Abstract
Hypertension is the most common primary diagnosis in the United States. Risks for long‐term consequences such as myocardial infarction, heart failure, stroke, and kidney disease continue to significantly increase as long as hypertension remains uncontrolled. This retrospective cohort study of 661,075 patients identified with uncontrolled hypertension, defined as systolic blood pressure (SBP) ≥140 mm Hg and/or diastolic blood pressure (DBP) ≥90 mm Hg, from a large integrated healthcare organization was conducted to examine multiple patient characteristics to determine their association with uncontrolled hypertension. Multivariate analysis revealed that compared with Caucasians, African Americans (odds ratio [OR], 1.18; 95% confidence interval [CI], 1.16–1.20) were significantly associated with uncontrolled hypertension, as were unpartnered populations (OR, 1.15; 95% CI, 1.14–1.17), number of antihypertensive medications prescribed (OR, 1.37; 95% CI, 1.33–1.41), and adherence to most antihypertensive medications. A secondary analysis found an association between uncontrolled blood pressure and Patient Health Questionnaire‐9 (PHQ‐9) score (OR, 1.21; 95% CI, 1.16–1.26). Our findings suggest that the presence of these identified risk factors recommends a commitment to a more aggressive hypertension management program to prevent cardiovascular disease caused by uncontrolled hypertension.
Hypertension is the most common primary diagnosis in the United States, representing 38.9 million office visits annually1 and affecting 78 million adults in the United States and nearly 1 billion worldwide.2 Every additional 20 mm Hg in systolic blood pressure (SBP) or 10 mm Hg in diastolic blood pressure (DBP) down to a threshold of at least 115/75 mm Hg has been shown to double the risk of cardiovascular disease (CVD) for individuals aged 40 to 70 years.3 When hypertension remains uncontrolled, risks for long‐term sequelae such as myocardial infarction, heart failure, stroke, and kidney disease significantly increase. As the US population continues to age, the negative impact of uncontrolled hypertension will increase unless risk factors associated with uncontrolled hypertension are identified and addressed.
Southern California Kaiser Permanente, a staff model–integrated healthcare organization, currently has a hypertension control rate of 84%, which is one of the highest control rates in the nation. However, despite intensive efforts over many years to control blood pressure (BP), the organization has encountered barriers to achieving higher hypertension control rates.4 The aim of this study was to examine a range of clinical variables to determine the association with failure to achieve BP control in a large cohort of patients with uncontrolled hypertension. Identification of key variables may allow for a more focused effort to address the needs of this population as well as to plan for appropriate resource allocation. Moreover, significant findings identifying potential risk factors could inform providers of the need for more aggressive hypertension management, potentially reducing patient risk for cardiovascular events.
Large clinical trials such as the Antihypertensive and Lipid‐Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) suggest that in order to effectively control BP, the majority of patients will require ≥2 antihypertensive agents.5, 6 The presence of comorbid conditions, such as dyslipidemia, type 2 diabetes mellitus, and chronic kidney disease is not uncommon with hypertension, and may frequently result in significant polypharmacy, which may raise the challenge of medication adherence, despite the availability of combination products, such as lisinopril‐hydrochlorothiazide.
Many studies have examined risk factors for hypertension and many comprehensive management guidelines have been published. However, the risk factors for uncontrolled hypertension are less well established. A study by Egan and colleagues7 examined uncontrolled and treatment‐resistant hypertension in the United States. The authors found that individuals diagnosed with hypertension, whether they have untreated, undertreated, or treatment‐resistant hypertension, have consistent characteristics that could provide insight to improve BP control. This key study examined race/ethnicity, diabetes mellitus, Framingham coronary heart disease risk, insurance status, and antihypertensive medications, but there are additional factors that need to be investigated. The objective of this study is to identify the risk factors associated with uncontrolled hypertension within a large, diverse population in a high performing healthcare system.
Methods
This retrospective cohort study sought to identify patient risk factors for uncontrolled BP among Southern California Kaiser Permanente patients with hypertension. This study evaluated patients with a diagnosis of hypertension over a 3‐year period between January 1, 2010 and December 31, 2012. Hypertension was defined as SBP ≥140mm Hg and/or DBP ≥90 mm Hg.
Study Cohort
The study cohorts were identified from an electronic medical record database containing demographic data, diagnoses, vital signs, pharmacy utilization, and personal information. Subjects included in the study were those at least 18 years old with an International Classification of Diseases‐Ninth Revision (ICD‐9) code diagnosis for hypertension and at least 1 elevated BP reading. Additionally, each subjects had at least 3 ICD‐9 hypertension diagnostic coding events and at least 3 recorded BP readings. The minimum 3 BP readings occurred within the 3‐year study period and were obtained at separate office visits. A subject's BP was measured once, however, if elevated, a repeat BP was taken 5 minutes later. The lowest BP reading was recorded. Home BP readings or readings obtained outside of Kaiser Permanente were not recorded in the electronic medical record system. Subjects who had a hypertension diagnosis for <6 months, patients with no medical record, and patients who were pregnant were excluded from the study.
Clinical Outcomes
“Uncontrolled hypertension” was defined as the last BP measurement in the study period that was elevated. This “last BP uncontrolled” has been shown to be highly correlated with overall hypertension control, and reflects Healthcare Effectiveness Data and Information Set (HEDIS)8 and Centers for Medicare & Medicaid Services (CMS) definitions of uncontrolled BP.9
Covariates
Covariates included in the analysis were age, gender, race/ethnicity, body mass index (BMI), non‐English speaking, partner status (partnered defined as any one of the following: married, common law marriage, co‐habitation, or domestic partnership; unpartnered defined as single, divorced, separated, unmarried, or widowed), family history of hypertension, thiazide‐naive (defined as those who have not been prescribed a thiazide medication dating as far back as 1996), total number of medications taken, the number of chronic medications (defined as at least 200 consecutive days' supply within the last 6 months of the last uncontrolled BP reading), hours of exercise per week (patient self‐reported; assumed to be zero if not reported), diagnosis of major depression, 9‐Item Patient Health Questionnaire (PHQ‐9) score, average number of primary care provider (PCP) visits per year, average number of canceled PCP visits per year, average number of emergency department visits per year, and average walk‐in BP measurements per year. Education level and median household income were imputed from the census block group for 2010 (interpolated to 2012). The 12 classes of antihypertensive medications identified in the National Health and Nutrition Examination Survey (NHANES)7 were examined. Angiotensin‐converting enzyme (ACE) inhibitor and angiotensin II receptor blocker (ARB) were grouped together as renin‐angiotensin system antagonists (Table 1). Combinations of antihypertensive medications were not evaluated. Assessment of antihypertensive treatment occurred in the 6‐month period prior to the last uncontrolled BP reading.
Table 1.
Antihypertensive Medication Classes
| 1. Angiotensin‐converting enzyme inhibitor/angiotensin II receptor blocker |
| 2. α‐Blocker |
| 3. α, β‐Blocker |
| 4. β‐Blocker |
| 5. Dihydropyridine calcium channel blocker |
| 6. Nondihydropyridine calcium channel blocker |
| 7. Aldosterone antagonist |
| 8. Potassium‐sparing diuretic |
| 9. Loop diuretic |
| 10. Thiazide |
| 11. Sympatholytic |
| 12. Vasodilator |
To assess impact of mental health in BP control, symptoms of depression were assessed by scores on the PHQ‐9, a brief psychological screening instrument designed to detect depression. The PHQ‐9 consists of 9 questions that have been validated to identify patients with clinically meaningful symptoms of depression during the previous 2‐week period. The PHQ‐9 questionnaire is scored between a range of 0 to 27 (Table 2).10 PHQ‐9 scores ≥10 have a sensitivity of 88% and a specificity of 88% for major depression. Kaiser Permanente randomly administers the PHQ‐9 as a screening tool for depression.
Table 2.
Interpretation of 9‐Item Patient Health Questionnaire Score
| Total Score | Depression Severity |
|---|---|
| 1–4 | Minimal depression |
| 5–9 | Mild depression |
| 10–14 | Moderate depression |
| 15–19 | Moderately severe depression |
| 20–27 | Severe depression |
A key variable considered for our study was adherence to medications, which we defined as proportion of days covered (PDC) by the prescriptions dispensed. PDC was calculated by dividing the number of days' supply dispensed to the patient by the total number of days in that period; in other words, PDC was the number of days with the medication on hand in a period of time.11 We defined adherence to medication as a PDC ≥80% based on HEDIS and CMS definitions.8
Statistical Analysis
Descriptive data for patient characteristics were tabulated. Crude odds ratios (ORs) of outcomes on single covariates were computed as well as adjusted ORs of outcomes corrected for the presence of the covariates. The Wilcoxon rank‐sum test was used for comparisons of demographic patient data. Analysis was performed using univariate and multivariate logistic regression of the last BP uncontrolled or controlled on all the derived demographic, administrative, and pharmacy records in order to determine ORs with 95% confidence intervals (CIs). The model was developed using a stepwise selection procedure requiring that any variable that was included in the model had to be significant at the .05 level and had to remain significant at the .05 level to be retained in the model. A similar secondary analysis was also performed that examined PHQ‐9 scores utilizing logistic regression analysis.
Results
Study Cohort
A total of 835,465 patients with a diagnosis of hypertension were identified in the medical record database. Of these, 174,390 cases were excluded because of incomplete data; hence, the study cohort was 661,075, with 107,016 cases of uncontrolled hypertension and 554,059 with controlled hypertension (Figure 1). A comparison of patient baseline characteristics for controlled and uncontrolled hypertension is presented in Table 3.
Figure 1.
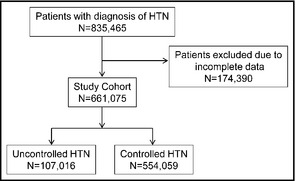
Flow diagram of study cohort population. HTN indicates hypertension.
Table 3.
Demographic Data
| Uncontrolled Hypertension (N=107,016) | Controlled Hypertension (N=554,059) | |
|---|---|---|
| Age, y | 67 | 64 |
| Male gender (%) | 47,531 (44.4) | 255,738 (46.2) |
| Race (%) | ||
| Caucasian | 46,315 (43.3) | 258,113 (46.6) |
| African American | 19,344 (18.1) | 77,464 (14.0) |
| Hispanic | 31,019 (29.0) | 156,342 (28.2) |
| Asian/Pacific Islander | 9,933 (9.3) | 60,133 (10.9) |
| Native American | 205 (0.2) | 1,040 (0.2) |
| Multiple races | 200 (0.2) | 967 (0.2) |
| Partner status (%) | 62,951 (58.8) | 351,011 (63.3) |
| Family history of hypertension (%) | 31,486 (29.4) | 159,710 (28.8) |
| Thiazide‐naive (%) | 30,047 (28.1) | 191,174 (34.5) |
| Non–English‐speaking (%) | 13,856 (12.9) | 75,325 (13.6) |
Adjusted Clinical Outcomes
In order to adjust for important sources of confounding variables, multivariable logistic regression models were created for the primary effectiveness outcome and ORs were calculated. ORs >1 were associated with uncontrolled hypertension and ORs <1 were associated with controlled hypertension. Following analysis of risk factors, clinically relevant covariates were identified for display in a forest plot (Figure 2). Covariates that were analyzed but found to have clinically insignificant differences between groups, and thus not reported in the forest plot, were BMI, hours of exercise per week, average number of PCP visits per year, average number of canceled PCP visits per year, average number of emergency department visits per year, average walk‐in BP measurements per year, and educational levels achieved.
Figure 2.
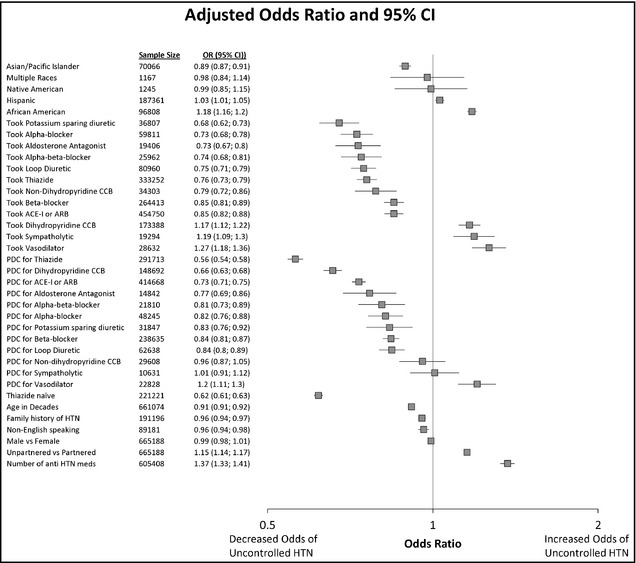
Forest plot showing the risk factors associated with uncontrolled vs controlled hypertension. Odds ratios >1 are associated with uncontrolled hypertension and odds ratios <1 are associated with controlled hypertension. CI indicates confidence interval; CCB, calcium channel blocker; ACE‐I angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; PDC, proportion of days covered; HTN, hypertension; meds, medications.
A significant association was found between race and BP control: compared with Caucasians, African Americans (OR, 1.18; 95% CI, 1.16–1.20) were significantly associated with uncontrolled hypertension. Conversely, Asian and Pacific Islander race was associated with BP control (OR, 0.89; 95% CI, 0.87–0.91).
Gender was not associated with BP control (OR, 0.99; 95% CI, 0.98‐1.01). However, partner status was a risk factor associated with uncontrolled BP. Patients who identified themselves as unpartnered were found to be associated with uncontrolled hypertension (OR, 1.15; 95% CI, 1.14–1.17).
The class of antihypertensive medications prescribed had a strong association with BP control. Treatment with ACE inhibitors/ARBs, α‐blockers, α, β‐blockers, aldosterone antagonists, β‐blockers, potassium‐sparing diuretics, loop diuretics, nondihydropyridine calcium channel blockers (CCBs), and thiazides were found to be associated with BP control. However, patients prescribed dihydropyridine CCBs, sympatholytics, and vasodilators were found to have an association with uncontrolled hypertension. Patients who were naive to thiazide therapy were found to be associated with controlled BP (OR, 0.62; 95% CI, 0.61–0.63).
As would be anticipated, an association was found between adherence to most antihypertensive medications and BP control. Adherence to thiazides, dihyrdopyridine CCBs, ACE inhibitors/ARBs, aldosterone antagonists, α, β‐blockers, α‐blockers, potassium‐sparing diuretics, β‐blockers, and loop diuretics were found to be associated with controlled hypertension. Lastly, the more antihypertensive medications a patient was provided, the more likely he/she would have uncontrolled hypertension (OR 1.37; 95% CI 1.33–1.41).
A secondary analysis was performed investigating PHQ‐9 scores, in which an association with uncontrolled hypertension was found (Table 2). The scores were dichotomized into two groups: patients with a score of ≥10 and <10.10 This cut‐off represents those who are considered moderately depressed compared with mildly depressed. This PHQ‐9 analysis found the OR for a patient having uncontrolled BP and scoring ≥10 was 1.21 (95% CI, 1.16–1.26) (Figure 3).
Figure 3.
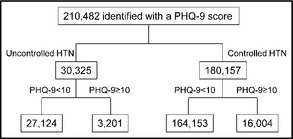
Flow diagram of 9‐Item Patient Health Questionnaire Score (PHQ‐9) secondary analysis.
Discussion
This retrospective cohort study identified significant patient characteristics associated with uncontrolled hypertension that includes African American race, partner status, medication adherence, and PHQ‐9 depression score. The association of last BP uncontrolled with antihypertensive treatment in the 6‐month period prior to the uncontrolled BP reading as opposed to the entire 3‐year study period was evaluated in order to eliminate periods of medication titration and perhaps switching of antihypertensive medications as a result of allergies, intolerances, or adverse reactions. African Americans, compared with Caucasians, were found to be at significantly higher risk for uncontrolled hypertension. Similarly, Egan and colleagues7 identified this racial disparity and found that patients with resistant hypertension were more likely to be African American. Hence, prudent vigilance when treating African American patients is warranted as they may benefit from more aggressive antihypertensive medication management.
Partner status also demonstrated an important association with hypertension control: unpartnered status—divorced, separated, and single—was associated with higher risk of uncontrolled hypertension. Studies conducted in Europe also evaluated partner status and its association with hypertension. In a Dutch population, patients without a partner were found to have had a higher risk of being unaware of or of not being treated for existing hypertension.12 Gaudemaris and colleagues13 studied a French population and observed that single men may have had an association with the prevalence of hypertension; however, this finding was not statistically significant.
Treatment with ACE inhibitors/ARBs was found to be strongly associated with a decreased risk of uncontrolled hypertension. Conversely, sympatholytics such as clonidine and vasodilators such as hydralazine were associated with uncontrolled hypertension. We postulate this is because these alternative antihypertensive medications are most commonly utilized in highly refractory patients.
Being thiazide‐naive was found to be associated with BP control. There could be various explanations for this counterintuitive observation. For example, this finding could be the result of a cohort of patients in our population with mild hypertension controlled on a single (nonthiazide) agent, such as an ACE inhibitor or ARB. These may represent cases where initiation of a thiazide antihypertensive agent would be undesirable or contraindicated, for example, in the presence of hypokalemia or hyponatremia.14 An additional explanation, perhaps more likely, is that thiazides are an index of hypertension severity. In other words, the thiazide‐naive and currently taking thiazide groups are fundamentally different—the latter group likely being more difficult to control. It could be postulated that the thiazide group is indeed more difficult to control, and thus, these patients should be taking more antihypertensive medication at the time of control, for example. Our findings also show that as the number of antihypertensive agents prescribed per patient increased, there was an increased likelihood that the patient had uncontrolled hypertension.
Results from the PHQ‐9 analysis suggest that uncontrolled BP may be associated with depression. Our study indicates that patients who are considered to have moderate depression based on a PHQ‐9 score ≥10 have increased odds of uncontrolled BP. A similar association has been reported in the literature with depression and asthma. Bender15 found that depression is associated with nonadherence to medications, poor treatment outcomes, and death from asthma.
A similar association with depression has also been shown with diabetes and HIV. Patients who are depressed were found to be less likely to take their medications and, thus, more at risk for medication nonadherence. A meta‐analysis found a relationship between depression and HIV medication nonadherence.16 These results suggest that depression is consistently associated with nonadherence to HIV treatment, which has important implications for treatment outcomes at the population level. Furthermore, another meta‐analysis of the literature on depression and diabetes treatment was performed in order to examine the strength of the relationship between depression and type 1 or type 2 diabetes.17 The authors found that there was a significant association of diabetes complications with depressive symptoms.
In integrated healthcare organizations where hypertension control rates may be high, the risk factors identified in the remaining uncontrolled cohort may be different than that of other health systems with lower control rates. According to NHANES data, the hypertension control rate improved nationwide from 27.3% in 1988–1994 to 50.1% in 2007–2008.2 Thus, factors associated with treatment resistance in the present study population may be different than factors associated with a population that has a control rate of 50%. Internal data demonstrate that the Kaiser Permanente membership population reflects the general demographics of the communities it serves. As a result, identifying risk factors associated with a difficult to control hypertension population may aid in the improvement of hypertension control rates in cohorts outside the Kaiser Permanente system.
Study Strengths and Limitations
This study had a number of strengths, including a large patient population reflecting the communities from which it was drawn. Additionally, a large number of variables were investigated to explore multiple associations with uncontrolled BP. The model utilized was robust as it required that each patient have at least 3 coded diagnoses for hypertension and at least 3 recorded BP readings. Furthermore, excluding patients with a hypertension diagnosis of <6 months allows for selection of a cohort with consistent follow‐up in the system.
However, several limitations exist in our investigation. First, there are inherent limitations associated with the retrospective cohort study design. Second, the reliance on ICD‐9 codes for diagnoses is a limitation. This study was designed to minimize the risk of incorrect hypertension diagnoses by requiring each patient have 3 or more ICD‐9 coding events for hypertension. Defining uncontrolled hypertension based on last BP reading creates variability in control status. However, HEDIS and CMS define uncontrolled hypertension in this manner. Moreover, alternative ways to define uncontrolled hypertension can be considered. For example, alternative definitions may define a resistant hypertension cohort as patients whose BP readings were never in control or identifying the uncontrolled population by isolating the last several uncontrolled BP measurements.
Future research should evaluate alternative definitions for uncontrolled hypertension including patients who never had controlled BP. As BP control status will fluctuate across visits within an individual over time, using all of the available BP readings to quantify control would be a unique analysis to perform. In addition, other studies should seek to develop a predictive and multivariate model to identify subgroups of patients with BP that is likely difficult to control. Lastly, determining associations between patients found to be moderately depressed and medication nonadherence would be worthy of future investigation.
Conclusions
In this retrospective cohort analysis, we identified sociodemographic factors and clinical factors associated with uncontrolled hypertension. Assessment of the presence of these risk factors is warranted to recommend aggressive hypertension management with the goal of reducing excessive risk of cardiovascular events caused by uncontrolled hypertension. Hypertension, compared with any other cardiovascular risk factor, has the most medications approved for treatment and has more clinical practice guidelines written, yet hypertension still remains underrecognized and undertreated.7 The findings of our study suggest careful consideration should be ascribed to patients who are African American, unpartnered, have poor medication adherence, and have a PHQ‐9 score ≥10 as they are more likely to have difficulty in controlling their hypertension.
Statement of Financial Disclosure
The authors report no specific funding in relation to this research and no conflicts of interest to disclose.
Acknowledgments
We would like to thank Tony Yiu, SAS programmer, from Kaiser Permanente Southern California Research and Evaluation for conducting the statistical analysis for this paper.
J Clin Hypertens (Greenwich). 2014;16:149–154. DOI: 10.1111/jch.12259. ©2014 Wiley Periodicals, Inc.
References
- 1. Centers for Disease Control and Prevention (CDC) . National Ambulatory Medical Care Survey: 2010 Summary Tables, table 13. http://www.cdc.gov/nchs/fastats/hyprtens.htm. Accessed September 4, 2013.
- 2. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 4. Jaffe MG, Lee GA, Young JD, et al. Improved blood pressure control associated with a large‐scale hypertension program. JAMA. 2013;310:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Black HR, Elliott WJ, Neaton JD, et al. Baseline characteristics and elderly blood pressure control in the CONVINCE trial. Hypertension. 2001;37:12–18. [DOI] [PubMed] [Google Scholar]
- 6. Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid‐lowering treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4:393–404. [DOI] [PubMed] [Google Scholar]
- 7. Egan BM, Zhao Y, Axon RN, et al. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124:1046–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. HEDIS & Performance Measurement . National Committee for Quality Assurance website. http://www.ncqa.org/tabid/59/Default.aspx. Accessed May 10, 2013.
- 9. Alexander M, Tekawa I, Hunkeler E, et al. Evaluating hypertension control in a managed care setting. Arch Intern Med. 1999;159:2673–2677. [DOI] [PubMed] [Google Scholar]
- 10. Kroenke K, Spitzer R, Williams JBW. The PHQ‐9 validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Benner JS, Glynn RJ, Mogun H, et al. Long‐term persistence in use of statin therapy in elderly patients. JAMA. 2002;288:455–461. [DOI] [PubMed] [Google Scholar]
- 12. Van Rossum CTM, van de Mheen H, Witteman JCM, et al. Prevalence, treatment, and control of hypertension by sociodemographic factors among the Dutch elderly. Hypertension. 2000;35:814–821. [DOI] [PubMed] [Google Scholar]
- 13. Gaudemaris RD, Lang T, Chatellier G, et al. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF Study. Hypertension. 2002;39:1119–1125. [DOI] [PubMed] [Google Scholar]
- 14. Rastogi D, Pelter MA, Deamer RL. Evaluations of hospitalizations associated with thiazide‐associated hyponatremia. J Clin Hypertens (Greenwich). 2012;14:158–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bender BG. Risk taking, depression, adherence, and symptom control in adolescents and young adults with asthma. Am J Respir Crit Care Med. 2006;173:953–957. [DOI] [PubMed] [Google Scholar]
- 16. Gonzales JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta‐analysis. J Acquir Immune Defic Syndr. 2011;58:181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. de Groot M, Anderson R, Freedland KE, et al. Association of depression and diabetes complications: a meta‐analysis. Psychosom Med. 2001;4:619–630. [DOI] [PubMed] [Google Scholar]


