Abstract
Objective
To evaluate the hypothesis that individuals with isolated dystonia are at an increased risk for suicidal behavior, we administered an anonymous electronic survey to patients with dystonia, asking them about their history of suicidal ideations and suicide attempt.
Methods
A total of 542 patients with dystonia completed an online 97-question survey, which captured the demographics of suicidal behavior and major psychiatric disorders. Statistical analyses examined the prevalence of suicidal behavior in patients with dystonia compared to the prevalence of suicidal ideations and attempt in the general global population and assessed the significance of risk associations between suicidality and psychiatric history in these patients.
Results
Overall, 32.3% of patients with isolated dystonia reported a lifetime history of suicidal behavior, which was significantly different from the reported rates of suicidal ideation (9.2%) and attempt (2.7%) in the general global population. The prevalence of suicidality was higher in patients with multifocal/segmental and generalized forms of dystonia (range of 46%–50%) compared to patients with focal dystonias (range of 26.1%–33.3%). The highest suicidal ideation-to-attempt ratio of 4:1 was found in patients with generalized dystonia. Suicidality in patients with focal dystonia was significantly associated with history of depression and anxiety disorders.
Conclusion
Patients with isolated dystonia have an increased, albeit unrecognized, prevalence of suicidal behavior compared to the general global population. Screening for suicidal risk should be incorporated as part of the clinical evaluation of patients with dystonia to prevent their suicide-induced injury and death.
Isolated dystonia is the third most prevalent movement disorder after essential tremor and Parkinson disease, affecting 3–30 per 100,000 in the general population.1–3 Several studies have determined that, in addition to debilitating motor symptoms, up to 90% of patients with dystonia have comorbid psychiatric disorders, most frequently including generalized or social anxiety, obsessive-compulsive disorder, and major depression.4–10 These psychiatric conditions are consistently found to be among the most significant risk factors for suicide,11 which is a leading cause of death worldwide.12 However, the incidence of suicidal ideations and behavior in patients with dystonia, especially those prone to psychiatric comorbidities, is unknown. Given the stigma surrounding suicidality and the tendency of a suicidal individual to avoid clinical interventions,13 we hypothesized that suicidal behavior in patients with dystonia might have remained undisclosed during routine neurologic evaluations, further increasing the risk of suicide in these patients. We conducted an anonymous electronic survey study that investigated the demographics and prevalence of suicidality and its relationship with co-occurring psychiatric disorders in a large cohort of 542 patients with different forms of isolated dystonia.
Methods
Study Participants and Data Collection
Study participants were recruited from our database of 613 patients with isolated dystonia, as well as the international patient registries of the Dystonia Research Medical Foundation and the National Spasmodic Dysphonia Association. The potential participants received an email invitation to complete the online survey, which was administered using Research Electronic Data Capture (REDCap)14,15 hosted at Mass General Brigham. REDCap is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to standard statistical packages; and (4) procedures for data integration and interoperability with external sources. The survey was active for online completion for 8 weeks.
The survey included 97 questions, which were asked in lay English and developed by the authors of this study based on the previously used questionnaire16 and Columbia–Suicide Severity Rating Scale (C-SSRS)17 (table 1). In addition, general demographics (age, sex, level of education), information about dystonia diagnosis, symptomatology and treatment, past and present psychiatric history (generalized and social anxiety, panic disorder, attention-deficit/hyperactivity disorder, major and bipolar depression, substance use disorder, and schizophrenia) were obtained. Six members of the laboratory mock-completed the survey to cross-check its content and format before its actual administration. All survey entries were confidential, with the identity of the participant being fully blinded to the investigators. All survey entries were checked for response completeness.
Table 1.
Research Electronic Data Capture (REDCap) Online Survey Questionnaire
A total of 3,138 individuals opened the survey link, and a total of 580 individuals (18.5%) participated in the survey. Among these, 10 participants responded to fewer than 75% of questions, and 28 participants listed a diagnosis other than isolated dystonia (e.g., essential tremor, secondary dystonia, myoclonus dystonia, muscle tension dysphonia, dopamine-responsive dystonia) or stated that their diagnosis of dystonia was not confirmed by a physician. These 38 participants (6.6%) were therefore excluded from the study. The final study cohort included a total of 542 participants (93.4% of a total participant cohort; mean age: 57.4 ± 13.3 years; 438 female/104 male) (table 2). All participants stated that their diagnosis of isolated dystonia was made by a physician. However, due to the anonymity of survey data collection, we were unable to request and review additional medical information to verify the diagnosis, which may represent a limitation of this survey study.
Table 2.
Participant Demographics
Data Analysis
All data were managed using REDCap electronic data capture tools and kept on the REDCap server hosted at Mass General Brigham.
Statistical analysis was conducted using Fisher exact tests of independence, which examined the prevalence rates of suicidal behavior in the overall study cohort and separately in each form of dystonia. Because patients with laryngeal dystonia comprised the majority of survey participants (59.4%, table 2), we analyzed their responses to the survey separate from patients with other focal dystonias to avoid data skewness within this group. The prevalence of suicidal behavior in patients with dystonia was compared to the reported rates of lifetime prevalence for suicidal ideations and suicide attempt in the general global population. Because suicidality rates differ by country,12,18 general global population rates were used as a more comprehensive and stringent measure to account for potential responses of patients located outside of the United States. In patients reporting suicidal behavior, the ratio of dystonia-induced to non–dystonia-induced suicidality and the ratio of suicidal ideations to suicide attempts were calculated. Fisher exact tests of independence were used to examine the statistical significance of associations between the psychiatric history and suicidality in the overall study cohort and within each of the dystonia forms, separately. The overall statistical threshold was set at p ≤ 0.001 (0.05/44 tests) to control for multiple comparisons.
Standard Protocol Approvals, Registrations, and Patient Consents
The study was approved by the Institutional Review Board of Mass General Brigham. Written online informed consent was obtained from all participants.
Data Availability
All data relevant to clinical and research information of the datasets used in this study are included. De-identified data and analysis pipeline may be shared upon request.
Results
Based on their clinical characteristics, 424 patients had focal dystonia (including 322 patients with laryngeal dystonia, 57 patients with cervical dystonia, 29 patients with focal hand dystonia, 11 patients with craniofacial dystonia, 4 patients with lower limb dystonia, 1 patient with abdominal/truncal dystonia), 63 patients had multifocal/segmental dystonia, 54 patients had generalized dystonia, and 1 patient had hemidystonia (table 2). The overall age at dystonia onset was 38.7 ± 13.3 years; the youngest age at onset was in patients with generalized dystonia (27.1 ± 18.0 years); the oldest age at onset was in patients with laryngeal dystonia (41.0 ± 14.6 years), which was in line with the general demographics of this disorder. The majority of patients were female, with an overall ratio of 4:1, which was also reflective of dystonia demographics. On average, 24.9% of patients reported a familial history of dystonia, ranging from 37.0% in patients with generalized dystonia to 21.4% in patients with laryngeal dystonia. As a frequent comorbidity,19–21 tremor was reported by, on average, 52.2% of patients, ranging from 74.1% in patients with generalized dystonia to 45.7% in patients with laryngeal dystonia (table 2). No significant history of other movement disorders or other neurologic conditions was reported.
Overall, 95.6% of patients reported receiving treatment for their symptoms at least once (table 2). Among these, the majority of patients (84.9%) reported receiving botulinum toxin injections. The use of oral medications (e.g., baclofen, gabapentin, clonazepam, primidone) was reported by 41.1% of patients, with the majority of patients having generalized dystonia (81.5%). Similarly, deep brain stimulation was reported mostly by patients with generalized dystonia (24.1%). Voice and speech therapy were mostly used in patients with focal laryngeal dystonia (72.1%) and patients with multifocal/segmental (41.3%) and generalized (27.8%) dystonias who had laryngeal involvement. In addition, symptom improvement following alcohol intake was reported by, on average, 49.1% of patients, with the range from 58.7% in patients with laryngeal dystonia to 33.3% in patients with other forms of focal dystonia.
Suicidality in Isolated Dystonia
The term “suicidal ideation” refers to any self-reported thoughts of engaging in suicidal behavior. “Suicide attempt” describes a failed but intentional act done by an individual to end their own life.22,23 In the general global population, the reported lifetime prevalence rate of suicidal ideations is 9.2%, and the reported rate of a suicide attempt is 2.7%.12
In the overall cohort of 542 patients, 32.3% of patients reported a lifetime history of suicidal ideations, which was significantly different from the reported rates in the general global population (Fisher exact test: odds ratio [OR] 9.8, 95% confidence interval [CI] 6.4–15.4; corrected p = 2.2e-16) (table 3). The overall rate of suicidal ideations did not vary significantly between male and female patients (28.8% in male vs 33.1% in female patients; OR 0.81, 95% CI 1.5–1.32; corrected p = 0.42).
Table 3.
Suicidality and Psychiatric History in Isolated Dystonia
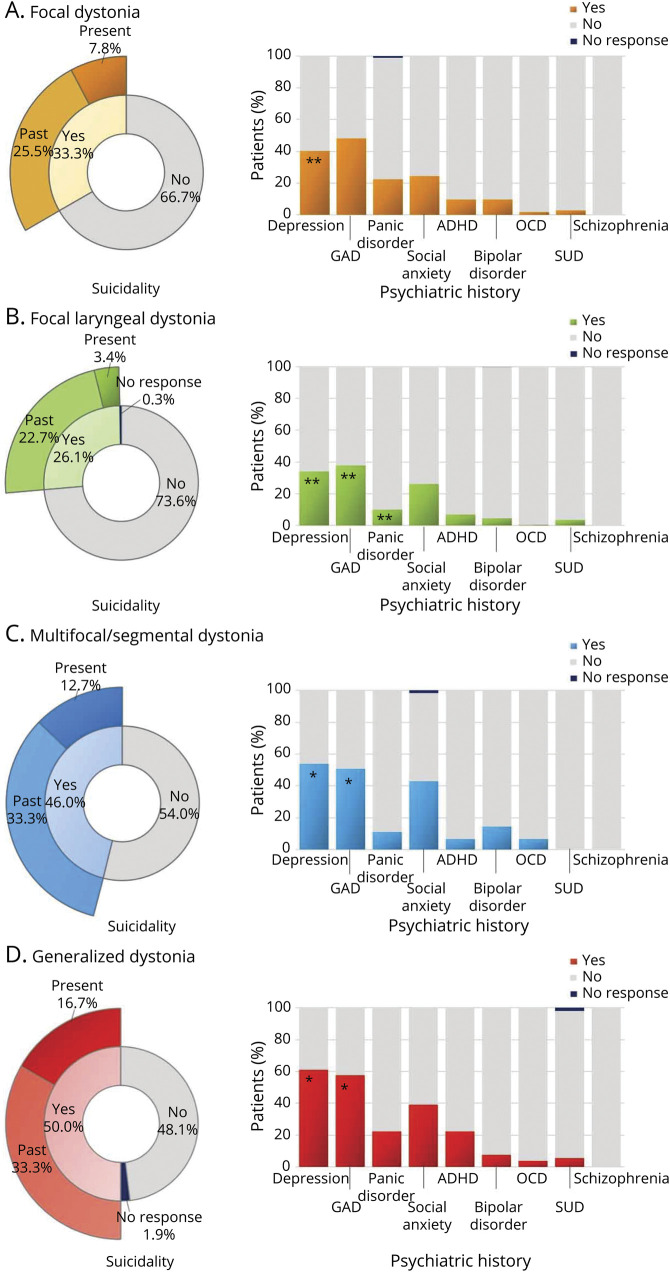
Among the different forms of dystonia, patients with generalized dystonia reported the highest incidence (50.0%) of suicidal ideations (OR 9.7, 95% CI 3.2–36.3; corrected p = 4.7e-06), followed by 46.0% in patients with multifocal/segmental dystonias (OR 8.0, 95% CI 2.9–25.9; corrected p = 6.9e-06), 33.3% in patients with focal dystonias, including cervical, focal hand, craniofacial, lower limb, abdominal/truncal forms (OR 5.1, 95% CI 2.2–13.0; corrected p = 2.5e-05), and 26.1% in patients with laryngeal dystonia (OR 3.4, 95% CI 2.2–5.6; corrected p = 2.7e-08) (figure and table 3). Overall, 1 out of 4 patients reported that their history of suicidal ideations was related to or induced by dystonia (table 3). This ratio varied across patients with different forms of dystonia, with the greatest 1:2 ratio of dystonia-induced vs non–dystonia-induced suicidality in generalized and focal dystonias (except for laryngeal dystonia), followed by 1:4 ratio in multifocal/segmental dystonia, and the lowest 1:9 ratio in laryngeal dystonia. Although the majority of patients reported having suicidal behavior in the past, the presence of suicidal ideations at the time of this study was reported by 16.7% of patients with generalized dystonia, 12.7% of patients with multifocal/segmental dystonias, 7.8% of patients with different forms of focal dystonia, and 3.4% of patients with laryngeal dystonia (figure and table 3).
Figure. Incidence of Suicidal Behavior and Psychiatric Disorders in Isolated Dystonia.
Multilevel pie charts depict the rates of suicidality and the time of occurrence (in the past or at present) in patients with (A) focal dystonia, (B) laryngeal dystonia, (C) multifocal/segmental dystonia, and (D) generalized dystonia. Corresponding stacked bar charts depict the rates of psychiatric disorders in these patients. Double asterisk marks a significant association between suicidality and psychiatric history; single asterisk marks a trend to significant association between suicidality and psychiatric history. ADHD = attention-deficit/hyperactivity disorder; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder; SUD = substance use disorder.
Among all patients with suicidal ideations, 16.6% reported having made a suicide attempt. Patients with generalized dystonia were found to have the highest incidence of a suicide attempt over their lifetime, displaying a 4:1 ideation-to-attempt ratio (table 3). The same 4:1 ideation-to-attempt ratio was seen in patients with generalized dystonia who reported their suicidal behavior was due to dystonia. Patients with laryngeal and multifocal/segmental dystonias had a lower incidence of a suicide attempt over their lifetime, which was, however, markedly increased due to dystonia (10:1 in lifetime vs 5:1 dystonia-induced in laryngeal dystonia and 5:1 in lifetime vs 4:1 dystonia-induced in multifocal/segmental dystonia). The dystonia-induced suicide attempt was lower in patients with other focal dystonias, who displayed a 4:1 ideation-to-attempt ratio over lifetime but an 8:1 ideation-to-attempt ratio specifically attributed to dystonia (table 3).
Relationship Between Suicide and Psychiatric History in Isolated Dystonia
The most frequent psychiatric disorder reported by the overall cohort of 542 patients was generalized anxiety (43.4%), followed by depression (40.4%), social anxiety (29.1%), and panic disorder (13.8%) (figure and table 3). The least common psychiatric disorders were attention-deficit/hyperactivity disorder (9.0%), obsessive-compulsive disorder (7.0%), substance abuse disorder (3.1%), and bipolar disorder (1.7%). There was no occurrence of schizophrenia reported in this patient cohort.
Suicidal ideations were significantly associated with a history of psychiatric disorders, including depression, generalized anxiety, panic disorder, and social anxiety (all p ≤ 0.0004) (figure, B and table 3). Specifically, significant relationships were established with depression in patients with all forms of focal dystonia (all p ≤ 1.4e-05). At the same time, trends to significance were observed in patients with multifocal/segmental and generalized dystonias (all p = 0.002). Generalized anxiety had a significant relationship with suicidality in patients with laryngeal dystonia (p ≤ 1.3e-05), with trends to significance in patients with multifocal/segmental and generalized dystonias (all p = 0.002). Panic disorder was significantly associated with suicidality in patients with laryngeal dystonia (p = 0.001) but not in other forms of dystonia (all p ≥ 0.04). Finally, social anxiety showed a significant relationship with suicidal behavior in the overall group of patients with dystonia (p = 0.0004) but was not significant when examining different forms of dystonia, separately (all p ≥ 0.03).
Discussion
This study demonstrated that patients with all forms of isolated dystonia have an overall 3.5-fold increased rate of suicidal behavior compared to the general global population. Patients with generalized and multifocal/segmental dystonias exhibited the highest rates of both suicidal ideations and attempt, thus representing the highest at-risk groups.
Suicidality is complex in its etiology and cannot be attributed to a single risk factor. Instead, different biological, psychological, social components and psychiatric disorders have a collective effect on the development of suicidal behavior.24 In patients with dystonia, it is plausible that more severe symptomatology of generalized and multifocal/segmental dystonias may underlie their higher rates of suicidal behavior compared to patients with focal dystonias who have more localized symptomatology. This assumption may be supported by our data showing that, at the presence of overall high suicidality across all forms of dystonia, there is a variability in suicidal behavior being specifically induced by dystonia. Dystonia-induced rates for both suicidal ideations and attempts were the highest in patients with generalized dystonia, which may be provoked by a greater body distribution and severity of their symptoms. However, a similarly high rate of dystonia-induced suicidal behavior was found in patients with focal dystonias (except for laryngeal dystonia), although these patients had the lowest ideation-to-attempt ratio. This suggests that other endogenous factors, in addition to disorder severity, may play an important role in predilection for suicide.
Along this line, we found a high prevalence of psychiatric disorders in patients with dystonia, as reported in earlier studies.4–10 Specifically, the high incidence of depression and anxiety disorders and their strong association with suicidal behavior is likely another significant contributor to the high suicidality rates across all forms of dystonia compared to the general global population. Notably, the relationship between suicidality and psychiatric disorders was not consistent between different forms of dystonia. That is, relatively lower-risk patients with focal dystonias had more significant associations between their suicidal behavior and psychiatric disorders. In contrast, higher-risk patients with multifocal/segmental and generalized dystonias showed only trends toward significance between their suicidality rates and incidence of psychiatric disorders. Therefore, although it is necessary to consider depression and other psychiatric history as potential risk factors for suicidal ideations and attempt, it is also critical to evaluate their interplay with dystonia symptomatology, the individual's propensity to suicide, and other potential social and biological stressors that may lead to suicidal behavior in patients with dystonia. In addition, the potential effects of genetic susceptibility, frequent comorbidities (e.g., tremor), treatment outcomes, and other extrinsic risk factors should be considered in future studies of suicidality in larger cohorts of patients with different forms of isolated dystonia.
Given the devastating effects of suicide, our findings strongly support the incorporation of a suicidal risk screening into the routine clinical evaluations of patients with dystonia. It is important to consider that challenges in clinical assessment and intervention may arise from the above-discussed multifactorial nature of suicidality and the tendency of suicidal patients to refrain from disclosing their thoughts of suicide to clinicians.25,26 Although these realities can make it difficult to assess the risk for suicide timely and accurately, the utilization of standardized, validated assessment tools, such as the C-SSRS,17 are nevertheless found to be effective in establishing the risk for suicide and assessing the presence of suicidal behavior.27 We propose that the use of suicidal risk assessments with follow-up clinical interventions in these patients would prevent potential suicide-associated injury and death.28 Depending on the level of risk for suicide, interventions may range from referral to a mental health clinician for further evaluation of suicidal behavior, psychiatric illnesses, or stressors to immediate hospitalization.29,30 Policies and specific protocols of intervention for patients with dystonia showing suicidal behavior may also vary by institution and need to be taken into consideration when determining further steps for their clinical care.
As our study provides the first insight into suicidality in dystonia, its limitations are important to acknowledge. Methodologically, an online questionnaire may have exposed the study to the self-reporting bias, and the anonymous data collection prevented us from tracking the patients' responses or conducting follow-ups, especially of those individuals who reported the presence of suicidal ideations at the time of study participation. On the other hand, the online and anonymous format of the survey allowed us to collect data from a large number of patients with this rare disorder in a relatively short period of time, as well as to increase the likelihood of patients responding truthfully to sensitive questions about their suicidality. In addition, our construction of survey questions based on a validated and widely practiced C-SSRS allowed us to capture patients' responses in a standardized manner.
Another limitation to consider is the variation in sample sizes within each dystonia cohort. Only one patient had hemidystonia, which limited our ability to conduct statistical analysis. However, because hemidystonia most commonly occurs secondary to stroke or injury,31 the exclusion of this patient further ensured the current study's focus on isolated dystonia. Patients with isolated laryngeal dystonia constituted a substantially larger group of survey participants, which prompted their separation from the group of patients with other forms of focal dystonia for the conduct of a meaningful statistical analysis. Despite the differences in cohort sizes, their overall demographics and clinical features were in line with other studies,10,32–34 suggesting an appropriate patient representation even in smaller cohorts. Moreover, statistical analysis focused on the examination of within-group differences in suicidality compared to the general global rates, further eliminating the potential bias of unbalanced group comparisons.
In conclusion, suicidality in dystonia may be a critical, albeit yet unrecognized, trait of isolated dystonia. Screening for suicidal risk should be incorporated as part of a clinical evaluation of patients with dystonia in order to prevent suicide-induced injury and death. Further research in international, multicenter clinical settings is warranted for the development of a more detailed understanding of the multifactorial mechanisms of suicidal behavior in dystonia.
Acknowledgment
The authors thank the Harvard Clinical and Translational Science Center of the Harvard Catalyst (UL 1TR002541) for providing support with statistical analysis.
Glossary
- C-SSRS
Columbia–Suicide Severity Rating Scale
- CI
confidence interval
- OR
odds ratio
- REDCap
Research Electronic Data Capture
Appendix. Authors

Footnotes
Editorial, page 511
CME Course: NPub.org/cmelist
Study Funding
This study was funded by grant R01DC012545 from the National Institute on Deafness and Other Communication Disorders, NIH, to K. Simonyan.
Disclosure
A. Worthley reports no disclosures. K. Simonyan receives funding from the NIH (R01NS088160, R01DC011805, R01DC012545), the Department of Defense (W911NF1810434), and Amazon Web Services, and serves on the Scientific Advisory Board of the Tourette Association of America. Go to Neurology.org/Nhttps://n.neurology.org/lookup/doi/10.1212/WNL.0000000000011596 for full disclosures.
References
- 1.Asgeirsson H, Jakobsson F, Hjaltason H, Jonsdottir H, Sveinbjornsdottir S. Prevalence study of primary dystonia in Iceland. Mov Disord 2006;21:293–298. [DOI] [PubMed] [Google Scholar]
- 2.de Carvalho Aguiar PM, Ozelius LJ. Classification and genetics of dystonia. Lancet Neurol 2002;1:316–325. [DOI] [PubMed] [Google Scholar]
- 3.Nutt JG, Muenter MD, Melton LJ III, Aronson A, Kurland LT. Epidemiology of dystonia in Rochester, Minnesota. Adv Neurol 1988;50:361–365. [PubMed] [Google Scholar]
- 4.Gündel H, Wolf A, Xidara V, Busch R, Ceballos-Baumann A. Social phobia in spasmodic torticollis. J Neurol Neurosurg Psychiatry 2001;71:499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zurowski M, McDonald W, Fox S, Marsh L. Psychiatric comorbidities in dystonia: emerging concepts. Mov Disord 2013;28:914–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cavallaro R, Galardi G, Cavallini MC, et al. Obsessive compulsive disorder among idiopathic focal dystonia patients: an epidemiological and family study. Biol Psychiatry 2002;52:356–361. [DOI] [PubMed] [Google Scholar]
- 7.Gündel H, Wolf A, Xidara V, et al. High psychiatric comorbidity in spasmodic torticollis: a controlled study. J Nerv Ment Dis 2003;191:465–473. [DOI] [PubMed] [Google Scholar]
- 8.Fabbrini G, Berardelli I, Moretti G, et al. Psychiatric disorders in adult-onset focal dystonia: a case-control study. Mov Disord 2010;25:459–465. [DOI] [PubMed] [Google Scholar]
- 9.Voon V, Butler TR, Ekanayake V, et al. Psychiatric symptoms associated with focal hand dystonia. Mov Disord 2010;25:2249–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berman BD, Junker J, Shelton E, et al. Psychiatric associations of adult-onset focal dystonia phenotypes. J Neurol Neurosurg Psychiatry 2017;88:595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bradvik L. Suicide risk and mental disorders. Int J Environ Res Public Health 2018;15:2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry 2008;192:98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull 2007;133:859–883. [DOI] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirke DN, Frucht SJ, Simonyan K. Alcohol responsiveness in laryngeal dystonia: a survey study. J Neurol 2015;262:1548–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 2011;168:1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawton K, van Heeringen K. Suicide. Lancet 2009;373:1372–1381. [DOI] [PubMed] [Google Scholar]
- 19.Defazio G, Conte A, Gigante AF, Fabbrini G, Berardelli A. Is tremor in dystonia a phenotypic feature of dystonia? Am Acad Neurol 2015:1053–1059. [DOI] [PubMed] [Google Scholar]
- 20.Jankovic J, Leder S, Warner D, Schwartz K. Cervical dystonia: clinical findings and associated movement disorders. Neurology 1991;41:1088–1091. [DOI] [PubMed] [Google Scholar]
- 21.Deuschl G, Bain P, Brin M. Consensus statement of the Movement Disorder Society on Tremor: Ad Hoc Scientific Committee. Mov Disord 1998;13(suppl 3):2–23. [DOI] [PubMed] [Google Scholar]
- 22.O'Carroll PW, Berman AL, Maris RW, Moscicki EK, Tanney BL, Silverman MM. Beyond the Tower of Babel: a nomenclature for suicidology. Suicide Life Threat Behav 1996;26:237–252. [PubMed] [Google Scholar]
- 23.Silverman MM, Berman A, Sanddal N, O'Carroll P, Joiner T. Rebuilding the Tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors part 2: suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav 2007;37:264–277. [DOI] [PubMed] [Google Scholar]
- 24.van Heeringen K, Mann JJ. The neurobiology of suicide. Lancet Psychiatry 2014;1:63–72. [DOI] [PubMed] [Google Scholar]
- 25.Cook E, Lotito M. A review of suicide risk assessment instruments and approaches. Ment Health Clinician 2015;5:216–223. [Google Scholar]
- 26.Silverman MM. Suicide risk assessment and suicide risk formulation. J Psychiatr Pract 2014;20:373–378. [DOI] [PubMed] [Google Scholar]
- 27.Oquendo MA, Bernanke JA. Suicide risk assessment: tools and challenges. World Psychiatry 2017;16:28–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burgess P, Pirkis J, Morton J, Croke E. Lessons from a comprehensive clinical audit of users of psychiatric services who committed suicide. Psychiatr Serv 2000;51:1555–1560. [DOI] [PubMed] [Google Scholar]
- 29.Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am J Psychiatry 2003;160:1–60. [PubMed] [Google Scholar]
- 30.New recommended standard care for people with suicide risk aims to fundamentally improve suicide care delivered nationwide: action alliance releases evidence-based guidance aimed at making health care safe for people with suicide risk. J Health Care Compliance 2018;20. [Google Scholar]
- 31.Jankovic J. Primary and secondary generalized dystonias. In: Office Practice of Neurology. Elsevier; 2003:816–821. [Google Scholar]
- 32.Schweinfurth JM, Billante M, Courey MS. Risk and demographics in patients with spasmodic dysphonia. Laryngoscope 2002;112:220–223. [DOI] [PubMed] [Google Scholar]
- 33.Phukan J, Albanese A, Gasser T, Warner T. Primary dystonia and dystonia-plus syndromes: clinical characteristics, diagnosis, and pathogenesis. Lancet Neurol 2011;10:1074–1085. [DOI] [PubMed] [Google Scholar]
- 34.Pirio Richardson S, Wegele AR, Skipper B, Deligtisch A, Jinnah HA; Dystonia Coalition Investigators. Dystonia treatment: patterns of medication use in an international cohort. Neurology 2017;88:543–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to clinical and research information of the datasets used in this study are included. De-identified data and analysis pipeline may be shared upon request.