Abstract
The authors conducted a study to assess the effects of yoga on blood pressure (BP). Patients were randomized to yoga (Blood Pressure Education Program [BPEP]), or a combined program (COMBO). Ambulatory BP was measured at baseline and at 12 and 24 weeks. Data are presented for all enrolled patients (n=137) and for completers only (n=90). Systolic BP (SBP) and diastolic BP (DBP) were significantly decreased within all groups at 12 and 24 weeks (P<.001) for enrolled patients and completers. SBP was significantly reduced in the yoga and COMBO groups as compared with the BPEP group at 12 weeks in all enrolled and completers. SBP differences were no longer significant at 24 weeks between groups in all enrolled patients; however, there was a greater reduction in SBP at 24 weeks in completers favoring BPEP over yoga. No differences in DBP between groups or in BP between the yoga and COMBO groups were present. The authors did not observe an additive benefit from combining yoga with BPEP measures. Reasons for this are unclear at this time. BP lowering with yoga, however, was similar to that achieved with lifestyle measures.
Hypertension is a major public health issue and affects approximately 70 million adults in the United States and more than a billion people worldwide and is a major risk factor in the development of stroke and cardiovascular and chronic kidney disease.1 The initial treatment of mild to moderate hypertension is to encourage lifestyle modification (LSM) before initiating drug therapy. LSM includes reducing dietary sodium intake, adoption of the Dietary Approaches to Stop Hypertension (DASH) diet (rich in fruits, vegetables, low‐fat dairy foods, and low saturated fats), encouragement of weight loss, reduction of alcohol intake, and increasing physical activity.2 LSMs are often difficult for patients to incorporate and successfully maintain, and many patients go on to require drug therapy to treat their hypertension effectively. Yoga has emerged as a popular approach to blood pressure (BP) reduction in Western cultures and represents an attractive alternative in patients with mild to moderate hypertension preferring to avoid the use of medication or additional medication.3, 4
We conducted a pilot study in which we observed significant decreases in 24‐hour ambulatory BP (ABP) readings after a 12‐week period of yoga participation.5 Based on this we conducted a larger randomized trial, the Lifestyle Modification and Blood Pressure Study II (LIMBS II), to determine the effects of yoga and enhanced LSM, alone or together, on lowering BP in patients with prehypertension and stage 1 hypertension.6 Our hypothesis was that yoga would be as effective as a dietary intervention. To our knowledge, no prior study of yoga has examined whether it adds to a dietary intervention; thus, we introduced this novel aspect as a third arm in our protocol.
Methods
Study Design
LIMBS II is a phase 2 randomized, nonblinded, prospective, controlled trial to assess the safety and efficacy of a 24‐week structured yoga program (YP) vs BP education program (BPEP) vs a combined yoga and education intervention (COMBO). The study population included adults aged 18 to 80 years with prehypertension to stage 1 hypertension who were not taking any antihypertensive medications for at least 3 months prior to participation in the study. The study was performed at a single center using a parallel design. Eligibility was determined by two screening visits with a mean of three office BP readings at each screening in the range of systolic BP (SBP) 130 mm Hg to 160 mm Hg and diastolic BP (DPB) <100 mm Hg. Inclusion and exclusion criteria are detailed in Table 1.
Table 1.
Inclusion and Exclusion Criteria for Lifestyle Modification and Blood Pressure Study
| Inclusion criteria |
| Willingness to and capacity for giving written informed consent |
| Age ≥18 y |
| Systolic blood pressure (SBP) ≥130 mm Hg but <160 mm Hg |
| Willingness to comply with all study‐related procedures |
| Exclusion criteria |
| Pregnancy or postpartum ≤3 months |
| Currently taking blood pressure–lowering medications or dietary supplements (eg, magnesium, potassium, calcium >1200 mg/d, fish oil, ephedra, hawthorn, forskolin) |
| Stage 2 hypertension (SBP >160 mm Hg OR diastolic blood pressure ≥100 mm Hg) |
| Nondominant arm circumference >50 cm |
| Body mass index ≥40.0 kg/m2 |
| Practiced yoga >1 time per month in the previous 6 months |
| Diabetes mellitus or established cardiovascular disease |
| Known arrhythmias such as atrial flutter or fibrillation or cardiac pacemaker |
| Any tobacco use (within the previous 30 days) |
| History of chronic kidney disease based on estimated glomerular filtration rate <60 mL/min |
| Consumption of >7 alcoholic drinks per week (for women) and >14 drinks per week (for men) Known autonomic neuropathy (eg, Shy‐Drager syndrome, orthostatic hypotension) |
| Known secondary causes of hypertension (renal artery stenosis, pheochromocytoma, coarctation of aorta, hyperaldosteronism) |
| Use of benzodiazepines, antipsychotic drugs (3‐month stable use of selective serotonin reuptake inhibitors allowed), or steroids |
| Known severe musculoskeletal problems such as spinal stenosis that may limit participation in yoga |
| Practice of other mind‐body therapies such as qigong, tai chi, or meditation |
Screening, inpatient stays, and follow‐up visits were conducted at the Clinical and Translational Research Center (CTRC) of the University of Pennsylvania (Penn). The YP intervention was conducted offsite at Studio 34 (Studio 34 Yoga, LLC) in West Philadelphia. The study was approved by the institutional review board and all participants provided written informed consent prior to participation in the study. Comprehensive details of the study methods have been previously published.6 All potential participants were interviewed first by a scripted telephone conversation to ensure that they met inclusion and exclusion criteria and, if eligible, participants had two outpatient BP screening visits at the CTRC.
Once eligible participants were enrolled they had three overnight visits to the CTRC, where they underwent 24‐hour ABP monitoring (ABPM), which was repeated at 12 and 24 weeks after randomization. Blood, saliva, and urine samples were collected. The entire study duration averaged 28 weeks, including two screening visits, three evaluation visits, and a termination visit.
Randomization
After completion of the baseline 24‐hour ABP visit, participants were randomized to either the YP, BPEP, or COMBO intervention using a simple (nonstratified), blocked randomization. Small blocks of six were used to avoid imbalances and ensure that no group was off by more than three participants per cohort. Using this system, a biostatistician from the Center for Clinical Epidemiology and Biostatistics at Penn generated a list from which patients were randomized in order of enrollment. Study classes began within 1 to 3 weeks of randomization.
Primary Outcomes
The primary outcome of LIMBS II was to determine the effect of a structured 24‐week YP on mean 24‐hour ABP in adults with prehypertension and stage 1 hypertension. In addition, LIMBS aimed to establish whether the combined effects of YP and BPEP were more effective in reducing 24‐hour ABP than either intervention alone.
BP Measurement
Screening BP and heart rate were recorded at two screening visits in the CTRC using the Datascope Accutorr Plus machine (Paramus, NJ) with an appropriately sized cuff. The patient was seated in a semirecumbent position for 5 minutes prior to the first BP reading. Three readings were taken at 1‐minute intervals and a mean was derived from this set. Eligible patients returned for an inpatient stay at weeks 0, 12, and 24 for ABP, which was recorded over 24 hours using Spacelabs model 90207 monitors (Snoqualmie, WA).7 Participants remained in the CTRC during the inpatient stay and were sedentary. Data were determined to be satisfactory if there were at least 48 (80%) acceptable readings (SBP between 70 mm Hg and 280 mm Hg and DBP between 40 mm Hg and 150 mm Hg) between 6 am and midnight, and six acceptable readings between midnight and 6 am. If any three consecutive readings averaged >180 mm Hg for SBP, or >110 mm Hg for DBP, the participant was discontinued.
Interventions
The YP intervention consisted of three components: semiprivate structured classes, self‐practice, and community‐structured classes. Patients started with biweekly yoga classes, gradually adding a self‐practice, and after the first 12 weeks, patients were transitioned into regularly, structured, community classes. All classes were taught by one of Studio 34's certified Forrest Yoga (FY) instructors. FY (http://www.forrestyoga.com) is a form of Hatha yoga. The 90‐minute class sequence and the structure of the YP have been previously described.6 Patients were provided with a 90‐minute DVD for home practice. YP participants were asked to record home practices to monitor progress and encourage accountability. The self‐practice was optional for the combined intervention patients.
The BPEP consisted of small‐group health education classes and a walking program, which has been previously described in detail.6 In total, the BPEP included 12 nutrition classes and 12 motivational experiences. BPEP patients were also expected to walk 6 days a week, gradually increasing to 180 minutes of walking per week or 10,000 steps per day. BPEP patients were provided with a pedometer to increase compliance and track progress. The nutrition classes provided a community atmosphere that mirrored that felt by YP participants attending community classes.
COMBO patients were required to attend two yoga classes per week in addition to the biweekly nutrition lecture and walking program. Home practices and motivational sessions were optional for COMBO patients.
Statistical Approach
Sample size
All sample size calculations were performed and verified using nQuery version 4 (Dataxiom Software Inc, Los Angeles, CA). We calculated that using a sample size of 34 in each group using one‐way analysis of variance (ANOVA) we would have 80% power to detect at the 0.05 level. Using these estimates, we would need to enroll 40 patients per group, anticipating a 15% dropout rate and aiming to have 34 completers per group or 102 total completed patients.
Statistical Analysis
All intermediate computations, statistical analyses, and graphical presentations were produced using SAS version 9 (SAS Institute, Cary, NC). Data quality was assessed by descriptive summaries and graphical methods to examine sample distribution of the key variables. This was done for demographic and outcome variables of interest. Based on our experience in our prior study we anticipated that the population distributions of the outcome variables for primary and secondary outcomes would be normal. We evaluated the balance between groups achieved by randomization, baseline values for variables of interest and compared between the YP, BPEP, and combined interventions. Group differences for continuous characteristics were computed using one‐way ANOVA. Proportions were compared between groups using the chi‐square test, or Fisher exact tests when expected cell counts were <5.
The primary outcome was the change in mean 24‐hour SBP and DBP. This endpoint was derived from ABPM. Mean 24‐hour SBP and DBP were calculated for each patient as (week 24 – baseline). Differences in the mean change between the YP, BPEP, and combined interventions were compared using the time‐group interactions under the random effect repeated measures ANOVA model in SAS PROC MIXED. An analogous test of group differences in mean change from baseline to 12 weeks were also provided by the random effects repeated measures ANOVA model. Although 12‐week data were provided and prespecified in the data analysis plan, the main outcome measure was the change in BP at 24 weeks. Analysis was performed for all patients enrolled (intention‐to‐treat analysis) and for completers only (per protocol analysis) and both sets of data are presented.
Safety
LSM was initially indicated for 6 months for patients with uncomplicated prehypertension and stage 1 hypertension.2 During the study, if participants developed worsening hypertension despite the intervention (SBP >180 mm Hg; DBP >110 mm Hg) they were withdrawn from the study and referred to their primary care physicians to initiate medication. If SBP was >180 mm Hg or DBP >110 mm Hg and the patient was symptomatic they were referred to the emergency department or immediately to their primary care physician for further evaluation.
Results
Study Participation and Retention
The study enrolled 137 participants and 90 completed the protocol. Figure 1 shows participant retention, reasons for withdrawal, and time of withdrawal. A total of 18% of participants withdrew either at randomization or within the first week because of dissatisfaction with randomization group or schedule conflicts. The baseline demographics of completers vs noncompleters were compared. The noncompleters were younger, with a mean age of 43.8 years vs 49.6 years (P=.016). The mean baseline BP was lower in the completers vs noncompleters (133/81 mm Hg vs 134/82 mm Hg, P<.05) and was significantly, but not clinically, different. There was an equal distribution of sexes between groups. Baseline body mass index (BMI) and weight were similar.
Figure 1.

Study flow diagram. BPEP indicates Blood Pressure Education Program; Combo, combined yoga and education intervention.
Baseline Demographics, BP, and Laboratory Data
Baseline demographics of enrolled patients are shown in Table 2. There were no significant baseline differences between groups in age, sex, or race. COMBO group patients had a higher baseline BMI and weight than the YP or BPEP groups. Baseline SBP and DBP values were significantly higher in the BPEP group than the YP and COMBO groups. HR was significantly higher in the COMBO group. Approximately two thirds of patients had prehypertension and one third had hypertension, and the distribution was similar across the groups. Baseline kidney function, serum potassium, and glucose levels were similar between groups.
Table 2.
Baseline Demographics for All Enrolled Participants
| Group | Yoga | BPEP | Combination Therapy |
|---|---|---|---|
| Participants, No. | 43 | 48 | 46 |
| Age, y | 47.4 (13) | 46.1 (13) | 48.9 (13) |
| Male/female, No. | 22/21 | 25/23 | 20/26 |
| Race, No. | |||
| African American | 18 | 22 | 28 |
| Asian | 1 | 1 | 0 |
| Caucasian | 23 | 23 | 18 |
| Hispanic | 1 | 2 | 0 |
| BMI, kg/m2 | 28.8 (6.7) | 28.2 (5.9) | 31.2 (6.3)a |
| Weight, kg | 85 (20.7) | 83.0 (17.7) | 93.5 (23.5)a |
| SBP baseline, mm Hg | 132.6 (16.1) | 134.2 (14.6)b | 132.8 (15.2) |
| DBP baseline, mm Hg | 80.6 (13.6) | 82.2 (13.1)b | 81.1 (13.2) |
| HR baseline, beats per min | 61.6 (23.4) | 61.4 (24.4) | 67.2 (22.8)a |
| Creatinine, mg/dL | 0.87 (0.1) | 0.90 (0.2) | 0.88 (0.1) |
| Glucose, mg/dL | 90.7 (9.9) | 89.1 (10.4) | 89.2 (8.9) |
| Potassium, mEq/L | 4.14 (0.2) | 4.11 (0.2) | 4.15 (0.2) |
| Sodium, mEq/L | 138.1 (2.0) | 138.7 (1.7) | 138.4 (1.7) |
Abbreviations: BPEP, Blood Pressure Education Program; BMI, body mass index; DBP, diastolic blood pressure; HR, heart rate; SBP, systolic blood pressure. Values are expressed as mean (standard deviation). a P<.05 combination therapy vs yoga and BPEP. b P<.05 BPEP vs yoga vs combination therapy.
Weight and BMI
There was significant weight gain and increase in BMI within the COMBO intervention from baseline to 24 weeks in the completer analysis, as shown in Figure 2. The significant changes of body weight and BMI may have contributed to changes in BP; therefore, analysis models of ABP data were adjusted for body weight and BMI.
Figure 2.
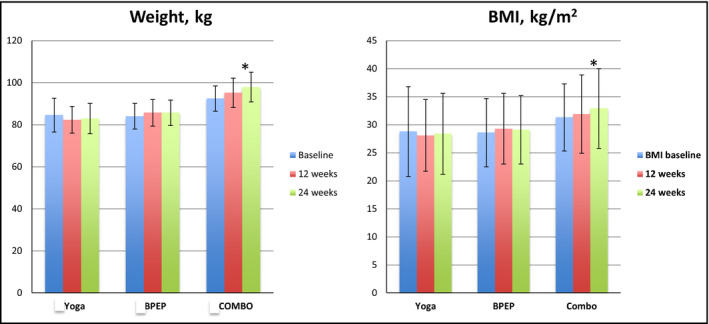
Weight and body mass index (BMI) changes within groups at baseline and 12 and 24 weeks. *Significant weight gain and increase in BMI in the combined yoga and education intervention (COMBO) from baseline to 24 weeks (P<.05). BPEP indicates Blood Pressure Education Program.
ABP data
Data are shown both for all enrolled participants and for completers using only least square means differences. Data are presented both ways as there was a higher than anticipated dropout rate in the study. All data were analyzed using differences in the mean change in BP to account for the higher baseline BP in the BPEP group, as shown in Table 3. BP data within intervention differences for all participants and for completers are shown in Table 4 and Figure 3a, b. There was a significant decrease in both SBP and DBP within all three interventions from baseline to 12 weeks and 24 weeks (P<.001). Results were significant for all the interventions and did not differ when assessing all enrolled patients vs completers only.
Table 3.
BP Changes Within Groups for All Participants (ITT) and All Completers (Per Protocol)
| Yoga | BPEP | Combination Therapy | |
|---|---|---|---|
| BP changes within all participants | |||
| Participants, No. | 43 | 48 | 46 |
| SBP at baseline, mm Hg | 132.6±16.1 | 134.2±14.6 | 132.8±15.2 |
| DBP at baseline, mm Hg | 80.6±13.6 | 82.2±13.1 | 81.1±13.2 |
| SBP at 12 weeks, mm Hg | 129.6±16a | 132.5±16a | 129.6±17a |
| DBP at 12 weeks, mm Hg | 78.6±14a | 80.4±13a | 79±14a |
| SBP at 24 weeks, mm Hg | 129.7±17a | 130.6±16a | 130±17a |
| DBP at 24 weeks, mm Hg | 78±14a | 80±13a | 78.6±14a |
| BP changes within groups for completers only | |||
| Participants, No. | 27 | 34 | 29 |
| SBP baseline, mm Hg | 132.2±16.1 | 134.0±14.6 | 132.5±15.3 |
| DBP baseline, mm Hg | 80.3±13.3 | 82.2±13.2 | 80.6±12.8 |
| SBP at 12 weeks, mm Hg | 128.8±15.4a | 132.4±15.6a | 128.8±16.8a |
| DBP at 12 weeks, mm Hg | 78.4±13.4a | 80.0±12.6a | 77.9±14a |
| SBP at 24 weeks, mm Hg | 129.9±17a | 130.6±15.6a | 130±16.8a |
| DBP at 24 weeks | 78.1±14.3a | 79.9±14a | 78.6±13.8a |
Abbreviations: BP, blood pressure; BPEP, Blood Pressure Education Program. Values are expressed as mean (standard deviation). a P<.0001 and are adjusted for weight and body mass index, systolic blood pressure (SBP), and diastolic blood pressure (DBP).
Table 4.
Mean Change Within Groups in SBP and DBP in All Enrolled Participants (ITT) and Completers (Per Protocol)
| Yoga | BPEP | Combination Therapy | |
|---|---|---|---|
| BP changes in all enrolled | |||
| ΔSBP: baseline to 12 weeks, mm Hg | −3.04 (−3.82 to −2.27)a | −1.61 (−2.31 to −0.91)a | −3.18 (−3.89 to −2.47)a |
| ΔSBP: baseline to 24 weeks, mm Hg | −2.91 (−3.70 to −2.13)a | −3.55 (−4.23 to −2.87)a | −2.81 (−3.52 to −2.10)a |
| ΔDBP: baseline to 12 weeks, mm Hg | −2.01 (−2.67 to −1.35)a | −1.75 (−2.34 to −1.16)a | −2.29 (−2.90 to −1.69)a |
| ΔDBP: baseline to 24 weeks, mm Hg | −2.58 (−3.25 to −1.92)a | −2.32 (−2.90 to −1.74)a | −2.48 (−3.08 to −1.87)a |
| BP changes in completers | |||
| ΔSBP: baseline to 12 weeks, mm Hg | −3.39 (−4.26 to −2.52)a | −1.68 (−2.43 to −0.93)a | −3.69 (−4.47 to −2.92)a |
| ΔSBP: baseline to 24 weeks, mm Hg | −2.26 (−3.12 to −1.39)a | −3.44 (−4.17 to −2.72)a | −2.48 (−3.24 to −1.72)a |
| ΔDBP: baseline to 12 weeks, mm Hg | −1.81 (−2.54 to −1.08)a | −2.09 (−2.72 to −1.45)a | 2.74 (−3.39 to −2.08)a |
| ΔDBP: baseline to 24 weeks, mm Hg | −2.15 (−2.88 to −1.42)a | −2.26 (−2.87 to −1.65)a | 2.01 (−2.65 to −1.37)a |
Abbreviations: ΔBP, change in blood pressure; DBP, diastolic blood pressure; ITT, intention to treat; SBP, systolic blood pressure. Results are expressed as least square means (confidence intervals). a P≤.001.
Figure 3.
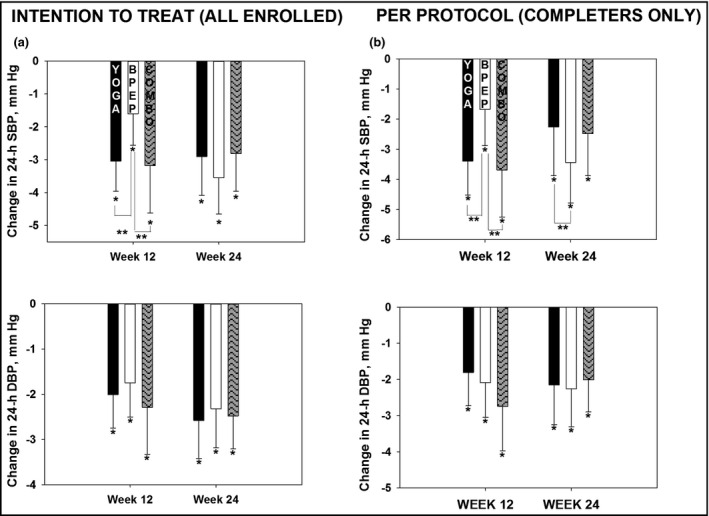
(a) Changes in systolic blood pressure (SBP) and diastolic blood pressure (DBP) for all enrolled participants (intention to treat) at 12 and 24 weeks. *P<.001 for change in SBP and DBP within groups. **P<.01 for difference in SBP between yoga and Blood Pressure Education Program (BPEP), the combined yoga and education intervention (COMBO), and BPEP at 12 weeks. (b) Changes in SBP and DBP for completers (per protocol) at 12 and 24 weeks. *P<.001 for change in SBP and DBP within groups. **P<.01 for difference in SBP between yoga and BPEP, in COMBO and BPEP at 12 weeks, and in SBP between BPEP and yoga at 24 weeks.
Between‐intervention changes adjusted for weight and BMI in SBP between YP and BPEP from baseline to 12 weeks for all enrolled patients were Δ1.1 mm Hg (P=.03) and between BPEP and COMBO were Δ1.5 mm Hg (P=.002), favoring YP and COMBO interventions over BPEP alone at 12 weeks. Differences between interventions were no longer significant at 24 weeks. There were no significant differences between interventions in DBP or between the YP and the COMBO interventions at any time period. For completers, only the between‐group adjusted ABP data showed a significant difference in SBP between YP and BPEP from baseline to 12 weeks (Δ1.6 mm Hg, P=.006) and between BPEP and COMBO (Δ2.08 mm Hg, P<.001), favoring YP and COMBO interventions over BPEP alone at 12 weeks. Between‐intervention changes in SBP from baseline to 24 weeks were only significant between YP and BPEP, favoring the BPEP group (Δ1.27 mm Hg, P=.03). DBP was not different between groups and there was no difference between the YP and the COMBO interventions at any time period.
Biochemical Measures
There were no significant differences in salivary cortisol within or between interventions from baseline to 12 or 24 weeks. There were no significant differences within or between interventions in urine sodium or potassium measurements; however, in the BPEP and COMBO interventions there was a trend toward decreased urine sodium, although changes were not statistically significant.
Discussion
LIMBS II was a rigorously conducted intervention study that assessed the efficacy of yoga on BP reduction by randomizing patients with prehypertension and stage 1 hypertension to either dietary intervention and a walking program; a regular, twice‐weekly, yoga practice; or a combination of these. We utilized ABPM to determine the primary outcome, which is considered the most accurate measure to determine changes in BP and is resistant to placebo effects.8 We observed that all three interventions had a favorable effect on 24‐hour ABP, with reductions in BP from baseline to 12 and 24 weeks in all intervention groups. The analysis was significant whether including all patients enrolled or when limited to only those who completed the study. When comparing between‐intervention differences there was a significantly greater reduction in SBP at 12 weeks in the yoga and the combination group, compared with the control group of diet and walking alone, whether analyzed in the entire cohort or completers only. Differences between interventions were no longer significant at 24 weeks when analyzing the entire cohort (ie, the intention‐to‐treat approach) and this may reflect the difficulty in maintaining lifestyle interventions over a longer period of time. SBP, however, was slightly but significantly reduced at 24 weeks in the diet/walking group vs the yoga group when analyzing completers only (ie, the per‐protocol analysis). An explanation for this is if patients were able to maintain an intervention for the entire study duration, the BPEP intervention could be slightly more effective than yoga. It is also possible that the effect of BPEP alone is slower but steady when the program is followed rigorously and is more evident at 24 weeks; however, we do not know whether this improvement at 24 weeks will be maintained at this level after further follow‐up. We did not observe an additive benefit from combining yoga with BPEP measures. The reasons for this are unclear at this time.
These BP reductions, although small, are noteworthy when compared with data from a meta‐analysis of 1 million adults from 61 prospective observational studies of BP and mortality, which demonstrated that even a small 2‐mm Hg fall in mean SBP was associated with a 7% and 10% decreased risk of death from ischemic heart disease and stroke, respectively.9 This supports the clinical importance that even small reductions in SBP, which can have important cardiovascular morbidity and mortality benefits.
Yoga is increasingly being studied for potential associated health benefits10 and the recent American Heart Association scientific statement regarding use of nonpharmacologic treatments for hypertension11 encouraged a trial of nonpharmacologic interventions (including alternative modalities) as part of initial treatment of stage 1 hypertension among patients wishing to avoid or delay drug therapy when clinically appropriate. It stated that most alternate approaches cause little to no side effects and may represent acceptable options for patients with multiple medication intolerances. They did not recommend yoga because of lack of high‐quality, randomized controlled trials pertaining to the potential BP‐lowering efficacy of yoga, adding that additional larger, high‐quality trials are needed. Aside from a small risk of musculoskeletal injury, there are few cardiovascular risks posed by yoga practice and no adverse events have been reported in published trials, as we observed in the current study. Our data demonstrate that regular weekly practice of yoga is a reasonable alternative, either alone or in combination with dietary and exercise measures, in the management of uncomplicated hypertension, with BP responses similar to those observed by recommended lifestyle interventions.
Three recent meta‐analyses of randomized controlled trials assessed the effects of yoga on BP reduction.12, 13, 14 Despite large differences in study methods, the meta‐analyses found relatively similar findings with respect to BP reduction demonstrating an SBP decrease of 4.2 mm Hg to 9.6 mm Hg and DBP of 3.3 mm Hg to 7.2 mm Hg.12, 13, 14 In the past 3 years there have been six randomized trials published assessing the effects of yoga on BP reduction.4, 5, 15, 16, 17, 18, 19 Despite the improved quality of research being performed in this area there remain issues with data quality and reproducibility, which limits the generalizability of these studies, but overall there does appear to be a real potential for regular yoga use to lower BP.
Our study did show a significant weight gain in the COMBO group. Reasons for this are unclear. Weight loss was not a specified goal of the study. Because of the possible effects of weight loss on BP reduction, the statistical analysis model was adjusted to account for this when analyzing the ABP data.
Limitations
We acknowledge several limitations in our study. There was a larger than anticipated dropout rate of 34% in the study. A total of 18% of patients dropped out within the first 2 weeks after randomization because of dissatisfaction with group randomization; 66% because of poor attendance, schedule conflicts, or time commitments; and 8% because of requiring initiation of drug therapy as a result of SBP >180 mm Hg. Clinical trials using LSMs are challenging to conduct and recent yoga trials for BP reduction report dropout rates in the range of 5% to 48%4, 5, 15, 16 Because the dropout rate was high, we felt it was important to do both an intention‐to‐treat as well as a per‐protocol analysis.
Conclusions
We observed that all three interventions lowered 24‐hour ABP within each group, with some difference in magnitude between interventions noted at 12 weeks that were no longer present at 24 weeks. There was, however, a greater reduction in SBP in the per‐protocol analysis only in the dietary/walking intervention at 24 weeks. We observed that 24 weeks of yoga was associated with 24‐hour ABP reductions similar to the other two interventions including diet and exercise, and a combination of diet and exercise with yoga in patients with prehypertension and untreated stage 1 hypertension. We found it challenging to maintain patients within a nonblinded study because of a priori expectations on the part of some enrollees who were not assigned to an intervention group of their liking. The magnitude of BP reduction we observed was sustained within groups between the 12th and 24th weeks of intervention, as measured by 24‐hour ABPM. Forrest Yoga seems, in our experience, to have a modest but definite beneficial effect on the 24‐hour BP profile of patients and appears to be as effective as LSM.
Disclosures
The study was funded by the National Center for Complementary and Alternative Medicine: 1RO1AT004921‐01A1. The authors have no other conflicts of interest to disclose.
J Clin Hypertens (Greenwich). 2016;18:809–816. DOI: 10.1111/jch.12772. © 2016 Wiley Periodicals, Inc.
Clinical Trials Registration number: NCT00964847
References
- 1. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 2. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 3. Bell RA, Suerken CK, Grzywacz JG, et al. CAM use among older adults age 65 or older with hypertension in the United States: general use and disease treatment. J Altern Complement Med. 2006;12:903–909. [DOI] [PubMed] [Google Scholar]
- 4. Thiyagarajan R, Pal P, Pal GK, et al. Additional benefit of yoga to standard lifestyle modification on blood pressure in prehypertensive subjects: a randomized controlled study. Hypertens Res. 2015;38:48–55. [DOI] [PubMed] [Google Scholar]
- 5. Cohen DL, Bloedon LT, Rothman RL, et al. Iyengar yoga versus enhanced usual care on blood pressure in patients with prehypertension to stage I hypertension: a randomized controlled trial. Evid Based Complement Alternat Med. 2011;2011:546428 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cohen DL, Bowler A, Fisher SA, et al. Lifestyle Modification in Blood Pressure Study II (LIMBS): study protocol of a randomized controlled trial assessing the efficacy of a 24 week structured yoga program versus lifestyle modification on blood pressure reduction. Contemp Clin Trials. 2013;36:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. O'Brien E, Mee F, Atkins N, O'Malley K. Accuracy of the SpaceLabs 90207 determined by the British Hypertension Society protocol. J Hypertens. 1991;9:573–574. [DOI] [PubMed] [Google Scholar]
- 8. Piper MA, Evans CV, Burda BU, et al. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: an updated systematic review for the U.S. preventive services task force. Ann Intern Med. 2015;162:192–204. [DOI] [PubMed] [Google Scholar]
- 9. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 10. McCall MC. In search of yoga: Research trends in a western medical database. Int J Yoga. 2014;7:4–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brook RD, Appel LJ, Rubenfire M, et al. Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association. Hypertension. 2013;61:1360–1383. [DOI] [PubMed] [Google Scholar]
- 12. Hagins M, States R, Selfe T, Innes K. Effectiveness of yoga for hypertension: systematic review and meta‐analysis. Evid Based Complement Alternat Med. 2013;2013:649836 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cramer H, Haller H, Lauche R, et al. A systematic review and meta‐analysis of yoga for hypertension. Am J Hypertens. 2014;27:1146–1151. [DOI] [PubMed] [Google Scholar]
- 14. Cramer H, Lauche R, Haller H, et al. Effects of yoga on cardiovascular disease risk factors: a systematic review and meta‐analysis. Int J Cardiol. 2014;173:170–183. [DOI] [PubMed] [Google Scholar]
- 15. Subramanian H, Soudarssanane MB, Jayalakshmy R, et al. Non‐pharmacological interventions in hypertension: a community‐based cross‐over randomized controlled trial. Indian J Community Med. 2011;36:191–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hagins M, Rundle A, Consedine NS, Khalsa SB. A randomized controlled trial comparing the effects of yoga with an active control on ambulatory blood pressure in individuals with prehypertension and stage 1 hypertension. J Clin Hypertens (Greenwich). 2014;16:54–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wolff M, Sundquist K, Larsson Lonn S, Midlov P. Impact of yoga on blood pressure and quality of life in patients with hypertension––a controlled trial in primary care, matched for systolic blood pressure. BMC Cardiovasc Disord. 2013;13:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blom K, Baker B, How M, et al. Hypertension analysis of stress reduction using mindfulness meditation and yoga: results from the HARMONY randomized controlled trial. Am J Hypertens. 2014;27:122–129. [DOI] [PubMed] [Google Scholar]
- 19. Cade WT, Reeds DN, Mondy KE, et al. Yoga lifestyle intervention reduces blood pressure in HIV‐infected adults with cardiovascular disease risk factors. HIV Med. 2010;11:379–388. [DOI] [PMC free article] [PubMed] [Google Scholar]


