Evidence from comprehensive systematic reviews and high‐quality studies demonstrates that excess salt intake causes raised blood pressure, a major risk factor for cardiovascular diseases.1, 2 Worldwide, nearly every country (181 of 187) consumes in excess of the World Health Organization (WHO)–recommended maximum intake of 5 g of salt per day.3 The United Nations and WHO have therefore called on Member States to reduce mean population salt intake by 30% by 2025.4 Between 2010 and 2014, the number of countries reporting some form of national salt reduction initiative more than doubled from 32 to 75.5 There are also other efforts to reduce population salt intake at subnational organizational, community, state, and provincial levels. An increasing number of programs are now being documented in order to share experiences and outcomes. It is within this context that this review aims to appraise studies reporting on the implementation of salt reduction initiatives that were identified as part of the Science of Salt Weekly systematic review series, with a view to informing future implementation of interventions to lower population salt consumption.6 A companion review aims to regularly summarize the growing volume of studies reporting the effects of salt intake on health outcomes.7
Methodology
Articles are identified on a weekly basis through a MEDLINE search strategy that was formulated using a Cochrane Collaboration systematic review on dietary salt and health.2, 8 The search retrieved studies on the implementation of salt reduction strategies from June 2, 2015 to October 31, 2015. The methodological approach used to identify and evaluate the literature in this review has been described in a previously published protocol.6
The review includes studies reporting or evaluating salt reduction interventions and studies that provide information pertinent to the design of salt reduction interventions. The studies are considered in four broad categories: (1) studies evaluating the impact of salt reduction interventions; (2) descriptive studies describing salt reduction initiatives being implemented; (3) studies measuring population salt intake, salt content in foods, sources of dietary salt, or consumers' knowledge, attitudes, and behaviors (KAB) related to salt; and (4) economic evaluations or modeling studies of salt reduction strategies. Overviews of regional support activities without details of specific intervention programs were excluded. Each study was appraised for risk of bias (ROB) and quality. To assess the ROB for studies evaluating the impact of population‐wide interventions, an adapted version of the Cochrane ROB tool developed for the review of population‐level interventions in government jurisdictions was used.9, 10 The same tool was used for studies measuring salt content in foods and studies examining the association between salt knowledge and intake. In order to determine how accurately population salt intake was measured, an ROB assessment was made based on WHO recommendations for measurement of population sodium intake,11, 12 National Heart, Lung, and Blood Institute of the US Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies,13 and the ROB assessment tool developed previously for intervention studies.10 A modified version of standard quality‐assessment guidelines for decision analytic modeling studies was used to assess the quality of modeling studies.14 It was not possible to assess the ROB for reviews of salt reduction initiatives being implemented nationally or regionally, thus the quality of these reviews was assessed against the draft framework defined by the WHO SALT toolkit for salt reduction.
Results
The MEDLINE search identified 2583 possibly relevant studies, of which 265 full‐text articles were assessed against the eligibility criteria after elimination of irrelevant studies based on screening of the titles and abstracts (Figure). Ultimately, there were 11 studies included in this review: four reported interventions being implemented (one of which also evaluated a pilot salt reduction intervention)15, 16, 17, 18 two cross‐sectional studies, which measured population salt intake19, 20 two repeated cross‐sectional studies on salt content of foods21, 22 one single cross‐sectional study on salt content in foods23 one cross‐sectional study on the association of salt knowledge and daily salt intake24 and one scenario modeling study.25 The appraisals of each study can be found as part of the online supplementary information (Appendix S1).
Figure 1.
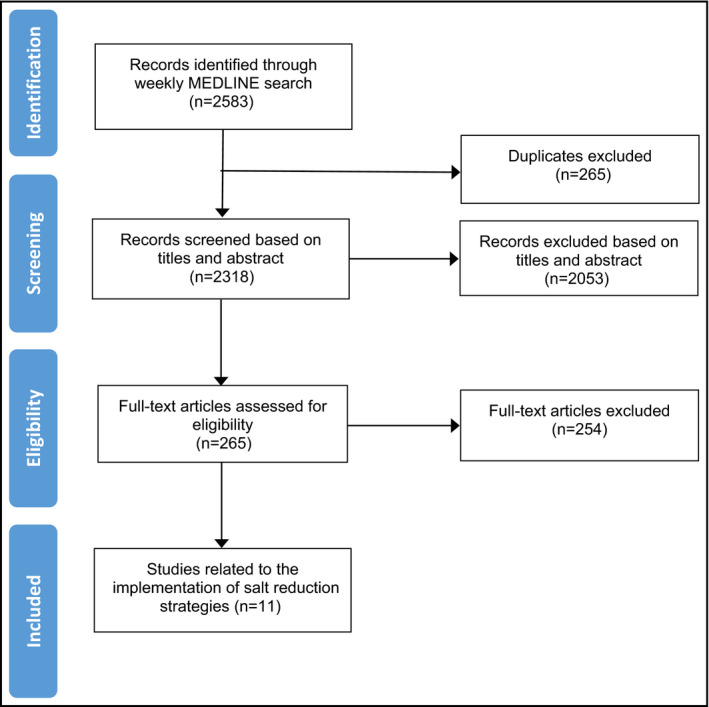
Studies included between June and October 2015.
Studies Evaluating the Impact of Salt Reduction Interventions
Developing a National Salt Reduction Strategy for Mongolia
Enkhtungalag B, Batjargal J, Chimedsuren O, et al. Cardiovasc Diagn Ther. 2015;5:229–237.
Summary. Enkhtungalag and colleagues outline the development of a proposed national salt reduction strategy in Mongolia, including baseline population assessment of adult salt intake and pilot intervention strategies. The review includes a description of a pilot initiative (Pinch Salt Mongolia), which aimed to reduce salt intake among employees of three food‐producing factories during a period of 2 years. The intervention included health and nutrition education for staff as well as reformulation of foods at company canteens and workers' kitchens. Pre‐intervention and post‐intervention 24‐hour urine samples were collected for 240 employees who also completed a questionnaire about their KAB regarding salt. Results demonstrated a significant reduction in mean salt intake for employees from 11.48 g (standard deviation, 7.32 g) (sodium 4592 mg) per day in 2011 to 8.65 g (standard deviation, 4.26 g) (sodium 1704 mg) per day in 2013 and improved consumer knowledge about which foods were high in salt. The salt content of meals served in company kitchens also reduced over the period.
Comment. Pinch Salt Mongolia is a pilot study that tests the feasibility of a workplace salt reduction initiative in Mongolia. There is limited detail about the pilot study as it is reported as part of a broader review of Mongolia's strategy. It is unclear from the paper how they were sampled and recruited and whether the sample was representative of the entire staff. Because of its uncontrolled study design, it is also likely to have a high risk of bias. Although the study showed a large reduction in salt intake based on 24‐hour urine samples, which is usually a reliable method for assessment, it was unclear whether all the urine collections were complete. However, the results align with improvements in knowledge and the salt content of meals served. This pilot study usefully informs the development of a national salt reduction strategy.
Studies Reporting Salt Reduction Initiatives Being Implemented
Salt Reduction in Australia: From Advocacy to Action
Webster J, Trieu K. Dunford E, et al. Cardiovasc Diagn Ther. 2015;5:207–218.
Summary. This paper provides an overview of salt reduction activities in Australia against an existing framework for salt reduction strategies and identifies gaps where further action is required. It describes both nongovernmental organizations (NGOs) and government action over the past decade and states that Australia lacks a government‐coordinated national implementation program, which is required to meet global salt reduction targets. Existing estimates of salt intake are between 8 g/d and 9 g/d (sodium 3200–3600 mg). However, there is no nationally representative baseline survey and no agreed upon mechanisms for ongoing monitoring. While food industry reformulation has been promoted over several decades by government and NGOs and reductions in salt content in some food categories have been measured, the government's Food and Health Dialogue did not set salt level targets in all key product categories. The more recent Health Star Rating system (a front‐of‐pack labeling scheme) has the potential to support improved consumer choices relating to salt as well as to drive food industry reformulation. There are plans for a consumer education campaign to support the rollout of the scheme. In Victoria, the Victorian Health Promotion Foundation has launched a state‐wide salt reduction strategy with a view to supporting existing federal government programs, but action in other states is currently limited to policies or guidelines in schools or hospitals. It is not clear what the impact of these is likely to be.
Comment. The authors conclude that additional efforts and more robust national monitoring mechanisms will be required for Australia to achieve a 30% reduction in salt by 2025. The overview of salt reduction initiatives in Australia over the past decade is comprehensive. It is based on a review of the literature and documentation of stakeholder activities and assesses these activities against an existing framework for salt reduction. It also refers to previously peer‐reviewed evidence to support claims of reductions in salt content in foods. However, it is written by members of advocacy organizations and state organizations advocating for greater federal government action on salt reduction in Australia, therefore it should be interpreted on that basis.
An Overview of Salt Intake Reduction Efforts in the Gulf Cooperation Council Countries
Alhamad N, Almalt E, Alamir N, et al. Cardiovasc Diagn Ther. 2015;5:172–177.
Summary. The authors provide an overview of salt reduction activities to date in six Gulf Cooperation Council countries: Bahrain, Kuwait, Oman, Qatar, Saudi Arabia, and the United Arab Emirates. Government initiatives to develop salt reduction implementation actions, primarily strategies to reduce salt in bread, are described. Current measurements of salt intake are 7 g/d to 8 g/d (sodium 2800–3200 mg; estimated based on spot urine) in Bahrain, 8 g/d to 10 g/d (sodium 3200–4000 mg; estimated based on dietary survey/food assessment) in Kuwait, and 11 g/d to 12 g/d (sodium 4400–4800 mg; estimated based on dietary survey) in Oman. Salt content in bread was assessed for different countries and ranged from 1.52 g salt/100 g (sodium 608 mg/100 g) in flat Arabic breads in Kuwait to 0.28 g salt/100 g (sodium 112 mg/100 g) in white bread in Jordan. The contribution of bread to total dietary salt ranged from 14.8% in Qatar to 53.9% in Morocco. All six countries have programs in place or are initiating programs to reduce salt in breads. The paper reports a 20% reduction in salt content in bread in Kuwait in 2013 and a 10% reduction in the salt content of bread in Qatar. All other countries are still in the early stages of implementation and have not yet reported reductions. No food labeling or consumer awareness initiatives are described.
Comment. The paper reviews existing activities in six countries with a focus on government leadership and reducing salt in bread, which is a main contributor to salt intake in the region. The authors conclude that regional salt reduction efforts vary between the early stages of planning to an achieved 20% reduction in salt content of bread in Kuwait. The methods used to monitor the change in salt content of breads in Kuwait and Qatar are not explained, and therefore the strength of the evidence is unclear. The paper is also written by representatives of government ministries responsible for implementing the salt reduction strategies in their respective countries, therefore the study should be interpreted in that context.
Sodium Intake Reduction Efforts in Lebanon
Almedawar MM, Nasreddine L, Olabi A, et al. Cardiovasc Diagn Ther. 2015;5:178–185.
Summary. The authors provide an overview of the Lebanese Action on Sodium and Health (LASH) strategy led by an academic institution, which began by undertaking a situational analysis to prompt salt reduction action. Population salt intake was estimated to be between 7.25 g/d and 7.83 g/d (sodium 2900–3132 mg) from national dietary survey data. Processed foods, including bread (26%), processed meat (12%), and dairy products (9%), were found to be the major sources of sodium in the diet. In addition, the authors report poor KAB toward reduction in dietary sodium intake. Consumer campaigns were implemented, which provided educational materials such as shopping guides, posters, and information leaflets aimed at addressing the gaps in knowledge and changing behaviors. Ministry‐selected food producers have agreed to undertake a pilot salt reduction initiative to reduce salt content in bread products, cured meats, pickles, olives, and cheeses. In addition, LASH has suggested a number of steps to standardize sodium levels in bread.
Comment. The paper reports LASH's strategy to reduce sodium intake in Lebanon, which has resulted in government action to reduce salt in some products. Baseline data on salt consumption and sources of salt in the diet were measured through a nationally representative dietary survey, so while the assessment of salt intake is likely to be an underestimation because of the tendency to underreport consumption and the inaccurate reporting of discretionary salt use, the data are nonetheless valuable in informing policy makers on the approach to reduce salt intake. Current consumers' KAB related to salt was measured in a random sample of 442 participants recruited from supermarkets in Beirut.26 These results were used to inform the development of the strategy. The authors are representatives of LASH, which developed the salt reduction strategy, therefore readers should interpret the study findings within this context. However, the recommended actions to reduce sodium intake in Lebanon do appear to be guided by the best available evidence.
Studies Measuring Population Salt Intake
Geographic and Socioeconomic Variation of Sodium and Potassium Intake in Italy: Results from the MINISAL‐GIRCSI Programme
Cappuccio FP, Ji C, Donfrancesco C, et al. BMJ Open. 2015;5:e007467.
Summary. The MINISAL‐GIRCSI survey measured sodium and potassium excretion in a subsample of participants from the Cardiovascular Epidemiology/Health Examination Survey, which included a randomly selected sample stratified by age and sex for each region of Italy. Sodium intake was estimated by a single 24‐hour urine collection from each participant, with incomplete samples excluded. A final sample of 3857 was included in the analysis. Overall, the median daily salt intake was approximately 9 g and the median urinary potassium excretion was 2246.4 mg/d. Bayesian geoadditive mixed models were used to assess variation by region and socioeconomic status. Results showed that there was significant regional variation, with higher intakes in the southern regions of Italy. Potassium excretion was higher in the central and southern regions of Italy. Variation by socioeconomic status was also identified with significantly higher intakes in lower socioeconomic groups defined by occupation and educational attainment (independent of age, sex, body mass index, hypertensive status, and self‐reported physical activity, alcohol consumption, and smoking status). Potassium excretion was lower in those with lower educational attainment.
Comment. This large study includes a representative sample of adults from Italy and estimates sodium and potassium intake using the “gold standard” method: 24‐hour urine collection. The methodology, including exclusions of incomplete collections based on low urine volume and creatinine excretion levels, is consistent with best‐practice guidelines produced by WHO, and there appears to be low risk of bias. The finding that salt intake is higher in disadvantaged social groups is in line with studies from other countries27, 28 and highlights the importance of designing salt reduction initiatives that minimize socioeconomic disparities.
Current Daily Salt Intake in Germany: Biomarker‐Based Analysis of the Representative DEGS Study
Johner SA, Thamm M, Schmitz R, et al. Eur J Nutr. 2015;54:1109–1115.
Summary. The study estimated the median daily salt intake in Germany using the German Health Interview and Examination Survey for Adults (DEGS) study conducted from 2008 to 2011 in residents aged 18 to 79 years. The survey is made up of a random sample from local population registries and participants from a previous study performed in 1998. The study obtained sodium and creatinine measurements from spot urine samples collected in 6962 participants and estimated 24‐hour sodium excretion by adjusting the sodium to creatinine ratio by age‐ and sex‐specific 24‐hour creatinine excretion reference values. Twenty‐four–hour creatinine excretion reference values were generated from the Verbundstudie Ernährungserhebung und Risikofaktoren–Analytik (VERA) study, which obtained 24‐hour urine samples from 2006 patients aged 18 to 88 years in 1986 and 1988. Based on this method, the estimated median salt intake in men was 10 g/d and 8.4 g/d in women. A total of 80% of men and 70% of women in Germany exceeded the nationally recommended salt intake limit of 6 g/d.
Comment. The study estimated median salt intake in the German population from a large survey (DEGS study) of participants made up of a random sample drawn from local population registries and is likely to be representative. The VERA study collected 24‐hour urine from a representative subsample taken randomly from a national survey and appropriate exclusions (based on 24‐hour urine volume and collection time) were made to generate the age‐ and sex‐specific 24‐hour creatinine reference values, which were used to estimate the 24‐hour sodium excretion from spot samples. Although the gold standard 24‐hour urine collection was not used, the large sample size and the use of population‐specific creatinine reference values help minimize the variability caused by using spot samples, meaning it is likely to be a reasonable estimate of the median salt intake in German adults. The study findings demonstrate that most of the German population likely exceeds the recommended daily salt intake by a considerable amount, and a national salt reduction strategy is needed to improve population health.
Studies Measuring Salt Content in Foods and Sources of Salt
Changes in the Sodium Content of New Zealand Processed Foods
Monro D, Mhurchu CN, Jiang Y, et al. Nutrients. 2015;7:4054–4067.
Summary. This study investigated the changes in the sodium content of processed foods in New Zealand between 2003 and 2013, using two cross‐sectional studies. The study collected nutrient data of nine food categories that were major contributors of sodium in the diet from four major supermarkets in Dunedin in 2003 (n=323) and two major supermarkets in Auckland in 2013 (n=885). The data on sodium content were obtained from Nutrition Information Panels (NIPs) on product packages. The study found no significant difference in the sodium content of all collected foods in 2003 and 2013. In addition, there were 182 products that were available for sale in both years (matched products), which were compared using paired t tests. There was no significant difference in the mean sodium content of these products either (454 mg/100 g in 2003 and 399 mg/100 g in 2013; P=.22).
Comment. This study showed no change in the sodium content of processed foods between 2003 and 2013. It is unclear how comparable the supermarkets surveyed in 2003 and 2013 in different cities were, or how closely they represented the whole food supply in New Zealand. Product sales information was not included in the analysis and could have provided additional insight if available. Sodium values were obtained from NIPs, which is a reasonable method of collecting nutrient data. Despite some limitations, acknowledged by authors, the study provides useful information about the mean sodium content of products and highlights foods on which to target reformulation efforts. The study findings also suggest the need for stronger efforts to lower the salt content in foods in New Zealand.
A Comparison of the Sodium Content of Supermarket Private‐Label and Branded Foods in Australia
Trevena H, Neal B, Dunford E, et al. Nutrients. 2015;7:7027–7041.
Summary. The authors compare the sodium content of private‐label products against branded products available in four major Australian supermarkets in Sydney. The study collected nutrient data for 15 food categories that typically contain added salt in 2011 (n=4501), 2012 (n=5184), and 2013 (n=5995). The data on sodium content were obtained from the NIPs on product packages and mean sodium values in private‐label and branded products were compared in: (1) all products in 2013; (2) products present in both 2011 and 2013; and (3) new products only available in 2013, using paired and unpaired t tests. The study found that the mean sodium content of private‐label products was significantly lower than branded products by 17% in all products available in 2013 and 11% in newly available products in 2013. There was a significant reduction, although less than 2%, in the mean sodium content of both private and branded products between 2011 and 2013. There was no significant difference in the change in sodium content between private‐label and branded products during this period.
Comment. This study showed that private‐label (supermarket) products had significantly lower sodium content than branded products and that there had been a small but significant reduction in the sodium content of both private‐label and branded products during the 3‐year study period. The large number of products (n=15,680) collected from all four of the major supermarkets suggest that they are representative of products available in Australia and that the study likely provides a fair comparison over time. Sodium values were obtained from NIPs, which is a reasonable method of collecting nutrient data. However, there was no use of sales information, which would have provided better insight into the likely effects of the observed differences on population health. Nevertheless, the main finding that private‐label products contain less sodium than branded products is useful and highlights the importance of further research to understand how these achievements can be extended to branded products.
Sodium Content in Processed Foods in Argentina: Compliance With the National Law
Allemandi L, Tiscornia MV, Ponce M, et al. Cardiovasc Diagn Ther. 2015;5:197–206.
Summary. This study compared the sodium content of processed food products against the maximum levels set by the national law in Argentina as a baseline against which the law's implementation can be assessed. Nutrient data were collected from 14 food groups from a leading supermarket chain in Buenos Aires in 2014 (n=1655) using a smartphone data collection application. A total of 292 products could be matched and compared against established maximum levels set by the national law. Results showed that maximum levels have already been met by most of the food groups. Fifteen of 18 food categories had median sodium content below the target and only 15% of the products overall (n=44) exceeded the maximum levels specified.
Comment. This study showed that 85% of the products collected in the survey were already in line with the new legislated salt targets. However, it is unclear whether the foods collected for analysis from one large supermarket chain are representative of the entire food supply in Argentina. The use of a smartphone data collection application with established quality assurance procedures is a satisfactory method of collecting nutrient data. Likewise, the use of median values to compare the sodium content of the food groups with the targets is a suitable approach, as it is less sensitive to extreme values and therefore can better describe the sodium content per food group. The study was conducted independently to allow objective monitoring and provides a useful baseline assessment of compliance with the national salt standards as well as indicating that the salt standards may need to be set progressively lower to drive significant change in salt intake.
Assessment of Consumers' KAB Related to Salt
Awareness of Salt Restriction Is Not Reflected in the Actual Salt Intake in Japanese Hypertensive Patients
Takahashi N, Tanabe K, Adachi T, et al. Clin Exp Hypertens. 2015;37:388–392.
Summary. This study investigated the relationship between salt intake estimated from spot urine samples and awareness of recommended guidelines for reducing salt intake in Japanese hypertensive patients. A convenience sample of 236 hypertensive outpatients who visited the cardiovascular division of Shimane University Hospital was enrolled in the study. The patients were administered a questionnaire asking which level of salt restriction awareness they had: low, moderate, high, or very high. Daily salt intake was estimated by a morning spot urine sample to which Tanaka's equation was applied. The study found that salt intake was 9.72 g/d in hypertensive outpatients and concluded that patients' awareness of the guidelines did not correlate with estimated daily salt intake.
Comment. The study was undertaken in a convenience sample of patients from one hospital. Participants were asked to report their own awareness, and single spot urine samples were used to estimate individual salt intake, therefore the results are unlikely to be representative and subject to a high risk of bias. There is also no indication of adjustments for confounding. Despite these limitations, which are duly acknowledged by the authors, the results are in line with previous studies which found that knowledge is not associated with actual salt intake in Japan.29 This finding, in conjunction with the observation that salt intake in hypertensive patients is almost double the WHO‐recommended amount, is useful and highlights the need for greater efforts to effectively manage salt intake and hypertension.
Modeling Studies on the Effect of Salt Reduction Strategies
Nutritional Impact of Sodium Reduction Strategies on Sodium Intake from Processed Foods
Hendriksen MA, Verkaik‐Kloosterman J, Noort MW, van Raaij JM. Eur J Clin Nutr. 2015;69:805–810.
Summary. The modeling study simulates the effect of two salt reduction strategies on population salt intake in the Netherlands: (1) modifying the sodium content of processed foods to the lowest technologically feasible levels, and (2) changing consumers' behaviors to choose low‐salt alternatives within the same food group. Food intake data were obtained from the Dutch National Food Consumption Survey 2007–2010, and sodium content in foods were derived from the 2011 Dutch Food Composition Table. In the first scenario, where sodium content was changed to the lowest technologically feasible levels, reductions in sodium levels ranged from 26% in pastries to 70% in canned vegetables, leading to a 38% reduction in median population salt intake. In the second scenario, most food groups could be replaced with a low‐sodium alternative with >75% less sodium, resulting in a 47% median reduction in salt intake from processed foods.
Comment. This study demonstrates that substantial changes could be achieved by either reducing sodium content in a wide range of processed foods to their minimum technologically feasible level, or persuading consumers to intentionally choose low‐salt alternatives. The data sources, food composition database, and national food consumption survey used to estimate potential sodium reductions are appropriate and of satisfactory quality. The food consumption survey collected data from a nationally representative sample, using two non‐consecutive 24‐hour dietary recalls. However, no sensitivity analyses were undertaken to understand the effect of alternative assumptions or the uncertainties of these estimates on potential sodium reductions. Minimum technologically feasible levels of sodium were based on expert opinion and a number of criteria set by the authors. The potential difficulty in replicating these findings in a real‐world setting was highlighted by comparing the results with the actual outcomes of the voluntary reformulation intervention in the United Kingdom, where smaller sodium reductions were achieved in fewer food groups. The authors also noted that major efforts were needed from the food industry to achieve the reductions. The second scenario of consumers replacing foods with the low‐sodium alternatives within the same food group is acknowledged by the authors to be less feasible, in that it is unlikely that consumers would replace all foods within a subcategory with one, potentially extreme, alternative that has the lowest sodium content. The findings of this modeling study provide useful information about the extent to which a range of processed foods need to be reformulated or consumers' food choices need to be improved to achieve a reduction in population salt intake.
Discussion
This periodic review (from June to October 2015) identified 11 studies that can inform the future implementation of interventions to lower population salt intake. Four studies provided a detailed overview of national programs to reduce salt intake and one included a pilot study that demonstrated the feasibility of reducing salt intake and improving KAB in workplaces in Mongolia. None of the studies evaluated the impact of salt reduction strategies on population‐wide salt intake. The four review studies were authored by advocacy or government organizations involved in the respective strategies providing insight about what factors and information influenced the development of initiatives. Countries included in the reviews adopted different approaches to reducing salt intake; most Gulf Cooperation Council countries have focused their efforts on reducing the salt content in bread, Lebanon has implemented health education and advocacy initiatives, and Australia has undertaken a multifaceted approach. Key recommendations from the overviews highlight the importance of gaining government and industry commitment towards salt reduction.
Lessons learned from previous reviews of salt reduction initiatives suggest that success is likely dependent on a multifaceted approach, which includes both structural changes, such as reformulation in an extensive range of food categories, in conjunction with interventions that change consumer behavior.5 The importance of not relying on consumer behavior interventions alone is demonstrated in the study by Takahashi and colleagues,24 which found no significant correlation between knowledge of salt guidelines and measured daily salt intake in hypertensive patients in Japan. Furthermore, the Netherlands modeling study demonstrates the large reductions in salt content that manufacturers would need to achieve or the extreme dietary changes consumers would need to make in order to achieve the recommended salt intake if the interventions were implemented separately, further reinforcing the need for multifaceted approaches.25
Studies that monitored the current situation in terms of salt intake, salt content of foods, and consumer KAB related to salt consumption not only help to inform strategy development but also provide a basis against which changes can be monitored. Two studies in Italy and Germany found that current population salt consumption far exceeded the WHO‐recommended daily maximum of 5 g, demonstrating the need for greater efforts to reduce salt intake.19, 20 In addition, the study of salt intake in Italy showed that intake was significantly higher in less advantaged social groups, which further supports the importance of implementing structural interventions that are more likely to deliver changes equitably across all socioeconomic groups.30
In most Western countries, processed foods are the main contributors of salt in the diet and therefore reformulation efforts are a key initiative.31 Three studies measured salt content in packaged foods in Argentina, Australia, and New Zealand based on NIPs. The study on salt content in foods in Argentina not only provides an important baseline comparison prior to the enforcement of the mandatory salt targets but also identifies that most products surveyed already comply with the established maximum levels, suggesting that progressively lower targets will need to be set in the short term.23 The study in Australia found that the mean salt content of private‐label foods was overall 17% lower compared with branded foods, which highlights the feasibility of producing lower‐sodium products and the need for companies manufacturing branded products to make greater efforts to reduce salt.21 In New Zealand, there has been NGO‐led action to encourage reformulation toward voluntary salt targets but no detectable impact, raising significant concerns about the non‐mandated approach employed.22 These analyses also highlight the importance of employing rigorous monitoring mechanisms to determine whether reformulation activities are having an impact. Argentina, Australia, and New Zealand are all part of Food Monitoring Group initiative to monitor the nutritional content of processed foods worldwide, which has standardized methodologies for robust surveillance that can be replicated in other countries.32
Conclusions
The 11 implementation studies are varied in nature and study design but provide important recommendations for the implementation of salt reduction strategies. These include achieving government commitment, implementing multi‐component interventions rather than just targeting consumer behavior, and using standardized methodologies to rigorously monitor the salt content of processed foods. All except one study are from high‐income countries, emphasizing the need for greater research and support for the implementation of programs to reduce salt in low‐ and middle‐income countries, where four of every five salt‐related deaths from cardiovascular causes are estimated to occur.33
Supporting information
Appendix S1. Risk of bias and quality appraisal tables for included studies.
Acknowledgments
The process to provide regular updates on the science of sodium is supported by the World Hypertension League, WHO Collaborating Centre on Population Salt Reduction (The George Institute for Global Health), Pan American Health Organization/World Health Organization (PAHO/WHO) Technical Advisory Group on Cardiovascular Disease Prevention through Dietary Sodium, and World Action on Salt & Health.
Disclosures
RM, CJ, JAS, BA, JA, TSR, and AAL have no conflicts of interest to declare. KT, JW, and BN are authors on some of the studies included in the review. NC is a member of World Action on Salt & Health a dietary salt reduction organization but has no financial interests to declare. MMYW is a research consultant with Renal Research Institute and Arbor Research Collaborative for Health. BN is chair of the Australian Division of World Action on Salt and Health. BN and JW have funding from the World Health Organization, VicHealth, and Australian National Health and Medical Research Council of Australia for research on salt reduction. JW is director of the World Health Organization Collaborating Centre on Population Salt Reduction and is supported by a National Health and Medical Research Council/National Heart Foundation Career Development Fellowship on international strategies to reduce salt.
J Clin Hypertens (Greenwich). 2016;18 487–494. DOI: 10.1111/jch.12806. © 2016. Wiley Periodicals, Inc.
References
- 1. He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta‐analysis of randomised trials. BMJ. 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 2. Aburto NJ, Ziolkovska A, Hooper L, et al. Effect of lower sodium intake on health: systematic review and meta‐analyses. BMJ. 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Powles J, Fahimi S, Micha R, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . NCD Global Monitoring Framework. Noncommunicable diseases and mental health 2013; http://www.who.int/nmh/global_monitoring_framework/en/. Accessed November 16, 2015.
- 5. Trieu K, Neal B, Hawkes C, et al. Salt reduction initiatives around the world—a systematic review of progress towards the global target. PLoS One. 2015;10:e0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Arcand J, Webster J, Johnson C, et al. Announcing “up to date in the science of sodium.” J Clin Hypertens (Greenwich). 2016;18:85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arcand J, Wong MM, Trieu K, et al. The science of salt: a regularly updated systematic review of salt and health outcome (June and July 2015). J Clin Hypertens (Greenwich). 2015. Dec 29 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization . Guideline: Sodium intake for adults and children. 2012; http://www.who.int/nutrition/publications/guidelines/sodium_intake_printversion.pdf. Accessed November 16, 2015. [PubMed]
- 9. The Cochrane Collaboration . Cochrane Handbook for Systematic Reviews of Interventions Chapter 8: Assessing risk of bias in included studies. Version 5.1.0 ed2011: http://bmg.cochrane.org/assessing-risk-bias-included-studies. Accessed November 16, 2015.
- 10. McLaren L, Sumar N, Lorenzetti DL, et al. Population‐level interventions in government jurisdictions for dietary sodium reduction (protocol). Cochrane Database Syst Rev. 2012;(10):Art. No.: CD010166. DOI: 10.1002/14651858.CD010166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Organization WH . Strategies to monitor and evaluate population sodium consumption and sources of sodium in the diet. Report of a joint technical meeting convened by WHO and the Government of Canada. 2011; http://apps.who.int/iris/bitstream/10665/44614/1/9789241501699_eng.pdf. Accessed November 16, 2015.
- 12. WHO/PAHO Regional Expert Group for Cardiovascular Disease Prevention through Population‐wide Dietary Salt Reduction . Protocol for Population Level Sodium Determination in 24‐hour Urine Samples. 2010; http://www.paho.org/hq/index.php?option=com_docman&task=doc_view&gid=21488&Itemid. Accessed November 16, 2015.
- 13. National Heart Lung and Blood Institute of the U.S . Quality Assessment Tool for Observational Cohort and Cross‐Sectional Studies 2014; https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort. Accessed November 27, 2015.
- 14. Philips Z, Bojke L, Sculpher M, et al. Good practice guidelines for decision‐analytic modelling in health technology assessment: a review and consolidation of quality assessment. Pharmacoeconomics. 2006;24:355–371. [DOI] [PubMed] [Google Scholar]
- 15. Almedawar MM, Nasreddine L, Olabi A, et al. Sodium intake reduction efforts in Lebanon. Cardiovasc Diagn Ther. 2015;5:178–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alhamad N, Almalt E, Alamir N, Subhakaran M. An overview of salt intake reduction efforts in the Gulf Cooperation Council countries. Cardiovasc Diagn Ther. 2015;5:172–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Webster J, Trieu K, Dunford E, et al. Salt reduction in Australia: from advocacy to action. Cardiovasc Diagn Ther. 2015;5:207–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Enkhtungalag B, Batjargal J, Chimedsuren O, et al. Developing a national salt reduction strategy for Mongolia. Cardiovasc Diagn Ther. 2015;5:229–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cappuccio FP, Ji C, Donfrancesco C, et al. Geographic and socioeconomic variation of sodium and potassium intake in Italy: results from the MINISAL‐GIRCSI programme. BMJ Open. 2015;5:e007467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Johner SA, Thamm M, Schmitz R, Remer T. Current daily salt intake in Germany: biomarker‐based analysis of the representative DEGS study. Eur J Nutr. 2015;54:1109–1115. [DOI] [PubMed] [Google Scholar]
- 21. Trevena H, Neal B, Dunford E, et al. A comparison of the sodium content of supermarket private‐label and branded foods in Australia. Nutrients. 2015;7:7027–7041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Monro D, Mhurchu CN, Jiang Y, et al. Changes in the sodium content of New Zealand processed foods: 2003–2013. Nutrients. 2015;7:4054–4067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Allemandi L, Tiscornia MV, Ponce M, et al. Sodium content in processed foods in Argentina: compliance with the national law. Cardiovasc Diagn Ther. 2015;5:197–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Takahashi N, Tanabe K, Adachi T, et al. Awareness of salt restriction is not reflected in the actual salt intake in Japanese hypertensive patients. Clin Exp Hypertens. 2015;37:388–392. [DOI] [PubMed] [Google Scholar]
- 25. Hendriksen MA, Verkaik‐Kloosterman J, Noort MW, van Raaij JM. Nutritional impact of sodium reduction strategies on sodium intake from processed foods. Eur J Clin Nutr. 2015;69:805–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nasreddine L, Akl C, Al‐Shaar L, et al. Consumer knowledge, attitudes and salt‐related behavior in the Middle‐East: the case of Lebanon. Nutrients 2014;6:5079–5102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ji C, Kandala NB, Cappuccio FP. Spatial variation of salt intake in Britain and association with socioeconomic status. BMJ Open. 2013;3:e002246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Grimes CA, Campbell KJ, Riddell LJ, CA N. Is socioeconomic status associated with dietary sodium intake in Australian children? A cross‐sectional study BMJ Open 2013;3:e002106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ohta Y, Tsuchihashi T, Ueno M, et al. Relationship between the awareness of salt restriction and the actual salt intake in hypertensive patients. Hypertens Res. 2004;27:243–246. [DOI] [PubMed] [Google Scholar]
- 30. Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities? PLoS Med. 2010;7:e1000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Webster J, Trieu K, Dunford E, Hawkes C. Target salt 2025: a global overview of national programs to encourage the food industry to reduce salt in foods. Nutrients. 2014;6:3274–3287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dunford E, Webster J, Metzler AB, et al. International collaborative project to compare and monitor the nutritional composition of processed foods. Eur J Prev Cardiol. 2012;19:1326–1332. [DOI] [PubMed] [Google Scholar]
- 33. Mozaffarian D, Fahimi S, Singh G, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–634. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Risk of bias and quality appraisal tables for included studies.


