Abstract
The objective of this periodic review was to identify, summarize, and appraise studies relating to the implementation of salt reduction strategies that were retrieved between November 2015 and February 2016. From the established MEDLINE search, 56 studies were identified as relevant to the implementation of salt reduction initiatives. Detailed appraisal was performed on seven studies that evaluated the impact of salt reduction interventions. While study quality varied, all had one or more risks related to bias. There was consistent evidence, from three studies, demonstrating that setting‐based structural interventions to improve the nutritional composition of foods were effective in reducing salt but mixed evidence in relation to the effectiveness of behavioral interventions. The development of an evaluation guidance framework that supports scientific rigor and external validity would aid future design and interpretation of studies evaluating salt reduction interventions, particularly for low‐resource countries.
There is a growing body of evidence on the adverse effects of excess salt consumption on health outcomes, namely raised blood pressure (BP), stroke, and coronary heart disease.1, 2 The World Health Organization (WHO) Action Plan for the Prevention and Control of Non‐Communicable Diseases (NCDs) calls on member states to take action to reduce population salt intake by 30% by 2025.3 Globally, countries are now translating this evidence into policies and strategies to reduce population‐wide salt intake.4
A number of systematic reviews have recently been published to collate information on the strategies implemented at national4, 5 and subnational6 levels to reduce population salt intake. These studies all identify the need to understand what works and why. To keep policy stakeholders up to date with the growing body of literature about effective program implementation, regularly updated critical appraisals of studies relating to the implementation of strategies are published in the Journal every few months.7 The objective of the current review is to critically appraise the literature on the effectiveness of salt reduction programs identified from November 2015 to February 2016.
Methodology
A detailed description of the method used to identify and screen studies for eligibility has been previously published.8 Articles were identified on a weekly basis through an established MEDLINE search. Studies relating to the implementation of salt reduction strategies in the real‐world setting retrieved from November 1, 2015, to February 2016 were screened and assessed for eligibility by two independent authors based on a revised inclusion and exclusion criteria (online Supplementary File 1).
The studies are considered in four broad categories: (1) studies evaluating the impact of salt reduction interventions with a population‐wide focus; (2) studies on monitoring and surveillance of salt intake, salt levels in foods, and consumers' knowledge, attitudes, and behavior; (3) economic evaluation or modeling studies of salt reduction strategies; and (4) other studies related to the implementation of salt reduction initiatives. Detailed appraisal of the risk of bias and commentary were performed just for the group of studies evaluating the impact of salt reduction interventions. Two independent authors assessed the risk of bias using the Cochrane risk of bias tool for randomized controlled trials (RCTs) and a modified version of the tool for non‐randomized trials (non‐RTs) of intervention studies.5, 9
Results
The MEDLINE search identified 1281 potentially relevant studies, of which 86 full‐text articles were assessed against the eligibility criteria after studies were screened based on abstracts (Figure 1). A total of 56 studies were considered relevant to the implementation of population‐wide salt reduction interventions. Seven studies were on evaluation of salt reduction interventions,10, 11, 12, 13, 14, 15, 16 22 on monitoring and surveillance, 10 on modeling, and 17 related to other aspects of implementation of salt reduction interventions. This review focused on the seven studies that evaluated the impact of interventions or policies to reduce salt intake (Table 1).
Figure 1.
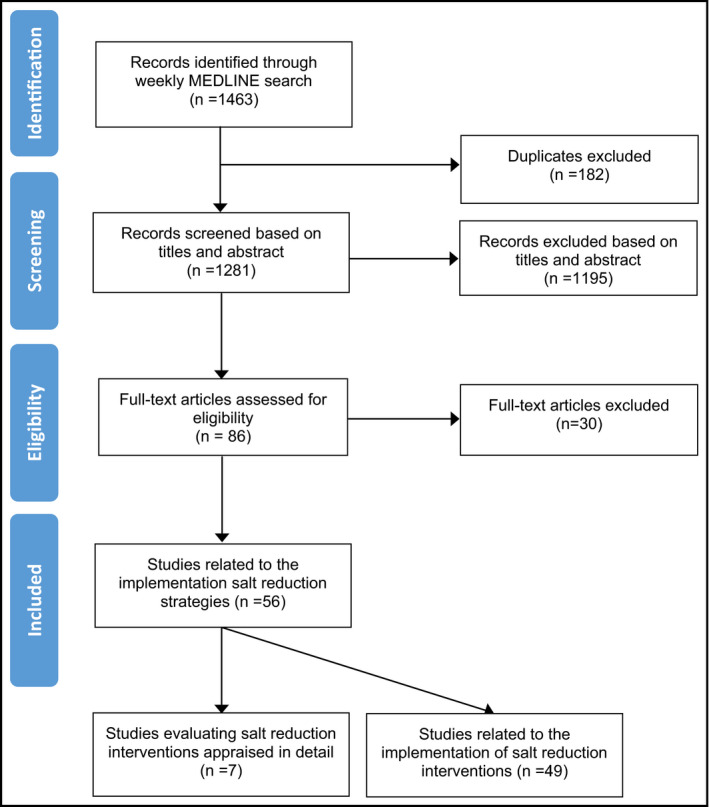
Studies included between November 2015 and February 2016 review.
Table 1.
Characteristics of the Included Intervention Studies
| Author, Year, Country | Study Design | Setting | Population | Intervention | Outcome Measure | Result |
|---|---|---|---|---|---|---|
| Structural salt reduction interventions that aim to improve the environment or settings | ||||||
| Moran et al (2015),10 United States | Pre‐ and post‐intervention | United States, between 2010 and 2014 | Eight private New York City hospitals selected based on voluntary participation | New York City's Healthy Hospital Food Initiative (HHFI)–nutrient based standards for regular patient meals that are voluntary for private hospitals | Nutritional composition of hospital meals on the menu | Pre‐implementation, 6 of 8 hospitals exceeded the daily limits of sodium and none met all of the HHFI nutrition standardsPost‐implementation, all 8 hospitals met all key nutrient standards including decreasing sodium by 19% |
| Merlo et al (2015),11 United States | Repeat cross‐sectional study | United States, 2000–2014 | US Federal schools | New nutrition standards in 2012 for schools requiring gradual reduction in salt content over 10 years | Salt‐lowering practices in schools | Between 2006 and 2014, there was an increase in the use of low‐sodium canned vegetables (15.6% to 51.8%), other seasonings instead of salt (39.2% to 65.1%), and low‐sodium recipes (45.8% to 68.0%) among the 55% of schools that prepared food on school premises |
| Janssen et al (2015),12 Netherlands | Randomized controlled trial (RCT) | Restaurant of the Future in Wageningen, 2011 | 81 students and employees of Wageningen University aged between 18 and 35 years, with body mass index between 18.5 and 25 | Provision of reduced‐salt lunches in an experimental real‐life canteen in Wageningen to uninformed intervention participants | 24‐hour urinary sodium excretion, acceptability of foods, and sensory attributes | Greater reduction in sodium excretion by 900 mg/d in the intervention group compared with the control group from baseline to week 5The liking of foods did not differ for 17 of 19 foods in the intervention and control group |
| Behavioral interventions to reduce population salt intake | ||||||
| Rubinstein et al (2015),13 Latin American countries | Parallel‐group RCT | Low‐resource urban settings in Argentina, Guatemala, and Peru | 637 participants, aged 30–60 years with prehypertension | Monthly motivational counseling calls and weekly personalized texts about diet quality and physical activity for 12 months |
Self‐reported sodium intake measured by a food frequency questionnaire (FFQ) Systolic blood pressure (SBP) and diastolic blood pressure (DBP) |
No difference in changes in salt intake of high‐sodium foods, SBP, and DBP between the intervention and control group |
| Anderson et al (2015),14 United States | RCT | Baltimore, Maryland, 2012–2014 | 40 participants, aged ≥18 years with hypertension, prehypertension, or diabetes | Multifactorial behavioral intervention emphasizing spices and herbs instead of salt to maintain lower sodium intake through group sessions, individual counseling, and contact by phone, text, or e‐mail | 24‐hour urinary sodium excretion | After 20 weeks of intervention, participants had lower urinary sodium excretion than controls by −957 mg/d (P=.002) |
| Brown et al (2015),15 United States | Cluster RCT | Texas | 760 participants, aged ≥18 years | Multicomponent, cultural, faith‐based behavior intervention to reduce stroke risk factors, which included self‐help materials, motivational calls, a newsletter, and a 2‐hour workshop on counseling for 12 months | Sodium intake measured by Block FFQ | Significantly greater reduction in salt intake in the intervention group compared with the control group, from baseline to follow‐up by −123.17 mg/d (P=.04) |
| Robson et al (2016),16 United States | Pilot observational study—pre‐post design | Midwest United States, 2014 | 6 adult‐child dyads recruited from employees at a children's medical center | Ten weekly cooking instruction sessions with a focus on nutrition, meal preparation, and behavior modification | Sodium intake based on 7‐day dietary record for adults and child | No statistically significant change in average intake of sodium at dinner after the intervention |
A summary of the other 49 studies is outlined in Table 2 and study references can be found in the online Supplementary File 2. Three quarters of these studies are conducted in high‐income countries and a quarter of studies are in low‐ or middle‐income countries (LMICs). Of the 22 surveillance studies, 12 monitored population salt consumption, nine measured salt content in foods, and one measured the healthcare providers' knowledge and attitudes relating to salt. Of the 10 modeling studies, most simulated the impact of population salt reduction on NCD mortality. The remaining 17 studies are varied, including studies examining the validity of different tools to measure salt intake, nutrition labeling studies, and the acceptability of low‐sodium foods.
Table 2.
Other Studies Related to the Implementation of Salt Reduction
| Types of Studies | Description | Number of Studies | Summary |
|---|---|---|---|
| Monitoring or surveillance studies | Population salt intake | 12 |
Country of study: 3 United States (US), 2 Australia, 2 China, 1 New Zealand, 1 Canada, 1 Brazil, 1 Bangladesh, 1 sub‐Saharan Africa Method of salt intake assessment: 4 through 24‐hour urine collection; 4 through 24‐hour food recall including the three US studies, which all utilized data from the National Health and Nutrition Examination Survey (NHANES); 1 total diet studies through weighing food intake and laboratory analysis of prepared foods; 1 assessed data on extra salt use through a structured questionnaire; 1 systematic review of studies reporting sodium intake; and 1 compared two methods in estimating sodium intake—a semiquantitative food frequency questionnaire vs a 12‐hour urinary excretion measurement Type of study population: 7 included an adult population, 2 included a child population, and 3 included both child and adult populations Study design: All of the studies were cross‐sectional in nature Study results: All studies that measured salt intake (9) showed that countries had an average daily salt intake above the World Health Organization–recommended amount of 5 g/d |
| Salt content in foods and meals | 9 |
Country of study: 2 in the US, 2 in Sweden, 2 in Australia, 1 in Austria, 1 in Germany, and 1 in both New Zealand and Australia Objective of measuring salt levels in foods: 3 measured compliance with nutrition standards; 3 obtained nutrient profile to support product labeling or consumer education or assess future changes; 2 compared nutrient content with counterparts; and 1 estimated the improvements from a supermarket's initiative Types of foods assessed: 5 included packaged foods with 1 focusing on baby and toddler food products and 1 on gluten‐free foods; 2 included meals with 1 focusing on school meals and 1 on recipes for home cooking from a food magazine; and 2 were mixed, which included commercially processed, restaurant, and homemade foods |
|
| Consumers' knowledge, attitudes, and behaviors related to salt | 1 | Country of study: 1 US cross‐sectional survey of healthcare providers to measure their knowledge, attitudes, perceptions, and beliefs regarding dietary recommendations | |
| Economic evaluations or modeling studies | Modeling the effects of salt reduction | 10 |
Country of study: 2 US, 1 global, 1 Australia, 1 Netherlands, 1 Germany, 1 Turkey, 1 South Africa, 1 China, 1 European countries Objective of modeling: 6 simulated the impact of salt reduction on noncommunicable disease mortality, 2 simulated the impact of salt reduction on sodium intake, 1 estimated the economic impact of salt reduction particularly healthcare cost savings, and 1 estimated both the health and economic impact of salt reduction |
| Other | Other studies related to salt reduction interventions | 17 |
Country of study: 4 US, 2 Korea, 2 Canada, 1 Guatemala, 1 Germany, 1 United Kingdom, 1 India, 1 Malaysia, 1 Belgium, 1 Switzerland, 1 China, 1 Brazil Type of study: 6 studies on validity of tools or dietary assessment methods for measuring salt intake; 5 labeling studies that include salt; 4 studies on acceptability of low‐sodium foods; and 2 reviews of interventions that include reducing salt intake |
The seven studies that evaluated the impact of salt reduction interventions are appraised in detail below and risk of bias assessments are included in Supplementary File S1. Five of the seven studies were undertaken in the United States, one was conducted in the Netherlands, and one in three Latin American countries (Argentina, Guatemala, and Peru). Four studies are RCTs (including one cluster RCT), two are pre‐ and post‐studies, and one is a repeated cross‐sectional study. Five studies evaluated the impact of interventions based on estimated salt intake in adults (one with adult and child dyads), one measured the nutritional composition of hospital meals, and one measured the prevalence of private schools undertaking salt‐lowering practices.
All seven studies scored high risk in one or more domains according to the modified risk of bias tool for intervention studies (Figure 2). All except one study scored high risk of performance bias, namely, not blinding study personnel or participants from knowledge of intervention assignment in RCTs or not controlling for potential confounding variables in non‐RCTs, meaning that exposure of other factors apart from the intervention may have affected the outcome. Just under half (three) of the studies had risk of bias related to poor outcome measurement and selection bias.
Figure 2.
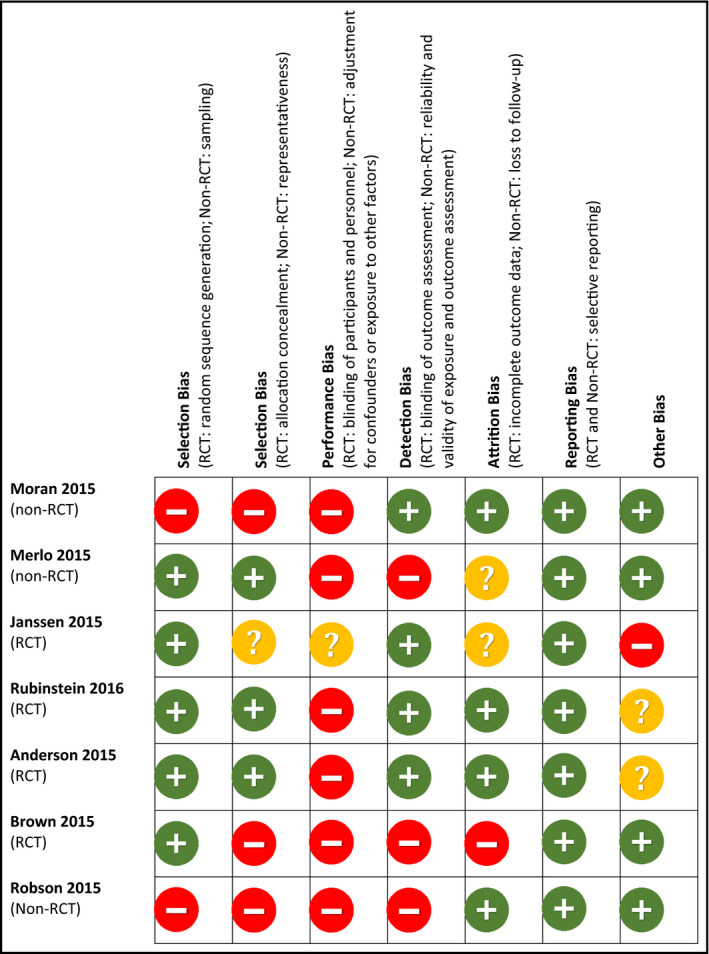
Risk of bias assessment summary adapted from Cochrane.
As described below, five of seven studies found that there was a positive salt‐related outcome as a result of either nutrition standards in hospitals10 and schools,11 lower sodium foods provided in a University canteen,12 or behavioral interventions.14, 15 The two studies that found a non‐significant change in salt intake were both broader behavioral interventions: one mobile phone–based intervention that aimed to improve the cardiometabolic profile in 553 pre‐hypertensive participants13 and the other included the provision of cooking lessons to improve the overall diet quality of parents and their children.16
Structural Salt Reduction Interventions Aiming to Improve the Environment or Settings
Moran A, Lederer A, Curtis CJ. Use of nutrition standards to improve nutritional quality of hospital patient meals: findings from New York City's Healthy Hospital Food Initiative. J Acad Nutr Diet. 2015;115:1847–1854.
Objective: To examine the regular‐diet patient menus before and after the implementation of New York City's Healthy Hospital Food Initiative (HHFI) nutrition standards.
Design: Pre‐ and post‐intervention.
Setting: Eight private New York City hospitals, participating in the HHFI between 2010 and 2014.
Intervention: The HHFI, which aims to improve the nutritional quality of hospital regular‐diet patient meals, introduced standards for the amount of sodium (mg) in hospital meals as part of broader nutrient‐based standards.
Outcomes: Nutritional composition of regular‐diet hospital meals based on hospital menus compared with HHFI standards.
Summary of results: No regular‐diet menu met all HHFI standards prior to participation in the initiative and most (6 of 8) exceeded the daily limits of sodium. Post‐implementation, all hospitals met all key nutrient standards including decreasing the median sodium from 2636 mg/d to 2149 mg/d (−19%, P<.05). There was also a significant increase in fresh fruit servings (667%, P<.05) and a decrease in full‐fat and reduced‐fat milk servings (−100%, P<.05).
Sources of funding: The HHFI was supported by the Community Transformation Grant and Sodium Reduction in Communities grant from the Centers for Disease Control and Prevention.
Comments: This analysis showed that participation in the HHFI, which provides standards for the nutritional composition of hospital meals, successfully reduced the sodium content of meals by 19% and improved a range of other nutritional indicators. This was based on an assessment of the new meals on the menu, and sodium or nutrient content was obtained from the products' Nutrition Facts label, from vendors when available, or the US food composition database. Patient food consumption was not measured. The extent of nutritional improvements found may be attenuated by patient acceptability of the new meals, consumption of additional snacks, and the availability of outside foods purchased by visitors. The study was based only on a sample of non‐government hospitals participating in the HHFI program, so the reach and effect of the voluntary program among all private hospitals is unknown. Overall, the study demonstrates that when hospitals are willing to work collaboratively with governments to improve hospital meals, an established framework of nutrient‐based standards can help significantly improve the nutritional content of meals.
Merlo C, Brener N, Kann L, et al. School‐level practices to increase availability of fruits, vegetables, and whole grains, and reduce sodium in school meals—United States, 2000, 2006, and 2014. MMWR Morb Mortal Wkly Rep. 2015;64: 905–908.
Objective: To examine the prevalence of practices adopted by schools to achieve the US Department of Agriculture school nutrition standards.
Design: Secondary analysis of repeat cross‐sectional surveys (School Health Policies and Practice Survey).
Participants/Settings: US federal schools between 2000 and 2014.
Intervention: Introduction of new standards in 2012, which require schools to gradually reduce sodium content in foods and serve more fruits, vegetables, and whole grains over 10 years.
Outcomes: Prevalence of school nutrition practices related to reducing salt intake and increasing the consumption of fruits, vegetables and whole grains.
Summary of results: The percentage of schools implementing the nutrition practices increased from 2000 to 2014. Between 2006 and 2014, among the 55% of schools that prepared food on school premises, the use of low‐sodium canned vegetables instead of regular canned vegetables increased from 15.6% to 51.8%, use of other seasonings instead of salt increased from 39.2% to 65.1%, and use of low‐sodium recipes increased from 45.8% to 68.0%. In addition, there were improvements in prevalence of schools offering two or more servings of fruits and vegetables.
Sources of funding: None reported.
Comments: This analysis of a repeated survey demonstrates that around half of the schools surveyed which prepare food on the premises are reporting to be taking action to reduce sodium in meals. While encouraging, the findings should be interpreted with caution. The findings were based on self‐reported information on nutrition practices and the catering staff would likely be inclined to report they are following the government guidelines. There may also be risk of bias associated with poor response rates. There were no comparisons between characteristics of participating schools and schools that did not participate in the survey. It would be useful to validate the study with chemical analysis of a subsample of the school meals from the nationally representative sample to ensure that the nutritional standards were being applied.
Janssen A, Kremer S, van Stipriaan W, et al. Reduced‐sodium lunches are well‐accepted by uninformed consumers over a 3‐week period and result in decreased daily dietary sodium intakes: a randomized controlled trial. J Acad Nutr Diet. 2015;115:1614–1625.
Objective: To assess whether consumers who are uninformed about the nature of the intervention accept commercially prepared reduced‐sodium lunches, and to measure the effect of reduced‐sodium lunches on estimated dietary sodium intake.
Design: RCT.
Setting: Wageningen, the Netherlands 2011.
Participants: A total of 81 students and employees of Wageningen University aged between 18 and 35 years who had a body mass index (BMI) between 18.5 and 25, were recruited through flyers, posters, and word of mouth.
Intervention: During a 2‐week run in period, all participants consumed regular lunches from an experimental buffet‐style “real‐life canteen” at the Restaurant of the Future in Wageningen University on weekdays and baseline assessments were undertaken. Following randomization, control participants continued to choose from regular buffet items, while intervention participants unknowingly chose from foods that were reduced in sodium by 29% to 61% for lunch for the remaining 3 weeks.
Outcomes: Twenty‐four–hour urinary sodium excretion and the liking and sensory attributes of foods were measured in week 2 and week 5. Food consumption (accounting for foods chosen, portion size, and amount consumed) at lunch was assessed in week 2 and week 4.
Summary of results: Mean energy intake per lunch did not differ significantly between the two groups, yet mean sodium intake per lunch was significantly lower in the intervention group (mean difference −1093 mg) compared with the control group. The reported liking was significantly different between the two groups for only 2 of 19 food items assessed during the intervention period. Mean 24‐hour urinary sodium excretion decreased in both groups from baseline (week 2) to outcome measurement at week 5; however, the reduction was greater in the intervention group. The 24‐hour urinary sodium excretion in the intervention group was significantly lower than the control group by approximately 900 mg/d after the reduced‐sodium lunches.
Source of funding: Dutch Ministry of Economic Affairs.
Comments: This RCT demonstrates that reduced‐sodium lunches were generally acceptable to uninformed consumers who chose lunch from a free buffet at a University restaurant and could significantly lower daily sodium intake. The authors attempted to blind participants to the nature of the study intervention in order to reduce bias; however, many participants were able to correctly identify the main aim of the study by the end of the intervention period. The sample population of University staff and students is likely to be more educated than a general population, which limits generalizability of the findings.
Behavioral Salt Reduction Interventions
Rubinstein A, Miranda J, Beratarrechea A, et al. Effectiveness of an mHealth intervention to improve the cardiometabolic profile of people with prehypertension in low‐resource urban settings in Latin America: a randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4:52–63.
Objective: To assess the impact of a mobile phone–based health (mHealth) tool on improving diet quality and reducing BP.
Design: Parallel‐group RCT trial.
Participants/Settings: Individuals (aged 30–60 years) with prehypertension (systolic BP between 120 and 139 mm Hg, diastolic BP between 80 and 89 mm Hg or both) from centers in low‐resource urban settings in Argentina, Guatemala, and Peru.
Intervention: Twelve‐month intervention consisting of monthly motivational counseling calls and weekly personalized text messages about diet quality and physical activity. The control group received a leaflet about adopting healthy lifestyles.
Outcomes: Mean between‐group differences in the changes in systolic and diastolic BP and the changes in self‐reported dietary sodium intake as measured by a validated food frequency questionnaire (FFQ) from baseline to 12 months.
Summary of results: There was no change in systolic BP (mean net change −0.37 mm Hg, 95% confidence interval [CI], −2.15 to 1.40; P=.43) or diastolic BP (0.01 mm Hg, 95% CI, −1.29 to 1.32; P=.99) in participants in the intervention group compared with the usual care group. Nor was there any reported difference in change in the intake of high‐sodium foods between groups in the primary analysis. A pre‐specified subgroup analysis found a decrease in diets high in sodium, fat, and simple sugars, as well as an increase in the intake of fruits and vegetables with increasing levels of intervention dose (<50% vs >75% of calls received).
Sources of funding: National Heart, Lung, and Blood Institute (US National Institutes of Health) and the Medtronic Foundation.
Comments: This RCT demonstrated that the mHealth intervention aiming to improve several stroke risk factors had no effect on salt intake or BP. This may be the result of the small intervention dose, as counseling about sodium was less common (20%) than other messages. Pre‐specified subgroup analyses showed some impact on consumption of high‐sodium foods related to higher intervention dose. However, this should be interpreted with caution as consumption of high‐sodium foods was measured through FFQ and therefore subject to self‐reporter bias, particularly among intervention participants who received education about lowering salt intake.
Anderson CA, Cobb LK, Miller ER, et al. Effects of a behavioral intervention that emphasizes spices and herbs on adherence to recommended sodium intake: results of the SPICE randomized clinical trial. Am J Clin Nutr. 2015;102:671–679.
Objective: To examine whether a behavioral intervention focusing on the use of spices and herbs as alternatives to salt can help individuals with hypertension, prehypertension, or diabetes maintain the recommended sodium intake of 1500 mg/d.
Design: RCT.
Setting and study duration: Baltimore, Maryland, from 2012 to 2014.
Participants: Forty participants older than 18 years (mean age 61 years, 65% women) with hypertension, prehypertension, or diabetes recruited through advertisements.
Intervention: All participants were provided an isocaloric and low‐sodium diet for a month. Intervention participants (n=20) then received a behavioral intervention to reduce salt intake consisting of one‐on‐one counseling, group sessions, and contact by phone or e‐mail for 20 weeks. Control participants were asked to continue eating a low‐sodium diet by following the advice of standard education materials.
Outcomes: Change in mean 24‐hour urinary sodium excretion between week 4 (assignment to groups) and the final study visit (week 24), measured by two complete 24‐hour urine samples.
Summary of results: After the controlled‐consumption phase, mean 24‐hour urinary sodium decreased from 3496 mg/d to 1654 mg/d among all participants. After 20 weeks of intervention, participants had lower urinary sodium excretion than the control group by −957 mg/d (95% CI, −1538.7 to −374.9 mg/d) (P=.002). Post‐intervention, 25% of participants in the intervention group consumed the recommended amount of 1500 mg/d per 2000 kcal compared with 5% of participants in the control group.
Source of funding: The McCormick Science Institute and in part a grant from the National Heart, Lung, and Blood Institute.
Comments: This RCT found that after 20 weeks of a multifactorial behavioral intervention, emphasizing the use of spices and herbs for the maintenance of a low‐sodium diet achieved a net difference in sodium intake of −957 mg/d between the intervention and control groups. This was accurately assessed using two 24‐hour urine collections for which completeness was measured by excluding collections with urine volume <500 mL. It should be noted that prior to randomization of participants to the intervention or control groups, 15 of 55 participants dropped out during phase 1 where participants were required to eat an isocaloric and low‐sodium diet, which may affect the generalizability of the results.
Brown DL, Conley KM, Sanchez BN, et al. A multicomponent behavioral intervention to reduce stroke risk factor behaviors: the Stroke Health and Risk Education cluster‐randomized controlled trial. Stroke. 2015;46:2861–2867.
Objective: To assess the effectiveness of a culturally sensitive, church‐based, multicomponent behavioral intervention to reduce stroke risk factor behaviors including salt intake.
Design: Cluster RCT.
Setting: The Stroke Health and Risk Education Project (SHARE) was undertaken in the Diocese of Corpus Christi, Texas.
Participants: A total of 760 participants (64% women) older than 18 years (median age, 53 years) who were Hispanic or Latino or non‐Hispanic white parishioners of a participating parish.
Intervention: One‐year culturally sensitive multicomponent behavioral intervention aiming to reduce stroke risk factors through providing materials, newsletters, and motivational calls. The control patients received skin cancer awareness materials and sunblock.
Outcomes: Sodium consumption measured by the Block 2005 FFQ validated in Hispanic or Latino and non‐Hispanic white populations.
Summary of results: The study found that the group which received the multicomponent behavior intervention had a greater reduction in sodium intake of 278 mg/d compared with 155 mg/d in the control group, resulting in a net difference of 123 mg/d (95% CI, −195 to −52; P=.04). However, there was no difference in treatment effect for systolic and diastolic BP.
Sources of funding: This project was supported by the National Institutes of Health and the research was partly supported by the National Center for Advancing Translational Sciences.
Comments: This cluster RCT found that, compared with control, a culturally appropriate, church‐based, multicomponent behavioral intervention resulted in a small reduction in sodium intake. These results should be interpreted with caution as the assessment of sodium intake through a validated FFQ is subject to self‐reporter bias. In addition, there was no blinding of personnel, participants, and outcome assessors. It should also be noted that only 60% of participants completed the 6‐month assessment and 82% completed the 12‐month assessment and noncompleters were younger. When adjusted for age, sex, ethnicity, and social desirability, there was a non‐significant change in sodium intake (P=.12).
Robson SM, Stough CO, Stark LJ. The impact of a pilot cooking intervention for parent‐child dyads on the consumption of foods prepared away from home. Appetite. 2016;99:177–184.
Objective: To pilot the feasibility and effectiveness of a parent‐child dyad cooking intervention and determine its effect on the number of dinners consumed away from home, confidence and attitudes about cooking, and nutrient intake.
Design: Pre‐post design pilot observational study.
Setting: Midwest United States, 2014.
Participants: Six parent‐child dyads were recruited from employees at a children's medical center. Participants were overweight primary caregivers (BMI ≥25 kg/m2) with a child aged between 3 and 10 years who ate convenience foods away from home three or more times per week.
Intervention: Participants undertook 10 weekly cooking instruction sessions with emphasis on nutrition, meal preparation (including recipes), and behavior modification. Children accompanied parents in the final four cooking sessions.
Outcomes: Parents completed a 7‐day dietary record for themselves and their child for dinner time meals at baseline and at the end of the 10‐week intervention. This included identification of meal type (eg, fast food or home prepared), specific foods, and amount consumed. Parents also reported their confidence with meal preparation for an evening meal, as well as their ease of providing home‐prepared evening meals using a visual analog scale.
Summary of results: The proportion of home‐prepared dinners increased from baseline (44%) to post‐intervention (75%). There was a non‐significant decrease in average intake of sodium at dinner over the period (−89.9 mg). Similarly, there was a nonsignificant change in energy, fat, and saturated fat intake but there was a significant reduction in cholesterol intake at dinner. Parents reported greater confidence in preparing home‐cooked meals, ease of cooking home‐prepared meals, enjoyment of cooking, and desire to cook.
Sources of funding: National Institute of Diabetes and Digestive and Kidney Diseases and the National Center for Advancing Translational Sciences of the National Institutes of Health.
Comments: This small pilot study demonstrated that a 10‐week cooking intervention could increase self‐reported number of meals or dinners prepared at home (instead of fast or restaurant food prepared outside the home) for parent‐child dyads. The small sample size, use of a convenience sample, lack of a control group, and use of subjective outcome measures are all potential sources of bias. However, the authors clearly state that the purpose of the study is to pilot the intervention, and acknowledge its limitations.
Discussion
This periodic review (from November 2015 to February 2016) identified 56 studies that can inform the future implementation of salt reduction strategies. While all of these studies are listed in Table 2, this paper focused on the seven studies that evaluated interventions. Five of seven studies found that the salt reduction intervention was effective. While the studies were of varying quality, the overview provides examples of successful structural strategies that aim to improve the environment or setting, such as introducing voluntary nutrition standards to improve the healthiness of hospital and school foods and the provision of reduced‐sodium lunches at canteens, which lowered daily salt intake. The review also included two behavioral interventions that were effective in reducing salt intake and two that demonstrated no significant change. Based on a comparison of the intervention characteristics, behavioral interventions that had several types of delivery modes were more likely to be effective.
Although all three structural interventions demonstrated a positive impact, it is important to interpret the study findings within the context of potential risks of bias. The two studies evaluating the impact of real‐world nutrition standards for foods sold in institutional settings demonstrate a trade‐off between validity of the outcome measurement and generalizability of the study findings. While the study by Merlo and colleagues11 was nationally representative of schools, the study outcome relied on schools themselves reporting whether they had adopted salt‐lowering practices, which is subject to a high risk of self‐reporter bias. Moran and colleagues10 used a more objective measurement and derived the sodium content of meals based on foods on hospital menus; however, it was limited to eight hospitals that were participating in the Healthy Hospital Food Initiative, so the impact of the program on all other hospitals is unknown. The more scientifically robust RCT by Janssen and colleagues12 complements the two studies by demonstrating in an experimental University canteen that reduced‐sodium lunches are well‐accepted by uninformed consumers and did not cause compensatory sodium consumption in other meals of the day, resulting in a significant reduction in 24‐hour urinary sodium excretion. Together, these studies provide encouraging evidence to support settings‐based approaches such as nutrition standards for foods procured, which were implemented in 42 (19 voluntary, 23 mandatory) countries nationwide and more led by state and local government jurisdictions in 2014.4
There is mixed evidence for the effectiveness of behavior change interventions to reduce estimated salt intake, with two demonstrating a positive effect and two demonstrating no effect on estimated daily salt intake. Both groups of effective and ineffective studies have one good‐quality (1 high risk of bias domain) and one poor‐quality (4 domains rated as high risk of bias) study. A comparison of the four indicates that the effective behavioral interventions emphasized their multicomponent nature allowing the salt reduction message to be reinforced through several mediums and potentially resulting in a higher intervention dose. The intervention promoting the use of spices instead of salt delivered its messages through one‐on‐one counseling, group sessions, information booklets, food‐record tool, and contact by phone or e‐mail.14 Similarly, the other successful behavioral intervention delivered its faith‐based messages about stroke risk factors through culturally sensitive materials, regular newsletters, motivational calls, and education workshops.15 Whereas the two studies that did not show a change in salt intake used one mode of delivery—mobile‐based coaching or cooking education sessions.13, 16 Other characteristics such as intervention duration, focus (salt‐specific vs broader intervention), and target population (healthy vs high‐risk) were balanced between the two effective studies and two ineffective studies, so their influence on the effectiveness could not be determined.
Future studies should examine the evidence for the effectiveness of behavior change interventions in further detail and address the common risks of bias identified in studies included in this review. These include nonrepresentative samples, subjective and unreliable outcome measures, and not controlling for other exposures that could affect the outcome. Given the uncertainty about the effectiveness of stand‐alone behavior change interventions, this review supports findings from previous studies which recommend that behavioral interventions are implemented alongside structural initiatives.7, 13
This review found that all study designs were useful for understanding which interventions may be effective in reducing population salt intake. Although observational and uncontrolled studies may not be as scientifically rigorous as RCTs, they were more externally valid such that their findings are more representative of the wider population in real‐world settings. Evaluation of intervention studies should pay greater attention to external validity,17 which should be incorporated in critical appraisals so study findings are not misinterpreted. The development of an evaluation guidance framework that considers external validity and scientific rigor while still feasible to implement, is required to help guide the design and interpretation of future evaluations of salt reduction interventions.
Lastly, only one study was conducted in LMICs and found the mobile phone–based intervention was not effective in reducing salt intake, contrary to previous studies of mHealth behavioral interventions conducted in high‐income countries.13, 18 This suggests that interventions which are effective in high‐income countries may not necessarily be successfully replicated in LMICs. This could be a result of lower resources, different sources of dietary salt, varying environmental contexts, and/or food systems. Given the rising levels of NCD deaths and disease in these countries, more resources are going to be required to support and evaluate salt reduction interventions in LMICs.
Conclusions
While varied in quality, the studies in this review show consistent evidence for the effectiveness of structural interventions and mixed evidence about the effectiveness of stand‐alone behavioral interventions for reducing population salt intake. To understand what interventions are effective in real‐world situations, studies should place greater emphasis on external validity, and an evaluation framework that supports both scientific robustness and external validity is needed. There is also a need for continued research in the development of appropriate cost‐effective interventions to reduce population salt intake, particularly in low‐resource countries.
Disclosures
KT, RM, CJ, JAS, and TSR have no conflicts of interest to declare. NC has a contract with Novartis Foundation to assist in hypertension control interventions in low‐resource settings and is a member of World Action on Salt and Health (a dietary salt reduction organization). JW is Director of the World Health Organization (WHO) Collaborating Centre on Population Salt Reduction and is supported by a National Health and Medical Research Council/National Heart Foundation Career Development Fellowship on International strategies to reduce salt. JW has funding from WHO, VicHealth, and the Australian National Health and Medical Research Council of Australia for research on salt reduction.
Supporting information
Appendix S1. Risk of bias tables for included studies on the evaluation of salt reduction interventions.
Appendix S2. Studies related to the implementation of salt reduction interventions identified between November 2015 and February 2016.
J Clin Hypertens (Greenwich). 2016;18:1194–1204. DOI: 10.1111/jch.12909. © 2016 Wiley Periodicals, Inc.
References
- 1. Arcand J, Wong MM, Trieu K, et al. The science of salt: a regularly updated systematic review of salt and health outcome (June and July 2015). J Clin Hypertens (Greenwich). 2015;18:371–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Johnson C, Raj TS, Trudeau L, et al. The science of salt: a systematic review of clinical salt studies 2013 to 2014. J Clin Hypertens (Greenwich). 2015;17:401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . Global action plan for the prevention and control of noncommunicable diseases 2013‐2020. 2013. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1. Accessed June 28, 2016.
- 4. Trieu K, Neal B, Hawkes C, et al. Salt reduction initiatives around the world—a systematic review of progress towards the global target. PLoS One. 2015;10:e0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McLaren L, Sumar N, Lorenzetti DL, et al. Population‐level interventions in government jurisdictions for dietary sodium reduction (Protocol). Cochrane Database Systemat Rev. 2012;(10):Art. No.: CD010166. DOI: 10.1002/14651858.CD010166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Christoforou A, Trieu K, Land MA, Bolam B, Webster J. State‐level and community‐level salt reduction initiatives: a systematic review of global programmes and their impact. J Epidemiol Community Health. 2016;24:2016. [DOI] [PubMed] [Google Scholar]
- 7. Trieu K, McLean R, Johnson C, et al. The science of salt: a regularly updated systematic review of the implementation of salt reduction interventions (June‐October 2015). J Clin Hypertens (Greenwich). 2016;18:487–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arcand J, Webster J, Johnson C, et al. Announcing “up to date in the science of sodium.” J Clin Hypertens (Greenwich). 2016;18:85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. The Cochrane Collaboration . Cochrane Handbook for Systematic Reviews of Interventions. Chapter 8: assessing risk of bias in included studies. Version 5.1.0 ed; 2011. http://bmg.cochrane.org/assessingrisk-bias-included-studies. Accessed November 16, 2015.
- 10. Moran A, Lederer A, Johnson Curtis C. Use of nutrition standards to improve nutritional quality of hospital patient meals: findings from New York city's healthy hospital food initiative. J Acad Nutr Diet. 2015;115:1847–1854. [DOI] [PubMed] [Google Scholar]
- 11. Merlo C, Brener N, Kann L, et al. School‐level practices to increase availability of fruits, vegetables, and whole grains, and reduce sodium in school meals—United States, 2000, 2006, and 2014. MMWR Morb Mortal Wkly Rep. 2015;64:905–908. [DOI] [PubMed] [Google Scholar]
- 12. Janssen AM, Kremer S, van Stipriaan WL, et al. Reduced‐sodium lunches are well‐accepted by uninformed consumers over a 3‐week period and result in decreased daily dietary sodium intakes: a randomized controlled trial. J Acad Nutr Diet. 2015;115:1614–1625. [DOI] [PubMed] [Google Scholar]
- 13. Rubinstein A, Miranda JJ, Beratarrechea A, et al. Effectiveness of an mHealth intervention to improve the cardiometabolic profile of people with prehypertension in low‐resource urban settings in Latin America: a randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4:52–63. [DOI] [PubMed] [Google Scholar]
- 14. Anderson CA, Cobb LK, Miller ER 3rd, et al. Effects of a behavioral intervention that emphasizes spices and herbs on adherence to recommended sodium intake: results of the SPICE randomized clinical trial. Am J Clin Nutr. 2015;102:671–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brown DL, Conley KM, Sanchez BN, et al. A multicomponent behavioral intervention to reduce stroke risk factor behaviors: the stroke health and risk education cluster‐randomized controlled trial. Stroke. 2015;46:2861–2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Robson SM, Stough CO, Stark LJ. The impact of a pilot cooking intervention for parent‐child dyads on the consumption of foods prepared away from home. Appetite. 2016;99:177–184. [DOI] [PubMed] [Google Scholar]
- 17. Bauman A, Nutbeam D. Planning and evaluating population interventions to reduce noncommunicable disease risk—reconciling complexity and scientific rigour? Public Health Res Pract. 2014;25:(1). [DOI] [PubMed] [Google Scholar]
- 18. Free C, Phillips G, Galli L, et al. The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10:e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Risk of bias tables for included studies on the evaluation of salt reduction interventions.
Appendix S2. Studies related to the implementation of salt reduction interventions identified between November 2015 and February 2016.


