Arterial hypertension,1 obesity,2 the renin‐angiotensin‐aldosterone system (RAAS),3 and uric acid4 are all independently ligated to an increased cardiovascular (CV) risk. Arterial hypertension and obesity are among the 20 leading risk factors that increase the mortality of the general population with hypertension, which is number one.1 In turn, obesity is one of the most common factors responsible for the development of arterial hypertension.5 On the other hand, the RAAS and uric acid have been shown to participate independently in the development and maintenance of arterial hypertension, as well as in the mechanisms leading to the development of hypertension in obesity.4, 6, 7 Furthermore, RAAS as well as uric acid have been shown to be related to an increase in CV morbidity and mortality in hypertension and obesity.8, 9 In fact, uric acid could play a role in the epidemic of obesity‐related metabolic syndrome and cardiorenal disease.10 In this issue of The Journal of Clinical Hypertension, Zhang and colleagues11 expand the knowledge of the participation of the RAAS and uric acid in the pathogenesis of hypertension in obesity. The authors describe that serum uric acid is strongly related to angiotensinogen in an obesity‐dependent manner in untreated hypertensive patients. They also describe that serum uric acid seems to contribute to the enhancement of plasma angiotensinogen and could be involved in the pathophysiology of obesity‐related hypertension where an increase in activity of RAAS is one of the mechanisms underlying the development and maintenance of arterial hypertension.5
The pathophysiological scene of hypertension in obesity is a vicious circle in which specific mechanisms can contribute at the same time to trigger others, leading to the progressive deterioration of the cardiorenal system. This crosstalk between hypertension and obesity is represented in the Figure1 where it is shown how these mechanisms are interconnected. In this context, hyperuricemia is strongly related to arterial hypertension.4, 12 At the same time, increased sympathetic activity and increased RAAS are also mechanisms underlying hypertension and obesity, where the results of Zhang and colleagues11 also point to angiotensinogen as an important player in the pathogenesis of obesity hypertension. The high level of circulating angiotensinogen observed in untreated hypertensive obese patients is also likely favored by the increase in fat mass observed in these patients. At the same time, high serum uric acid levels are a signature of the metabolic syndrome that also reflects a disturbed underlying renal hemodynamic effect. That is because the hyperinsulinemia and insulin resistance that accompanies obesity can induce the specific activation of the tubular sodium‐hydrogen exchanger facilitating the active reabsorption of uric acid and decreasing its renal clearance.13 Therefore, as the Figure1 shows, we know the players associated with obesity‐related hypertension (as uric acid, angiotensinogen, RAAS, insulin, endothelial dysfunction, among others) and also the relationship of these factors with each other (eg, insulin resistance favors hyperuricemia and this, in turn, enhances RAAS activity). However, it is still not completely clear whether factors such as uric acid are the cause or the consequence of the cardiorenal deterioration observed in hypertension associated with obesity. Several clinical evidences have pointed out that uric acid could be an important causal factor in the onset of essential hypertension and obesity. In this sense, the observations of the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) study,14 in which losartan‐treated hypertensive patients showed reduced uric acid levels associated with reduced cardiovascular morbidity and mortality, or more recent trials in which treatment with allopurinol demonstrated decreased blood pressure in obese adolescents15 and also delayed progression of renal disease,16 show that drugs with uricosuric capacity may be considered as new therapeutic strategies in medical practice to treat obesity‐related hypertension. However, larger and conclusive clinical trials are still needed to establish the specific clinical benefits of lowering uric acid in the setting of hypertension in obesity.
Figure 1.
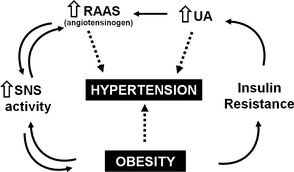
Common pathogenesis pathways related to hypertension and obesity. UA indicates uric acid; RAAS, renin‐angiotensin‐aldosterone system; SNS, sympathetic nervous system.
References
- 1. Ezzati M, Lopez AD, Rodgers A, et al. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–1360. [DOI] [PubMed] [Google Scholar]
- 2. Murphy NF, MacIntyre K, Stewart S, et al. Long‐term cardiovascular consequences of obesity: 20‐year follow‐up of more than 15 000 middle‐aged men and women (the Renfrew‐Paisley study). Eur Heart J. 2006;27:96–106. [DOI] [PubMed] [Google Scholar]
- 3. Ma TK, Kam KK, Yan BP, Lam YY. Renin‐angiotensin‐aldosterone system blockade for cardiovascular diseases: current status. Br J Pharmacol. 2010;160:1273–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ruilope LM. Blood pressure and uric acid in diabetes mellitus. J Clin Hypertens (Greenwich). 2014;16:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Schlaich MP, Grassi G, Lambert GW, et al. European Society of Hypertension working group on obesity obesity‐induced hypertension and target organ damage: current knowledge and future directions. J Hypertens. 2009;27:207–211. [DOI] [PubMed] [Google Scholar]
- 6. Vasan RS, Evans JC, Larson MG, et al. Serum aldosterone and the incidence of hypertension in nonhypertensive persons. N Engl J Med. 2004;351:33–41. [DOI] [PubMed] [Google Scholar]
- 7. Feig DI, Kang DH, Johnson RJ. Uric acid and cardiovascular risk. N Engl J Med. 2008;359:1811–1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alderman MH, Madhavan S, Ooi WL, et al. Association of the renin‐sodium profile with the risk of myocardial infarction in patients with hypertension. N Engl J Med. 1991;324:1098–1104. [DOI] [PubMed] [Google Scholar]
- 9. Ruilope LM, Pontremoli R. Serum uric acid and cardio‐renal diseases. Curr Med Res Opin. 2013;29(Suppl 3):25–31. [DOI] [PubMed] [Google Scholar]
- 10. Johnson RJ, Lanaspa MA, Gaucher EA. Uric acid: a danger signal from the RNA world that may have a role in the epidemic of obesity, metabolic syndrome, and cardiorenal disease: evolutionary considerations. Semin Nephrol. 2011;31:394–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang JZY, Deng W, Chen B. Elevated serum uric acid is associated with angiotensinogen in obese patients with untreated hypertension. J Clin Hypertens (Greenwich). 2014;■■■■:■■■■–■■■■. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Johnson RJ, Feig DI, Herrera‐Acosta J, Kang DH. Resurrection of uric acid as a causal risk factor in essential hypertension. Hypertension. 2005;45:18–20. [DOI] [PubMed] [Google Scholar]
- 13. Puig JG, Ruilope LM. Uric acid as a cardiovascular risk factor in arterial hypertension. J Hypertens. 1999;17:869–872. [DOI] [PubMed] [Google Scholar]
- 14. Høieggen A, Alderman MH, Kjeldsen SE, et al. The impact of serum uric acid on cardiovascular outcomes in the LIFE study. Kidney Int. 2004;65:1041–1049. [DOI] [PubMed] [Google Scholar]
- 15. Soletsky B, Feig DI. Uric acid reduction rectifies prehypertension in obese adolescents. Hypertension. 2012;60:1148–1156. [DOI] [PubMed] [Google Scholar]
- 16. Goicoechea M, de Vinuesa SG, Verdalles U, et al. Effect of allopurinol in chronic kidney disease progression and cardiovascular risk. Clin J Am Soc Nephrol. 2010;5:1388–1393. [DOI] [PMC free article] [PubMed] [Google Scholar]


