Abstract
Objectives
To examine the effect of micro-osteoperforation (MOP) on the space closure rate using passive self-ligating or conventional brackets.
Materials and Methods
This was a two-arm parallel randomized controlled trial undertaken at the outpatient department of a dental college. There were 60 participants (30 women and 30 men) who fulfilled the inclusion criteria. Both the study and control groups were subjected to MOPs throughout the period of space closure. MOPs were repeated every 28 days. The experimental group (mean age 19.5 ± 1.66 years) was bonded with passive self-ligating brackets while the control group (mean age 19.9 ± 1.13 years) was bonded with conventional brackets. Both groups were examined and compared for rate of space closure. An evaluation was conducted for both groups until the entire extraction space was closed and confirmed by evaluation of a tight contact between the canine and the second premolar using a piece of dental floss.
Results
Before the initiation of retraction, all initial criteria were similar between the two groups (P > .05). No difference was observed between the two groups in the rate of space closure (P > .05).
Conclusions
MOP in conjunction with passive self-ligation does not increase the rate of orthodontic space closure when compared with MOP used with conventional brackets.
Keywords: Micro-osteoperforations, Space closure, Passive self-ligating appliances
INTRODUCTION
Closure of the extraction space in orthodontics is achieved by employing either low- or high (sliding)–friction mechanics. Closing loops and a clear understanding of biomechanics are required to achieve proper space closure with low-friction methods; space closure with sliding mechanics is relatively easier and less demanding for the clinician.1,2 This ease comes at the cost of increased friction at the bracket-wire interface, and the nature of ligation can affect this friction.3–5 Self-ligating brackets were introduced as a means to reduce friction and enable closure of space using physiological forces of considerably low magnitude,6–8 but this reduced friction may not always necessarily translate into a shorter treatment time.9,10
Apart from self-ligating brackets, many other attempts have been made to decrease the total treatment time, including surgical and nonsurgical methods. Currently, many investigations have been undertaken to determine the potency of various surgical methods in increasing the rate of space closure,11 but some evidence via meta-analysis and randomized controlled trials has indicated that surgical methods may be effective in accelerating the rate of space closure.12,13 Micro-osteoperforations (MOPs) of the alveolar bone have been employed to induce microtrauma and initiate a regional acceleratory phenomenon adjacent to the extraction space. Compared with other methods, they can be used easily in a clinical setting by the orthodontist alone. In a recently published randomized controlled trial, it was concluded that MOPs were effective in accelerating the rate of space closure when used with conventional appliances without any added discomfort to the patient.14 To investigate further, it was hypothesized that a combination of MOPs and low-friction appliances such as passive self-ligating brackets might have a synergistic effect when employed together.
The present trial was conducted to evaluate and compare the rate of space closure in patients undergoing extraction orthodontic therapy between MOPs with passive self-ligating brackets and MOPs with conventional brackets. The null hypothesis was that there would be no difference in the rate of space closure between passive self-ligating appliances and conventional ligating appliances in patients with MOPs.
MATERIALS AND METHODS
Trial Design
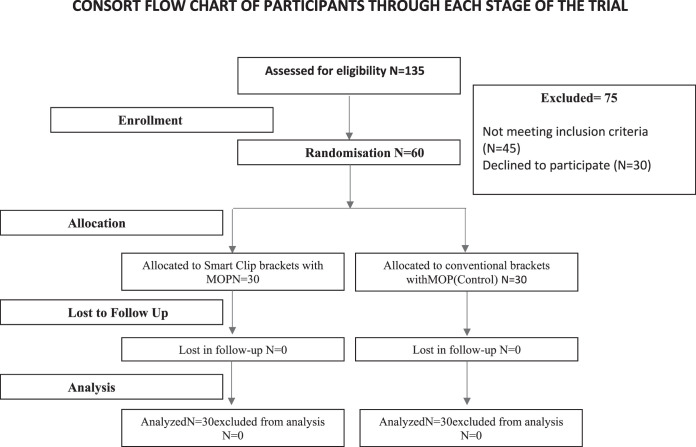
The study had an equal allocation ratio with two parallel arms. Patients participating in the trial had given prior consent, and clearance was obtained from the ethical clearance committee of the Institute of Dental Studies and Technologies (IDST/ERB/2014-17/15). The trial was registered at the National Trial Registry (CTRI/2018/03/012331) and was conducted in accordance with the Declaration of Helsinki guidelines15 and CONSORT guidelines (Figure 1).16
Figure 1.
CONSORT flowchart.
Participants, Eligibility Criteria, and Settings
The outpatient department of the Institute of Dental Studies and Technologies served as the primary source of the participants for the trial. The trial was initiated in January 2016 with initial screening and was completed in March 2017. Inclusion criteria for the trial included (1) patients in permanent dentition (13–20 years), (2) Little's Irregularity Index of <5 mm with bidental protrusion, (3) treatment plan involving extraction of the first premolars in both arches, (4) healthy periodontal condition, (5) patients with no underlying systemic conditions, and (6) Frankfurt mandibular angle between 20° and 25°. Exclusion criteria included (1) patients requiring orthognathic surgery, (2) existing medical conditions, (3) patients with active periodontal disease, (4) patients with congenital disorders, (5) patients who underwent prior orthodontic therapy, and (6) patients with underlying skeletal Class II and Class III malocclusion.
Interventions
Patients were randomly assigned to either the experimental or control groups. The experimental group consisted of patients treated with 3M Smart Clip brackets supplemented with MOP. These brackets were considered passive self-ligating appliances despite the use of nickel titanium springs as the archwire was passively held in the bracket slot.11 Finite element analysis revealed that there was no clip stress after the insertion of 0.019 × 0.025-inch stainless steel wire, making the Smart Clip bracket effectively a passive self-ligating bracket.17 The control consisted of patients treated with 3M Gemini brackets supplemented with MOP. All brackets had the MBT prescription. The first premolars were extracted at the start of the treatment, prior to the commencement of leveling and alignment. Leveling and alignment were accomplished until the 0.019 × 0.025-inch stainless steel wires fit passively.18 Retraction was initiated after a period of 3 weeks from the completion of leveling and alignment, immediately after MOP, in both groups. En masse retraction was carried out using active tie backs, and the force was standardized at 150 g using a Dontrix gauge. Provisions were made to ensure that every participant received MOPs after exactly 28 days. Second molar banding in both arches and cross-arch (transpalatal arch) stabilization in the maxillary arch served as the anchorage. As the sample included only Class I bidental protrusion cases (none of the participants developed into a Class II or a Class III during the course of space closure), Class I force was used for space closure, and intermaxillary elastics were not employed during the period of space closure. Patients were advised to inform the primary investigator immediately if bracket failure occurred, and the bracket was rebonded after thorough sandblasting to remove any residual composite in the bracket mesh. No bracket failures were reported by any participant during the space closure period. The orthodontic treatment and MOPs were performed by a single orthodontist, and extractions for all participants were done by a single surgeon. All participants were informed about the use of non-steroidal anti-inflammatory drugs and their interference with space closure. Participants were further instructed to inform the primary investigator of any medication that was taken, if a need arose during the course of space closure. Patient recruitment and treatment were performed by the primary investigator, whereas the data analysis was done by a secondary investigator who was blinded to the patient allocation.
Procedure for MOP
A PROPEL device (Propel Orthodontics, Ossining, NY) was used to perform MOPs. A pointed stainless steel tip (driven manually) was used for cortical bone perforation. The dimension of the tips used was 1.6 mm × 7 mm. Protective sleeves could be used to preset the depths of MOPs at 1 mm, 3 mm, 5 mm, and 7 mm. Chlorhexidine gluconate solution was applied, and topical local anesthetic (2% lidocaine) was sprayed prior to performing MOP. Three vertically oriented perforations were made distal to the canine, which were 1.5 mm in width and 2 to 3-mm deep within the alveolar bone. No mucoperiostal flaps were raised, and the perforations were made directly through the gingiva. The perforation was made in the edentulous area distal to the canine. Careful approximation of the canine root was made clinically by manual palpation to avoid any accidental perforation of the canine root.
Primary and Secondary Outcomes
The rate of space closure in millimeters per month was the primary outcome, and MOPs were performed throughout the period space closure, every 28 days. Pre- and postretraction models were digitized using a scanner (COMET5, 100-200-400, Steinbichler Optotechnik, Germany), and software was used to make measurements to the nearest 0.001 mm (resolution = v ± .000001 mm). A mid-palatine line was used as the reference for measurements. Perpendicular lines were drawn from the distal surface of the canine to the mesial surface of the second premolar on the reference line. Repeatability and retest reliability were assessed by remeasuring 20 randomly selected patients (10 from each group) by the same assessor after 2 weeks (intraclass coefficient = .88), and the standard error of the mean was found to be statistically not significant. Space closure was confirmed by evaluation of a tight contact between the canine and the second premolar by passing a piece of dental floss.
Randomization
Block randomization was done to achieve an equal number of participants in both groups. Patient case record numbers were used as input in the allocation sequence. The concealed sequences in sealed envelopes were then chosen by the patient. The primary investigator was not involved in randomization.
Sample Size Calculation
Calculations for the sample size were done using the nMaster 2.0 software. A power analysis was done based on the space closure data of a previous published study,14 which indicated that 21 patients per group were needed (80% power, α error = .05, Cohen's effect size .8). To further increase the power, it was decided to enroll a sample of 30 per group.
Blinding
The models were coded to blind the investigator performing data analysis to the identity of the two groups. Blinding of the participants and the primary investigator was not possible because of the nature of the trial.
Statistical Analysis
SPSS software (version 20.0; SPSS Inc, Chicago, Ill) was used. Baseline pretreatment parameters (Table 1) were compared using independent t-tests to ensure uniformity of the data. Normality of the data was checked using Shapiro-Wilk tests (Table 2) and was found to be normally distributed. The average rate of space closure was calculated as:
Table 1. .
Descriptive Statistics
| Descriptive |
Group 1 (Experimental) |
Group 2 (Control) |
| Age, y, mean ± SD | 19.5 ± 1.66 | 19.9 ± 1.13 |
| Sex, male/female | 16/14 | 14/16 |
| Mean incisor irregularity (maxilla), mm | 2.39 ± 0.51 | 2.45 ± 0.48 |
| Mean incisor irregularity (mandible), mm | 2.11 ± 0.75 | 2.20 ± 0.61 |
| Mean preretraction extraction space (maxilla), mm | 5.11 ± 0.74 | 5.09 ± 0.85 |
| Mean preretraction extraction space (mandible), mm | 5.14 ± 0.64 | 5.16 ± 0.61 |
Table 2. .
Shapiro-Wilk Normality Tests
| Parameter |
Statistic |
Degree of Freedom |
Significance |
| Monthly rate of space closure (right side maxilla) | .984 | 60 | .248 |
| Monthly rate of space closure (left side maxilla) | .954 | 60 | .277 |
| Monthly rate of space closure (right side mandible) | .955 | 60 | .236 |
| Monthly rate of space closure (left side mandible) | .974 | 60 | .301 |
Available extraction space after leveling and alignment × 28 days/days taken for the closure of extraction space.
Mean and standard deviation were used to describe the data, and independent t-test was used to check for statistically significant differences (P < .05) in the rate of space closure between the two groups (Table 3).
Table 3. .
Comparisons of Rate of Space Closure (mm/mo) Between the Groups
| Variable, mm |
Group 1 (Experimental), Mean ± SD |
Group 2 (Control), Mean ± SD |
Mean Difference |
Standard Error of Difference |
95% Confidence Interval |
P Value |
|
| Lower |
Upper |
||||||
| Monthly rate of space closure (right-side maxilla) | 0.81 ± 0.07 | 0.79 ± 0.05 | 0.014 | 0.31 | –0.05 | 0.08 | .651 |
| Monthly rate of space closure (left-side maxilla) | 0.81 ± 0.12 | 0.80 ± 0.12 | 0.007 | 0.054 | –0.10 | 0.12 | .89 |
| Monthly rate of space closure (right-side mandible) | 0.78 ± 0.08 | 0.78 ± 0.11 | 0.008 | 0.044 | –0.10 | 0.85 | .859 |
| Monthly rate of space closure (left-side mandible) | 0.77 ± 0.15 | 0.78 ± 0.07 | 0.028 | 0.054 | –0.14 | 0.08 | .615 |
RESULTS
Of the 135 subjects who were evaluated for the trial, 45 did not meet the inclusion criteria, and 30 were not willing to participate. A total of 60 participants (30 men and 30 women) were enrolled, and none of the participants were lost during the trial. Evaluation of pretreatment baseline values showed no differences between the two groups. Independent t-test was used to analyze differences between the groups. No statistically significant difference between the two groups was observed (Table 3). The mean rate of space closure per month in the experimental group was 0.81 ± 0.07 mm for the maxilla (right), 0.81 ± 0.12 mm for the maxilla (left), 0.78 ± 0.08 mm for the mandible (right), and 0.77 ± 0.15 mm for the mandible (left). In the control group, it was 0.79 ± 0.05 mm for the maxilla (right), 0.80 ± 0.12 mm for the maxilla (left), 0.78 ± 0.11 mm for the mandible (right), and 0.78 ± 0.07 mm for the mandible (left; Table 3). The total time for space closure was 190 ± 9 days for the maxilla and 200 ± 6 days for the mandible.
Harms
Accidental root perforation was the only known potential harm evaluated for the study. No such incidents were reported.
DISCUSSION
The results of the study indicated that there was no additional enhancement in the rate of space closure when MOP was combined with a low-friction environment provided by a self-ligating appliance. Friction and subsequent force loss were previously shown to be influenced by the bracket type.19 Low levels of static and dynamic friction were observed in association with passive self-ligating brackets20,21; however, this was observed only in vitro. Some authors found an increased rate of space closure,22 but most of the literature pointed toward the ineffectiveness of self-ligating brackets in increasing the rate of space closure.23–25 MOPs were shown to be effective in increasing the rate of space closure, but their efficacy in a low-friction environment was not previously evaluated.
Various methods have been described in the literature for speeding up space closure.11,26 However, only recently have attempts been made to combine the two methods and check for any synergistic effect the two techniques might have when employed together. A recent study was done to assess the combination of low-level laser therapy and MOPs to enhance the rate of space closure. The combination was then compared with the individual methods separately.27 The authors concluded that the combination was more effective than the application of each technique separately. A similar synergistic effect may be observed if MOPs are combined with any other technique. Because the low friction provided by the self-ligating appliances had not been effective clinically in previous studies, combining them with MOPs might have provided a similar synergistic effect.27 Heavy orthodontic forces are usually required to overcome friction before space closure can be initiated, which may result in hyalinization and slowing of tooth movement.28 Lower friction and the longer reactivation schedule associated with passive self-ligating appliances and MOPs might have provided an environment in which faster space closure was possible.
It was essential to standardize the age of the participants in the two groups, as it has been shown that the age of the patient does have a bearing on the rate of space closure.29 There was no statistically significant difference in mean age between the groups. Also, participants included in the trial had an average Frankfort-mandibular plane angle (FMA) (20°–25°), as a vertical growth pattern might be associated with the bite force, which in turn might have affected the rate of space closure.30
The rate of tooth movement in the present trial was slower than the rate associated with MOPs in the literature. This variation may have been due to the use of different archwires and inconsistent forces in moving canines, measurement methods, and operative methods employed in the different trials. Or there may have been operator bias, as blinding was not possible in this trial.
Archwire binding has been shown to play an important role once the contact angle between the archwire and the slot increases beyond 3.7°.31 However, in the present trial, retraction was done on a 0.019 × 0.022-inch stainless steel archwire in a 0.022 × 0.028-inch slot. The critical contact angle for this archwire-bracket slot combination has been shown to be less than 3.7° for any given bracket width.32
To compensate for the force decay of elastomeric ligatures during space closure, ligatures used in this trial were from a single manufacturer. As the maximum force decay is known to occur within 24 hours and then declines before reducing further after 4 weeks, the elastomeric module active tie backs were replaced every 28 days.33
Limitations of the Study
To address a nonlinear event such as space closure, a summary table could have been used. In this study, millimeters/month was used to quantify the rate of space closure, following established protocols.34
Generalizability
The results can be applied in a typical clinical scenario as the trial was conducted in an accredited and recognized dental college in an outpatient setting, which could mimic a typical orthodontic case load. Orthodontic therapy was provided by postgraduate resident doctors under faculty supervision.
CONCLUSION
MOP in conjunction with passive self-ligation does not offer any additional synergistic benefit in increasing the rate of orthodontic space closure.
DISCLOSURES
The authors declared no conflict of interest. There was no external source of funding for this trial.
REFERENCES
- 1.Roth RK. Treatment mechanics for the straight wire appliance. In: Graber TM, editor. Current Principles and Techniques in Orthodontics. St Louis, Mo: Mosby; 1985. pp. 665–716. [Google Scholar]
- 2.Bennett J, McLaughlin RP. Fundamentals of Orthodontic Treatment Mechanics. London: Le Grande Publishing; 2014. [Google Scholar]
- 3.Schumacher H, Bourauel C, Drescher D. The effect of the ligature on the friction between bracket and arch. J Orofac Orthop. 1990;51:106–116. doi: 10.1007/BF02164848. [DOI] [PubMed] [Google Scholar]
- 4.Kuruvadi S, Eichmiller F, Kudlick E. Frictional resistance: the interaction of bracket design and archwire alloy. Am J Orthod Dentofac Orthop. 1997;112:355. [Google Scholar]
- 5.Iwasaki LR, Beatty MW, Randall CJ. Clinical ligation forces and intraoral friction during sliding on a stainless steel archwire. Am J Orthod Dentofac Orthop. 2003;123:408–415. doi: 10.1067/mod.2003.61. [DOI] [PubMed] [Google Scholar]
- 6.Sims APT, Waters NE, Birnie DJ. A comparison of the forces required to produce tooth movement in vitro using two self-ligating brackets and a pre-adjusted bracket employing two types of ligation. Eur J Orthod. 1993;15:377–385. doi: 10.1093/ejo/15.5.377. [DOI] [PubMed] [Google Scholar]
- 7.Shivapuja PK, Berger J. A comparative study of conventional ligation and self-ligation bracket systems. Am J Orthod Dentofac Orthop. 1994;106:472–480. doi: 10.1016/S0889-5406(94)70069-9. [DOI] [PubMed] [Google Scholar]
- 8.Pizzoni L, Ravnholt G, Melsen B. Frictional forces related to self-ligating brackets. Eur J Orthod. 1998;20:283–291. doi: 10.1093/ejo/20.3.283. [DOI] [PubMed] [Google Scholar]
- 9.Miles PG. Smartclip versus conventional twin brackets for initial alignment: is there a difference. Aust Orthod J. 2005;21:123–127. [PubMed] [Google Scholar]
- 10.Miles PG, Weyant RJ, Rustveld L. A clinical trial of Damon 2 versus conventional twin brackets during initial alignment. Angle Orthod. 2006;76:480–485. doi: 10.1043/0003-3219(2006)076[0480:ACTODV]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Shirude SS, Rahalkar JS, Agarkar S. Interventions for accelerating orthodontic tooth movement: a systematic review. J Indian Orthod Soc. 2018;52:265–271. [Google Scholar]
- 12.Hoogeveen EJ, Jansma J, Ren Y. Surgically facilitated orthodontic treatment: a systematic review. Am J Orthod Dentofacial Orthop. 2014;145(4 suppl):S51–S64. doi: 10.1016/j.ajodo.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 13.Gil APS, Haas OL, Jr, Méndez-Manjón I. Alveolar corticotomies for accelerated orthodontics: a systematic review. J Craniomaxillofac Surg. 2018;46:438–445. doi: 10.1016/j.jcms.2017.12.030. [DOI] [PubMed] [Google Scholar]
- 14.Attri S, Mittal R, Batra P, Sonar S, Sharma K, Raghavan S. Comparison of rate of tooth movement and pain perception during accelerated tooth movement associated with conventional fixed appliances with micro-osteoperforations: a randomised controlled trial. J Orthod. 2018;45:225–233. doi: 10.1080/14653125.2018.1528746. [DOI] [PubMed] [Google Scholar]
- 15.World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63:e1–e37. doi: 10.1016/j.jclinepi.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Trevisi H, Bergstrand F. The SmartClip self-ligating appliance system. Semin Orthod. 2008;14:87–100. [Google Scholar]
- 18.McLaughlin RP, Bennett JC. The transition from standard edgewise to preadjusted appliance systems. J Clin Orthod. 2008;23:142–153. [PubMed] [Google Scholar]
- 19.Tecco S, Di Iorio D, Cordasco G. An in vitro investigation of the influence of self-ligating brackets, low friction ligatures, and archwire on frictional resistance. Eur J Orthod. 2007;29:390–397. doi: 10.1093/ejo/cjm007. [DOI] [PubMed] [Google Scholar]
- 20.Seo YJ, Lim BS, Park YG. Effect of self-ligating bracket type and vibration on frictional force and stick-slip phenomenon in diverse tooth displacement conditions: an in vitro mechanical analysis. Eur J Orthod. 2015;37:474–480. doi: 10.1093/ejo/cju060. [DOI] [PubMed] [Google Scholar]
- 21.Kim KR, Baek SH. Effect of passive self-ligating bracket placement on the posterior teeth on reduction of frictional force in sliding mechanics. Korean J Orthod. 2016;46:73–80. doi: 10.4041/kjod.2016.46.2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hassan SE, Hajeer MY, Alali OH. The effect of using self-ligating brackets on maxillary canine retraction: a split-mouth design randomised controlled trial. J Contemp Dent Pract. 2016;17:496–503. doi: 10.5005/jp-journals-10024-1879. [DOI] [PubMed] [Google Scholar]
- 23.Miles PG. Self-ligating vs conventional twin brackets during en-masse space closure with sliding mechanics. Am J Orthod Dentofacial Orthop. 2007;132:223–225. doi: 10.1016/j.ajodo.2007.04.028. [DOI] [PubMed] [Google Scholar]
- 24.Burrow SJ. Canine retraction rate with self-ligating brackets vs conventional edgewise brackets. Angle Orthod. 2010;80:626–633. doi: 10.2319/060809-322.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong H, Collins J, Tinsley D, Sandler J, Benson P. Does the bracket–ligature combination affect the amount of orthodontic space closure over three months? A randomized controlled trial. J Orthod. 2013;40:155–162. doi: 10.1179/1465313313Y.0000000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharma K, Batra P, Sonar S, et al. Periodontically accelerated orthodontic tooth movement: a narrative review. J Indian Soc Periodontol. 2019;23:5–11. doi: 10.4103/jisp.jisp_207_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdelhameed AN, Mubarak Refai WM. Evaluation of the effect of combined low energy laser application and micro-osteoperforations versus the effect of application of each technique separately on the rate of orthodontic tooth movement. Open Access Maced J Med Sci. 2018;6:2180–2185. doi: 10.3889/oamjms.2018.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ong MM, Wang HL. Periodontic and orthodontic treatment in adults: a review. Am J Orthod Dentofacial Orthop. 2002;122:420–428. doi: 10.1067/mod.2002.126597. [DOI] [PubMed] [Google Scholar]
- 29.Dudic A, Giannopoulou C, Kiliaridis S. Factors related to the rate of orthodontically induced tooth movement. Am J Orthod Dentofacial Orthop. 2013;143:616–621. doi: 10.1016/j.ajodo.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 30.Pepicelli A, Woods M, Briggs C. The mandibular muscles and their importance in orthodontics: a contemporary review. Am J Orthod Dentofacial Orthop. 2005;128:774–780. doi: 10.1016/j.ajodo.2004.09.023. [DOI] [PubMed] [Google Scholar]
- 31.Kusy RB, Whitley JQ. Assessment of second-order clearances between orthodontic archwires and bracket slots via the critical contact angle for binding. Angle Orthod. 1999;69:71–80. doi: 10.1043/0003-3219(1999)069<0071:AOSOCB>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Kang B-S, Baek S-H, Mah J, Yang W-S. Three-dimensional relationship between the critical contact angle and the torque angle. Am J Orthod Dentofac Orthop. 2003;123:64–73. doi: 10.1067/mod.2003.55. [DOI] [PubMed] [Google Scholar]
- 33.Mohammadi A, Mahmoodi F. Evaluation of force degradation pattern of elastomeric ligatures and elastomeric separators in active tieback state. J Dent Res Dent Clin Dent Prospects. 2015;9:254–260. doi: 10.15171/joddd.2015.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hosni S, Harrison JE. Relevant research from orthodontic journals: focus on rate of tooth movement. J Orthod. 2018;45:218–222. doi: 10.1080/14653125.2018.1501938. [DOI] [PubMed] [Google Scholar]