Abstract
An aggressive strategy to manage hypertension in a large integrated healthcare organization achieved blood pressure control in 82% of hypertensive patients, as compared with 52% nationwide. It is unknown why the remaining 18% is uncontrolled. The objective of this study was to identify characteristics associated with patients whose blood pressure remains continuously uncontrolled. This nested case‐control study included 1583 continuously uncontrolled cases and 7901 matched controls. Univariate analysis revealed patients who visited their primary care provider frequently (odds ratio, 0.42; 95% confidence interval, 0.39–0.46) were adherent to antihypertensive medications (odds ratio, 0.12; 95% confidence interval, 0.10–0.14), and dispensed more medications (odds ratio, 0.86; 95% confidence interval, 0.85–0.87) were less likely to be continuously uncontrolled. Patient characteristics that were associated with continuously uncontrolled hypertension were the Patient Health Questionnaire‐9 score and higher body mass index. Since patients with controlled hypertension visited their provider more often, patients with continuously uncontrolled hypertension may benefit from more interaction with their healthcare system.
Hypertension is the most common medical diagnosis in the United States, affecting more than 67 million people,1 and is one of the most significant risk factors for cardiovascular disease (CVD).2, 3, 4, 5 Hypertension contributes to as many as 348,000 deaths a year in the United States.6
Individuals between the ages of 40 and 70 years with a blood pressure (BP) ranging from 115 mm Hg to 185/75–115 mm Hg have a two‐fold increased CVD risk for each incremental elevation of 20 mm Hg systolic BP (SBP) or 10 mm Hg diastolic BP (DBP).6 BP and risk of CVD events have a relationship that is continuous, consistent, and independent of other risk factors. Hypertension correlates with a greater risk of myocardial infarction, heart failure, stroke, and kidney disease; therefore, it is vital to achieve normotensive BP.7, 8, 9 Without broad and effective treatment strategies, hypertension rates are expected to further increase with aging populations.2
Despite aggressive BP control efforts in the United States, currently only 52% of hypertensive patients have achieved BP goal.2 Previous Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines recommend a target of SBP <140 mm Hg and DBP <90 mm Hg to reduce CVD complications, while in patients with hypertension and diabetes or renal disease, a BP goal of <130/80 mm Hg is recommended by JNC 7.7, 10
In comparison with national rates, Kaiser Permanente Southern California (KPSC), a large integrated staff model healthcare system, has attained an overall hypertension control rate of 82% (84% in Caucasians and 79% in African Americans).11 Factors associated with the remaining 18% of the population above BP goals are currently unknown. KPSC has focused efforts to improve hypertension control rates resulting in rapid improvement and exceeding national rates. Sim and colleagues11 published these system‐wide improvement measures, which include: (1) creation of a hypertension registry, (2) BP measurement standardization, (3) the use of an evidence‐based and easy‐to‐remember treatment algorithm, and (4) a multidisciplinary approach to care including medical assistants, nurses, and pharmacists with shared responsibilities in BP management.11, 12 Understanding factors, including practice patterns, associated with patients remaining out of control, might assist clinicians and organizations to better focus scarce healthcare resources.
A recently published retrospective cohort study by our research group13 identified several factors associated with uncontrolled hypertension: African American race, unpartnered relationship status, and high number of dispensed antihypertensive medications. In addition, nonadherence to antihypertensive medications and the presence of moderate depression (identified through Patient Health Questionnaire‐9 score ≥10) were also found to be associated with uncontrolled hypertension. Uncontrolled hypertension in this study was defined as having the last BP reading ≥140 mm Hg systolic and/or ≥90 mm Hg diastolic in the study period. Our research suggested that there was a subset of patients with uncontrolled hypertension with continuously uncontrolled BP that might warrant further investigation.
This study explores a unique patient population, identifying patients with continuously uncontrolled hypertension. Continuously uncontrolled hypertension was defined in this study as all medical office‐based BP readings (100%) with an SBP ≥140 mm Hg and/or DBP ≥90 mm Hg for 18 consecutive months during the study period. The primary objective of this study was to identify risk factors associated with continuously uncontrolled BP in this patient population.
Methodology
We conducted a retrospective, nested case‐control study designed to identify risk factors associated with continuously uncontrolled BP among patients with a diagnosis of hypertension. This study evaluated hypertensive patients during a 3‐year period from January 1, 2010 to December 31, 2012.
Study Population
Patients were identified from an electronic medical record (EMR) database and were included if they were 18 years or older, a member of the health plan for at least 6 months with an International Classification of Diseases‐Ninth Revision (ICD‐9) code for hypertension, and at least one or more elevated medical office BP readings with an SBP ≥140 mm Hg and/or a DBP ≥90 mm Hg. Kaiser Permanente's EMR contains a complete patient medical record including demographics, medical history, social history, family history, imaging records, laboratory results, procedures, surgery, encounter notes, hospitalization, dispensed medication, and refill history. Only patients with three or more BP readings during separate office visits during the 3‐year study period entered into the study. Patients were excluded if they had a hypertension diagnosis of less than 6 months prior to the study period, pregnancy during the study period, incomplete record of BP readings, antihypertensive medications, or marital status.
Kaiser Permanente's prescription drug database was used as the source of the prescription data. This provided detailed information regarding the patients' prescriptions including date written, dispensed date, refill dates, quantity dispensed, and quantity of the prescription written.
Continuously Uncontrolled Hypertension Cases
Cases consisted of continuously uncontrolled hypertension, which was defined as all BP readings (100%) with an SBP ≥140 mm Hg and/or DBP ≥90 mm Hg during the 18 consecutive months of the study period. Current Joint National Committee (JNC 8)14 guidelines had not yet been published during this study period. Therefore, an SBP ≤140 mm Hg and a DBP ≤90 mm Hg, from JNC 7 guidelines,7 were used to determine BP goals in the study to reflect the medical practice in place during the study period. In addition, this goal is also consistent with the Healthcare Effectiveness Data and Information Set (HEDIS) and the Centers for Medicare & Medicaid Services (CMS).15 Patients were not initially stratified based on comorbidities; therefore, BP goals specific for diabetes mellitus (DM) or chronic kidney disease (CKD) were not taken into consideration during the match.
Matched Controls
Controls were defined as patients with hypertension whose last two BP readings in the study period were SBP <140 mm Hg and DBP <90 mm Hg. Both HEDIS and CMS define BP control as an SBP <140 mm Hg and a DBP <90 mm Hg at the most recent BP reading during the measurement year.15 To ensure that this study included patients who had controlled hypertension we used a higher standard of control than that of HEDIS and CMS. Instead of using a single last BP reading, we required that the last two BP readings during the study period be controlled with a reading of <140/90 mm Hg. Five controls were matched to each case by sex, ethnicity, and a date range of birth plus or minus 6 months. This study was designed to probe deeper to identify previously undescribed risk factors associated with uncontrolled hypertension. Since ethnicity was previously described as a risk factor for uncontrolled hypertension in this population,13 we decided to match patients based on ethnicity.13, 16, 17, 18 In order to match appropriately, some control patients were used more than once.
Covariates
Covariates analyzed included demographics, lifestyle, and physiology. This included body mass index (BMI), non–English speaking, and partner status. Partner status compared partnered (married, common law, registered domestic partner) vs unpartnered (single, divorced, separated, legally separated, widowed, unknown marital status, unreported marital status) patients.
In addition, family history of hypertension, thiazide‐naive status (defined as those who have not been dispensed a thiazide medication dating as far back as 1996 in the EMR), total number and therapeutic classes of hypertensive medications dispensed, number of chronic medications (defined as at least 200 consecutive days' supply within the past 6 months of the last BP reading13), and hours of exercise per week were analyzed. The hours of weekly exercise were a self‐reported variable, and if it was not reported, then it was assumed zero hours per week. Other covariates included depression according to the nine‐item Patient Health Questionnaire (PHQ‐9) score, average number of primary care provider (PCP) visits per year, education level, and median household income. Both education and income were based on data from the patients' census block group for 2010 (interpolated to 2012) rather than individual data. Twelve therapeutic classes of antihypertensive medications were examined, which reflected the classes identified from the National Health and Nutrition Examination Survey.19 Angiotensin‐converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) were combined into one category. Combination antihypertensive medications (eg, hydrochlorothiazide and lisinopril) were not evaluated as a single medication; instead, they were treated as two separate classes. Antihypertensive treatment was assessed in the 6‐month period prior to the last BP reading.
In order to narrow down the results from the numerous ICD‐9 codes that were assessed, comorbidities were grouped together rather than analyzed individually. Comorbidities were assessed based on ICD‐9 codes and categorized into 10 different groups: diseases of the digestive system (ICD‐9 codes 520–579), respiratory system (ICD‐9 codes 460–519), circulatory system (ICD‐9 codes 390–459), sense organs (ICD‐9 codes 360–389), nervous system (ICD‐9 codes 320–359), mental disorder (ICD‐9 codes 290–319), diseases of blood or blood‐forming organs (ICD‐9 codes 280–289), endocrine, nutritional and metabolic diseases, immunity disorders (ICD‐9 codes 240–279), and symptoms, signs, and ill‐defined conditions (ICD‐9 codes 780–799). The last category included conditions originating in the perinatal period (ICD‐9 code 760–779); however, it was excluded based on previous exclusion criteria.
Another important variable assessed was adherence to antihypertensive medications, defined as proportion of days covered (PDC) based on the dispensed outpatient prescription fill dates. PDC was calculated based on the prescription dispense dates and calculated days' supply. HEDIS and CMS defined medication adherence as PDC ≥80%.15
Statistical Analysis
Chi‐square and Kruskal‐Wallis tests were used to evaluate demographic and descriptive patient data. Initial univariate examinations of the covariates involved chi‐square tests for discrete or categorical variables, and Wilcoxon rank sum tests for continuous or ordered variables. Conditional logistic regression analysis was used to compute odds ratios (ORs) and 95% confidence intervals (CIs) to evaluate univariate associations between covariates and uncontrolled hypertension and, subsequently, multivariate associations between covariates and uncontrolled hypertension. A post hoc power analysis was completed for 1500 cases and five controls per case with 90% power. If the standard deviation of mean PDC is 0.3 and there is a five‐to‐one ratio of controls to cases, we could detect a difference of <0.028 in mean PDC at the .05 significance level.
Results
There were a total of 9484 patients entered into this study: 1583 cases of continuously uncontrolled hypertension matched with 7901 controls (Figure 1). Because there was an inadequate number of controls to fit the match criteria with all of the cases, 160 controls were used twice and two were used three times. As expected, there was no statistical difference between the two groups in terms of age, sex, and ethnicity (Table).
Figure 1.
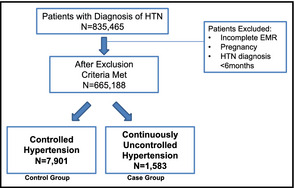
Patient population. HTN indicates hypertension; EMR, electronic medical record.
Table 1.
Patient Demographics
| Controlled Hypertension (n=7901) | Uncontrolled Hypertension (n=1583) | P Value | |
|---|---|---|---|
| Age, mean, y | 58.0 | 58.1 | .90 |
| Male sex, % | 3926 (49.7) | 787 (49.7) | .98 |
| Ethnicity, % | |||
| White | 2689 (34.0) | 538 (34.0) | 1.00 |
| Black | 2267 (28.7) | 455 (28.7) | |
| Hispanic | 2255 (28.5) | 451 (28.5) | |
| Native American/Alaskan | 15 (0.2) | 3 (0.2) | |
| Asian/Pacific Islander | 660 (0.08) | 132 (0.08) | |
| Multiple races | 15 (0.19) | 4 (0.25) | |
Among the univariate conditional logistic regressions, patients dispensed more total medications, more medications for chronic illnesses, or more antihypertensive medications were more likely to have controlled hypertension (OR, 0.86; 95% CI, 0.85–0.87; OR, 0.78; 95% CI, 0.76–0.8; OR, 0.78; 95% CI, 0.74–0.83, respectively). The average number of dispensed chronic medications by the control group was 4.61 compared with the cases 2.85 (P<.0001). Those who were dispensed an ACE inhibitor/ARB, β‐blocker, thiazide, or dihydropyridine (DHP) calcium channel blocker (CCB) were more likely to have continuously uncontrolled hypertension (OR, 1.29; 95% CI, 1.14–1.47; OR, 1.41; 95% CI, 1.26–1.57; OR, 1.59; 95% CI, 1.42–1.78; OR, 2.47; 95% CI, 2.20–2.77, respectively). Similarly, patients dispensed an aldosterone antagonist, sympatholytic, or vasodilators were also more likely to have continuously uncontrolled hypertension (OR, 1.74; 95% CI, 1.34–2.25; OR, 3.06; 95% CI, 2.42–3.86; OR, 4.2; 95% CI, 3.41–5.18, respectively). There was no statistically significant difference between patients dispensed an α‐blocker or an α‐β–blocker (OR, 0.93; 95% CI, 0.74–1.18; OR, 1.06; 95% CI, 0.8–1.41, respectively) (Figure 2).
Figure 2.
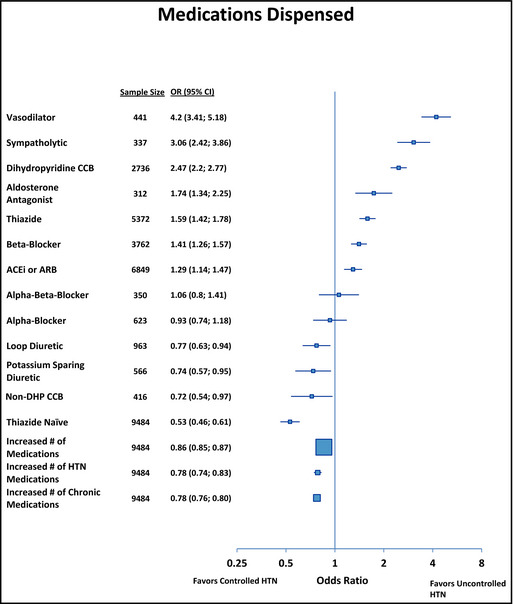
Forest plot of antihypertensive medication dispensed. OR indicates odds ratio; CI, confidence interval; CCB, calcium channel blocker; ACEi, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; DHP, dihydropyridine; HTN, hypertension.
Patients who had greater overall average adherence (determined by PDC ≥80%) with their antihypertensive medications were more likely to have controlled hypertension (OR, 0.12; 95% CI, 0.1–0.14). Patients who were dispensed a CCB but with poor adherence (as determined by PDC <80%), compared with those who were not dispensed a CCB at all, were more likely to have continuously uncontrolled hypertension (OR, 3.21; 95% CI, 2.75–3.75). Similarly, patients dispensed either a thiazide diuretic, vasodilator, or sympatholytic, who were also nonadherent, compared with those who were not dispensed the respective class of antihypertensive, were more likely to have continuously uncontrolled hypertension (OR, 2.05; 95% CI, 1.8–2.33; OR, 4.64; 95% CI, 3.43–6.27; OR, 4.5; 95% CI, 3.11–6.52, respectively). Patients dispensed a vasodilator or sympatholytic and also adherent to the medication, compared to those who were not dispensed the respective antihypertensive medication, were also more likely to have continuously uncontrolled hypertension (OR, 2.35; 95% CI, 1.62–3.41; OR, 1.62; 95% CI, 1.1–2.40, respectively). Patients adherent (PDC ≥80%) to a vasodilator, sympatholytic, or DHP CCB were more likely to have continuously uncontrolled hypertension (OR, 3.73; 95% CI, 2.69–5.17; OR, 2.63; 95% CI, 1.86–3.71; OR, 1.32; 95% CI, 1.13–1.53, respectively) (Figure 3).
Figure 3.
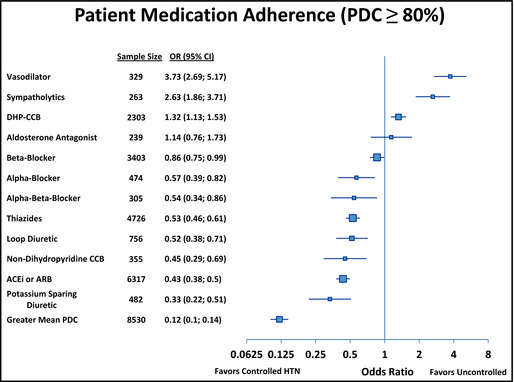
Forest plot of medication adherence (proportion of days covered ≥80%). OR indicates odds ratio; CI, confidence interval; CCB, calcium channel blocker; ACEi, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; DHP, dihydropyridine; HTN, hypertension.
Patients in the control group had an average number of 1.75 PCP visits per year, whereas the cases had an average of 0.89 (P<.0001). Patients who visited their PCP more frequently were also likely to have controlled BP (OR, 0.42; 95% CI, 0.39–0.46). Patients who had a life partner were also more likely to have controlled BP (OR, 0.77; 95% CI, 0.69–0.87). There was no statistically significant difference between cases and controls in terms of family history of hypertension or increased hours per week of exercise (OR, 0.9; 95% CI, 0.8–1.02; OR, 0.98; 95% CI, 0.96–1.01, respectively). Patients who had an increased BMI (defined as BMI ≥30, categorized as obese) or higher PHQ‐9 score (PHQ‐9 score ≥10, representing moderate depression) were more likely to have continuously uncontrolled hypertension (OR, 1.02; 95% CI, 1.02–1.03; OR 1.05; 95% CI, 1.01–1.1, respectively) (Figure 4). In all 10 studied comorbidity categories, there were no statistically significant differences detected between the controls and continuously uncontrolled hypertension groups (P<.0001). However, patients with more disease state comorbidities were more likely to have controlled hypertension (Figure 5).
Figure 4.
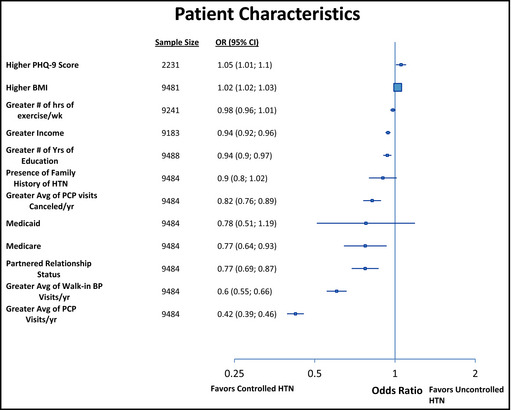
Forest plot of patient characteristics. PDC indicates proportion of days covered; OR, odds ratio; CI, confidence interval; CCB, calcium channel blocker; ACEi, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; DHP, dihydropyridine; HTN, hypertension.
Figure 5.
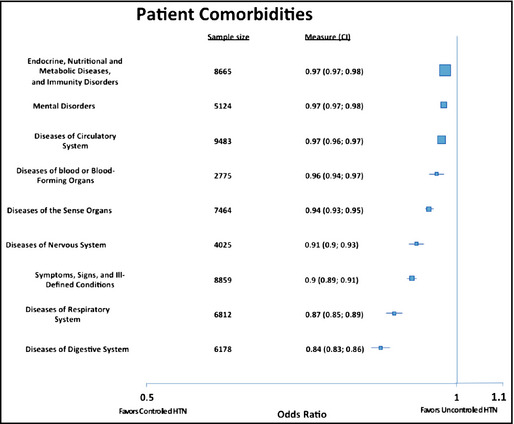
Forest plot of comorbidities. PDC indicates proportion of days covered; OR, odds ratio; CI, confidence interval; CCB, calcium channel blocker; ACEi, angiotensin‐converting enzyme inhibitor; ARB, angiotensin receptor blocker; DHP, dihydropyridine; HTN, hypertension.
A multivariate analysis was conducted. We required the variables to have a statistically significant P value of <.0005 in order to be included in the analysis. This effectively built in the Bonferroni correction for multiple comparisons, as we started with approximately 100 variables in the multivariate model and reduced it to 22 variables upon completion of the analysis.
Discussion
Our research group previously examined factors associated with uncontrolled hypertension in a large, ethnically diverse population within a staff model, integrated healthcare system.13 Factors previously identified to be associated with uncontrolled hypertension included ethnicity (eg, African American), drug classes (ie, DHP CCB, sympatholytics, and vasodilators), partnered status, and higher scores on the PHQ‐9 scale (ie, moderate to severe depression).13 Within the uncontrolled cohort we found a large number of patients with recorded BPs never within goal and yet did not necessarily fit the traditional definition of resistant hypertension (ie, three or more antihypertensives from different classes at optimal doses but with BP not at goal).20 To examine this group further, we limited our cases to those who had all reported BPs (at least 18 consecutive months of data) greater than goal. We then controlled for some of the factors that were associated with uncontrolled hypertension in the first study. Since our original study found a strong association of uncontrolled hypertension with African American ethnicity, we controlled for ethnicity as well as age and sex in the current study in order to explore additional factors that might set this very hard‐to‐control population apart.
Sim and colleagues11 identified and characterized resistant hypertension in an integrated healthcare system, KPSC. That study defined resistant hypertension as individuals having SBP 140 mm Hg or higher or diastolic BP 90 mm Hg or higher while taking three different antihypertensive medications concurrently or taking four or more medications concomitantly regardless of BP. The authors found that black race, older age, male sex, obesity, higher medication adherence rates, CKD, DM, and cardiovascular disease were associated with higher risk of resistant hypertension. The investigators stated that the cross‐sectional design of the study was a potential limitation, as they could not evaluate chronic medication use over a long time. Other studies have shown that two or more antihypertensive medications are usually necessary to control BP.16, 21
Previous studies examined hypertension or resistant hypertension risk factors; however, none investigated a patient population with BPs that were continuously uncontrolled over time. Rather, they explored various definitions of resistant hypertension. For example, resistant hypertension has historically been defined as failure to achieve BP control with the use of three or more antihypertensive medications (some definitions include using a diuretic) or the use of four or more antihypertensive medications irrespective of BP control.7, 17, 18, 20, 22, 23 It is important to note that the current study is not examining the classically defined resistant hypertension, but rather a cohort of patients to determine why they are continuously uncontrolled.
The Table shows demographic variables controlled for age, sex, and ethnicity between the patients and controls. As previously described by Sim and colleagues,11 KPSC developed a clinical practice guideline with a stepwise treatment approach to controlling hypertension with literature‐supported positive patient health outcomes14, 24 (ie, thiazides, ACE inhibitors/ARBs, DHP‐CCBs as first‐line agents, and β‐blockers/spironolactone as later additions to therapy). The findings from this study indicate that our strategy of stepwise escalation in drug therapy was being followed as evidenced by the sample sizes associated with each drug class (with thiazides as first step, ACE inhibitor or ARB second step, DHP‐CCB third and so on). That is, as defined by our guidelines, those who are uncontrolled end up being treated with a thiazide and ACE inhibitor or ARB, DHP‐CCB, and likely a β‐blocker or spironolactone as doses and regimens are escalated and agents are progressively added to achieve control. Use of vasodilators, sympatholytics, α‐β–blockers, and non–DHP CCBs are considered fifth‐line agents and beyond for patients whose hypertension remains uncontrolled. Our data indicate that patients treated with these agents were indeed not controlled despite indications of adherence with their medications. Given that the adherence of our first‐line therapies is fairly high (ie, PDC ≥80%) and that providers are prescribing medications with solid evidence‐based benefits, we believe that our study indicates that factors, other than drug therapy and adherence, are primarily associated with continuously uncontrolled BPs.
As noted by others, patients taking multiple antihypertensives were more likely to have controlled BPs.16, 24 Indeed, Figure 2 shows that patients with a higher number of antihypertensives are more likely to have controlled BP. This was also true for those concomitantly dispensed medications for other chronic illnesses (Figure 5). In fact, Figure 5 demonstrates that the more common comorbidities are associated with greater hypertension control. Not surprisingly, patients with overall greater adherence to antihypertensives were more likely to have controlled BP (Figure 2).
This study reconfirmed the finding from our earlier paper that higher PHQ‐9 score is associated with uncontrolled hypertension. Depression has previously been associated with hypertension25 as well as other conditions.26 Increased BMI (BMI ≥30) is also associated with higher risk of uncontrolled hypertension. A greater number of exercise hours was not significantly different compared with those with controlled hypertension. This may seem surprising, but it is important to note that while this information is recorded at each provider visit, it is unconfirmed patient self‐reporting that may be subject to misrepresentation (recall bias).
There were a number of findings associated with controlled BP that are worth noting. There was a statistically significant yet minor association of greater income and education with controlled BP. Within KPSC's system, patients have access to affordable first‐line antihypertensive agents (which are available as generics). Therefore, we do not believe that the ability to pay would account for better control. Medicare recipients were more likely to have controlled BP. Metrics devised and scored by CMS likely create organizational awareness and resource allocations to assist elderly patients in achieving positive therapeutic outcomes. Furthermore, there is published evidence that elderly patients are more likely to adhere to their medication regimens than younger people.27 However, Medicaid status did not show a statistical difference in BP control. As with our first study, patients who had a significant partner in life were more likely to have controlled BP. Perhaps our most significant finding was the association of controlled BP with a greater frequency of visits to healthcare providers. Moreover, the number of appointment cancelations was associated with BP control (Figure 4).
We analyzed our variables to determine the impact of risk on control of BP. Figure 2 stratifies statistical risk of uncontrolled hypertension based on multivariate analysis. Patients in the highest risk categories were dispensed a prescription for a vasodilator or sympatholytic. However, we believe this to be a function of the stepwise level of care rather than a true risk (ie, these agents are generally reserved for add‐on therapy after the four main classes of drugs have been employed). Adherence to the primary four categories of first‐line therapies was related to better hypertension control (Figure 3). As the number of provider visits increased, so did the rate of controlled hypertension. Taking more medications was related to better control. However, this study was not designed to determine whether the cause was psychosocial or inadequate patient management and may be a subject for future research.
Study Strengths
This study has a number of strengths, including a large patient population that reflected communities within Southern California.28 We derived our data using a prospectively collected electronic medical database including pharmacy prescription data. Kaiser Permanente providers utilize an evidence‐based process for the management of hypertension, which minimizes prescribing variation. Patients do not encounter significant barriers to accessing healthcare providers or medications.
Study Limitations
This study's limitations are those characteristic of retrospective observational designs, eg, inability to control for confounding variables that are unknown or unmeasurable. First, the study was dependent on ICD‐9 codes for the diagnosis of hypertension. However, this risk of bias was limited by requiring patients to have one or more elevated BP readings. Second, we did not define BP goals based on JNC 8 guidelines, as this study was initiated while JNC 7 was the most current guideline available. Lastly, our design is not a predictive risk model, thus it cannot be used to predict which individuals will likely have uncontrolled hypertension. Such a predictive model may be the goal of future research.
Conclusions
Patients with overall greater adherence to antihypertensives were more likely to have controlled BP. However, patients dispensed vasodilators, sympatholytics, α‐β–blockers, and non‐DHP CCBs were more likely to be uncontrolled despite adherence to these medications, indicating that factors other than just adherence are associated with uncontrolled BP. In addition, patients with a higher PHQ‐9 score and higher BMI were associated with uncontrolled hypertension. Patients who were dispensed more antihypertensives or medications for chronic illnesses visit their provider more frequently, have a greater income and education, and have a partnered relationship were more likely to have controlled BP. In this study, sociodemographic and clinical factors were identified for hypertensive patients who are more likely to continuously have BP values that are uncontrolled over a prolonged period. Thus, we can use this information to improve our organization's resources to help improve hypertension rates. We believe that eliminating other causes, such as behavioral traits and attitudes, may play a role in controlling continuously uncontrolled hypertension; however, future prospective studies will be needed to further investigate this theory. This study was not designed to determine whether the cause of uncontrolled BP was caused by psychosocial or inadequate patient management (intentional or nonintentional); this is suggested for future prospective research. Longitudinal hypertension control might be associated with a patient's specific attitude or behavior, which may be important to consider in an integrated healthcare team model when treating hypertension.
Acknowledgment and Disclosures
We gratefully acknowledge Dina Elperin, PharmD, for her valuable support in the study development and Troy Phipps, PhD, PharmD, for his critical review of this manuscript. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
J Clin Hypertens (Greenwich). 2015;17:281–289. DOI: 10.1111/jch.12478. © 2015 Wiley Periodicals, Inc.
References
- 1. CDC . Vital signs: prevalence, treatment, and control of hypertension—United States, 1999–2002 and 2005–2008. MMWR. 2011;60:103–108. [PubMed] [Google Scholar]
- 2. Lloyd‐Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 3. McAlister FA, Robitaille C, Gillespie C, et al. The impact of cardiovascular risk‐factor profiles on blood pressure control rates in adults from Canada and the United States. Can J Cardiol. 2013;29:598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Murphy SL, Xu JQ, Kochanek KD. Deaths: final data for 2010. National Vital Statistics Reports; Vol. 61 No. 4. Hyattsville, MD: National Center for Health Statistics; 2013. [PubMed]
- 5. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension (SHEP). JAMA. 1991;265:3255–3264. [PubMed] [Google Scholar]
- 6. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 7. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 8. Yeh RW, Sidney S, Chandra M, et al. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;364:2155–2165. [DOI] [PubMed] [Google Scholar]
- 9. MacMahon S, Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease, part 1: prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774. [DOI] [PubMed] [Google Scholar]
- 10. American Diabetes Association . Treatment of hypertension in adults with diabetes. Diabetes Care. 2003;26(suppl 1):S80–S82. [DOI] [PubMed] [Google Scholar]
- 11. Sim JJ, Handler J, Jacobsen SJ, Kanter MH. Systemic implementation strategies to improve hypertension: the Kaiser Permanente Southern California experience. Can J Cardiol. 2014;30:544–552. [DOI] [PubMed] [Google Scholar]
- 12. Go AS, Bauman MA, Coleman King SM, et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. J Am Coll Cardiol. 2014;63:1230–1238. [DOI] [PubMed] [Google Scholar]
- 13. Elperin D, Pelter M, Deamer R, et al. A large cohort study evaluating risk factors associated with uncontrolled hypertension. J Clin Hypertens (Greenwich). 2014;16:149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. James PA, Oparil S, Carter BL, et al. Evidence‐based guidelines for the management of high blood pressure in adults. Report from the panel members appointed to the eighth Joint National committee (JNC 8). JAMA. 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 15. HEDIS & Performance Measurement . National Committee for Quality Assurance. HEDIS 2014 Volume 2. www.ncqa.org. Accessed April 2, 2014.
- 16. Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid‐lowering treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4:393–404. [DOI] [PubMed] [Google Scholar]
- 17. Munterner P, Davis BR, Cushman WC, et al. Treatment‐resistant hypertension and the incidence of cardiovascular disease and end‐stage renal disease: results from the antihypertensive and lipid‐lowering treatment to prevent heart attack trial (ALLHAT). Hypertension. 2014;64:1012–1021. [DOI] [PubMed] [Google Scholar]
- 18. Sarafidis P, Bakris G. Resistant hypertension an overview of evaluation and treatment. J Am Coll Cariol. 2008;512:1749–1757. [DOI] [PubMed] [Google Scholar]
- 19. Egan BM, Zhao Y, Axon RN, et al. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124:1046–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Calhoun DA, Jones D, Textor S, et al. Resistant hypertension diagnosis, evaluation, and treatment: a scientific statement from the American heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–e526. [DOI] [PubMed] [Google Scholar]
- 21. Black HR, Elliott WJ, Neaton JD, et al. Baseline characteristics and elderly blood pressure control in the CONVINCE trial. Hypertension. 2001;37:12–18. [DOI] [PubMed] [Google Scholar]
- 22. Sim J, Bhandari S, Shi J, et al. Characteristics of resistant hypertension in a large, ethnically diverse hypertension population of an integrated health system. Mayo Clin Proc. 2013;88:1099–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moser M, Setaro JF. Clinical Practice. Resistant or difficult‐to‐control hypertension. N Engl J Med. 2006;355:385–392. [DOI] [PubMed] [Google Scholar]
- 24. Gradman AH, Basile JN, Carter BL, Bakris GL. American Society of Hypertension Writing Group. Combination therapy in hypertension. J Am Soc Hypertens. 2010;4:42–50. [DOI] [PubMed] [Google Scholar]
- 25. Moise N, Davidson KW, Chaplin W, et al. Depression and clinical inertia in patients with uncontrolled hypertension. JAMA Intern Med. 2014;174:818–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta‐analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107. [DOI] [PubMed] [Google Scholar]
- 27. Butler RJ, Davis TK, Johnson WG, Gardner HH. Effects of nonadherence with prescription drugs among older adults. Am J Manag Care. 2011;17:153–160. [PubMed] [Google Scholar]
- 28. Koebnick C, Langer‐Gould A, Gould M, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16:37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]


