Abstract
Objective
To evaluate the impact of rapid maxillary expansion (RME) on the condylar position, disc joint, joint space, and interarticular relationship in growing patients.
Materials and Methods
A systematic search was performed in nine databases. The clinical studies selected included those with pre- and post-magnetic resonance, conventional computed tomography or cone beam tomography in growing patients. Risk of bias assessment was performed using the Cochrane Collaboration tool for controlled clinical studies and National Heart, Lung, and Blood Institute (NHLBI) Quality Assessment for Before-After Studies With No Control Group.
Results
Initially, 4303 records were identified. Only eight studies fulfilled the criteria and were included in the qualitative analysis. Of those, two were controlled clinical studies with a risk of uncertain to high bias. The remaining papers had a low to moderate risk of bias. Results showed that RME in children and adolescents promoted the following: remodeling in the head and or condylar branch, changes in condylar position and joint space, maintenance of improved symmetry between the condyles, and no ability to modify the position or shape of the articular disc.
Conclusions
RME in growing patients is able, in the short term, to modify the condyle-fossa relationship but does not change the position or shape of the articular disc. The intercondylar symmetric relationship is maintained or improved. Although the NHLBI score shows low to moderate risk of bias, the clinical relevance of these review findings is limited by Cochrane and Grades of Recommendation, Assessment, Development and Evaluation scores.
Keywords: Systematic review, Rapid maxillary expansion, Temporomandibular joint
INTRODUCTION
Rapid maxillary expansion (RME) has been used as a routine clinical procedure, with the main objective of mechanically separating the palatine suture in young patients with maxillary transverse constriction, deep palatal vault, and or posterior crossbite. It has also been used in cases of crowding by increasing the perimeter of the arch and other situations where a transverse increase is necessary.1,2
After opening the median palatal suture, not only transverse but also vertical and anteroposterior changes occur. Clockwise rotation of the mandibular plane, resulting from a lower and posterior position of the mandible after RME, has been one of the most reported effects.3,4 These changes may directly or indirectly affect other structures of the craniofacial complex to which the maxilla is interconnected, including the temporomandibular joint (TMJ).5
TMJ is referred to as the most complex articulation of the human organism, with its visualization difficult due to the anatomy and presence of neighboring structures. Thus, computed tomography (CT) is the examination of choice for the detailed study of changes in TMJ skeletal structures and magnetic resonance imaging (MRI) is the preferred diagnostic method for observation of the TMJ joint disc.6 Studies of the effects of RME on the TMJ are controversial. It is essential to synthesize the evidence and clarify the real impact of this intervention on the TMJ.
A previous systematic review summarized TMJ alterations after correction of posterior crossbites in growing patients.7 However, the authors included studies in which patients received other orthodontic procedures associated with RME. In one of them,8 there was intervention in the maxilla and mandible, including the McNamara expander and U-Bow type I activator. This may have increased the risk of bias since mandibular protrusion may have induced condylar remodeling in growing patients.9 This same study used ultrasound as the method of analysis of the TMJ, which does not give sharpness and precision in the assessment of articular structures.10
The current systematic review evaluated the impact of RME on condylar position, disc joint, joint space, and interarticular relationship in growing patients by means of CT or MRI. The studies included were those in which subjects underwent RME only.
MATERIALS AND METHODS
Registration and Protocol
This review was registered in the PROSPERO database under protocol CRD42017055790 (https://www.crd.york.ac.uk/PROSPERO/), in accordance with the PRISMA check-list of systematic reviews and meta-analyses.11
Sources of Information, Research Strategy and Selection of Studies
The scientific literature was searched in May 2018 and alerts were received from the databases until October 2019. The search was conducted to identify articles reporting the effects of RME on the TMJ by means of MRI, CT, or cone beam tomography. A detailed search was conducted in the following electronic databases: PubMed, Scopus, Web of Science, Cochrane, Lilacs, Science Direct, OpenGrey, Google Scholar, and ClinicalTrials. An additional hand search was conducted to identify additional relevant publications. No restrictions were placed on the publication date or language. Specific search strategies were developed for each database (Appendix A). All relevant quotations were saved in the Endnote bibliographic reference manager (version X7, Thomson Reuters). The triage of articles by title and abstract; and full text, data extraction, and quality assessment were done independently by the first two authors. Disagreements were resolved through a consensus meeting and, where appropriate, consulted with a third author.
Eligibility Criteria
The eligibility criteria were defined based on the PICO research strategy for clinical practice based on scientific evidence.
Inclusion Criteria
Participants: growing patients with mixed or young permanent dentition and without symptomatology of temporomandibular dysfunction;
Intervention: RME;
Comparison: Evaluation before RME or growing patients receiving no treatment;
Outcome: Measurements in TMJ by means of CT or MRI; and
Types of studies: Randomized, non-randomized, prospective, or retrospective clinical trials.
Exclusion Criteria
Studies examining patients with cleft lip and or palate or any craniofacial anomalies;
Studies including cases with extraction of permanent teeth, previous orthodontic treatment, and any other type of interventions associated with RME; and
Case series, opinion articles, in vitro or animal studies, and literature reviews.
After reading the titles and abstracts, the articles that were not in accordance with the proposed theme were eliminated, the remaining articles were read for eligibility, and a final decision was made.
Data Items and Collection
A data extraction table was developed with the following items: author's name, year of publication, type of malocclusion, and the need for expansion, sample size, age, expander device used, activation protocol, time measurement, and result of interest.
Risk of Bias in Individual Studies
The articles finally selected and included in this review were analyzed for risk of bias. For randomized controlled trials with a control group, the Cochrane Collaboration tool was used for systematic reviews of intervention.12 For studies without a control group, the National Heart, Lung, and Blood Institute (NHLBI) tool was used for Pre-Post studies.13
Evaluation of the Level of Evidence
The level of evidence was calculated using the Grading of Recommendations, Assessment, Development and Evaluation Pro software (GRADEpro Guideline Development Tool, available online at www.gradepro.org).14
RESULTS
Selection and Characteristics of the Studies
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of the study selection process is presented in Figure 1. The established search strategy found the following number of records per database: PubMed (n = 1883), Scopus (n = 755), Web of Science (n = 689), Cochrane (n = 206), Lilacs (n = 408), Science direct (n = 168), OpenGrey (n = 0), and Google scholar (n = 194), totaling 4303 records. After deletion of duplicates, there were 2750 records for title and abstract reading of which 2735 were eliminated because they were not related to the topic or were case reports, editorials, letters, or literature reviews. Thus, the remaining 15 records were selected for full-text reading. Of these, one study was eliminated because it was a protocol proposal to be followed in future studies,15 one for evaluating pre- and post-intervention changes through gypsum models and bite registration,16 one for assessing condylar change by means of zonograms,17 and five studies were excluded since they examined patients who underwent slow maxillary expansion.10,18–21 Therefore, seven articles from the systematic search were included for qualitative analysis;22–28 as well as one record found by hand search (n = 1);29 totaling eight articles included in this review (Table 1). A quantitative analysis was not feasible given the heterogeneity in the methodology of the selected articles.
Figure 1.
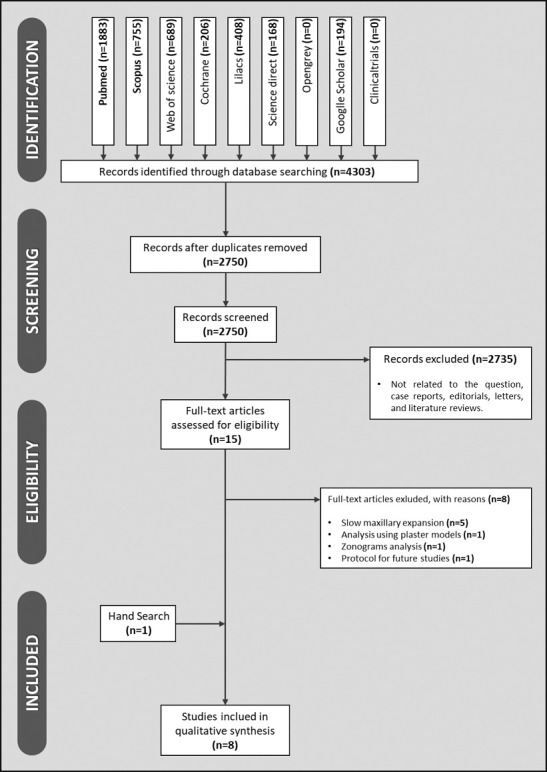
Flow diagram representative of this review (PRISMA model).
Table 1. .
Data Extraction of Articles Included in This Systematic Reviewa
| Author and Year |
Sample and Age |
Malocclusion Class |
Need for Expansion |
Expander Device |
Activation Protocol |
Measurement Type |
Interest Outcome |
| Arat et al. (2008)22 | 18 patients | NA | Unilateral or bilateral posterior crossbite | Haas | Magnetic Resonance Imaging | RME promotes remodeling in the head and / or condylar branch. | |
| (9.75–14.8 years) | 2/4 turn/d until overcorrection | •Condylar remodeling | |||||
| •At the beginning of the treatment, 6 and 18 weeks after the activations | |||||||
| Arat et al. (2008)23 | 18 patients | NA | Unilateral or bilateral posterior crossbite | Haas | 2/4 turn/d until overcorrection | Magnetic Resonance Imaging | RME does not change the position of the articular disc. |
| (9.75–14.8 years) | •Positioning of the articular disc | ||||||
| •At the beginning of the treatment and 18 weeks after the activations | |||||||
| Masi et al. (2009)24 | 30 patients | I, II, or III | FUPC | Haas | 1 turn/d until overcorrection | Magnetic Resonance Imaging | RME does not change the position of the articular disc. |
| (6.8–14.2 years) | •Positioning and shape of the articular disc | ||||||
| •At the beginning of the treatment, 12 and 18 weeks after the activations | |||||||
| Matta et al. (2009)25 | 10 patients | I | FUPC | Haas | 2/4 turn/d until overcorrection | RME altered the condylar position and joint space, promoting greater spatial symmetry between the crossed and non-crossed sides. | |
| (7.2–11.2 years) | Conventional tomography | ||||||
| •Condylar position and joint space | |||||||
| •At the beginning of the treatment and 12 weeks after the activations | |||||||
| Leonardi et al. (2012)26 | 39 patients | I | Group 1: 26 patients | Hyrax | 3/4 turn for up to 18 days | Conventional tomography | RME promoted an increase of the joint spaces maintaining the symmetry of the condyle-fossa joint relationship. |
| (8.2–11.6 years) | 26 patients | •Conventional tomography | |||||
| Maxillary constriction with FUPC | •At the beginning of treatment and at the end of activations | ||||||
| Group 2: | |||||||
| 13 patients | |||||||
| Palatine displaced canine without FUPC | |||||||
| Melgaço et al. (2014)27 | 34 patients | I | Maxillary constriction without posterior crossbite | Haas and Hyrax | Cone-beam tomography | RME induces a change in condylar position, down and forward symmetrically on both sides, without generating asymmetry. | |
| (average age of 12 years and 10 months for girls and 13 years for boys) | 1 full turn on the first day and 2/4 turn in the next 6 days | •Condilar position | |||||
| •At the beginning of treatment and 12 weeks after activations | |||||||
| Mcleod et al. (2016)28 | 37 patients | NA | Group 1: | Hyrax | 2/4 turn/d until overcorrection | Cone-beam tomography | RME does not alter the condylar position in the glenoid cavity. |
| (11–17 years) | 19 patients | •Glenoid fossa and joint space | |||||
| Maxillary constriction with FUPC | •At the beginning of treatment and 24 weeks after activations | ||||||
| Group 2: | |||||||
| 18 patients | |||||||
| With delayed treatment | |||||||
| Ghoussoub et al. (2018)29 | 27 patients | NA | Group 1: | Hyrax | 2/4 turn/d until overcorrection | Cone-beam tomography | RME is effective during growth, widening the interglenoid fossa distance and the lateral positions of the condyles. |
| (8–13 years) | 18 patients | •Condyllar position and glenoid fossa | |||||
| Maxillary constriction with BPC | •At the beginning of treatment and 24 weeks after activations | ||||||
| Group 2: | |||||||
| 9 patients | |||||||
| With delayed treatment |
NA indicates not available; FUPC, functional unilateral posterior crossbite; BPC, bilateral posterior crossbite; RME, rapid maxillary expansion.
The patients' ages ranged from 6.8 years24 to 17 years.28 The sample size ranged from 10 patients25 to 39 patients.27 Regarding the method used to measure changes, three articles used MRI, of which two evaluated the articular disc,23,24 and the other one evaluated remodeling of the head and the condylar branch.22 Five articles evaluated the condylar position and articular spaces by means of tomography: two by conventional tomography25,26 and three by cone beam tomography.27–29
The standard protocol for RME employed by several authors4,5 consisted of two quarter-turns of activation per day until overcorrection was reached. That protocol was used for six of the studies included.22–25,28,29 Leonardi et al. (2012)26 used the protocol of three quarter-turns per day while Melgaço et al. (2014)27 achieve one full turn per day.
All of the studies carried out measurements prior to expansion. However, variability was observed in relation to the time of measurement fafter the activations. One study evaluated after 6 and 18 weeks,22 two after 12 weeks,25,27 one after 12 and 18 weeks,24 one after 18 weeks,23 two after 24 weeks,28,29 and one immediately after the activations.26
Results of Individual Studies
Arat et al. (2008)22 observed that RME induced remodeling in the head and condylar branch. One article reported that RME modified joint space and condylar postion, promoting greater spatial symmetry between the crossbite and non-crossbite25 side. Three articles found that the RME was able to change the individual condylar position27,28,30 and joint space,26,29 maintaining the symmetric relationship between the condyles.26,27,29 There was no evaluation of intercondylar symmetry in the measures used by McLeod et al. (2016),28 who observed no alteration of the condylar position in the glenoid fossa in individuals.
The two studies that analyzed the articular disc reported that RME did not alter the articular disc either in shape24 or in position,23,24 whether they were normally placed or had displacement prior to expansion.
Risk of Bias in the Studies—Cochrane Score
In the study published by McLeod et al. (2016),28 there was insufficient information about the process of random sequence generation, concealment of allocation, and blinding of outcome assessors. An imbalance was also observed in the number of patients included and the absence of a sample calculation. Four attempts over two months were made to contact the authors to obtain the necessary information; however, there was no response. Quality score was “risk of uncertain bias.”
No random sequence generation, allocation concealment, and an imbalance in the number of subjects between groups was observed in Ghoussoub et al. (2018).29 Quality score was “high risk of bias.”
Blinding of participants or professionals would not affect the outcome; (Figure 2).
Figure 2.
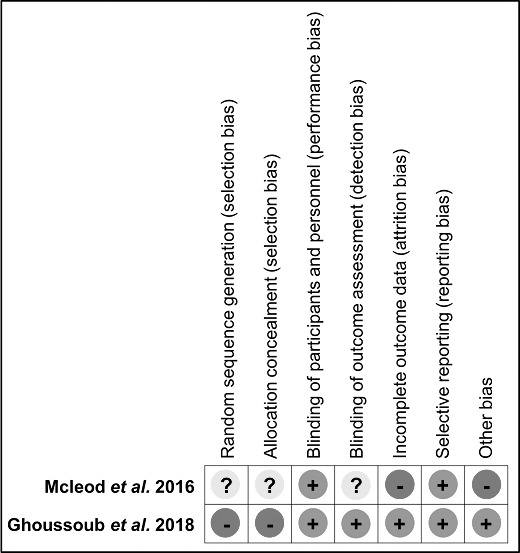
Cochrane Qualifier score.
Risk of Bias in the Studies—NHLBI Score
Arat et al. (2008) conducted a large study subdivided into three articles. In the present review, parts 222 and 3,23 which analyzed the condylar remodeling and articular disc, respectively, were assessed for risk of bias in a single way and using the term “Arat et al. (2008).22,23”
The NHLBI assessment revealed, in Table 2, that three articles had a “good” score indicating low bias risk24,26,27 and three articles had a “fair” score indicating moderate risk of bias.22,23,25 None of those scored a “bad” score that would indicate a high risk of bias. Only one study27 presented an adequate methodology for all items on the checklist of the qualifier.
Table 2. .
NHLBI Qualifier Scorea
| Arat et al. (2008)22,23 |
Masi et al. (2009)24 |
Matta et al. (2009)25 |
Leonardi et al. (2012)26 |
Melgaço et al. (2014)27 |
|
| 1. Was the study question or objective clearly stated? | YES | YES | YES | YES | YES |
| 2. Were eligibility/selection criteria for the study population prespecified and clearly described? | YES | NR | NR | YES | YES |
| 3. Were the participants in the study representative of those who would be eligible for the test/service/intervention in the general or clinical population of interest (mixed or permanent dentition in growing patients)? | YES | YES | YES | YES | YES |
| 4. Were all eligible participants that met the prespecified entry criteria enrolled (no symptoms of TMD, no fixed appliances)? | NR | NR | YES | YES | YES |
| 5. Was the sample size sufficiently large to provide confidence in the findings? | NR | NR | NR | YES | YES |
| 6. Was the test/service/intervention clearly described and delivered consistently across the study population? | YES | YES | YES | YES | YES |
| 7. Were the outcome measures prespecified, clearly defined, valid, reliable, and assessed consistently across all study participants (CBT or resonance + adequate parameters to evaluate the outcome)? | YES | YES | YES | YES | YES |
| 8. Were the people assessing the outcomes blinded to the participants' exposures/interventions? | YES | YES | NR | YES | YES |
| 9. Was the loss to follow-up after baseline 20% or less? Were those lost to follow-up accounted for in the analysis? | YES | YES | YES | YES | YES |
| 10. Did the statistical methods examine changes in outcome measures from before to after the intervention? Were statistical tests done that provided P values for the pre-to-post changes? | NO | YES | YES | YES | YES |
| 11. Were outcome measures of interest taken multiple times before the intervention and multiple times after the intervention (ie, did they use an interrupted time-series design)? | NR | YES | NR | YES | YES |
| 12. If the intervention was conducted at a group level (eg, a whole hospital, a community, etc.) did the statistical analysis take into account the use of individual-level data to determine effects at the group level? | NA | NA | NA | NA | NA |
| QUALITY ASSESSMENT | FAIR | GOOD | FAIR | GOOD | GOOD |
NA indicates not applicable; NR, not reported.
The primary outcome of each study as well as the quality assessment results are shown in Table 3.
Table 3. .
Outcome Summary and Qualifiers Used
| Included Studies |
TMJ Assessment |
Alteration |
Intercondilar Symmetry (pre and post RME) |
Quality Assessment |
||
| Condylar Position |
Disc Joint |
Joint Space |
||||
| Arat et al. (2008)22 | X* | YES | NE | NHLBI (Fair) | ||
| Arat et al. (2008)23 | X | NO | NE | NHLBI (Fair) | ||
| Masi et al. (2009)24 | X | NO | NE | NHLBI (Good) | ||
| Matta et al. (2009)25 | X | X | YES to both | Asymmetrical to symmetrical | NHLBI (Fair) | |
| Leonardi et al. (2012)26 | X | X | YES to both | Symmetrical and remained the same | NHLBI (Good) | |
| Melgaço et al. (2014)27 | X | YES | Symmetrical and remained the same | NHLBI (Good) | ||
| McLeod et al. (2016)28 | X | NO | NA | Cochrane (Uncertain) | ||
| Ghoussoub et al. (2018)29 | X | X | YES to both | Symmetrical and remained the same | Cochrane (High risk) | |
condylar position assessed by remodeling; RME indicates rapid maxillary expansion; NE, not evaluable (used resonance); NA, not available.
Assessment of the Quality of Evidence
The GRADE (Grading of Recommendations, Assessment, Development and Evaluation) evidence profile table is described in Table 4. The evidence for the outcomes evaluated ranged from low to very low quality, suggesting that the estimate reported can differ significantly from the measure evaluated.
Table 4. .
GRADE Evidence: Can the Condylar Position, Articular Disc, and Joint Space of TMJ Be Altered by RME in Growing Patients?
| Certainty Assessment |
Impact |
Certainty |
Importance |
||||||
| No. of Studies |
Study Design |
Risk of Bias |
Inconsistency |
Indirect Evidence |
Inaccuracy |
Other Considerations |
|||
| CHANGES IN CONDYLAR POSITION (randomized) | |||||||||
| 1 | randomized controlled trial | seriousa | not serious | not seriousb | very seriousc | none | RME does not alter the condylar position. | ⊕○○○ VERY LOW | CRITICAL |
| CHANGES IN CONDYLAR POSITION (observational) | |||||||||
| 4 | observational study | serious | not serious | not serious | not serious | none | RME alters the condylar position. | ⊕○○○ VERY LOW | CRITICAL |
| SIGNS OF MANDIBULAR CONDYLE REMODELING | |||||||||
| 1 | observational study | not serious | not serious | not serious | graved | none | RME promotes condylar remodeling. | ⊕○○○ VERY LOW | IMPORTANT |
| CHANGES IN ARTICULAR JOINT SPACE | |||||||||
| 3 | observational study | gravee | not serious | not serious | not serious | none | RME promotes joint space symmetry. | ⊕○○○ VERY LOW | CRITICAL |
| CHANGES IN THE ARTICULAR DISK POSITION | |||||||||
| 2 | observational study | not serious | not serious | not serious | not serious | none | RME does not modify the position of the articular disc. | ⊕⊕○○ LOW | CRITICAL |
| CHANGES IN THE ARTICULAR DISK SHAPE | |||||||||
| 1 | observational study | not serious | not serious | not serious | not serious | none | RME does not modify the shape of the articular disc. | ⊕⊕○○ LOW | CRITICAL |
a Serious concern regarding an unclear risk of bias in one article and a high risk in another.
b The age range of patients could include those who were no longer growing.
c There was insufficient information about the process of random sequence generation, concealment of allocation, and blinding of outcome assessors.
d The authors chose to use only one method of visual inspection, not using statistical analysis.
e Serious concern regarding a high risk of bias in one article.
DISCUSSION
No previous systematic review evaluating changes in the TMJ after RME using only 3D images was found in the literature. In the present review, articles that evaluated changes after RME in the condyle, disc, and/or fossa by means of CT or MRI were included. All articles included in this review had a well-defined study objective, a sample consistent with the need for maxillary expansion, intervention with a well-described treatment protocol, and well-defined prespecified outcome measures.
For a significant difference between two groups of one standard deviation, 33 individuals would generate 80% power to detect this difference at a significance level of an alpha level of 0.05. Three studies fulfilled this requirement,26–28 with a sample of 34, 39, and 37 individuals, respectively. Thus, to fill item 5 of the NHLBI qualifier, “NR” (not reported) was attributed to articles that did not report the sample size calculation, since it was not possible to determine if the sample would be representative of the population. However, if there were articles where the sample size was less than 10 patients in the interest group, the item would be classified as “No” because this small sample size would probably not be adequate to provide reliable results. This protocol was adopted by Lisboa et al. (2018)30 in their review on the effects of mandibular advancement or retreat surgery on soft facial tissue.
Four articles22,23,28,29 did not report the type of malocclusion of the patients. Three studies used only patients with Class I malocclusion,25–27 while one article24 used a sample with 11 patients with Class I malocclusion, 17 with Class II malocclusion (11 subdivision and six total), and two patients with Class III malocclusion. In all articles included in this review there was no report on modification or correction of malocclusion after RME. In a systematic review about sagittal changes after RME in Class II patients,31 it was concluded that the studies found had methodological deficiencies with controversial or non-relevant sagittal effects. Coskuner and Ciger (2015)18 verified that a Class II relationship can be corrected to a certain extent by slow expansion of the maxilla with a quadhelix; however, there was no significant effect on the TMJ.
The proper use of statistics minimized errors in reporting the results and interpreting findings. Based on the “Tutorial for statistical test tutorial,”32 all of the studies used adequate tests for their analysis, with the exception of Arat et al. (2008)22,23 who did not perform the Wilcoxon test suggested by the tutorial. In that study, a method of visual inspection was used instead, ignoring the inferential statistical analysis.
Of the eight articles included in this review, two24,29 did not report whether there were no clinical signs and symptoms of temporomandibular dysfunction. Based on this review, it was observed that RME did not promote intercondylar impairment in patients with funtional unilateral posterior crossbite (FUPC) or maxillary constriction with bimaxillary posterior crossbite. Intercondylar asymmetry was improved to a symmetric position in patients with FUPC. Kasimoglu et al. (2007)33 investigated the relationship between vertical asymmetries of the mandibular condyle with different occlusion types and concluded that growing patients with FUPC might be at risk for developing skeletal mandibular asymmetries in the future and the early correction of posterior crossbite can help practitioners to prevent skeletal asymmetries.
During the analysis of the results of the two studies that evaluated the articular disc,23,24 it was concluded that RME was not able to change the articular disc even in patients who had pretreatment disc displacement. This was in agreement with Wadhawan et al. (2008)34 who used the Twin-Block and Bionator orthopedic appliances in growing patients. Kinzinger et al. (2006),35 used functional mandibular advancement devices and showed that, although the joints initially showed partial or total anterior displacement of the disc, a significant improvement could be achieved.
There were no studies regarding the effects of RME on the TMJ after the retention period. All studies evaluated the immediate effects, with the post-treatment evaluation being performed shortly after the active period or in the retention period (12 to 24 weeks after activation). Lagravère et al. (2006),36 in their systematic review on the long-term skeletal effects of RME, showed that changes in the mandibular position were temporary. Garib et al. (2007)37 evaluated the effects of RME and long-term orthodontic treatment. Three years after the end of treatment, the immediate effects of RME were not significant in the long term.
CONCLUSIONS
RME in growing patients is able, in the short term, to modify the condyle-fossa relationship, not modifying the position or shape of the articular disc, but able to maintain or improve the intercondylar symmetry relationship.
Although the NHLBI score is low to moderate risk of bias, the clinical relevance of these review findings is limited by the Cochrane and GRADE scores.
Clinical Implications
Due to the methodological quality of the available evidence, RME cannot be indicated for the sole purpose of altering the TMJ individually or inter-articularly in growing patients requiring maxillary expansion.
Recommendations for Future Research
There is a need for improved reliability of evidence on the subject, preferably through randomized controlled trials with long-term follow-up that cover post-retention stability and investigate a possible mitigation of the risk of developing future mandibular skeletal asymmetries in growing patients requiring maxillary expansion.
APPENDIX A.
Search Strategy for Each Database
|
PUBMED |
Search ((((((((((((((((((((((((((((((((((((((((((((“palatal expansion technique”[MeSH Terms]) OR “palatal expansion technique”[Title/Abstract]) OR “expansion technique, palatal”[Title/Abstract]) OR “expansion techniques, palatal”[Title/Abstract]) OR “palatal expansion techniques”[Title/Abstract]) OR “technique, palatal expansion”[Title/Abstract]) OR “palatal expansion technic”[Title/Abstract]) OR “expansion technic, palatal”[Title/Abstract]) NOT “expansion technics, palatal”[Title/Abstract]) OR “palatal expansion technics”[Title/Abstract]) OR “technic, palatal expansion”[Title/Abstract]) OR “maxillary expansion”[Title/Abstract]) OR “expansion, maxillary”[Title/Abstract]) OR “Rme”[Title/Abstract]) OR “rapid maxillary expansion”[Title/Abstract]) OR “rapid palatal expansion”[Title/Abstract]) OR “palatal disjunction”[Title/Abstract]) OR “rapid palatal expander”[Title/Abstract]) OR “hass appliance”[Title/Abstract]) OR “hass expander”[Title/Abstract]) OR “modified hass appliance”[Title/Abstract]) OR “hygenic rapid expander”[Title/Abstract]) OR “hirax appliance”[Title/Abstract]) OR “hirax expander”[Title/Abstract]) OR “hyrax appliance”[Title/Abstract]) OR “hyrax expander”[Title/Abstract]) OR “modified hirax appliance”[Title/Abstract]) OR “bonded expander”[Title/Abstract]) OR “bonded rapid maxillary expander”[Title/Abstract]) OR “haas-type orthopedic appliance”[Title/Abstract]) OR “haas-type orthopedic appliances”[Title/Abstract]) OR “haas-type expansion appliance”[Title/Abstract]) OR “haas- type expansion appliances”[Title/Abstract]) OR “tooth borne expander”[Title/Abstract]) OR “mcnamara appliance”[Title/Abstract]) OR “mcnamara expander”[Title/Abstract]) OR “modified mcnamara appliance”[Title/Abstract]) OR “rapid midpalatal suture opening”[Title/Abstract]) OR “rapid midpalatal suture disjunction”[Title/Abstract]) OR “opening the midpalatal suture”[Title/Abstract]) OR “maxillary orthopedic expansion”[Title/Abstract]) OR “orthopedic maxillary expansion”[Title/Abstract])) AND (((((((((((((((“child”[MeSH Terms]) OR “child”[Title/Abstract]) OR “Children”[Title/Abstract]) OR “Kid”[Title/Abstract]) OR “Kids”[Title/Abstract]) OR “boy”[Title/Abstract]) OR “boys”[Title/Abstract]) OR “Girl”[Title/Abstract]) OR “girls”[Title/Abstract])) OR (((((((((((((((((((“adolescent”[MeSH Terms]) OR “adolescent”[Title/Abstract]) OR “adolescents”[Title/Abstract]) OR “adolescence”[Title/Abstract]) OR “Teens”[Title/Abstract]) OR “Teen”[Title/Abstract]) OR “teenagers”[Title/Abstract]) OR “Teenager”[Title/Abstract]) OR “youth”[Title/Abstract]) OR “Youths”[Title/Abstract]) OR “adolescents, female”[Title/Abstract]) OR “adolescent, female”[Title/Abstract]) OR “female adolescent”[Title/Abstract]) OR “female adolescents”[Title/Abstract]) OR “adolescents, male”[Title/Abstract]) OR “adolescent, male”[Title/Abstract]) OR “male adolescent”[Title/Abstract]) OR “male adolescents”[Title/Abstract]) OR “Young”[Title/Abstract])) OR ((((((“temporomandibular joint”[MeSH Terms]) OR “temporomandibular joint”[Title/Abstract]) OR “joint, temporomandibular”[Title/Abstract]) OR “joints, temporomandibular”[Title/Abstract]) OR “temporomandibular joints”[Title/Abstract]) OR “TMJ”[Title/Abstract])) OR (((((((((((((((((((((((((((((((“temporomandibular joint disc”[MeSH Terms]) OR “temporomandibular joint disc”[Title/Abstract]) OR “disc, temporomandibular joint”[Title/Abstract]) OR “discs, temporomandibular joint”[Title/Abstract]) OR “joint disc, temporomandibular”[Title/Abstract]) OR “joint discs, temporomandibular”[Title/Abstract]) OR “temporomandibular joint discs”[Title/Abstract]) OR “disk, temporomandibular joint”[Title/Abstract]) OR “articular disc, temporomandibular”[Title/Abstract]) OR “articular discs, temporomandibular”[Title/Abstract]) OR “disc, temporomandibular articular”[Title/Abstract]) OR “discs, temporomandibular articular”[Title/Abstract]) OR “temporomandibular articular disc”[Title/Abstract]) OR “temporomandibular articular discs”[Title/Abstract]) OR “articular disk, temporomandibular”[Title/Abstract]) OR “articular disks, temporomandibular”[Title/Abstract]) OR “disk, temporomandibular articular”[Title/Abstract]) OR “disks, temporomandibular articular”[Title/Abstract]) OR “temporomandibular articular disk”[Title/Abstract]) OR “temporomandibular articular disks”[Title/Abstract]) OR “temporomandibular joint disk”[Title/Abstract]) OR “disks, temporomandibular joint”[Title/Abstract]) OR “joint disk, temporomandibular”[Title/Abstract]) OR “joint disks, temporomandibular”[Title/Abstract]) OR “temporomandibular joint disks”[Title/Abstract]) OR “condyle-disc positions”[Title/Abstract]) OR “condyle disc positions”[Title/Abstract]) OR “condyle disc position”[Title/Abstract]) OR “condyle-disc position”[Title/Abstract]) OR “articular disc position”[Title/Abstract]) OR “articular disc positions”[Title/Abstract])) OR ((((((((((((((((((“mandibular condyle”[MeSH Terms]) OR “mandibular condyle”[Title/Abstract]) OR “condyle, mandibular”[Title/Abstract]) OR “condyles, mandibular”[Title/Abstract]) OR “mandibular condyles”[Title/Abstract]) OR “coronal condylar angles”[Title/Abstract]) OR “condylar spatial changes”[Title/Abstract]) OR “condyle”[Title/Abstract]) OR “condyles”[Title/Abstract]) OR “condylar remodeling”[Title/Abstract]) OR “condylar head”[Title/Abstract]) OR “Condylar”[Title/Abstract]) OR “condylar height”[Title/Abstract]) OR “condyle position”[Title/Abstract]) OR “condylar position”[Title/Abstract]) OR “condylar response”[Title/Abstract]) OR “condylar regions”[Title/Abstract]) OR “coronal condylar angle”[Title/Abstract])) OR (((((((((((((((((((“glenoid cavity”[MeSH Terms]) OR “glenoid cavity”[Title/Abstract]) OR “cavities, glenoid”[Title/Abstract]) OR “cavity, glenoid”[Title/Abstract]) OR “glenoid fossa of the scapula”[Title/Abstract]) OR “glenoid fossa”[Title/Abstract]) OR “fossa, glenoid”[Title/Abstract]) OR “fossas, glenoid”[Title/Abstract]) OR condyle fossa relationship”[Title/Abstract]) OR “condyle fossa relationships”[Title/Abstract]) OR “joint spaces”[Title/Abstract]) OR “anterior space”[Title/Abstract]) OR “superior space”[Title/Abstract]) OR “posterior space”[Title/Abstract]) OR “joint space”[Title/Abstract]) OR “joint spaces”[Title/Abstract]) OR “glenoid fossa”[Title/Abstract]) OR “articular fossa”[Title/Abstract]) OR “mandibular fossa depth”[Title/Abstract]))) |
| SCOPUS | ( TITLE-ABS-KEY ( child* ) TITLE-ABS-KEY ( kid* ) OR TITLE-ABS-KEY ( boy* ) OR TITLE-ABS-KEY ( girl* ) OR TITLE-ABS-KEY ( adolescen* ) OR TITLE-ABS-KEY ( teen* ) OR TITLE-ABS-KEY ( youth* ) OR TITLE-ABS-KEY ( “female adolescent*” ) OR TITLE-ABS-KEY ( “male adolescent*” ) OR TITLE-ABS-KEY ( “adolescent*, female” ) OR TITLE-ABS-KEY ( “adolescent*, male” ) OR TITLE-ABS-KEY ( young ) OR TITLE-ABS-KEY ( “temporomandibular joint” * ) OR TITLE-ABS-KEY ( “joint*, temporomandibular” ) OR TITLE-ABS-KEY ( tmj ) OR TITLE-ABS-KEY ( “temporomandibular joint disc*” ) OR TITLE-ABS-KEY ( “disc*, temporomandibular joint” ) OR TITLE-ABS-KEY ( “joint disc*, temporomandibular” ) OR TITLE-ABS-KEY ( “disk*, temporomandibular joint” ) OR TITLE-ABS-KEY ( “articular disc*, temporomandibular” ) OR TITLE-ABS-KEY ( “disc*, temporomandibular articular” ) OR TITLE-ABS-KEY ( “temporomandibular articular disc*” ) OR TITLE-ABS-KEY ( “articular disk*, temporomandibular” ) OR TITLE-ABS-KEY ( “disk*, temporomandibular articular” ) OR TITLE-ABS-KEY ( “temporomandibular articular disk*” ) OR TITLE-ABS-KEY ( “condyle-disc positions” ) OR TITLE-ABS-KEY ( “condyle-disk positions” ) OR TITLE-ABS-KEY ( “condyle-disc positions” ) OR TITLE-ABS-KEY ( “mandibular condyle*” ) OR TITLE-ABS-KEY ( “condyle*, mandibular” ) OR TITLE-ABS-KEY ( “coronal condylar angles” ) OR TITLE-ABS-KEY ( “condylar spatial changes” ) OR TITLE-ABS-KEY ( condyle* ) OR TITLE-ABS-KEY ( “condylar remodeling” ) OR TITLE-ABS-KEY ( “condylar head” ) OR TITLE-ABS-KEY ( condylar ) OR TITLE-ABS-KEY ( “condylar height” ) OR TITLE-ABS-KEY ( “condyle position” ) OR TITLE-ABS-KEY ( “condylar position” ) OR TITLE-ABS-KEY ( “condylar response” ) OR TITLE-ABS-KEY ( “condylar regions” ) OR TITLE-ABS-KEY ( “coronal condylar angle” ) OR TITLE-ABS-KEY ( condyle AND disc AND position* ) OR TITLE-ABS-KEY ( “condyle-disc position*” ) OR TITLE-ABS-KEY ( “glenoid cavit*” ) OR TITLE-ABS-KEY ( “cavit*, glenoid” ) OR TITLE-ABS-KEY ( “fossa*, glenoid” ) OR TITLE-ABS-KEY ( “condyle fossa relationship*” ) OR TITLE-ABS-KEY ( “joint space*” ) OR TITLE-ABS-KEY ( “superior space” ) OR TITLE-ABS-KEY ( “posterior space” ) OR TITLE-ABS-KEY ( “articular fossa” ) OR TITLE-ABS-KEY ( “mandibular fossa depth” ) ) AND ( TITLE-ABS-KEY ( “palatal expansion technique” ) OR TITLE-ABS-KEY ( “expansion technique, palatal” ) OR TITLE-ABS-KEY ( “expansion techniques, palatal” ) OR TITLE-ABS-KEY ( “palatal expansion techniques” ) OR TITLE-ABS-KEY ( “technique, palatal expansion” ) OR TITLE-ABS-KEY ( “palatal expansion technic” ) OR TITLE-ABS-KEY ( “expansion technic, palatal” ) OR TITLE-ABS-KEY ( “expansion technics, palatal” ) OR TITLE-ABS-KEY ( “expansion technics, palatal” ) OR TITLE-ABS-KEY ( “technic, palatal expansion” ) OR TITLE-ABS-KEY ( “maxillary expansion” ) OR TITLE-ABS-KEY ( “expansion, maxillary” ) OR TITLE-ABS-KEY ( rme ) OR TITLE-ABS-KEY ( “rapid maxillary expansion” ) OR TITLE-ABS-KEY ( “rapid palatal expansion” ) OR TITLE-ABS-KEY ( “palatal disjunction” ) OR TITLE-ABS-KEY ( “rapid palatal expander” ) OR TITLE-ABS-KEY ( “hass appliance” ) OR TITLE-ABS-KEY ( “hass expander” ) OR TITLE-ABS-KEY ( “hass expander” ) OR TITLE-ABS-KEY ( “modified hass appliance” ) OR TITLE-ABS-KEY ( “hirax appliance” ) OR TITLE-ABS-KEY ( “hyrax appliance” ) OR TITLE-ABS-KEY ( “hyrax expander” ) OR TITLE-ABS-KEY ( “hirax expander” ) OR TITLE-ABS-KEY ( “modified hirax appliance” ) OR TITLE-ABS-KEY ( “bonded expander” ) OR TITLE-ABS-KEY ( “bonded rapid maxillary expander” ) OR TITLE-ABS-KEY ( “haas-type orthopedic appliance” ) OR TITLE-ABS-KEY ( “haas-type orthopedic appliances” ) OR TITLE-ABS-KEY ( “haas-type expansion appliance” ) OR TITLE-ABS-KEY ( “haas- type expansion appliances” ) OR TITLE-ABS-KEY ( “tooth borne expander” ) OR TITLE-ABS-KEY ( “mcnamara appliance” ) OR TITLE-ABS-KEY ( “mcnamara expander” ) OR TITLE-ABS-KEY ( “mcnamara expander” ) OR TITLE-ABS-KEY ( “rapid midpalatal suture opening” ) OR TITLE-ABS-KEY ( “rapid midpalatal suture disjunction” ) OR TITLE-ABS-KEY ( “opening the midpalatal suture” ) OR TITLE-ABS-KEY ( “maxillary orthopedic expansion” ) OR TITLE-ABS-KEY ( “orthopedic maxillary expansion” ) ) |
| WEB OF SCIENCE | #1: Tópico: (child OR children OR kid OR kids OR boy OR boys OR girl OR girls OR adolescent OR adolescents OR adolescence OR teens OR teen OR teenagers OR teenager OR youth OR youths OR “adolescents, female” OR “adolescent, female” OR “female adolescent” OR “female adolescents” OR “adolescents, male” OR “adolescents, male” OR “male adolescente” OR “male adolescents” OR young OR “temporomandibular joint” OR “joint, temporomandibular” OR “joints, temporomandibular” OR “temporomandibular joints” OR tmj OR “temporomandibular joint disc” OR “temporomandibular joint disc” OR “discs, temporomandibular joint” OR “joint disc, temporomandibular” OR “joint discs, temporomandibular” OR “temporomandibular joint discs” OR “disk, temporomandibular joint” OR “disk, temporomandibular joint” OR “articular discs, temporomandibular” OR “disc, temporomandibular articular” OR “discs, temporomandibular articular” OR “temporomandibular articular disc” OR “temporomandibular articular discs” OR “articular disk, temporomandibular” OR “articular disks, temporomandibular” OR “disk, temporomandibular articular” OR “disk, temporomandibular articular” OR “temporomandibular articular disk” OR “temporomandibular articular disks” OR “temporomandibular joint disk” OR “disks, temporomandibular joint” OR “disks, temporomandibular joint” OR “joint disks, temporomandibular” OR “joint disks, temporomandibular” OR “condyle-disc positions” OR “articular disc position” OR “articular disc positions” OR “mandibular condyle” OR “condyle, mandibular” OR “condyles, mandibular” OR “mandibular condyles” OR “coronal condylar angles” OR “condylar spatial changes” OR condyle OR condyles OR “condylar remodeling” OR “condylar remodeling” OR “condylar head” OR condylar OR “condylar height” OR “condyle position” OR “condylar position” OR “condylar response” OR “condylar regions” OR “coronal condylar angle” OR “condyle disc position” OR “condyle disc positions” OR “condyle-disc position” OR “condyle-disc positions” OR “glenoid cavity” OR “cavities, glenoid” OR “cavity, glenoid” OR “cavity, glenoid” OR “glenoid fossa” OR “fossa, glenoid” OR “fossas, glenoid” OR “condyle fossa relationship” OR “condyle fossa relationships” OR “joint spaces” OR “anterior space” OR “superior space” OR “posterior space” OR “joint space” OR “joint spaces”“glenoid fossa” Or “articular fossa” OR “mandibular fossa depth”) #2: Tópico: (“palatal expansion technique” OR “expansion technique, palatal” OR “expansion techniques, palatal” OR “palatal expansion techniques” OR “technique, palatal expansion” OR “palatal expansion technic” OR “expansion technic, palatal” OR “expansion technics, palatal” OR “expansion technics, palatal” OR “technic, palatal expansion” OR “maxillary expansion” OR “expansion, maxillary” OR rme OR “rapid maxillary expansion” OR “rapid palatal expansion” OR “palatal disjunction” OR “rapid palatal expander” OR “hass appliance” OR “hass expander” OR “modified hass appliance” OR “modified hass appliance” OR “hirax appliance” OR “hyrax appliance” OR “hyrax expander” OR “hirax expander” OR “modified hirax appliance” OR “bonded expander” OR “bonded rapid maxillary expander” OR “haas-type orthopedic appliance” OR “haas-type orthopedic appliances” OR “haas-type expansion appliance” OR “haas- type expansion appliances” OR “tooth borne expander” OR “mcnamara appliance” OR “mcnamara expander” OR “mcnamara expander” OR “rapid midpalatal suture opening” OR “rapid midpalatal suture disjunction” OR “opening the midpalatal suture” OR “maxillary orthopedic expansion” OR “orthopedic maxillary expansion”) #1 AND #2 |
| COCHRANE $ | #1: MeSH descriptor: [Child] this term only #2: child or children or kid or kids or boy or boys or girl or girls:ti,ab,kw (Word variations have been searched) #3: MeSH descriptor: [Adolescent] this term only #4: adolescent or adolescents or adolescence or teens or teen or teenagers or teenager or youth or youths or “adolescents, female” or “adolescent, female” or “female adolescent” or “female adolescents” or “adolescents, male” or “adolescents, male” or “male adolescente” or “male adolescents” or young:ti,ab,kw (Word variations have been searched) #5: MeSH descriptor: [Temporomandibular Joint] this term only #6: “temporomandibular joint” or “joint, temporomandibular” or “joints, temporomandibular” or “temporomandibular joints” or tmj:ti,ab,kw (Word variations have been searched) #7: MeSH descriptor: [Temporomandibular Joint Disc] this term only #8: “temporomandibular joint disc” or “temporomandibular joint disc” or “discs, temporomandibular joint” or “joint disc, temporomandibular” or “joint discs, temporomandibular” or “temporomandibular joint discs” or “disk, temporomandibular joint” or “disk, temporomandibular joint” or “articular discs, temporomandibular” or “disc, temporomandibular articular” or “discs, temporomandibular articular” or “temporomandibular articular disc” or “temporomandibular articular discs” or “articular disk, temporomandibular” or “articular disks, temporomandibular” or “disk, temporomandibular articular” or “disk, temporomandibular articular” or “temporomandibular articular disk” or “temporomandibular articular disks” or “temporomandibular joint disk” or “disks, temporomandibular joint” or “disks, temporomandibular joint” or “joint disks, temporomandibular” or “joint disks, temporomandibular” or “condyle-disc positions” or “articular disc position” or “articular disc positions”:ti,ab,kw (Word variations have been searched) #9: MeSH descriptor: [Mandibular Condyle] this term only #10: “mandibular condyle” or “condyle, mandibular” or “condyles, mandibular” or “mandibular condyles” or “coronal condylar angles” or “condylar spatial changes” or condyle or condyles or “condylar remodeling” or “condylar remodeling” or “condylar head” or condylar or “condylar height” or “condyle position” or “condylar position” or “condylar response” or “condylar regions” or “coronal condylar angle” or “condyle disc position” or “condyle disc positions” or “condyle-disc position” or “condyle-disc positions”:ti,ab,kw (Word variations have been searched) #11: MeSH descriptor: [Glenoid Cavity] this term only #12: “glenoid cavity” or “cavities, glenoid” or “cavity, glenoid” or “cavity, glenoid” or “glenoid fossa” or “fossa, glenoid” or “fossas, glenoid” or “condyle fossa relationship” or “condyle fossa relationships” or “joint spaces” or “anterior space” or “superior space” or “posterior space” or “joint space” or “joint spaces” “glenoid fossa” or “articular fossa” or “mandibular fossa depth”:ti,ab,kw (Word variations have been searched) #13: #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 #14: MeSH descriptor: [Palatal Expansion Technique] this term only #15: “palatal expansion technique” or “expansion technique, palatal” or “expansion techniques, palatal” or “palatal expansion techniques” or “technique, palatal expansion” or “palatal expansion technic” or “expansion technic, palatal” or “expansion technics, palatal” or “expansion technics, palatal” or “technic, palatal expansion” or “maxillary expansion” or “expansion, maxillary” or rme or “rapid maxillary expansion” or “rapid palatal expansion” or “palatal disjunction” or “rapid palatal expander” or “hass appliance” or “hass expander” or “modified hass appliance” or “modified hass appliance” or “hirax appliance” or “hyrax appliance” or “hyrax expander” or “hirax expander” or “modified hirax appliance” or “bonded expander” or “bonded rapid maxillary expander” or “haas-type orthopedic appliance” or “haas-type orthopedic appliances” or “haas-type expansion appliance” or “haas- type expansion appliances” or “tooth borne expander” or “mcnamara appliance” or “mcnamara expander” or “mcnamara expander” or “rapid midpalatal suture opening” or “rapid midpalatal suture disjunction” or “opening the midpalatal suture” or “maxillary orthopedic expansion” or “orthopedic maxillary expansion”:ti,ab,kw (Word variations have been searched) #16: #14 or #15 #17: #13 and #16 |
| LILACS $ | (tw:((mh:(child)) OR (tw:(child OR children OR kid OR kids OR boy OR boys OR girl OR girls)) OR (mh:(adolescent)) OR (tw:(adolescent OR adolescents OR adolescence OR teens OR teen OR teenagers OR teenager OR youth OR youths OR “adolescents, female” OR “adolescent, female” OR “female adolescent” OR “female adolescents” OR “adolescents, male” OR “adolescents, male” OR “male adolescente” OR “male adolescents” OR young)) OR (mh:(“temporomandibular joint” )) OR (tw:(“temporomandibular joint” OR “joint, temporomandibular” OR “joints, temporomandibular” OR “temporomandibular joints” OR tmj)) OR (mh:(“temporomandibular joint disc” )) OR (tw:(“temporomandibular joint disc” OR “temporomandibular joint disc” OR “discs, temporomandibular joint” OR “joint disc, temporomandibular” OR “joint discs, temporomandibular” OR “temporomandibular joint discs” OR “disk, temporomandibular joint” OR “disk, temporomandibular joint” OR “articular discs, temporomandibular” OR “disc, temporomandibular articular” OR “discs, temporomandibular articular” OR “temporomandibular articular disc” OR “temporomandibular articular discs” OR “articular disk, temporomandibular” OR “articular disks, temporomandibular” OR “disk, temporomandibular articular” OR “disk, temporomandibular articular” OR “temporomandibular articular disk” OR “temporomandibular articular disks” OR “temporomandibular joint disk” OR “disks, temporomandibular joint” OR “disks, temporomandibular joint” OR “joint disks, temporomandibular” OR “joint disks, temporomandibular” OR “condyle-disc positions” OR “articular disc position” OR “articular disc positions”)) OR (mh:(“mandibular condyle” )) OR (tw:(“mandibular condyle” OR “condyle, mandibular” OR “condyles, mandibular” OR “mandibular condyles” OR “coronal condylar angles” OR “condylar spatial changes” OR condyle OR condyles OR “condylar remodeling” OR “condylar remodeling” OR “condylar head” OR condylar OR “condylar height” OR “condyle position” OR “condylar position” OR “condylar response” OR “condylar regions” OR “coronal condylar angle” OR “condyle disc position” OR “condyle disc positions” OR “condyle-disc position” OR “condyle-disc positions”)) OR (mh:(“glenoid cavity” )) OR (tw:(“glenoid cavity” OR “cavities, glenoid” OR “cavity, glenoid” OR “cavity, glenoid” OR “glenoid fossa” OR “fossa, glenoid” OR “fossas, glenoid” OR “condyle fossa relationship” OR “condyle fossa relationships” OR “joint spaces” OR “anterior space” OR “superior space” OR “posterior space” OR “joint space” OR “joint spaces”“glenoid fossa” Or “articular fossa” OR “mandibular fossa depth”)))) AND (tw:((mh:(“palatal expansion technique”)) OR (tw:(“palatal expansion technique”)) OR (tw:(“palatal expansion techniques”)) OR (tw:(“rapid maxillary expansion”)) OR (tw:(rme)) OR (tw:(“rapid palatal expansion”)) OR (tw:(“rapid palatal disjunction”)) OR (tw:(“rapid maxillary disjunction”)) OR (tw:(“midpalatal suture opening”)) OR (tw:(“midpalatal suture disjunction”)) OR (tw:(haas)) OR (tw:(hass)) OR (tw:(hirax)) OR (tw:(hyrax)) OR (tw:(mcnamara)))) |
| SCIENCE DIRECT * | (((child* OR adolescent OR teen* OR youth* OR temporomandibular joint* OR temporomandibular joint disc* OR mandibular condyle* OR tmj OR temporomandibular articular disc* OR “glenoid cavity”)) AND (palatal expansion technique* OR rapid maxillary expansion* OR rme OR palatal disjunction* OR midpalatal suture opening* OR hass OR hirax OR hyrax OR mcnamara OR “orthopedic maxillary expansion”)) in title , abstract and keywords of research articles |
| OPENGREY | “Temporomandibular Joint” AND “Rapid Maxillary Expansion” “Temporomandibular Joint” AND “Palatal Expansion Technique” |
| GOOGLE SCHOLAR | “temporomandibular joint”+”rapid maxillary expansion” -”case report” -”review” |
| CLINICALTRIALS | Temporomandibular Joint + Rapid Maxillary Expansion |
REFERENCES
- 1. .McNamara JA. Maxillary transverse deficiency. Am J Orthod Dentofacial Orthop. 2000;117;:567–570. doi: 10.1016/s0889-5406(00)70202-2. [DOI] [PubMed] [Google Scholar]
- 2. .McNamara JA, Brudon WL. Orthodontics and Dentofacial Orthopedics. Ann Arbor, MI: Needham Press; 2001. pp. 97–110. [Google Scholar]
- 3. .Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the midpalatal suture. Angle Orthod. 1961;31:73–90. [Google Scholar]
- 4. .Lima Filho RM, Ruellas AC. Long-term anteroposterior and vertical maxillary changes in skeletal Class II patients treated with slow and rapid maxillary expansion. Angle Orthod. 2007;77:870–874. doi: 10.2319/071406-293.1. [DOI] [PubMed] [Google Scholar]
- 5. .Doruk C, Bicakci AA, Basciftci FA, Agar U, Babacan H. A comparison of the effects of rapid maxillary expansion and fan-type rapid maxillary expansion on dentofacial structures. Angle Orthod. 2004;74:184–194. doi: 10.1043/0003-3219(2004)074<0184:ACOTEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6. .Garcia MM, Machado KFS, Mascarenhas MH. Magnetic resonance imaging and computed tomography of the temporomandibular joint: beyond dysfunction. Radiol Bras. 2008;41:337–342. [Google Scholar]
- 7. .Ellabban MT, Abdul-Aziz AI, Salah Fayed MM, AboulFotouh MH, Elkattan ES, Dahaba MM. Positional and dimensional temporomandibular joint changes after correction of posterior crossbite in growing patients: a systematic review. Angle Orthod. 2018;88:638–648. doi: 10.2319/110217-749.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. .Lam PH, Sadowsky C, Omerza F. Mandibular asymmetry and condylar position in children with unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1999. pp. 569–575. [DOI] [PubMed]
- 9. .Santamaría-Villegas A, Manrique-Hernandez R, Alvarez-Varela E, Restrepo-Serna C. Effect of removable functional appliances on mandibular length in patients with Class II with retrognathism: systematic review and meta-analysis. BMC Oral Health. 2017;17:52. doi: 10.1186/s12903-017-0339-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. .Klatkiewicz T, Gawriołek K, Radzikowska MP, Czajka-Jakubowska A. ultrasonography in the diagnosis of temporomandibular disorders: a meta-analysis. Med Sci Monit. 2018;24:812–817. doi: 10.12659/MSM.908810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. .Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analy-sis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. .Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. (eds) Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011. Available at: http://handbook.cochrane.org.
- 13. .National Heart, Lung, and Blood Institute (NHLBI) - Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group. 2018 Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools Accessed October 14.
- 14. .Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for Grading the Quality of Evidence and the Strength of Recommendations using the GRADE Approach. 2019 GRADE Working Group; 2013. Available at: https://gdt.gradepro.org/app/handbook/handbook.html Accessed May 22.
- 15. .Ghoussoub MS, Rifai K, Garcia R, Sleilaty G. Effect of rapid maxillary expansion on glenoid fossa and condyle-fossa relationship in growing patients (MEGP): study protocol for a controlled clinical trial. J Int Soc Prev Community Dent. 2018;8:130–136. doi: 10.4103/jispcd.JISPCD_458_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. .Illipronti filho E, de Fantini SM, de Paiva JB. Condylar positional changes with unilateral posterior crossbite, before and after rapid maxillary expansion [in Italian] Revista Clínica de Ortodontia Dental Press. 2012;11:46–52. [Google Scholar]
- 17. .Pinto AS, Buschang PH, Throckmorton GS, Chen P. Morphological and positional asymmetries of young children with functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 2001;120:513–520. doi: 10.1067/mod.2001.118627a. [DOI] [PubMed] [Google Scholar]
- 18. .Coskuner HG, Ciger S. Three-dimensional assessment of the temporomandibular joint and mandibular dimensions after early correction of the maxillary arch form in patients with Class II division 1 or division 2 malocclusion. Korean J Orthod. 2015;45:121–112. doi: 10.4041/kjod.2015.45.3.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. .Hesse KL, Artun J, Joondeph DR, Kennedy DB. Changes in condylar position and occlusion associated with maxillary expansion for correction of functional unilateral posterior crossbite. Am J Orthod Dentofacial Orthop. 1997;111:410–418. doi: 10.1016/s0889-5406(97)80023-6. [DOI] [PubMed] [Google Scholar]
- 20. .Lippold G, Hoppe G, Moiseenko T, Ehmer U, Danesh G. Analysis of condylar differences in functional unilateral posterior crossbite during early treatment – a randomized clinical study. J Orofac Orthop. 2008;69:283–296. doi: 10.1007/s00056-008-0803-9. [DOI] [PubMed] [Google Scholar]
- 21. .Nerder PH, Bakke M, Solow B. The functional shift of the mandible in unilateral posterior crossbite and the adaptation of the temporomandibular joints: a pilot study. Eur J Orthod. 1999;21:155–166. doi: 10.1093/ejo/21.2.155. [DOI] [PubMed] [Google Scholar]
- 22. .Arat FE, Arat ZM, Tompson B, Tanju S, Erdene I. Muscular and condylar response to rapid maxillary expansion. Part 2: Magnetic resonance imaging study of the temporomandibular joint. Am J Orthod Dentofacial Orthop. 2008;133:823–829. doi: 10.1016/j.ajodo.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 23. .Arat FE, Arat ZM, Tompson B, Tanju S, Erdene I. Muscular and condylar response to rapid maxillary expansion. Part 3: magnetic resonance assessment of condyle-disc relationship. Am J Orthod Dentofacial Orthop. 2008;133:830–836. doi: 10.1016/j.ajodo.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 24. .Masi M, Lederman HM, Yamashita HK, de Arruda Aidar LA. Temporomandibular joint evaluation with magnetic resonance imaging in children with functional unilateral posterior crossbite, treated with rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2009;136:207–217. doi: 10.1016/j.ajodo.2007.10.048. [DOI] [PubMed] [Google Scholar]
- 25. .Matta ENR, Sousa MMG, Sant'anna EF, Silvia SC. Evaluation with helicoidal computed tomography of rapid maxillary expansion effects in the condylar position of patients with functional posterior crossbite [in Portuguese) R Dental Press Ortodon Ortop Facial Maringá. 2009;14:161–169. [Google Scholar]
- 26. .Leonardi R, Caltabiano M, Cavallini C, et al. Condyle fossa relationship associated with functional posterior crossbite, before and after rapidmaxillary expansion. Angle Orthod. 2012;82:1040–1046. doi: 10.2319/112211-725.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. .Melgaço CA, Columbano Neto J, Jurach EM, Nojima Mda C, Nojima LI. Immediate changes in condylar position after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2014;145:771–779. doi: 10.1016/j.ajodo.2014.01.024. [DOI] [PubMed] [Google Scholar]
- 28. .McLeod L, Hernández IA, Heo G, Lagravère MO. Condylar positional changes in rapid maxillary expansion assessed with cone-beam computertomography. Int Orthod. 2016;14:342–356. doi: 10.1016/j.ortho.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 29. .Ghoussoub MS, Garcia R, Sleilaty G, Rifai K. Effect of rapid maxillary expansion on condyle-fossa relationship in growing patients. J Contemp Dent Pract. 2018;19:1189–1198. [PubMed] [Google Scholar]
- 30. .Lisboa CO, Martins MM, Ruellas ACO, Ferreira DMTP, Maia LC, Mattos CT. Soft tissue assessment before and after mandibular advancement or setback surgery using three-dimensional images: systematic review and meta-analysis. Int J OralMaxillofac Surg. 2018;47:1387–1397. doi: 10.1016/j.ijom.2018.05.022. [DOI] [PubMed] [Google Scholar]
- 31. .Feres MF, Raza H, Alhadlaq A, El-Bialy T. Rapid maxillary expansion effects in Class II malocclusion: a systematic review. Angle Orthod. 2015;85:1070–1079. doi: 10.2319/102514-768.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. .Normando D, Tjäderhane L, Quintão CCA. A. PowerPoint-based guide to assist in choosing the suitable statistical test. Dental Press J Orthod. 2010;15:101–106. [Google Scholar]
- 33. .Kasimoglu Y, Tuna EB, Rahimi B, Marsan G, Gencay K. Condylar asymmetry in different occlusion types. Cranio. 2014;33:10–14. doi: 10.1179/0886963414Z.00000000039. [DOI] [PubMed] [Google Scholar]
- 34. .Wadhawan N, Kumar S, Kharbanda OP, Duggal R, Sharma R. Temporomandibular joint adaptations following two-phase therapy: an MRI study. Orthod Craniofac Res. 2008;11:235–250. doi: 10.1111/j.1601-6343.2008.00436.x. [DOI] [PubMed] [Google Scholar]
- 35. .Kinzinger GS, Roth A, Gulden N, Bücker A, Diedrich PR. Effects of orthodontic treatment with fixed functional orthopaedic appliances on the disccondyle relationship in the temporomandibular joint: a magnetic resonance imaging study (Part II) Dentomaxillofac Radiol. 2006;35:347–356. doi: 10.1259/dmfr/70972585. [DOI] [PubMed] [Google Scholar]
- 36. .Lagravére MO, Heo G, Major PW, Flores-Mir C. Meta–analysis of immediate changes with rapid maxillary expansion treatment. J Am Dent Assoc. 2006;137:44–53. doi: 10.14219/jada.archive.2006.0020. [DOI] [PubMed] [Google Scholar]
- 37. .Garib DG, Henriques JF, Carvalho PE, Gomes SC. Longitudinal effects of rapid maxillary expansion. Angle Orthod. 2007;77:442–448. doi: 10.2319/0003-3219(2007)077[0442:LEORME]2.0.CO;2. [DOI] [PubMed] [Google Scholar]


