Abstract
Neurologists around the country and the world are rapidly transitioning from traditional in-person visits to remote neurologic care because of the coronavirus disease 2019 pandemic. Given calls and mandates for social distancing, most clinics have shuttered or are only conducting urgent and emergent visits. As a result, many neurologists are turning to teleneurology with real-time remote video-based visits with patients to provide ongoing care. Although telemedicine utilization and comfort has grown for many acute and ambulatory neurologic conditions in the past decade, remote visits and workflows remain foreign to many patients and neurologists. Here, we provide a practical framework for clinicians to orient themselves to the remote neurologic assessment, offering suggestions for clinician and patient preparation before the visit; recommendations to manage common challenges with remote neurologic care; modifications to the neurologic examination for remote performance, including subspecialty-specific considerations for a variety of neurologic conditions; and a discussion of the key limitations of remote visits. These recommendations are intended to serve as a guide for immediate implementation as neurologists transition to remote care. These will be relevant not only for practice today but also for the likely sustained expansion of teleneurology following the pandemic.
The coronavirus disease 2019 (COVID-19) pandemic has rapidly changed clinical practice. In response to calls for social distancing and home sheltering, clinics have closed, and ambulatory care has gone virtual nearly overnight. The federal government recently relaxed telehealth technology regulations, allowing the use of a wider range of software platforms to extend care.1 The Center for Medicare & Medicaid Services (CMS) simultaneously expanded telemedicine reimbursements.2 The U.S. Department of Health and Human Services recently urged state governors to modify telemedicine regulatory barriers, including waiving licensure requirements for out-of-state clinicians.3 Many private insurance companies followed suit, loosening previous restrictions on telehealth delivery, although questions remain surrounding coding, billing, and reimbursements for services delivered remotely.4,5 In addition, although this new environment has fostered teleneurology expansion, the move from clinic-based neurology to telemedicine has been an uneasy transition for many clinicians, practices, and hospitals.
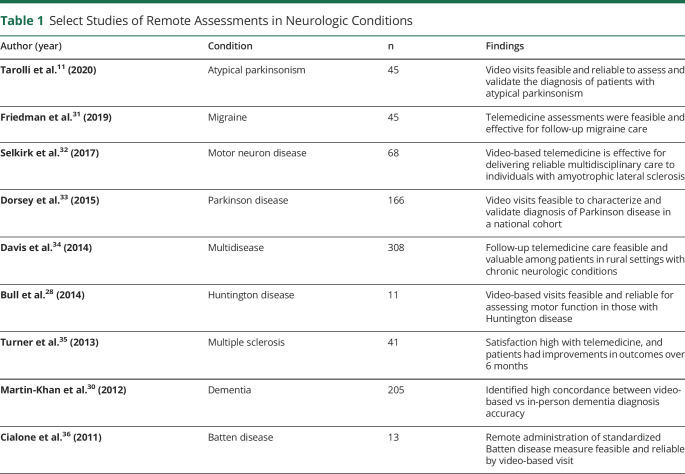
As neurologists convert traditional to virtual workflows, the in-person physical examination must be replaced by a virtual version. This is particularly challenging for neurologists who rely on the in-person examination to diagnose and manage patients. In addition to acute conditions like stroke, the feasibility of remote examinations has been demonstrated across many ambulatory neurologic conditions including headache disorders, motor neuron disease, dementia, and movement disorders (table 1). In addition, neurologic societies like the American Academy of Neurology provide guidance to assist in the transition to telemedicine.6 Despite challenges in the transition, we believe that this crisis will leave the neurologic community better positioned to embrace teleneurology, and although remote assessments are unlikely to fully replace in-person visits, they can supplement current care models and expand access to neurologic care.
Table 1.
Select Studies of Remote Assessments in Neurologic Conditions
Here, we aim to provide a practical guide to the remote video-based assessment of patients with neurologic disease. We focus on (1) general principles for conducting a remote ambulatory neurology visit; (2) methods to adapt the neurologic examination for remote performance, including disease-specific considerations and the use of available digital technologies to supplement the remote examination; and (3) limitations of the remote examination.
General Principles for the Remote Assessment
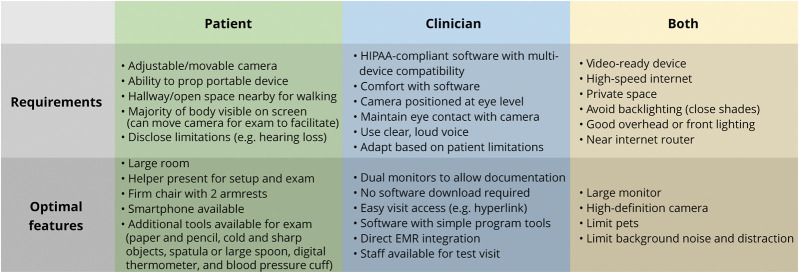
Hardware and Software
The ability to deliver video-based telemedicine to patients at home relies on the availability of specific hardware and software for both the patient and the clinician (figure 1). Each must have a device capable of transmitting video; this could include a smartphone, tablet, laptop, or desktop computer. If patients have multiple devices available, they should select the device with the best available camera and monitor. The benefits of portability with smartphones and tablets should be balanced against disadvantages, such as smaller screen and button sizes, which may be challenging for older patients. Beyond the device itself, teleneurology delivery requires a high-speed internet connection. Slow connection speeds degrade video quality and limit the neurologist's ability to assess the patient. Most patients with cable and fiber optic connections (with or without WiFi) have sufficient connection speeds, although those in rural areas may have reduced signal strength. Digital subscriber line and cellular (3G and 4G) connections are also likely sufficient, whereas dial-up connections are not.
Figure 1. Patient and Clinician Considerations During Virtual Visit Setup.
EMR = electronic medical record; HIPAA = Health Insurance Portability and Accountability Act.
Real-time video assessments are performed through several software options. Optimally, visits should be conducted using Health Insurance Portability and Accountability Act (HIPAA)-compliant software. Some electronic medical records (EMRs) have built-in telemedicine capabilities. Versions of Epic (WI), e.g., integrate video platforms to allow the patient and clinician to log into the visits using MyChart and Hyperspace, respectively. Practices without EMRs with telemedicine capabilities can use popular platforms such as Zoom Enterprise (CA), Updox (OH), and Vidyo (NJ). Although relaxed federal regulations have expanded use into HIPAA noncompliant platforms, given the potential for breach of confidentiality, we only suggest these options if no other options exist.1 Optimal software features include multiplatform (smartphone, tablet, and computer) functionality, easy visit access (accessible by hyperlink), and simple program tools (e.g., few clicks to start a visit). In addition, programs without software download requirements increase the likelihood of a successful connection.
General Considerations and Visit Setup
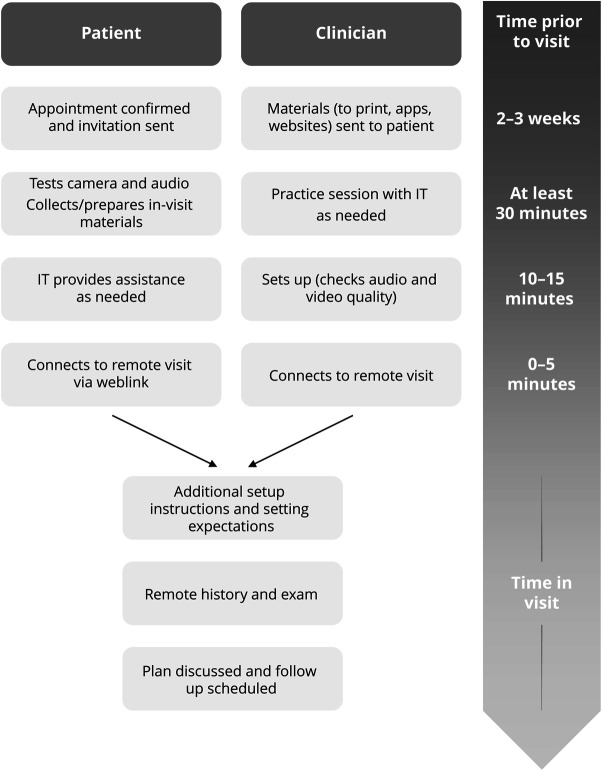
Although not required, some additional resources optimize teleneurology delivery (figure 2). First, a troubleshooting team can help clinicians and patients with basic difficulties, such as connecting to the visit. Second, if feasible, a brief previsit test between the patient and office staff increases the chance of a smooth visit. Finally, clinicians should familiarize themselves with the software to manage technical difficulties during the visit itself.
Figure 2. Visit Workflow and Timeline for the Remote Neurologic Assessment.
Patients should be instructed on how to set up for the visit in their home (figure 1). Room selection and patient positioning are some of the most important factors. Patients should select a large, private room with good lighting that is near their internet router (if using WiFi) and a seat without windows behind it to avoid degrading the video because of backlighting. Camera positioning should allow the neurologist to assess global and spontaneous movements, which requires viewing the entire body. The patient can move their camera or chair during the examination to facilitate this assessment. Optimally, patients should conduct the visit with another person available to hold or move the camera, assist with technology, or assist with the examination.
Clinicians should similarly consider camera positioning, room selection, and webside manner, particularly if conducting the visit from home. A second monitor is useful to facilitate watching the patient while concurrently reviewing and documenting in the EMR. It is also important to be mindful of virtual empathy. Strong verbal communication is important to obtain an accurate history and examination.7 Clinicians should speak loudly and clearly, introduce themselves with their first and last names, and ask the patient and helper how they would like to be addressed. The clinician should also orient the patient to the visit, as video-based visits are likely foreign to most, and at the end of the encounter, should ask the patient to repeat a brief summary of recommendations to ensure understanding. In addition to verbal communication, examiners should be mindful of body language and nonverbal communication. It is important to maintain open body language and good eye contact while interviewing. Clinicians should look at the camera itself while speaking to more closely approximate in-person eye contact.
Basic expectations for an in-office visit, such as professional attire for the clinician and patient, and avoiding interruptions should be upheld during the telemedicine visit. Should there be risk of interruption (e.g., because of concurrent time at home with children), clinicians should alert patients to this possibility at the start of the visit. Most states require clinicians to obtain consent from patients before conducting a telemedicine visit. This should include an overview of the limitations of and alternatives to the telemedicine encounter, including privacy risks, potential financial liability, and an inability to make some diagnostic decisions. Finally, at the start of a visit, it is imperative to confirm information from the patient in case of an emergency, including patient address and a reliable telephone number.
The Remote Neurologic Examination
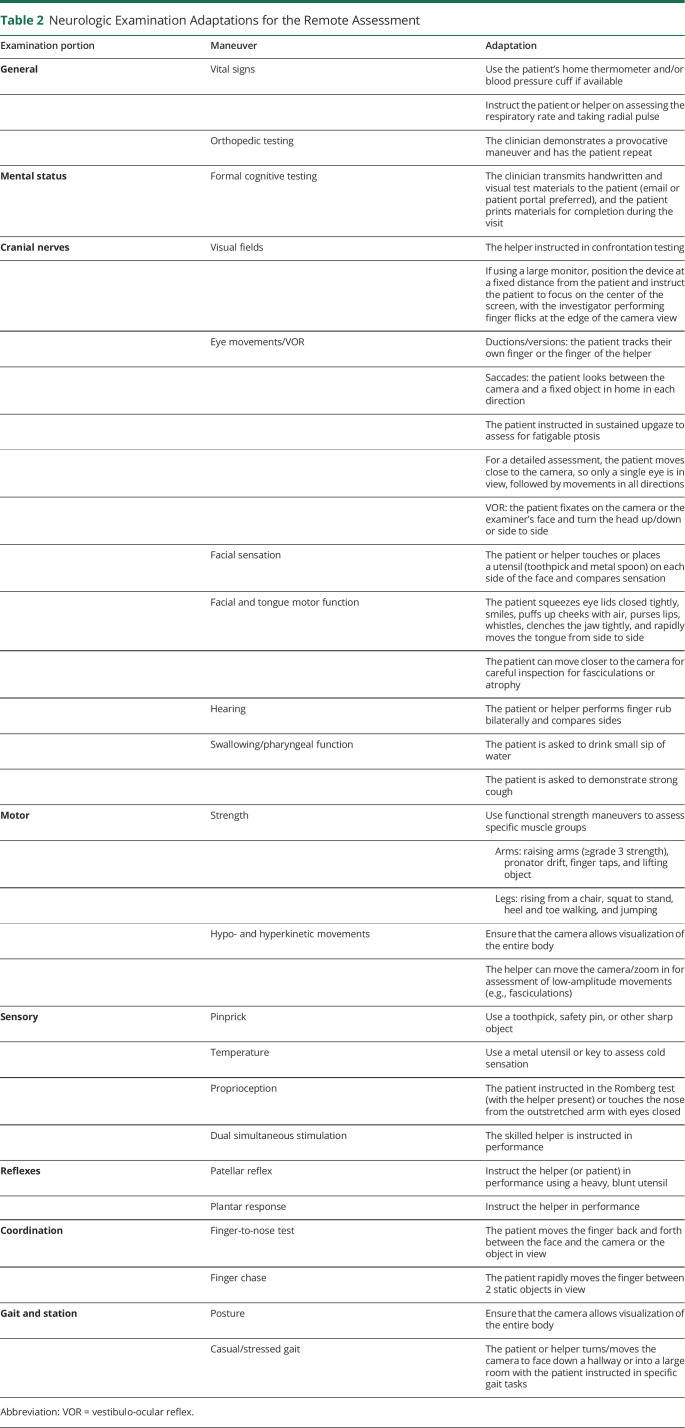
Many portions of the neurologic examination rely on simple observations and can be performed by video without additional modifications beyond appropriate lighting and patient positioning. Other aspects of the examination, like fundoscopy and objective strength assessments, require advanced digital tools or the assistance of an experienced onsite examiner. Many of the remaining portions of the examination can be performed remotely, but require modifications for the virtual environment (table 2). Beyond these modifications, clinicians should consider performance and documentation of disease-specific rating scales (e.g., Movement Disorder Society–Unified Parkinson Disease Rating Scale8,9 and Amyotrophic Lateral Sclerosis Functional Rating Scale–Revised10) to standardize assessments across visits, quantify disease severity, and track disease progression. Although some are not validated for remote performance, most can be modified easily for the virtual visit. Here, we describe the approach to the remote neurologic examination and provide a remote examination template (optimized for Epic EMR) for clinicians to use, which can help standardize the examination in practice (supplementary materials, links.lww.com/CPJ/A179).
Table 2.
Neurologic Examination Adaptations for the Remote Assessment
General Examination
Essential components of the general examination vary based on the chief complaint. Simple inspection can be performed as it would be in the office by adjusting patient or camera position. For example, dystrophic skin changes, Raynaud phenomena, or loss of hair may suggest small fiber neuropathy or other underlying diseases. The remote examination additionally allows assessment of the patient's home, facilitating evaluation for fall risks in those with imbalance, or the sleep environment in those with sleep disorders. Vital signs may be useful in some patients, and many have digital thermometers and portable blood pressure cuffs; assessment of orthostatic vital signs is feasible with instruction.11 Among those without this equipment, the neurologist or onsite helpers can assess the respiratory rate, and savvy patients or family members could be instructed to take a radial pulse. The clinician can also demonstrate provocative orthopedic maneuvers (e.g., slump test and Finkelstein test) before performance by the patient to assess the musculoskeletal system.
Mental Status
Assessment of the patient's level of alertness, orientation, language, and memory can be completed as it would in the office. Formal mental status testing can also be performed remotely with a number of measures validated for remote performance.12–14 The Montreal Cognitive Assessment (MoCA) can be modified in several ways, depending on needs and preference (mocatest.org/remote-moca-testing/). The trail making test can be performed verbally, and instructions can be given to draw a figure and clock. A blind version of the MoCA is also available and is helpful for telephone visits, when a patient has vision loss, or when there are other limitations like poor video quality.15
Cranial Nerves
The cranial nerve examination requires some of the most modifications for remote performance. Visual field testing and eye movements, for example, traditionally rely on confrontational maneuvers in front of the patient. However, through creative modifications and patient or family member instruction, many components of the cranial nerve examination can still be performed (table 2). In addition, a basic pupillary examination can be performed depending on the camera quality and zoom-in capabilities in the software used. Gross assessment of facial sensation can also be performed, including evaluation of temperature (using a cold utensil) or pinprick (if a toothpick or pin is available) sensation. Cranial nerves IX and X can be assessed by listening to speech, and patients can be asked to take a small sip of water during the visit to assess swallowing.16
Motor Examination
Patient positioning, camera quality, and room lighting are particularly important for the motor examination. Careful observation allows adequate assessment of muscle bulk and overall movement when viewing the patient from a distance; close-up assessment for fasciculations or other low-amplitude movements is possible among those with high-quality cameras. During a remote encounter, strength testing relies on inference using functional strength assessment. Patients can be asked to perform actions that use specific muscle groups (pronator drift, finger taps, rising from a chair, and heel or toe walking).
Sensory Examination
The sensory examination generally requires a reliable helper to administer the remote examination, compare right and left sides, and assess response to dual simultaneous stimulation. As above, assessment of temperature and pinprick sensation is possible with tools available in most homes. Patients can be instructed how to perform the Romberg test (with a family member nearby if concerns for safety/falls) or to touch their nose with eyes closed to assess proprioceptive function. Patients can also perform provocative sensory testing (e.g., Phalen or Tinel test) with instruction.
Coordination
Coordination testing can be performed with minimal modifications during the remote examination. Finger-to-nose testing, for example, can be performed between the patient and a helper or between the patient and a stationary object visible on the screen. Similarly, the finger chase test can be approximated by observing rapid arm movements between 2 targets. Rapid alternating movements, finger tapping, and heel-to-shin testing are performed without modification, assuming appropriate camera positioning.
Reflexes
Reflexes are challenging without a reliable onsite helper. However, family members could be instructed in performance of the plantar response or patellar reflex using the blunt side of a heavy utensil (e.g., serving spoon and large spatula), given a general familiarity with the maneuver. Other reflex assessments are not feasible remotely.
Gait
The gait examination should be performed with the assistance of a helper with the patient, both for safety and to assist with repositioning the camera. In addition, clinicians should screen for baseline postural instability and modify the gait examination to reduce the risk of falling during the remote visit. Pointing the camera into a hallway or large room cleared of obstacles allows observation of the patient's entire body. Pull testing for postural stability should be deferred because of safety concerns.
Additional Considerations by Subspecialty
Cognitive and Geriatric Assessment
Additional special consideration should be given to patients with cognitive impairment, visual impairment, and hearing loss. When assessing elderly patients, longer visit times may be required, and technology may prove overwhelming. A plain background behind the clinician can limit visual distraction during the visit. While useful for any telemedicine encounter, the presence of a family member or knowledgeable informant is particularly important here to help with technology and corroborate the history. It is important to have the patient in full view to observe spontaneous movements and interactions with the environment and family (e.g., need for cues from a family member and difficulty focusing on the camera/screen). Likewise, it is helpful to observe for signs that family members are reluctant to discuss information in the presence of the patient (e.g., shaking their head and remaining quiet for fear of angering the patient); if identified, clinicians can suggest a private follow-up call with family members. Patients with hearing aids may experience acoustic feedback or rely on a helper to repeat information. Still, despite some limitations, home teleneurology visits offer a unique insight into a person's daily life and may facilitate assessment of home safety.
Movement Disorder Assessment
Evaluation of patients with hypo- and hyperkinetic movement disorders largely relies on simple observation. Again, full body view during the entire examination allows the examiner to monitor for subtle movements that are only intermittently present or not visible with a narrow view. Adequate internet connection speed is particularly important for assessment of patients with Parkinson disease to ensure that observed bradykinesia is disease related rather than technology related. As in the office, assessment of tremor should include evaluation for postural, kinetic, rest, and vocal tremor. Having a pen and paper on hand allows Archimedes spiral drawing. Tech-savvy patients using a tablet with digital stylus can screen share a digital spiral.
Neuromuscular Assessment
The diagnosis of many neuromuscular disorders relies on a detailed neurologic examination and electrophysiologic studies not yet possible with remote assessments. Still, despite some limitations, teleneurology can establish gross localization for most patients. History taking and functional strength and sensory testing allow evaluation for proximal, distal, and asymmetric abnormalities. In addition, neurologists can document at least grade 3 (antigravity) or grade 4 (able to provide some resistance) strength during the functional strength assessment. Some diagnoses may be easily identifiable during the visit in those with typical history and examination features (e.g., myasthenia gravis, myotonic dystrophy, and dermatomyositis).
The remote assessment is also useful to triage patients requiring urgent in-person evaluation, such as those with bulbar or respiratory weakness. A simple swallow assessment, observing for forceful cough, or having patients count as high as they can in a single breath allows assessment of pharyngeal and respiratory muscle function. Patients can also be asked to lie down in view of the camera to assess breathing comfort in a supine position, observing for abdominal lift and chest expansion. Quantifying functional strength assessments (e.g., time required to stand from a seated position over 5 trials) could also be repeated in serial remote visits to trend strength in specific muscle groups.17
Novel Digital Tools
A wide range of new technologies, from wearables and biosensors to machine learning-powered augmented reality systems, are expanding the capabilities of teleneurology today. Although the majority of these are not widely available, many patients already own commercially available technologies that can supplement the remote neurologic examination. For example, as described, patients with a digital stylus can screen share a writing sample during the visit. Smartphone applications or smart watches monitoring daily step counts, heart rate, sleep, or other disease-specific features18 can provide objective information to neurologists about overall function at home. In addition, ambulatory monitoring tools such as home sleep apnea testing, nocturnal pulse oximetry, and snoring recordings can still be deployed to the home for objective assessments. Although many other disease-specific technologies are not yet validated in the clinical realm, we expect expanded use during the current crisis, followed by a more sustained boon when it ends, facilitating further expansion of teleneurology.
Limitations of the Remote Neurologic Examination
There are portions of the neurologic examination that cannot be performed via telemedicine, even under the best circumstances. In addition, many practices have limited the performance of tests viewed as extensions of the neurologic examination, including EMG and electroencephalography, in the setting of the COVID-19 pandemic. The absence of these data can limit the neurologist's ability to make a diagnosis or to facilitate medical decision making, particularly for patients being seen for initial assessment or for those with a substantial change compared with a prior in-person visit. Still, as described for the neuromuscular examination above, given uncertainty about the timing of return to normal clinical practice, remote assessment of new patients is likely necessary across all specialties. We suggest that clinicians inform patients about the limitations of the remote examination and the potential need for in-person follow-up at the start of each encounter. In practice settings where informed consent is required to initiate a telemedicine visit, this language can be incorporated into the consent script or documentation.
Although increased medico-legal risk may exist, the American Medical Association has lobbied for expanded liability coverage for physicians providing services via telehealth during the COVID-19 pandemic.19 Some states have limited malpractice litigation against care delivered during the crisis.20–22 Still, clinicians should confirm their medical liability coverage includes care provided via telemedicine. Clinicians should also document any limitations of the visit that may affect their medical decision making and share these concerns with the patient; this should include limitations in the reliability of any examination portions performed by patients or family members at home.
Beyond the limitations in examination and diagnostic capabilities, real and perceived social and societal limitations of telemedicine exist. First, the technological requirements for conducting a telemedicine visit limit access. Reassuringly, around 90% of American households have access to high-speed internet at home (73% with a broadband connection and 17% with a smartphone with cellular data without other home internet).23 Still, this suggests at least 1 in 10 Americans lack such access with overrepresentation among older patients, those in rural locations, underrepresented minority groups, and those of low socioeconomic status.23–26 Patients with neurologic disease may be overrepresented in this group, given the older age of many in the population.27 In addition, the majority of patients without access to this technology are from vulnerable populations. In a time when a substantial proportion of visits are being converted to telemedicine, this has the potential to exacerbate existing disparities in care.
Despite rising use of telemedicine, patients and neurologists may worry that visits will be impersonal. Reassuringly, assessment of remote encounters across multiple neurologic conditions demonstrates that patients and neurologists establish similar comfort as compared to routine in-person visits.11,28,29 Again, older patients with neurologic disease or those with advanced disability may feel less comfortable with the use of technology. Although previous studies have demonstrated the feasibility of remote visits among those with advanced neurodegenerative conditions, patients or families with greater baseline comfort with visits may self-select for participation in these studies, limiting generalizability.11,30
The rapid conversion to video-based teleneurology may be daunting for clinicians. However, neurologists should rest assured that most components of the in-person visit, including a substantial proportion of the neurologic examination, are directly translatable to the virtual environment with the modifications described here.7 In addition, although some patients may have initial reservations about teleneurology, many view remote visits as a convenient alternative to seeing a clinician in the office. In fact, teleneurology has the potential to expand access to care for patients with impaired mobility, limited transportation options, or limited health care provider availability in their area, assuming that they have access to the appropriate technology. This can address important gaps in care by better incorporating teleneurology into postpandemic care models.
Teleneurology is well suited for follow-up of most neurologic conditions, particularly during a crisis when the alternative is often no care. Assessing treatment response, identifying treatable symptoms, and finding ways to preserve independence are based primarily on the neurologic history. In addition, quantification of portions of the examination generates objective or pseudo-objective measures that can be followed over time. Even multidisciplinary care can be delivered remotely with physical therapists, speech pathologists, counselors, or social workers jointly attending a televisit. Remote visits can also be used to diagnose some patients with neurologic chief complaints, although we continue to consider an in-person examination preferable to a remote examination for new patients. However, given uncertainty surrounding the duration of the current crisis, the ability to triage potentially vulnerable patients for the need for in-person assessment exploits the benefits of teleneurology while mitigating risk for the patient.
Neurologists should work to incorporate remote video visits into practice today to improve their comfort with technology and the remote examination. In addition, clinicians should consider the use of novel digital tools to supplement the remote examination, including potential validation for use in clinical practice. This potentially chaotic transition to remote visits provides an opportunity to develop organized, efficient, and scalable workflows to facilitate long-term teleneurology implementation and improve traditional care models. This rapid conversion will undoubtedly set the stage for a wider adoption of teleneurology moving forward. Additional advocacy to extend the removal of barriers to telemedicine, expand physician liability protections, ensure adequate reimbursement for telehealth, and standardize the teleneurology examination and workflow can ensure that more patients with neurologic disease have ready access to care. Neurologists should act now to prepare themselves for the future of our field.
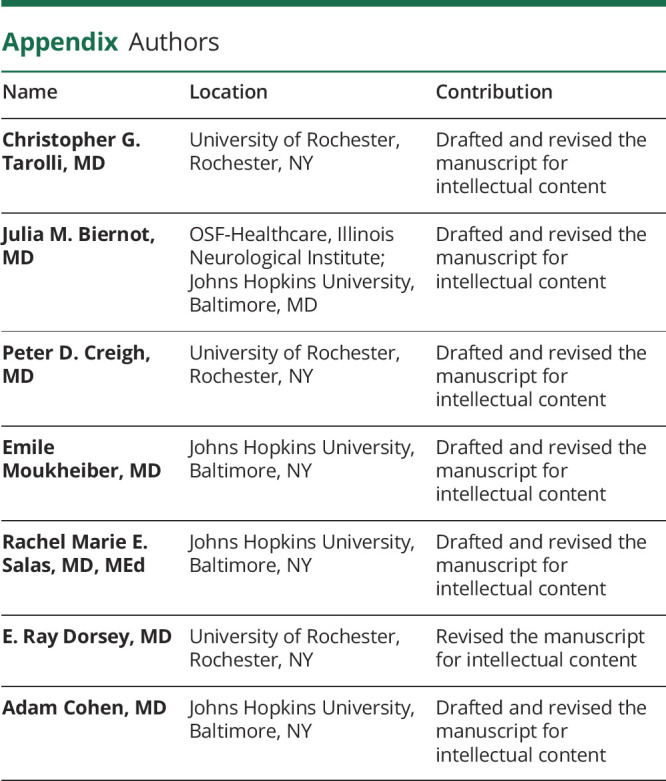
Appendix. Authors
Footnotes
Study Funding
Research reported in this publication was supported in part by the National Institute of Neurological Disorders and Stroke of the NIH under award number P50NS108676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Disclosure
Drs. Tarolli, Biernot, Creigh, and Moukheiber report no financial disclosures related to the preparation of this manuscript. Dr. Salas receives royalties from UpToDate for chapter authorship. Dr. Dorsey has received research support from AMC Health, Greater Rochester Health Foundation, Prana Biotechnology, Great Lakes Neurotechnologies, and Patient-Centered Outcomes Research Institute. Dr. Cohen consults for Pear Therapeutics and Thirty Madison and has stock options in the latter. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.U.S. Department of Health and Human Services. Emergency Situations: Preparedness, Planning, and Response. In: Services HaH, ed. Available at: www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/index.html#2020. Accessed March 31, 2020. [Google Scholar]
- 2.Centers for Medicare & Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. In: Services CfMM, ed: cms.gov; 2020. Available at: www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed March 31, 2020. [Google Scholar]
- 3.Azar AM. Secretary of Health and Human Services Letter to Governors. In: Services HaH, ed; 2020. Available at: www.aau.edu/sites/default/files/AAU-Files/Key-Issues/Campus-Safety/GovernorLetterfromAzarMarch24.pdf. Accessed April 2, 2020. [Google Scholar]
- 4.Excellus Blue Cross Blue Shield. Excellus BCBS Updates on COVID-19 (Coronavirus). In: Excellus Blue Cross Blue Shield; 2020. Available at: provider.excellusbcbs.com/coronavirus. Accessed March 29, 2020. [Google Scholar]
- 5.Aetna. Coronavirus: We're Here to Help. Aetna; 2020. Available at: www.aetna.com/individuals-families/member-rights-resources/covid19/telemedicine.html. Accessed March 31, 2020. [Google Scholar]
- 6.American Academy of Neurology. Telemedicine and Covid-19 Implementation Guide. 2020. Available at: https://www.aan.com/siteassets/home-page/tools-and-resources/practicing-neurologist–administrators/telemedicine-and-remote-care/20-telemedicine-and-covid19-v103.pdf. Accessed March 26, 2020. [Google Scholar]
- 7.Hampton JR, Harrison MJ, Mitchell JR, Prichard JS, Seymour C. Relative contributions of history-taking, physical examination, and laboratory investigation to diagnosis and management of medical outpatients. Br Med J 1975;2:486–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goetz CG, Tilley BC, Shaftman SR, et al. Movement Disorder Society-Sponsored Revision of the Unified Parkinson's Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 2008;23:2129–2170. [DOI] [PubMed] [Google Scholar]
- 9.Abdolahi A, Scoglio N, Killoran A, Dorsey ER, Biglan KM. Potential reliability and validity of a modified version of the Unified Parkinson's Disease Rating Scale that could be administered remotely. Parkinsonism Relat Disord 2013;19:218–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cedarbaum JM, Stambler N, Malta E, et al. The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 1999;169:13–21. [DOI] [PubMed] [Google Scholar]
- 11.Tarolli CG, Zimmerman GA, Goldenthal S, et al. Video research visits for atypical parkinsonian syndromes among Fox Trial Finder participants. Neurol Clin Pract 2019;10:7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdolahi A, Bull MT, Darwin KC, et al. A feasibility study of conducting the Montreal Cognitive Assessment remotely in individuals with movement disorders. Health Informatics Journal 2016;22:304–311. [DOI] [PubMed] [Google Scholar]
- 13.Ciemins EL, Holloway B, Coon PJ, McClosky-Armstrong T, Min SJ. Telemedicine and the mini-mental state examination: assessment from a distance. Telemed J E Health 2009;15:476–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DeYoung N, Shenal BV. The reliability of the Montreal Cognitive Assessment using telehealth in a rural setting with veterans. J Telemed Telecare 2019;25:197–203. [DOI] [PubMed] [Google Scholar]
- 15.Pendlebury ST, Welch SJ, Cuthbertson FC, Mariz J, Mehta Z, Rothwell PM. Telephone assessment of cognition after transient ischemic attack and stroke: modified telephone interview of cognitive status and telephone Montreal Cognitive Assessment versus face-to-face Montreal Cognitive Assessment and neuropsychological battery. Stroke 2013;44:227–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morrell K, Hyers M, Stuchiner T, et al. Telehealth stroke dysphagia evaluation is safe and effective. Cerebrovasc Dis 2017;44:225–231. [DOI] [PubMed] [Google Scholar]
- 17.Buatois S, Miljkovic D, Manckoundia P, et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J Am Geriatr Soc 2008;56:1575–1577. [DOI] [PubMed] [Google Scholar]
- 18.Zhan A, Mohan S, Tarolli C, et al. Using smartphones and machine learning to quantify Parkinson disease severity: the mobile Parkinson disease score. JAMA Neurol 2018;75:876–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Medical Association. Policy Options for States to Address COVID-19. 2020. Available at: www.ama-assn.org/delivering-care/public-health/policy-options-states-address-covid-19. Accessed May 6, 2020. [Google Scholar]
- 20.Certain liability protection for health care providers during disasters. In. 8.01—Civil Remedies and Procedure 2008. Virginia General Assembly: Code of Virginia. Title 8.01-225.02. Available at: https://law.lis.virginia.gov/vacode/title8.01/chapter3/section8.01-225.02/. Accessed May 6, 2020 [Google Scholar]
- 21.Cuomo AM. Continuing Temporary Suspension and Modification of Laws Relating to the Disaster Emergency. In: Office NYSGs, ed: governor.ny.gov; 2020. Available at: www.governor.ny.gov/news/no-20210-continuing-temporary-suspension-and-modification-laws-relating-disaster-emergency. Accessed March 31, 2020. [Google Scholar]
- 22.An Act to Provide Liability Protections for Health Care Workers and Facilities During the COVID-19 Pandemic. Massachusetts State Legislature. 191st Session. Bill S.2630. Available at: https://malegislature.gov/Bills/191/S2630. Accessed May 6, 2020. [Google Scholar]
- 23.Pew Research Center. Internet/broadband fact sheet. In: Technology PRCI, ed: Pew Research Center; 2019. Available at: www.pewresearch.org/internet/fact-sheet/internet-broadband/. Accessed April 2, 2020. [Google Scholar]
- 24.Anderson M, Perrin A. Nearly one-in-five teens can't always finish their homework because of the digital divide. FacTank: News in the Numbers. 2018. Available at: www.pewresearch.org/fact-tank/2018/10/26/nearly-one-in-five-teens-cant-always-finish-their-homework-because-of-the-digital-divide/. Accessed April 2, 2020.
- 25.Anderson M, Perrin A. Digital divide persists even as lower-income Americans make gains in tech adoption. FacTank: News in the Numbers. 2019. Available at: www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/. Accessed April 2, 2020.
- 26.Perrin A. Digital gap between rural and nonrural America persists. FacTank: News in the Numbers. 2019. Available at: www.pewresearch.org/fact-tank/2019/05/07/digital-divide-persists-even-as-lower-income-americans-make-gains-in-tech-adoption/. Accessed April 2, 2020.
- 27.Pew Research Center. Technology use among seniors. In: Technology PRCI, ed: Pew Research Center; 2017. Available at: www.pewresearch.org/internet/2017/05/17/technology-use-among-seniors/. Accessed April 2, 2020. [Google Scholar]
- 28.Bull MT, Darwin K, Venkataraman V, et al. A pilot study of virtual visits in Huntington disease. J Huntingtons Disease 2014;3:189–195. [DOI] [PubMed] [Google Scholar]
- 29.Beck CA, Beran DB, Biglan KM, et al. National randomized controlled trial of virtual house calls for Parkinson disease. Neurology 2017;89:1152–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martin-Khan M, Flicker L, Wootton R, et al. The diagnostic accuracy of telegeriatrics for the diagnosis of dementia via video conferencing. J Am Med Directors Assoc 2012;13:487.e19–487.e24. [DOI] [PubMed] [Google Scholar]
- 31.Friedman DI, Rajan B, Seidmann A. A randomized trial of telemedicine for migraine management. Cephalalgia 2019;39:1577–1585. [DOI] [PubMed] [Google Scholar]
- 32.Selkirk SM, Washington MO, McClellan F, Flynn B, Seton JM, Strozewski R. Delivering tertiary centre specialty care to ALS patients via telemedicine: a retrospective cohort analysis. Amyotroph Lateral Scler Frontotemporal Degener 2017;18:324–332. [DOI] [PubMed] [Google Scholar]
- 33.Dorsey ER, Wagner JD, Bull MT, et al. Feasibility of virtual research visits in Fox trial finder. J Parkinsons Dis 2015;5:505–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis LE, Coleman J, Harnar J, King MK. Teleneurology: successful delivery of chronic neurologic care to 354 patients living remotely in a rural state. Telemed J E Health 2014;20:473–477. [DOI] [PubMed] [Google Scholar]
- 35.Turner AP, Wallin MT, Sloan A, et al. Clinical management of multiple sclerosis through home telehealth monitoring: results of a pilot project. Int J MS Care 2013;15:8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cialone J, Augustine EF, Newhouse N, Vierhile A, Marshall FJ, Mink JW. Quantitative telemedicine ratings in Batten disease: implications for rare disease research. Neurology 2011;77:1808–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]