We read with interest the recent article by Badal et al. highlighting clinical characteristics of 1810 paediatric COVID-19 cases. While we agree that children have a better prognosis [1], the neonatal population, as opposed to older children, is susceptible to vertical transmission of SARS-CoV-2 [2], which includes in-utero, intrapartum and early postnatal infection [3].
We aimed to determine the clinical manifestations of neonatal COVID-19 and outcomes based on severity groups. We conducted a systematic review (CRD42020183500) and searched Embase, PubMed, and China Knowledge Resource Integrated (CNKI) from 01 December 2019 to 01 August 2020, using the terms “infant”, “newborn”, “SARS-CoV-2″, “COVID-19″ and variants (Supplemental Material 1). Additional studies were identified from references of included studies and the John Hopkins Centre for Humanitarian Health database. Studies reporting neonates (≤ 28 days old) who tested positive for SARS-CoV-2 by reverse transcriptase PCR (RT-PCR) were included. Descriptive statistics were used to compare mild-moderately ill neonates (non-severe group) with severe-critically ill neonates (severe group). Grouping was based on World Health Organization’s definition [4].
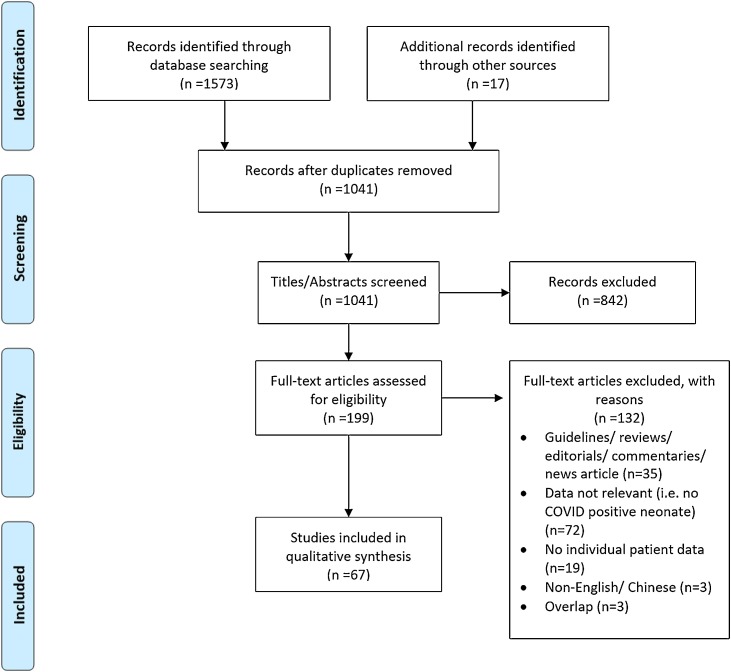
We reviewed 199 full-text articles; 67 studies fulfilled the inclusion criteria (Fig. 1 ). Quality assessment scores were moderate for the 52 case series (mean = 3.06) and 15 cohort studies (mean = 5) included (Supplemental Material 2). Of 99 neonates diagnosed with COVID-19 infection, 27 (27.3 %) were asymptomatic. Amongst symptomatic neonates, respiratory symptoms were common — dyspnoea (36.1 %), nasal symptoms (19.4 %), cough (18.1 %); 55.6 % had fever. Thirty neonates (30.3 %) had severe-critical illness. Compared to the non-severe group, more neonates in the severe group were symptomatic (100 % vs 60.9 %, p < 0.001), admitted to the intensive care unit (91.7 % vs 41.7 %, p < 0.001), had dyspnoea (66.7 % vs 14.3 %, p < 0.001) and abnormal chest radiographic findings (84.6 % vs 61.5 %, p = 0.038). Mild-moderately ill neonates had increased incidence of fever (69.0 % vs 36.7 %, p = 0.006) and gastrointestinal symptoms (26.2 % vs 3.33 %, p = 0.01). Laboratory findings were similar between these two groups (Table 1 ).
Fig. 1.
PRISMA Flow Chart.
Table 1.
Neonates with COVID-19 diagnosed by positive RT-PCR test.
| Mild/moderate condition Non-severe group (n = 69) |
Severe/critical condition Severe group (n = 30) |
p value | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Gestational age at birth, weeks | |||||
| ≥ 37 | 33/40 | 82.5 | 15/24 | 62.5 | 0.128 |
| 32 to < 37 | 4/40 | 10.0 | 8/24 | 33.3 | |
| 28 to < 32 | 2/40 | 5.0 | 1/24 | 4.2 | |
| <28 | 1/40 | 2.5 | 0/24 | 0.0 | |
| Age at diagnosis, days (median, IQR) | 7 (2–17.5) | 6 (2–13.75) | 0.692 | ||
| Birth weight, g (median, IQR) | 3120 (2743–3470) | 2930 (2520–3370) | 0.408 | ||
| Gender | |||||
| Male | 27/41 | 65.9 | 17/27 | 63.0 | 0.807 |
| Female | 14/41 | 34.1 | 10/27 | 37.0 | |
| Symptomatic | 42/69 | 60.9 | 30/30 | 100.0 | <0.001* |
| Symptoms in symptomatic neonates | |||||
| Fever | 29/42 | 69.0 | 11/30 | 36.7 | 0.006* |
| Dyspnoea (apnoea, tachypnoea, hypoxia, cyanosis, chest retractions, increased work of breathing, desaturation) | 6/42 | 14.3 | 20/30 | 66.7 | <0.001* |
| Cough | 9/42 | 21.4 | 4/30 | 13.3 | 0.379 |
| Nasal symptoms (congestion, stuffiness, discharge, sneezing) | 10/42 | 23.8 | 4/30 | 13.3 | 0.268 |
| Gastrointestinal symptoms (diarrhoea, vomiting) | 11/42 | 26.2 | 1/30 | 3.33 | 0.01* |
| Feeding problems | 11/42 | 26.2 | 12/30 | 40.0 | 0.215 |
| Laboratory and radiological findings | |||||
| Leukopenia (<5.0 × 109/L) | 3/23 | 13.0 | 4/19 | 21.1 | 0.488 |
| Leukocytosis (>19.0 × 109/L) | 1/21 | 4.76 | 1/16 | 6.25 | 0.843 |
| Lymphopenia (<3.0 × 109/L) | 11/24 | 45.8 | 7/17 | 41.2 | 0.767 |
| Thrombocytopenia (<200 × 109/L) | 1/15 | 6.67 | 2/14 | 14.3 | 0.501 |
| Elevated C-reactive protein (>10 mg/L) | 2/19 | 10.5 | 3/19 | 15.8 | 0.631 |
| Elevated procalcitonin (>0.5ug/L) | 1/13 | 7.69 | 2/8 | 25.0 | 0.271 |
| Elevated d-dimer (>0.5ug/mL) | 1/1 | 100.0 | 4/4 | 100.0 | NA |
| Elevated serum lactate dehydrogenase (>860 u/L) | 0/4 | 0.0 | 2/3 | 66.7 | 0.143** |
| Chest X-Ray or Computed Tomography or Lung Ultrasound | |||||
| Normal findings | 10/26 | 38.5 | 4/26 | 15.4 | |
| Suggestive of pneumonia | 16/26 | 61.5 | 18/26 | 69.2 | 0.038* |
| Other findings, not of pneumonia | 0/26 | 0.0 | 4/26 | 15.4 | |
| Clinical outcomes | |||||
| Intensive care unit (ICU) admission | 15/36 | 41.7 | 22/24 | 91.7 | <0.001* |
| Duration of hospital stay (median, IQR) | 7.5 (2–16) | 8 (4.5–18) | 0.143 | ||
| Survival | 60/60 | 100.0 | 28/28 | 100.0 | NA |
Significant at p<0.05, Chi-square test.
Fisher’s Exact test.
Similar to older children, neonates with dyspnoea were more likely to develop severe illness [5]. However, diagnosis of severe illness may be confounded by co-existing respiratory diseases present in many neonates with critical COVID-19. Contrary to adults [6], presence of fever did not predict for more severe disease in neonates.
The angiotensin-converting enzyme 2, a major virus receptor, is expressed in the gastrointestinal tract. Thus, in children, gastrointestinal symptoms were correlated with critical illness [7]. However, in our review, gastrointestinal symptoms were associated with milder illness. Amongst 11 mild-moderately ill neonates displaying gastrointestinal symptoms, 10 did not have dyspnoea. We postulate that the presence of gastrointestinal symptoms alone predicts a better prognosis, while gastrointestinal symptoms with dyspnoea predicts a worse outcome, as in adults [8].
Prognosis of COVID-19 neonates were favourable, with no serious complications or mortalities reported. However, included studies were of moderate quality, with incomplete reporting of clinical and investigation results. Additionally, asymptomatic or mildly ill neonates could have been underdiagnosed and hence unaccounted for. As the pandemic evolves, prospective [9] and more systematic reporting of cases will improve our understanding of neonatal COVID-19 and verify utility of symptoms and laboratory tests in predicting disease severity.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Kia Hui Lim: Substantial contributions to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; AND final approval of the version to be published;
Faith Si Jia Soong: Substantial contributions to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; AND final approval of the version to be published;
Yi Fen Low: Substantial contributions to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; AND final approval of the version to be published;
Xin Lei Goh: Substantial contributions to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; AND final approval of the version to be published;
Zubair Amin: Substantial contributions to the conception or design of the work; the interpretation of data for the work; drafting the work or revising it critically for important intellectual content; AND final approval of the version to be published;
Yvonne Peng Mei Ng: Substantial contributions to the conception or design of the work; the interpretation of data for the work; drafting the work or revising it critically for important intellectual content; AND final approval of the version to be published.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
We thank Dr Dimple Rajgor for helping with editing, formatting, and submission of the manuscript for publication.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jcv.2021.104819.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Badal S., Thapa Bajgain K., Badal S., Thapa R., Bajgain B.B., Santana M.J. Prevalence, clinical characteristics, and outcomes of pediatric COVID-19: a systematic review and meta-analysis. J. Clin. Virol. 2020 doi: 10.1016/j.jcv.2020.104715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goh X.L., Low Y.F., Ng C.H., Amin Z., Ng Y.P.M. Incidence of SARS-CoV-2 vertical transmission: a meta-analysis. Arch. Dis. Child. Fetal Neonatal Ed. 2020 doi: 10.1136/archdischild-2020-319791. Jun 25;fetalneonatal-2020-319791. doi: 319710.311136/archdischild-312020-319791. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . World Health Organization; 2021. Definition and Categorization of the Timing of Mother-to-child Transmission of SARS-CoV-2: Scientific Brief.https://ddec1-0-en-ctp.trendmicro.com:443/wis/clicktime/v1/query?url=https%3a%2f%2fwww.who.int%2fpublications%2fi%2fitem%2fWHO%2d2019%2dnCoV%2dmother%2dto%2dchild%2dtransmission%2d2021.1&umid=d5a1367e-13df-4e78-8b6f-10a9f7441c16&auth=8d3ccd473d52f326e51c0f75cb32c9541898e5d5-69d5788a687768e6454885c61e984ead6845a1cc Available at. Accessed 23 March 2021; 2021. [Google Scholar]
- 4.World Health Organization . World Health Organization; 2020. Clinical Management of COVID-19.https://www.who.int/publications/i/item/clinical-management-of-covid-19 May 27 Available at: Accessed 01 Sept, 2020.; 2020. [Google Scholar]
- 5.Hoang A., Chorath K., Moreira A., Evans M., Burmeister-Morton F., Burmeister F., et al. COVID-19 in 7780 pediatric patients: a systematic review. EClin. Med. 2020;24 doi: 10.1016/j.eclinm.2020.100433. Published online 102020 Jun 100426. doi: 100410.101016/j.eclinm.102020.100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou C., Huang Z., Tan W., Li X., Yin W., Xiao Y., et al. Predictive factors of severe coronavirus disease 2019 in previously healthy young adults: a single-center, retrospective study. Respir. Res. 2020;21:157. doi: 10.1186/s12931-020-01412-1. https://doi.org/110.1186/s12931-12020-01412-12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giacomet V., Barcellini L., Stracuzzi M., Longoni E., Folgori L., Leone A., et al. Gastrointestinal symptoms in severe COVID-19 children. Pediatr. Infect. Dis. J. 2020;39:e317–e320. doi: 10.1097/INF.0000000000002843. [DOI] [PubMed] [Google Scholar]
- 8.Sulaiman T., Algharawi A.A., Idrees M., Alzaidy R.H., Faris K., Cullingford G., et al. The prevalence of gastrointestinal symptoms among patients with COVID-19 and the effect on the severity of the disease. JGH Open n/a. 2020 doi: 10.1002/jgh3.12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gale C., Quigley M.A., Placzek A., Knight M., Ladhani S., Draper E.S., et al. Characteristics and outcomes of neonatal SARS-CoV-2 infection in the UK: a prospective national cohort study using active surveillance. Lancet Child Adolesc. Health. 2020 doi: 10.1016/S2352-4642(20)30342-4. Nov 9:S2352-4642(2320)30342-30344. doi: 30310.31016/S32352-34642(30320)30342-30344. Epub ahead of print. PMID: 33181124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.