Abstract
A growing body of evidence links obstructive sleep apnea (OSA) with hypertension. The authors performed a retrospective cohort study using the University Hospital of Larissa Sleep Apnea Database (1501 patients) to determine predictors of in‐laboratory diagnosed OSA for development of hypertension. Differences in continuous variables were assessed via independent samples t test, whereas discrete variables were compared by Pearson's chi‐square test. Multivariate analysis was performed via discriminant function analysis. There were several significant differences between hypertensive and normotensive patients. Age, body mass index, comorbidity, daytime oxygen saturation, and indices of hypoxia during sleep were deemed the most accurate predictors of hypertension, whereas apnea‐hypopnea index and desaturation index were not. The single derived discriminant function was statistically significant (Wilk's lambda=0.771, χ2=289.070, P<.0001). Daytime and nocturnal hypoxia as consequences of chronic intermittent hypoxia play a central role in OSA‐related hypertension and should be further evaluated as possible severity markers in OSA.
Obstructive sleep apnea (OSA) is characterized by repetitive interruption of ventilation during sleep caused by collapse of the pharyngeal airway. The apnea‐hypopnea index (AHI) is the number of apneas and hypopneas per hour of sleep and has been used to characterize the severity of the OSA syndrome (OSAS). A diagnosis of OSAS is accepted when a patient has an AHI >5 and associated symptoms (eg, excessive daytime sleepiness, fatigue, or impaired cognition) or an AHI ≥15 regardless of associated symptoms.1, 2
OSA is a common condition of sleep‐disordered breathing and occurs in approximately 5% to 10% of the general population, regardless of race and ethnicity.3 It is estimated that 30% to 40% of hypertensive patients have OSA and 50% to 56% of OSA patients have hypertension.4 An association between OSA and hypertension has been observed since the early description of OSA in the 1970s.5, 6, 7 However, it had been difficult to clarify the cause‐effect relationship between the two disorders. This is because patients with hypertension and patients with OSA have common risk factors such as age, sex, obesity, smoking, and alcohol abuse.8, 9, 10 In recent years, there has been a large body of evidence estimating the role of OSA as an independent risk factor for hypertension. However, the results of these studies were controversial. Data from some studies support a dose‐response relationship of OSA at baseline and the cumulative incidence of hypertension.11, 12 In contrast, other studies have reported that the unadjusted risk of hypertension increases in concert with AHI, but this association was not significant after adjustment for potential confounding variables.13, 14 Furthermore, the mechanisms underlying hypertension in patients with OSAS are still poorly understood. Intermittent hypoxia (defined as repetitive short cycles of desaturation followed by rapid re‐oxygenation) is supposed to play a pivotal role in the cardiovascular disease process.15, 16, 17
Thus, we performed a retrospective cohort study to investigate the relationship between OSA and hypertension and find predictive factors of in‐laboratory diagnosed OSA patients for development of hypertension.
Methods
Study Population
We studied 1501 patients (50±15.2 years, 246 women) who complained of snoring or/and sleep interruption and excessive daytime sleepiness and had been consecutively referred to University Hospital of Larissa for investigations of possible OSA between January 2000 and December 2010. They underwent full standard in‐laboratory polysomnography (PSG). We designed a database including patient demographics, clinical history, respiratory function data (spirometry), and finally all parameters included in their in‐laboratory PSG. Patients (n=1227) with an AHI >5 and associated symptoms (eg, excessive daytime sleepiness, fatigue, or impaired cognition) were included in the final statistical analyses (Figure). Individuals with previously diagnosed respiratory failure of any etiology were excluded.
Figure 1.
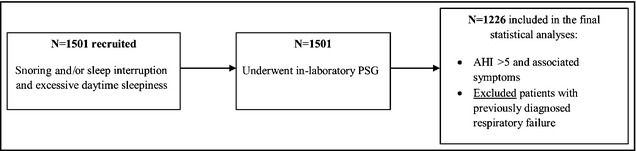
Flow diagram. PSG indicates polysomnography; AHI, apnea‐hypopnea index.
Hypertensive patients were defined as individuals who were previously diagnosed as hypertensive and were also taking antihypertensive medication. The age‐adjusted Charlson Comorbidity Index (CCI) score for each patient was calculated based on the algorithm formatted as Microsoft Excel Macro, developed by Hall and colleagues.18 Comorbidity was determined as the concurrence of a disease included in and scored by the CCI criteria. Daytime mean oxygen saturation (SaO2) was estimated as the average measurement of the pulse oximetry over an hour as the patient was awake, at rest, and in a sitting position. The study protocol and related procedures were approved by the institutional review board of the University Hospital of Larissa and the University of Thessaly Medical School.
Polysomnography
PSG included electroencephalography, electrooculography, submental electromyography, anterior tibialis electromyography, nasal cannula airflow signal using a nasal cannula/pressure transducer system, oral thermistor, electrocardiography, and body position. Sleep was scored manually according to the criteria of Rechtschaffen and Kales. Respiratory efforts were monitored with abdominal and thoracic bands. Arterial SaO2 was measured using pulse oximetry. Arousals were scored according to standard criteria. Apnea was defined as complete cessation of airflow for at least 10 seconds in duration. Hypopnea was defined as one of the following three: (1) >50% reduction in airflow, (2) <50% reduction in airflow associated with a desaturation of >3%, or (3) a moderate reduction in airflow with associated arousal by electroencephalography. Apneas were classified as obstructive, central, or mixed according to the presence or absence of respiratory efforts.1, 2
Statistical Analysis
Univariate Analyses
Demographic, clinical history, respiratory function data, and all parameters included in patients’ in‐laboratory PSG were expressed as mean±standard deviation for continuous variables and percentages for discrete variables. Univariate analysis was performed by independent samples t test and Pearson's chi‐square for continuous and discrete variables, respectively. Data normality was assessed by the Kolmogorov‐Smirnov test.
Multivariate Analyses
Multivariate analysis was performed via discriminant function analysis (DFA). Our study applied a linear discriminant model, a linear function of continuous predictor variables that best allocate subjects between c groups, where c ≥2. Furthermore, the resulting function may be subsequently used to classify new cases. The discriminant formula for a population of [1, 2…, n] subjects, with [1, 2…, i] coefficients is described below,
where:
“j” is the number of discriminant functions extracted, with j∈[1, c‐1].
“D j” is the discriminant function score for the jth discriminant function,
“A” is the constant,
“k i” is the discriminant function coefficient,
“m ni” is the predictor variable value for the ith subject and the nth discriminant function coefficient.
The Wilk's lambda test is used to determine the derived discriminant function's statistical significance. A confusion matrix is further used to determine the function's predictive accuracy, whereas the cross‐validated predictive accuracy is estimated via the “leave‐one‐out” classification process.19
Linear DFA with a binary (categorical) dependent variable represents the simplest form of DFA in which a single discriminant function is derived. In terms of classification accuracy and predictor extraction, it is similar with binary logistic regression, particularly in sufficiently large populations (ie, >50).20 In lieu of its capability to produce a predictive linear function that can categorize sizeable populations with considerable accuracy compared with other methods, linear DFA represents a viable approach to our study's aims.
Input Variable Selection for DFA
Input variable selection in linear DFA has been shown to produce simpler models with improved predictive accuracy that would otherwise be hindered by the presence of redundant variables.21 In this study, we opted to base the variable selection process by producing a cutoff in the univariate analyses test statistic, ie, the independent samples t test.
Comparisons of t statistics to a critical value rely mainly on (1) degrees of freedom for a given sample, and (2) the desired (two‐tailed) level of significance. If t stat>t critical, the null hypothesis of equal group means is rejected.22 In order to obtain a t stat cutoff, we first determined the average P value for all statistically significant variables from the independent samples t test (Table 2). The values produced a mean of 0.00297±0.00714. For 1226 degrees of freedom, this probability level corresponds to a t crit=2.976. As no t stat ∈ [2.976, 3.0], the cutoff was rounded to 3.
Table 2.
Univariate Analysis Between Hypertension and Demographic, Respiratory, and Sleep Apnea Characteristics
| Hypertensive Patients | Normotensive Patients | Hypertension P Value | |
|---|---|---|---|
| Age, y | 57.2±11.2 | 45.8±15.8 | <.0001 |
| BMI, kg/m2 | 33.3±6.3 | 30.3±5.8 | <.0001 |
| CCI | 1.8±2 | 0.5±1.1 | <.0001 |
| ESS | 10.1±9.9 | 8.5±4.9 | <.0001 |
| FEV1, % | 86.3±18.5 | 95.9±41.5 | <.0001 |
| FVC, % | 87.1±16.6 | 96.3±15.1 | <.0001 |
| FEV1/FVC | 79.9±8.3 | 81.2±6.2 | .003 |
| Daytime SaO2, % | 96.6±2 | 97.5±1.6 | <.0001 |
| Mean SaO2, % | 87.7±5.5 | 89.2±5.3 | <.0001 |
| Minimum SaO2, % | 75.5±11.8 | 80.2±11.1 | <.0001 |
| REM mean SaO2, % | 89.8±5.7 | 92.3±6.2 | <.0001 |
| NREM mean SaO2, % | 93.3±39.8 | 93±3.1 | .848 |
| DI | 42±29.3 | 32.1±31.5 | <.0001 |
| AHI | 36.5±26.6 | 28.7±28.6 | <.0001 |
| Apneas/h | 14.4±18 | 12.2±18.5 | .023 |
| Hypopneas/h | 22.3±17.9 | 17.3±17.3 | <.0001 |
| AI | 39.7±36.2 | 35.4±24.4 | .019 |
Abbreviations: AHI, apnea‐hypopnea index; AI, arousal index; apneas/h, number of apneas per hour of total sleep time; BMI, body mass index; CCI, Charlson Comorbidity Index; daytime SaO2, daytime mean oxygen saturation; DI, desaturation index; ESS, Epworth Sleepiness Scale; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; hypopneas/h, number of hypopneas per hour of total sleep time; mean SaO2, mean oxygen saturation during respiratory events; minimum SaO2, minimum oxygen saturation during sleep; NREM mean SaO2, mean oxygen saturation during non‐rapid eye movement sleep, REM mean SaO2, mean saturation during rapid eye movement sleep. Values are expressed as mean±standard deviation. Spirometry data were available for approximately 938 of 1227 patients and analyzed with independent samples t test.
As spirometry data were available for approximately 938 of 1227 patients, we did not include these variables in the multivariate analysis since it would greatly reduce the predictive power of the discriminant function. Furthermore, spirometry data were based on information from the individual medical history of the patients and not collected by standard procedures, ie, as part of our study or from a single pulmonary clinic. For these reasons, they were included in the univariate analyses as descriptive between groups but otherwise excluded from the multivariate analyses.
By employing a t statistic cutoff value ≥3, we selected age, body mass index (BMI), CCI, daytime mean SaO2, mean SaO2 during respiratory events, mean saturation during REM (REM mean SaO2), desaturation index (DI), AHI, number of hypopneas per hour of total sleep time (hypopneas/h), and Epworth Sleepiness Scale (ESS) for the discriminant model.
Subsequently, we retrospectively compared the predictive accuracy of a discriminant function (D a) including all statistically significant univariate predictors vs a postvariable selection discriminant function (D b) to determine the optimal model; D a's predictive accuracy was estimated to be 70.1% vs 73.9% for D b.
Interpretation of Discriminant Loadings
Discriminant loadings are essentially coefficients describing the correlation between each independent variable and the discriminant function.19 In a similar manner to typical correlation coefficients (Pearson's or Spearman's), a ±0.30 cutoff is commonly interpreted as the limit between less important and more important variables.19, 23, 24 It should be stressed that this interpretation regards the contribution of each predictor to the function; as such, they are qualitatively characterized by their loadings but are not censored from the function itself.
For all analyses, a P value <.05 was considered statistically significant. Statistical analysis was performed using SPSS 19.0 (IBM Corporation, San Diego, CA).
Results
Table 1 shows anthropometric, clinical history, and respiratory characteristics (spirometry and PSG data) of the studied population. Of the studied population, 60.2% had an AHI >15. A total of 554 patients (37.6%) had hypertension, and 392 (70.8%) of hypertensive individuals had an AHI >15.
Table 1.
Demographic, Respiratory, and Sleep Apnea Characteristics of the Studied Population
| Age, y | 50±15.3 |
| Male sex % | 83.6 |
| BMI, kg/m2 | 31.5±6.2 |
| CCI | 1±1.6 |
| ESS | 9.1±7.2 |
| Current smokers, % | 39.5 |
| Hypertensive, % | 37.6 |
| FEV1, % | 92.2±34.9 |
| FVC, % | 92.7±16.3 |
| FEV1/FVC | 80.7±7.1 |
| Daytime SaO2, % | 97.1±1.8 |
| Mean SaO2, % | 88.7±5.5 |
| Minimum SaO2, % | 78.2±11.6 |
| REM mean SaO2, % | 91.4±6.1 |
| NREM mean SaO2, % | 93.1±23.4 |
| DI | 35.7±31 |
| AHI | 32±28.2 |
| AI | 36.8±28.9 |
Abbreviations: AHI, apnea‐hypopnea index; AI, arousal index; BMI, body mass index; CCI, Charlson Comorbidity Index; daytime SaO2, daytime mean oxygen saturation; DI, desaturation index; ESS, Epworth Sleepiness Scale; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; mean SaO2, mean oxygen saturation during respiratory events; minimum SaO2, minimum oxygen saturation during sleep; NREM mean SaO2, mean oxygen saturation during non‐rapid eye movement sleep; REM mean SaO2, mean oxygen saturation during rapid eye movement. Continuous variables are presented as mean±standard deviation and discrete variables as percentages.
Anthropometric, clinical history, and respiratory characteristics (continuous variables) of hypertensive and normotensive individuals are presented in Table 2. Hypertensive patients were older (mean, 57.1±11.2 years vs 45.8±15.8 years) and more obese (mean BMI, 33.3±6.3 kg/m2 vs 30.3±5.8 kg/m2) than normotensive patients.
Univariate analysis determined age, BMI, CCI, ESS, forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), FEV1/FVC, daytime mean SaO2, mean SaO2 during respiratory events, minimum SaO2 during sleep, mean saturation during REM (REM mean SaO2), DI, AHI, and ESS to be significantly associated with hypertension (Table 2). There were no significant differences between hypertensive and normotensive patients in terms of sex and smoking.
Multivariate analysis was subsequently performed via the application of a linear discriminant model. Table 3 shows the canonical discriminant function coefficients, ie, the unstandardized coefficients used to create the discriminant model:
| (1) |
Table 3.
Discriminant Function Coefficients
| Variable | Coefficient |
|---|---|
| Age | 0.038 |
| CCI | 0.330 |
| BMI | 0.068 |
| Daytime SaO2 | −0.071 |
| Minimum SaO2 | −0.025 |
| REM mean SaO2 | 0.012 |
| Mean SaO2 | −0.018 |
| DI | −0.005 |
| Hyponeas/h | 0.005 |
| AHI | −0.004 |
| ESS | 0.016 |
Abbreviations: AHI, apnea‐hypopnea index; BMI, body mass index; CCI, Charlson Comorbidity Index; daytime SaO2, daytime mean oxygen saturation; DI, desaturation index; ESS, Epworth Sleepiness Scale; hypopneas/h, number of hypopneas per hour of total sleep time; mean SaO2, mean oxygen saturation during respiratory events; minimum SaO2, minimum oxygen saturation during sleep; REM mean SaO2, mean saturation during rapid eye movement sleep.
Table 4 displays the structure matrix equation (1), namely the correlations between each variable and the discriminant function. By setting a cutoff of 0.3 (absolute value) for the interpretation of the discriminant loadings, age, BMI, CCI, daytime SaO2, mean SaO2, minimum SaO2, and REM mean SaO2 were deemed as the most accurate predictors for hypertension. AHI, DI, and ESS were not assessed as the most dominant predictive factors for development of hypertension. The overall cross‐validated model accuracy of this model was determined to be 73. The single derived discriminant function was statistically significant (Wilk's lambda=0.771, χ2=289.070, P<.0001).
Table 4.
Structure Matrix Displaying the Correlation of Each Predictor With the Discriminant Function
| Predictors of Hypertension | Discriminant Loadings |
|---|---|
| Age | 0.692 |
| CCI | 0.667 |
| BMI | 0.446 |
| Daytime SaO2 | −0.426 |
| Minimum SaO2 | −0.386 |
| REM mean SaO2 | −0.350 |
| Mean SaO2 | −0.326 |
| DI | 0.284 |
| Hyponeas/h | 0.275 |
| AHI | 0.243 |
| ESS | 0.241 |
| Wilk's lambda=0.771, χ2=289.070, P<.0001 |
Abbreviations: AHI, apnea‐hypopnea index; BMI, body mass index; CCI, Charlson Comorbidity Index; daytime SaO2, daytime mean oxygen saturation; DI, desaturation index; ESS, Epworth Sleepiness Scale; hypopneas/h, number of hypopneas per hour of total sleep time; mean SaO2, mean oxygen saturation during respiratory events; minimum SaO2, minimum oxygen saturation during sleep; REM mean SaO2, mean saturation during rapid eye movement sleep.
Discussion
Analysis of our data indicated several statistically significant differences between individuals with hypertension and those without hypertension. However, age, BMI, comorbidity (CCI), daytime SaO2, and indices of hypoxia during sleep were estimated to be the most precise predictors for hypertension. In contrast, AHI and DI participated weakly in the statistical model. Therefore, although AHI and DI were independent predictive factors for hypertension, both were not included in the most accurate predictors for development of hypertension. Our findings support that daytime and nocturnal hypoxia play an essential role in OSA‐related hypertension.
Scientific data and clinical knowledge about the interaction between OSA and hypertension are continuously increasing. However, whether OSA is truly an independent risk factor for hypertension has yet to be definitively established. The Wisconsin Sleep Cohort revealed a statistically significant association between moderate or worse OSA (AHI ≥15) at baseline and incident hypertension in 4 years (odds ratio of 2.89) compared with those without OSA.11 In contrast, in the more recent 5‐year follow‐up from the Sleep Heart Health Study, O'Connor and colleagues13 reported that the unadjusted risk for hypertension increased in concert with AHI, but that this interaction was not significant after adjustment for BMI. In 2011, Cano‐Pumarega and colleagues14 published data from the Vitoria Sleep Cohort and found that the risk of hypertension increased significantly with higher respiratory disturbance indices, but the odds ratios were no longer significant once adjusted for age and other potential confounding variables. On the other hand, a recent study from Spain identified an increased hazard ratio for incident hypertension in OSA patients compared with control patients, and the correlation between OSA and hypertension remained independent of confounders including age and obesity. Furthermore, follow‐up of this patient cohort disclosed a dose‐response relationship between the severity of OSA and the cumulative incidence of hypertension.12
These discordant conclusions may be related to differences in the study design and the characteristics of the studied populations. Moreover, there are multiple confounding variables for hypertension that usually coexist in OSA patients, such as age and obesity. The prevalence of OSA has been illustrated to increase with age in adults, up to the age of 65.3, 25 In a subgroup analysis of the Sleep Heart Health Study that categorized patients across age groups, OSA patients younger than 60 years were more likely to demonstrate a significant association between minimum SaO2 and the development of hypertension.26 Furthermore, it has long been observed that obesity plays an essential role in the development of OSA. It is estimated that 60% to 90% of patients with OSAS are obese.27 It has recently been proposed that adipose tissue hypoxia may be a trigger of inflammation in obesity, and inflammation is a well‐known intermediary mechanism in cardiometabolic dysfunction.28, 29 Thus, our results amplify the current awareness that hypertension and OSA share common risk factors including age and BMI. Our study supports that AHI, DI, and other parameters of SaO2 included in in‐laboratory PSG––expressions of the severity of OSA––are significant determinants of hypertension. Table 3 shows the correlation of each predictor in the model with the discriminant function. Age, comorbidity (CCI), BMI, daytime SaO2, and indices of hypoxia during sleep are the most precise predictive factors for hypertension. Nevertheless, AHI participates weakly in the statistical model. It seems that AHI plays a synergistic role with age, comorbidity, obesity, daytime, and nocturnal hypoxia in the development of hypertension.
Moreover, the mechanisms underlying hypertension in patients with OSAS are still incompletely understood. Respiratory events in patients with OSAS and intrathoracic pressure swings cause intermittent hypoxia, recurrent hypercapnia, arousals, and sleep fragmentation, with acute changes in blood pressure and heart rate. Repetitive hypoxia–re‐oxygenation plays a pivotal role in the cardiovascular disease process15, 16, 17 and probably activates a broad spectrum of intermediate mechanisms including sympathetic nervous system overactivity,30, 31 inflammation,32, 33 oxidative stress,34, 35, 36 endothelial dysfunction37, 38 and metabolic deregulation involving insulin resistance39, 40 and disordered lipid metabolism.41, 42 There is increasing evidence that nocturnal hypoxia in OSA patients is associated with the eventual development of daytime hypoxia. Analyzing data from the Sleep Heart Health Study, Sanders and colleagues43 reported that patients with sleep apnea without obstructive airway disease had a 20‐fold higher odds ratio for nocturnal desaturation than that of healthy persons, even after adjustment for age, sex, height, weight, race, smoking status, and awaking oxygen saturation. A recent study revealed that patients with OSA, in the absence of lung comorbidity, had lower values of daytime partial pressure of oxygen in arterial blood (PaO2) than those expected on the basis of age. An increase of percent sleep time with reduced SaO2 was associated with a decrease in daytime PaO2.44 Data from the European Sleep Apnea Database (ESADA) cohort study recently showed that both AHI and DI were independently related to prevalent hypertension after adjustment for relevant covariates such as smoking, obesity, dyslipidemia, and diabetes. However, in multiple regression analysis with both DI and AHI in the model, DI was independently associated with prevalent hypertension, whereas AHI was not.45 In addition to that evidence, we found that daytime mean SaO2, mean saturation during respiratory events, minimum saturation during sleep, and mean saturation during REM were included in the most accurate predictors for hypertension, whereas AHI and DI were not. It seems that AHI and DI are more complex measures reflecting the degree of intermittent hypoxia, and therefore are susceptible to variability in the clinical setting. We suggest that daytime and nocturnal hypoxemia as consequences of chronic intermittent hypoxia play a central role in OSA‐related hypertension. In particular, the shift from chronic intermittent hypoxia to daytime and nocturnal hypoxia may represent a direct prelude to the development of hypertension.
Strengths and Limitations
The present data are derived from a large retrospective cohort of patients (1501 individuals) with clinical features of OSAS. All patients underwent full standard in‐laboratory PSG. Multivariate analysis was performed via discriminant function analysis. Discriminant analysis produces a linear function of continuous predictor variables that best allocate patients between two or more naturally occurring groups. In the present study, we used discriminant function analysis to determine which continuous variables distinguish between normotensive and hypertensive individuals.
A possible limitation of our study is the choice of the studied population that may not be representative of the general population. We studied individuals who complained of snoring or/and sleep interruption and excessive daytime sleepiness and had been consecutively referred to our laboratory for investigation of possible OSA. However, this should not be a significant limitation since the principal objective was to examine the relationship between OSAS and hypertension. The fact that the majority of the studied population was male may also be a bias of our study. Nevertheless, there are several studies in which the majority of examined patients were men.12, 37, 38, 45 Furthermore, hypertensive individuals were defined as patients who were previously diagnosed as hypertensive and were also taking at least one antihypertensive agent. Blood pressure measurements taken in the sleep clinic were not used to diagnose hypertension, as these were single readings obtained in the sitting position, which cannot be used as a reliable indicator for a hypertension definition. Moreover, single clinic blood pressure readings might be affected by ongoing medication and could be transiently elevated in some patients because of a white‐coat effect.46, 47
Conclusions
Our findings amplify the current awareness that there is a significant association between OSA and hypertension. Several well‐known risk factors for OSA such as age and obesity are also risk factors for hypertension. Our study revealed that age, BMI, comorbidity, and daytime and nocturnal hypoxia are the most accurate predictive factors for development of hypertension. We suggest that hypoxemia plays an important role in OSAS‐related hypertension. Consequently, daytime SaO2 and indices of hypoxia during sleep should be further evaluated as possible severity markers in OSAS patients.
Disclosures
The authors report no specific funding in relation to this research and no conflicts of interest to disclose. This was not an industry‐supported study.
Supporting information
Data S1. Predictive level of daytime/nocturnal mean oxygen saturation.
Figure S1. Receiver operating characteristic curve for the discriminant score produced by function (1).
Figure S2. Linear representation of the relationship between the cutoff value and each respective centroid (hypertensive vs normotensive).
J Clin Hypertens (Greenwich). 2016;18:146–152. DOI: 10.1111/jch.12645. © 2015 Wiley Periodicals, Inc.
References
- 1. Sleep‐related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–689. [PubMed] [Google Scholar]
- 2. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc. 2011;86:549–554; quiz 554–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Drager LF, Genta PR, Pedrosa RP, et al. Characteristics and predictors of obstructive sleep apnea in patients with systemic hypertension. Am J Cardiol. 2010;105:1135–1139. [DOI] [PubMed] [Google Scholar]
- 5. Fletcher EC, DeBehnke RD, Lovoi MS, Gorin AB. Undiagnosed sleep apnea in patients with essential hypertension. Ann Intern Med. 1985;103:190–195. [DOI] [PubMed] [Google Scholar]
- 6. Guilleminault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 1976;27:465–484. [DOI] [PubMed] [Google Scholar]
- 7. Kales A, Bixler EO, Cadieux RJ, et al. Sleep apnoea in a hypertensive population. Lancet. 1984;2:1005–1008. [DOI] [PubMed] [Google Scholar]
- 8. Stradling J, Davies RJ. Sleep apnea and hypertension–what a mess! Sleep. 1997;20:789–793. [DOI] [PubMed] [Google Scholar]
- 9. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–1239. [DOI] [PubMed] [Google Scholar]
- 10. Konecny T, Kara T, Somers VK. Obstructive sleep apnea and hypertension: an update. Hypertension. 2014;63:203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep‐disordered breathing and hypertension. N Engl J Med. 2000;342:1378–1384. [DOI] [PubMed] [Google Scholar]
- 12. Marin JM, Agusti A, Villar I, et al. Association between treated and untreated obstructive sleep apnea and risk of hypertension. JAMA. 2012;307:2169–2176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. O'Connor GT, Caffo B, Newman AB, et al. Prospective study of sleep‐disordered breathing and hypertension: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2009;179:1159–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cano‐Pumarega I, Durán‐Cantolla J, Aizpuru F, et al. Obstructive sleep apnea and systemic hypertension: longitudinal study in the general population: the Vitoria Sleep Cohort. Am J Respir Crit Care Med. 2011;184:1299–1304. [DOI] [PubMed] [Google Scholar]
- 15. Levy P, Ryan S, Oldenburg O, Parati G. Sleep apnoea and the heart. Eur Respir Rev. 2013;22:333–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McNicholas WT, Bonsigore MR, the Management Committee of EU COST ACTION B26 . Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J. 2007;29:156–178. [DOI] [PubMed] [Google Scholar]
- 17. Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52:686–717. [DOI] [PubMed] [Google Scholar]
- 18. Hall WH, Ramachandran R, Narayan S, et al. An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer. 2004;4:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Burns RB, Burns RA (eds). Business Research Methods and Statistics Using SPSS. London: SAGE Publications Ltd; 2009. Additional advanced chapters on Companion Websites; Chapter 25‐ Discriminant analysis; 589‐607. http://www.uk.sagepub.com/burns/website%20material/Chapter%2025%20-%20Discriminant%20Analysis.pdf. Accessed June 5, 2015. [Google Scholar]
- 20. Antonogeorgos G, Panagiotakos DB, Priftis KN, Tzonou A. Logistic regression and linear discriminant analyses in evaluating factors associated with asthma prevalence among 10‐ to 12‐years‐old children: divergence and similarity of the two statistical methods. Int J Pediatr. 2009;2009:952042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Louw N, Steel SJ. Input Variable Selection in Kernel Fisher Discriminant Analysis. In: Spiliopoulou M, Kruse R, Borgelt C, Nuruberger A, Gaul W, eds. From Data and Information Analysis to Knowledge Engineering. Heidelberg: Springer; 2006:126–133. [Google Scholar]
- 22. NIST/SEMATECH e‐Handbook of Statistical Methods. http://www.itl.nist.gov/div898/handbook/eda/section3/eda3672.htm. Accessed June 5, 2015.
- 23. Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003;44:614–619. [PubMed] [Google Scholar]
- 24. Field A. Multivariate Analysis of Variance (MANOVA). In: Carmichael M, ed. Discovering Statistics Using IBM SPSS Statistics, 4th edn. London: SAGE Publications Ltd; 2013:623–664. [Google Scholar]
- 25. Young T, Shahar E, Nieto FJ, et al; Sleep Heart Health Study Research Group . Predictors of sleep‐disordered breathing in community‐dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162:893–900. [DOI] [PubMed] [Google Scholar]
- 26. Haas DC, Foster GL, Nieto FJ, et al. Age‐dependent associations between sleep‐disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the Sleep Heart Health Study. Circulation. 2005;111:614–621. [DOI] [PubMed] [Google Scholar]
- 27. Peppard PE, Young T, Palta M, et al. Longitudinal study of moderate weight change and sleep‐disordered breathing. JAMA. 2000;284:3015–3021. [DOI] [PubMed] [Google Scholar]
- 28. Berg AH, Scherer PE. Adipose tissue, inflammation, and cardiovascular disease. Circ Res. 2005;96:939–949. [DOI] [PubMed] [Google Scholar]
- 29. Trayhurn P, Wang B, Wood IS. Hypoxia in adipose tissue: a basis for the dysregulation of tissue function in obesity? Br J Nutr. 2008;100:227–235. [DOI] [PubMed] [Google Scholar]
- 30. Fletcher EC, Bao G, Li R. Renin activity and blood pressure in response to chronic episodic hypoxia. Hypertension. 1999;34:309–314. [DOI] [PubMed] [Google Scholar]
- 31. Tamisier R, Pépin JL, Rémy J, et al. 14 nights of intermittent hypoxia elevate daytime blood pressure and sympathetic activity in healthy humans. Eur Respir J. 2011;37:119–128. [DOI] [PubMed] [Google Scholar]
- 32. Arnaud C, Poulain L, Lévy P, Dematteis M. Inflammation contributes to the atherogenic role of intermittent hypoxia in apolipoprotein‐E knock out mice. Atherosclerosis. 2011;219:425–431. [DOI] [PubMed] [Google Scholar]
- 33. Ryan S, Taylor CT, McNicholas WT. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation. 2005;112:2660–2667. [DOI] [PubMed] [Google Scholar]
- 34. Christou K, Kostikas K, Pastaka C, et al. Nasal continuous positive airway pressure treatment reduces systemic oxidative stress in patients with severe obstructive sleep apnea syndrome. Sleep Med. 2009;10:87–94. [DOI] [PubMed] [Google Scholar]
- 35. Christou K, Moulas AN, Pastaka C, Gourgoulianis KI. Antioxidant capacity in obstructive sleep apnea patients. Sleep Med. 2003;4:225–228. [DOI] [PubMed] [Google Scholar]
- 36. Christou K, Markoulis N, Moulas AN, et al. Reactive oxygen metabolites (ROMs) as an index of oxidative stress in obstructive sleep apnea patients. Sleep Breath. 2003;7:105–110. [DOI] [PubMed] [Google Scholar]
- 37. Baguet JP, Hammer L, Lévy P, et al. The severity of oxygen desaturation is predictive of carotid wall thickening and plaque occurrence. Chest. 2005;128:3407–3412. [DOI] [PubMed] [Google Scholar]
- 38. Jafari B, Mohsenin V. Endothelial dysfunction and hypertension in obstructive sleep apnea – is it due to intermittent hypoxia? J Cardiovasc Dis Res. 2013;4:87–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Punjabi NM, Sorkin JD, Katzel LI, et al. Sleep‐disordered breathing and insulin resistance in middle‐aged and overweight men. Am J Respir Crit Care Med. 2002;165:677–682. [DOI] [PubMed] [Google Scholar]
- 40. Priou P, Le Vaillant M, Meslier N, et al; The IRSR Sleep Cohort Group . Independent association between obstructive sleep apnea severity and glycated hemoglobin in adults without diabetes. Diabetes Care. 2012;35:1902–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Li J, Savransky V, Nanayakkara A, et al. Hyperlipidemia and lipid peroxidation are dependent on the severity of chronic intermittent hypoxia. J Appl Physiol (1985). 2007;102:557–563. [DOI] [PubMed] [Google Scholar]
- 42. Levy P, Bonsignore MR, Eckel J. Sleep, sleep‐disordered breathing and metabolic consequences. Eur Respir J. 2009;34:243–260. [DOI] [PubMed] [Google Scholar]
- 43. Sanders MH, Newman AB, Haggerty CL, et al; for The Sleep Heart Health Study . Sleep and sleep‐disordered breathing in adults with predominantly mild obstructive airway disease. Am J Respir Crit Care Med. 2003;167:7–14. [DOI] [PubMed] [Google Scholar]
- 44. Fanfulla F, Grassi M, Taurino AE, et al. The relationship of daytime hypoxemia and nocturnal hypoxia in obstructive sleep apnea syndrome. Sleep. 2008;31:249–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tkacova R, McNicholas WT, Javorsky M, et al; on behalf of the European Sleep Apnoea Database study collaborators . Nocturnal intermittent hypoxia predicts prevalent hypertension in the European Sleep Apnoea Database cohort study. Eur Respir J. 2014;44:931–941. [DOI] [PubMed] [Google Scholar]
- 46. Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26:1505–1526. [DOI] [PubMed] [Google Scholar]
- 47. Parati G, Omboni S, Bilo G. Why is out‐of‐office blood pressure measurement needed? Home blood pressure measurements will increasingly replace ambulatory blood pressure monitoring in the diagnosis and management of hypertension. Hypertension. 2009;54:181–187. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Predictive level of daytime/nocturnal mean oxygen saturation.
Figure S1. Receiver operating characteristic curve for the discriminant score produced by function (1).
Figure S2. Linear representation of the relationship between the cutoff value and each respective centroid (hypertensive vs normotensive).


