PRACTICAL IMPLICATIONS
COVID-19 may be associated with neurologic complications. Patients with COVID-19 may develop an acute inflammatory painful polyradiculoneuritis that seems to respond to intravenous human immunoglobulin.
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has emerged in Wuhan, China, in December 2019,1 and the World Health Organization has declared it a pandemic in March 2020. Since then, severe neurologic complications associated with COVID-19 have been described, including encephalitis and stroke.2,3 Recently, it has been recognized that acute neuropathies may also occur.4,5 Herein, we report a patient with COVID-19 presenting an acute refractory painful polyradiculoneuritis.
Case
A 38-year-old man presented with a 5-day history of fever, dry cough, and fatigue, followed by respiratory distress. His chest CT revealed bilateral ground-glass opacities, and he was admitted to the intensive care unit (ICU) requiring mechanical ventilation. His medical history included Class I obesity, regular alcohol, and cigarette consumption. He was treated with oseltamivir, hydroxychloroquine, azithromycin, and antibiotics for nosocomial pneumonia. Nasopharyngeal RT-PCR for SARS-CoV-2 was positive on days 1 and 12. He received a tetravalent vaccine for influenza on day 6. Sedation was discontinued 15 days after ICU admission, when he started complaining of proximally excruciating pain in both legs. Although strength and deep tendon reflexes were preserved, he was diagnosed with critical illness polyneuropathy by the ICU team, and morphine, duloxetine, and pregabaline were started. He was discharged 20 days after admission with persisting pain and negative RT-PCR.
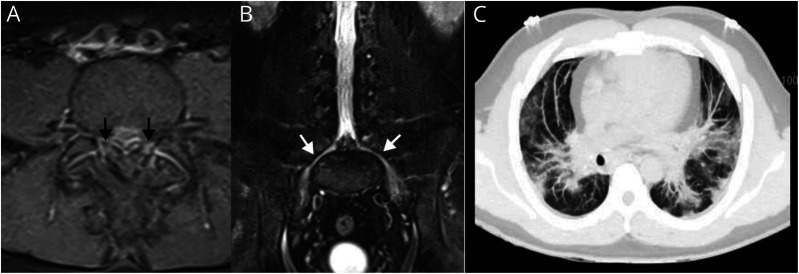
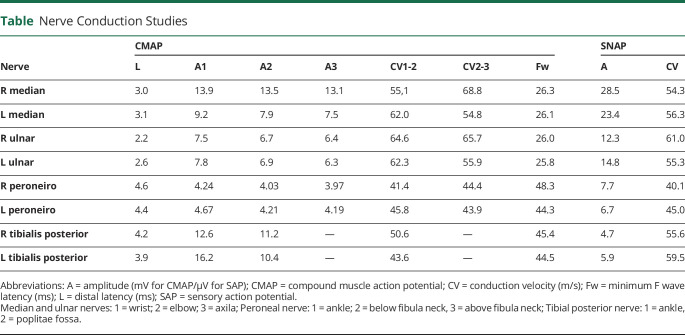
Five days after hospital discharge, he was evaluated by a neurologist, reporting a visual analogue scale (VAS) for pain of 10 in 10 (10/10). Treatment was adjusted (duloxetine, pregabaline, amitriptyline, morphine, and vitamins supplementation), and in few days, his VAS turned 0/10. However, 1 week later, his painful manifestations returned, including tingling paresthesia and burning pain distally in lower limbs. At this time, his neurologic examination showed weakness in muscles of L5 myotomal distribution bilaterally, and pinprick-evoked pain reduced distally on both feet, accompanied by intense tactile allodynia. Deep tendon reflexes, vibration, and proprioception were normal. He had flexor plantar responses bilaterally. Cranial nerves were normal. There were no dysautonomic or sphincter abnormalities. Nerve conductions studies, including F waves, were within normal limits, and concentric needle examination showed signs of acute denervation in lumbosacral muscles innervated by right L4-L5-S1 and left L5-S1 roots (figure and table). Spinal cord MRI revealed enhancement of L5 bilaterally. CSF revealed albuminocytologic dissociation (cells: 0; protein: 76 mg/dL). An acute painful inflammatory polyradiculoneuritis was suspected, and high-dose intravenous human immunoglobulin (IVIG 0.4 g/kg for 5 days) was prescribed. He has been stable (VAS 3–4/10) on the following 2 weeks. At the last visit to the neurologist, 3 weeks after IVIG infusion, the patient reported significant clinical improvement, persisting only with mild radicular pain on both legs.
Figure. Lumbosacral MRI and Chest CT.
(A) T1-weighted postcontrast axial with fat suppression reveals enhancement of bilateral L5 roots (black arrows). (B) T2-weighted coronal with fat suppression shows hyperintensity of bilateral L5 nerves (white arrows). (C) Chest CT with bilateral ground-glass opacities.
Table.
Nerve Conduction Studies
Discussion
We described a case of acute inflammatory painful polyradiculoneuritis and suggest that it could be an atypical neurologic manifestation related to COVID-19 infection.
Recently, acute neuropathies have been described in relation to COVID-19. Toscano et al.4 reported 5 patients with COVID-19 diagnosed as having Guillain-Barré syndrome (GBS). All had severe SARS-CoV-2 infection, and neurologic symptoms emerged within the first 10 days (parainfectious profile). Four of 5 presented lower-limb flaccid weakness and arreflexia that progressed to flaccid tetraparesis/tetraplegia. Two had high CSF protein levels, and 3 had been classified as an axonal variant. Another report described a patient with severe polyradiculoneuritis leading to a locked-in syndrome.5 By contrast, our patient had a clinical profile restricted to lower limbs and predominantly painful, considered an acute inflammatory lumbosacral polyradiculoneuritis.
In addition, 3 Chinese patients presenting an acute painful autoimmune small-fiber neuropathy were described.6 They had antecedent infectious disease, presented clinically with severe pain distally in a glove-and-stocking distribution plus dysautonomia and also albuminocytologic dissociation. These key aspects (previous infectious disease, acute painful neuropathy, and albuminocytologic dissociation) are present in our patient's history and support the autoimmune nature of the peripheral nerve involvement. The symptoms evolved to the lumbosacral roots, as corroborated by MRI and EMG findings, leading us to classify it as a polyradiculoneuritis rather than a diffuse small-fiber neuropathy.
Neuropathic pain has already been described in patients with COVID-19.2 Because no additional information was provided, it is possible that they also had a polyradiculoneuritis, similar to our case. Previous exposure to seasonal influenza vaccination should be considered a confounding causal factor, but recent epidemiologic studies question the association of this vaccine and GBS.7 Unfortunately, we were unable to perform RT-PCR on the CSF to exclude a direct lesion by the virus.
In conclusion, our case report suggests that patients with COVID-19 may develop an acute inflammatory painful polyradiculoneuritis that seems to respond to IVIG.
Appendix. Authors
Footnotes
Study Funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020;77:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moriguchi T, Harii N, Goto J, et al. A first case of meningitis/encephalitis associated with SARS-coronavirus-2. Int J Infect Dis 2020;94:55–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toscano G, Palmerini F, Ravaglia S, et al. Guillain–Barré syndrome associated with SARS-CoV-2. N Engl J Med 2020;382:2574–2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pfefferkorn T, Dabitz R, von Wernitz-Keibel T, et al. Acute polyradiculoneuritis with locked-in syndrome in a patient with covid-19. J Neurol 2020;267:1883–1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuki N, Chan AC, Wong AHY, et al. Acute painful autoimmune neuropathy: a variant of Guillain-Barré syndrome. Muscle Nerve 2018;57:320–324. [DOI] [PubMed] [Google Scholar]
- 7.Grave C, Boucheron P, Rudant J, et al. Seasonal influenza vaccine and Guillain-Barré syndrome: a self-controlled case series study. Neurology 2020;94:e2168–e2179. [DOI] [PubMed] [Google Scholar]