. This may have influenced the results of the studies.
Finally, one study was included twice,10 which may have increased its weight in the meta‐analysis; however, two independent trials were performed in this study and were considered as such.
Conclusions
Our meta‐analysis suggests that garlic supplementation is superior to placebo in reducing BP in hypertensive patients, especially in those with high SBP. More trials should be performed to explore the association between dosage and duration of garlic and change in BP. The safety of long‐term use should also be investigated before garlic is used as conventional therapy for hypertension.
Disclosures
The authors report no specific funding in relation to this research and no conflicts of interest to disclose.
Supporting information
Figure S1. Effect of garlic on systolic blood pressure after excluding low quality trials.
Figure S2. Effect of garlic diastolic blood pressure after excluding low quality trials.
Figure S3. Effect of garlic on diastolic blood pressure in normotensive/hypertensive after excluding trial hold by Ried in 2010.
Figure S4. Dose‐response relationship and duration in the trial hold by Reid et al in 2012.
Figure S5. Dose‐response relationship and duration in the trial hold by Ashraf et al in 2013.
J Clin Hypertens (Greenwich). 2015;17:223–231. DOI: 10.1111/jch.12473 © 2015. Wiley Periodicals, Inc.
Reference
- 1. Fagard RH. Resistant hypertension. Heart. 2012;98:254–261. [DOI] [PubMed] [Google Scholar]
- 2. Benavides GA, Squadrito GL, Mills RW, et al. Hydrogen sulfide mediates the vasoactivity of garlic. Proc Natl Acad Sci USA. 2007;104:17977–17982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sharifi AM, Darabi R, Akbarloo N. Investigation of antihypertensive mechanism of garlic in 2K1C hypertensive rat. J Ethnopharmacol. 2003;3:219–224. [DOI] [PubMed] [Google Scholar]
- 4. Al‐Qattan KK, Khan I, Alnaqeeb MA, Ali M. Mechanism of garlic (Allium sativum) induced reduction of hypertension in 2K‐1C rats: a possible mediation of Na/H exchanger isoform‐1. Prostaglandins Leukot Essent Fatty Acids. 2003;69:217–222. [DOI] [PubMed] [Google Scholar]
- 5. Lanzotti V. The analysis of onion and garlic. J Chromatogr A. 2006;2:3–22. [DOI] [PubMed] [Google Scholar]
- 6. Adler AJ, Holub BJ. Effect of garlic and fish‐oil supplementation on serum lipid and lipoprotein concentrations in hypercholesterolemic men. Am J Clin Nutr. 1997;65:445–450. [DOI] [PubMed] [Google Scholar]
- 7. Sobenin IA, Andrianova IV, Fomchenkov IV, et al. Time‐released garlic powder tablets lower systolic and diastolic blood pressure in men with mild and moderate arterial hypertension. Hypertens Res. 2009;32:433–437. [DOI] [PubMed] [Google Scholar]
- 8. Ried K, Frank OR, Stocks NP. Aged garlic extract lowers blood pressure in patients with treated but uncontrolled hypertension: a randomised controlled trial. Maturitas. 2010;67:144–150. [DOI] [PubMed] [Google Scholar]
- 9. Ried K, Frank OR, Stocks NP. Aged garlic extract reduces blood pressure in hypertensives: a dose‐response trial. Eur J Clin Nutr. 2013;67:64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nakasone Y, Nakamura Y, Yamamoto T, Yamaguchi H. Effect of a traditional Japanese garlic preparation on blood pressure in prehypertensive and mildly hypertensive adults. Exp Ther Med. 2013;5:399–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ashraf R, Khan RA, Ashraf I, Qureshi AA. Effects of Allium sativum (garlic) on systolic and diastolic blood pressure in patients with essential hypertension. Pak J Pharm Sci. 2013;26:859–863. [PubMed] [Google Scholar]
- 12. Ackermann RT, Mulrow CD, Ramirez G, et al. Garlic shows promise for improving some cardiovascular risk factors. Arch Intern Med. 2001;161:813–824. [DOI] [PubMed] [Google Scholar]
- 13. Silagy CA, Neil HA. A meta‐analysis of the effect of garlic on blood pressure. J Hypertens. 1994;12:463–468. [PubMed] [Google Scholar]
- 14. Ried K, Frank OR, Stocks NP, et al. Effect of garlic on blood pressure: a systematic review and meta‐analysis. BMC Cardiovasc Disord. 2008;8:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rivlin RS. Historical perspective on the use of garlic. J Nutr. 2001;131:951S–954S. [DOI] [PubMed] [Google Scholar]
- 16. Gebhardt R, Beck H, Wagner K. Inhibition of cholesterol biosynthesis by allicin and ajoene in rat hepatocytes and HepG2 cells. Biochim Biophys Acta. 1994;1213:57–62. [DOI] [PubMed] [Google Scholar]
- 17. Cai H, Harrison DG. Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res. 2000;87:840–844. [DOI] [PubMed] [Google Scholar]
- 18. Laursen JB, Rajagopalan S, Galis Z, et al. Role of superoxide in angiotensin II‐induced but not catecholamine‐induced hypertension. Circulation. 1997;95:588–593. [DOI] [PubMed] [Google Scholar]
- 19. Prasad K, Laxdal VA, Yu M, Raney BL. Antioxidant activity of allicin, an active principle in garlic. Mol Cell Biochem. 1995;148:183–189. [DOI] [PubMed] [Google Scholar]
- 20. Ali M, Al‐Qattan KK, Al‐Enezi F, et al. Effect of allicin from garlic powder on serum lipids and blood pressure in rats fed with a high cholesterol diet. Prostaglandins Leukot Essent Fatty Acids. 2000;62:253–259. [DOI] [PubMed] [Google Scholar]
- 21. Seutsuna K. Isolation and characterization of angiotensin I‐converting enzyme inhibitor dipeptides derived from Allium sativum L (garlic). J Nutr Biochem. 1998;9:415–419. [Google Scholar]
- 22. He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: cochrane systematic review and meta‐analysis of randomised trials. BMJ. 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 23. Kandziora J. The blood pressure lowering and lipid lowering effect of a garlic preparation in combination with a diuretic. Artzliche Forschung. 1988;35:3–8. [Google Scholar]
- 24. Auer W, Eiber A, Hertkorn E, et al. Hypertension and hyperlipidaemia: garlic helps in mild cases. Br J Clin Pract Suppl. 1990;69:3–6. [PubMed] [Google Scholar]
- 25. Vorberg G, Schneider B. Therapy with garlic: results of a placebo‐controlled, double‐blind study. Br J Clin Pract Suppl. 1990;69:7–11. [PubMed] [Google Scholar]
- 26. Holzgartner H, Schmidt U, Kuhn U. Comparison of the efficacy and tolerance of a garlic preparation vs. bezafibrate. Arzneimittelforschung. 1992;42:1473–1477. [PubMed] [Google Scholar]
- 27. Jain AK, Vargas R, Gotzkowsky S, McMahon FG. Can garlic reduce levels of serum lipids? A controlled clinical study Am J Med. 1993;94:632–635. [DOI] [PubMed] [Google Scholar]
- 28. Kiesewetter H, Jung F, Jung EM, et al. Effects of garlic coated tablets in peripheral arterial occlusive disease. Clin Investig. 1993;71:383–386. [DOI] [PubMed] [Google Scholar]
- 29. Saradeth T, Seidl S, Resch KL, Ernst E. Does garlic alter the lipid pattern in normal volunteers? Phytomedicine. 1994;1:183–185. [DOI] [PubMed] [Google Scholar]
- 30. Simons LA, Balasubramaniam S, von Konigsmark M, et al. On the effect of garlic on plasma lipids and lipoproteins in mild hypercholesterolaemia. Atherosclerosis. 1995;113:219–225. [DOI] [PubMed] [Google Scholar]
- 31. Steiner M, Khan AH, Holbert D, Lin RI. A double‐blind crossover study in moderately hypercholesterolemic men that compared the effect of aged garlic extract and placebo administration on blood lipids. Am J Clin Nutr. 1996;64:866–870. [DOI] [PubMed] [Google Scholar]
- 32. Zhang XH, Lowe D, Giles P, et al. A randomized trial of the effects of garlic oil upon coronary heart disease risk factors in trained male runners. Blood Coagul Fibrinolysis. 2001;12:67–74. [DOI] [PubMed] [Google Scholar]
- 33. Williams MJ, Sutherland WH, McCormick MP, et al. Aged garlic extract improves endothelial function in men with coronary artery disease. Phytother Res. 2005;19:314–319. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Effect of garlic on systolic blood pressure after excluding low quality trials.
Figure S2. Effect of garlic diastolic blood pressure after excluding low quality trials.
Figure S3. Effect of garlic on diastolic blood pressure in normotensive/hypertensive after excluding trial hold by Ried in 2010.
Figure S4. Dose‐response relationship and duration in the trial hold by Reid et al in 2012.
Figure S5. Dose‐response relationship and duration in the trial hold by Ashraf et al in 2013.


