Anthony A Amato
Anthony A Amato, MD
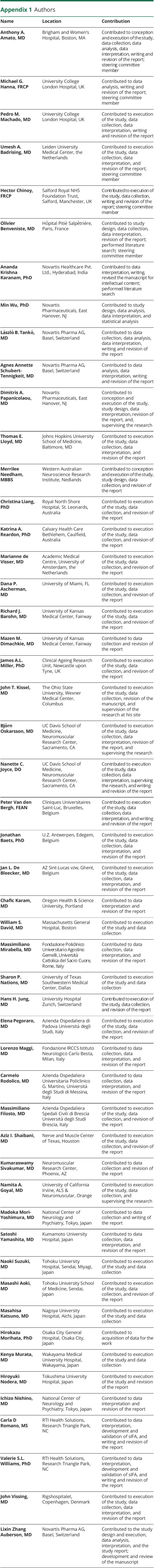
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,✉,
Michael G Hanna
Michael G Hanna, FRCP
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Pedro M Machado
Pedro M Machado, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Umesh A Badrising
Umesh A Badrising, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Hector Chinoy
Hector Chinoy, FRCP
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Olivier Benveniste
Olivier Benveniste, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Ananda Krishna Karanam
Ananda Krishna Karanam, PhD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Min Wu
Min Wu, PhD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
László B Tankó
László B Tankó, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Agnes Annette Schubert-Tennigkeit
Agnes Annette Schubert-Tennigkeit, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Dimitris A Papanicolaou
Dimitris A Papanicolaou, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Thomas E Lloyd
Thomas E Lloyd, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Merrilee Needham
Merrilee Needham, MBBS
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Christina Liang
Christina Liang, PhD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Katrina A Reardon
Katrina A Reardon, PhD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Marianne de Visser
Marianne de Visser, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Dana P Ascherman
Dana P Ascherman, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Richard J Barohn
Richard J Barohn, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Mazen M Dimachkie
Mazen M Dimachkie, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
James AL Miller
James AL Miller, PhD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
John T Kissel
John T Kissel, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Björn Oskarsson
Björn Oskarsson, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Nanette C Joyce
Nanette C Joyce, DO
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Peter Van den Bergh
Peter Van den Bergh, FEAN
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Jonathan Baets
Jonathan Baets, PhD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Jan L De Bleecker
Jan L De Bleecker, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Chafic Karam
Chafic Karam, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
William S David
William S David, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Massimiliano Mirabella
Massimiliano Mirabella, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Sharon P Nations
Sharon P Nations, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Hans H Jung
Hans H Jung, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Elena Pegoraro
Elena Pegoraro, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Lorenzo Maggi
Lorenzo Maggi, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Carmelo Rodolico
Carmelo Rodolico, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Massimiliano Filosto
Massimiliano Filosto, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Aziz I Shaibani
Aziz I Shaibani, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Kumaraswamy Sivakumar
Kumaraswamy Sivakumar, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Namita A Goyal
Namita A Goyal, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Madoka Mori-Yoshimura
Madoka Mori-Yoshimura, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Satoshi Yamashita
Satoshi Yamashita, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Naoki Suzuki
Naoki Suzuki, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Masashi Aoki
Masashi Aoki, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Masahisa Katsuno
Masahisa Katsuno, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Hirokazu Morihata
Hirokazu Morihata, PhD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Kenya Murata
Kenya Murata, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Hiroyuki Nodera
Hiroyuki Nodera, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Ichizo Nishino
Ichizo Nishino, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Carla D Romano
Carla D Romano, MS
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Valerie SL Williams
Valerie SL Williams, PhD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
John Vissing
John Vissing, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1,
Lixin Zhang Auberson
Lixin Zhang Auberson, MD
1From the Department of Neurology (A.A.A.), Brigham and Women's Hospital and Harvard Medical School, Boston, MA; Medical Research Council Centre for Neuromuscular Diseases (M.G.H., P.M.M.) and Institute of Neurology, Department of Neuromuscular Diseases & Centre for Rheumatology (P.M.M.), University College London; Department of Rheumatology & Queen Square Centre for Neuromuscular Diseases (P.M.M.), University College London Hospitals NHS Foundation Trust; Department of Rheumatology (P.M.M.), Northwick Park Hospital, London North West University Healthcare NHS Trust, UK; Department of Neurology (U.A.B.), Leiden University Medical Center, Netherlands; National Institute for Health Research Manchester Biomedical Research Centre (H.C.), Manchester University NHS Foundation Trust, Manchester Academic Health Science Centre, The University of Manchester, UK; Department of Internal Medicine and Clinical Immunology (O.B.), Pitié-Salpêtrière Hospital, Sorbonne Université, Paris, France; Novartis Healthcare Pvt. Ltd. (K.A.K), Hyderabad, India; Novartis Pharmaceuticals (M.W., D.A.P.), East Hanover, NJ; Novartis Pharma AG (L.B.T., A.A.S-T.), Basel, Switzerland; Department of Neurology (T.E.L.), The Johns Hopkins University School of Medicine, Baltimore, MD; Institute for Immunology & Infectious Diseases (M.N.), Fiona Stanley Hospital, Murdoch University and Notre Dame University, Perth; Department of Neurology (C.L.), Royal North Shore Hospital, New South Wales; Calvary Health Care Bethlehem (K.A.R.), Caulfield South, Australia; Department of Neurology (M.d.V), Amsterdam University Medical Centre, the Netherlands; Department of Medicine (D.P.A.), University of Miami, FL; Department of Neurology (R.J.B., M.M.D.), University of Kansas Medical Center, Kansas City; Department of Neurology (J.A.L.M.), Newcastle upon Tyne Hospitals NHS Foundation Trust, UK; Department of Neurology (J.T.K.), The Ohio State University Wexner Medical Center, Columbus; Neuromuscular Research Center (B.O., N.C.J.), UC Davis School of Medicine, Sacramento, CA; Department of Neurology (P.V.d.B.), University Hospital Saint-Luc, University of Louvain, Brussels; Neuromuscular Reference Centre, Department of Neurology (J.B.), Antwerp University Hospital; Institute Born-Bunge (J.B.), University of Antwerp; Department of Neurology (J.L.d.B.), Ghent University Hospital, Belgium; Department of Neurology (C.K.), Oregon Health & Science University, Portland; Department of Neurology (W.S.D.), Massachusetts General Hospital, Neuromuscular Diagnostic Center and Electromyography Laboratory, Boston; Department of Neurology (M.M.), Fondazione Policlinico Universitario Agostino Gemelli IRCCS; Università Cattolica del Sacro Cuore (M.M.), Rome, Italy; Department of Neurology (S.P.N.), University of Texas Southwestern Medical Center, Dallas; Department of Neurology (H.H.J.), University Hospital and University of Zurich, Switzerland; Department of Neurosciences (E.P.), University of Padova School of Medicine; Fondazione IRCCS Istituto Neurologico Carlo Besta (L.M.), Milan; Unit of Neurology and Neuromuscular Disorders (C.R.), Azienda Ospedaliera Universitaria Policlinico G Martino, University of Messina; Center for Neuromuscular Diseases (M.F.), Unit of Neurology, ASST Spedali Civili and University of Brescia, Italy; Nerve and Muscle Center of Texas (A.I.S.), Houston; Neuromuscular Research Center (K.S.), Phoenix, AZ; Department of Neurology (N.A.G.), ALS & Neuromuscular Center, University of California Irvine, Orange; Department of Neurology (M.M.-Y.), National Center Hospital, National Center of Neurology and Psychiatry, Tokyo; Department of Neurology (S.Y.), Kumamoto University Hospital; Department of Neurology (N.S.), Tohoku University Hospital, Miyagi; Department of Neurology (M.A.), Tohoku University School of Medicine, Sendai; Department of Neurology (M.K.), Nagoya University Hospital, Aichi; Department of Neurology (H.M.), Osaka City General Hospital; Wakayama Medical University Hospital (K.M.); Tokushima University Hospital (H.N.); Department of Neuromuscular Research (I.N.), National Institute of Neuroscience, National Center of Neurology and Psychiatry, Tokyo, Japan; RTI Health Solutions (C.D.R., V.S.L.W.), Research Triangle Park, NC; Copenhagen Neuromuscular Center (J.V.), Rigshospitalet, University of Copenhagen, Denmark; and UCB (L.Z.A.), Bulle, Switzerland. H.N. is currently affiliated with the Department of Neurology, Kanazawa Medical University, Ishikawa, Japan. B.O. is currently affiliated with the Department of Neurology, Mayo Clinic, Jacksonville, FL.
1;
on behalf of the RESILIENT Study Extension Group1