Abstract
Nonbacterial thrombotic endocarditis, formerly known as marantic endocarditis, is a very rare complication of advanced malignancy and other hypercoagulable states in which sterile, fibrin vegetations develop on heart valve leaflets. The most common malignancies associated with this entity are lung, pancreatic and gastric cancer. It has also been described as a presentation of COVID-19, which is known to be frequently complicated with coagulopathy and thromboembolic events. We report the case of a 62 year-old female patient newly diagnosed with stage IV gastric cancer and acute SARS-CoV-2 infection, presenting with confusion and homonymous hemianopsia in the setting of multiple acute ischemic strokes complicating a nonbacterial thrombotic mitral endocarditis. Herein, we discuss the underlying pathophysiology and make the hypothesis that SARS-CoV-2 infection could have participated in the pathogenesis of nonbacterial thrombotic endocarditis in our patient suffering from a gastric cancer.
Keywords: Nonbacterial thrombotic endocarditis, Gastric cancer, Acute ischemic stroke, SARS-CoV-2
Introduction
Nonbacterial thrombotic endocarditis (NBTE), formerly known as marantic endocarditis, is a very rare complication of hypercoagulable states in which sterile, fibrin vegetations develop on heart valve leaflets. Those hypercoagulable states include malignancies—mostly lung, pancreatic, gastric cancer and adenocarcinomas of unknown primary site—and systemic lupus erythematosus (Libman–Sacks endocarditis) particularly in the setting of antiphospholipid syndrome [1]. It has also been recently described as a presentation of COVID-19 [2]. Indeed, although coronavirus disease is principally expressed as a pulmonary infection, SARS-CoV-2 infection is frequently complicated with coagulopathy and thromboembolic events [3].
The diagnosis is based on the finding of valvular vegetations on echocardiogram without evidence of systemic infection. Clinical manifestations include those of valvular dysfunction and systemic embolization [1].
The prognosis of NBTE is often poor due to its association with advanced malignancy. Current management focuses on identifying and treating the underlying disease while managing the risk for thromboembolic events with long-term heparin anticoagulation. Surgery is sometimes needed to improve valvular dysfunction [1].
Case report
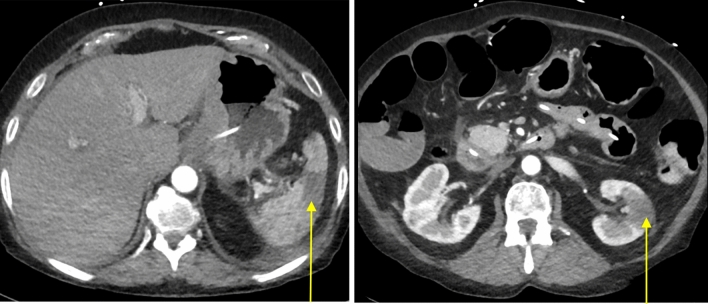
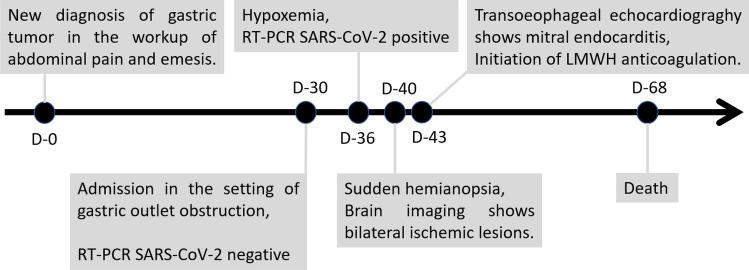
We report the case of a 62 year-old female patient with a newly diagnosed stage IV, microsatellite stable (MSS), poorly differentiated gastric adenocarcinoma and peritoneal carcinomatosis. Her medical history is remarkable for hereditary nonpolyposis colorectal cancer (HNPCC) 20 years before treated by right hemicolectomy, hypertension, type 2 diabetes and dyslipidemia. She was hospitalized to initiate nasojejunal nutrition because of gastric outlet obstruction. During her stay, she developed SARS-CoV-2 infection with low oxygen requirements of 1–2 L per minute. She presented progressive confusion and sudden left homonymous hemianopsia, which motivated a brain computed tomography (CT) that showed hypodense bilateral parieto-occipital lesions. Magnetic resonance imaging (MRI) of the brain further showed multiple lesions ranging from 3 to 45 mm, in hypersignal T2/Flair and DWI (Fig. 1). Those lesions were located bilaterally in the supratentorial region, infratentorial region and brain stem. Since this was compatible with acute ischemic strokes from embolic origin, the patient underwent electrocardiographic monitoring which showed normal sinus rhythm and the absence of atrial fibrillation. Transoesophageal echocardiography was remarkable for a hyperechogenic nodule of 6 mm on the posterior leaflet of the mitral valve (Fig. 2) associated with mild to moderate regurgitation. The left auricle was empty and there was no patent foramen ovale. Serial blood cultures with prolonged incubation returned negative. At this point, a diagnosis of NBTE was made. The eye fundus showed known moderate diabetic retinopathy, but no emboli. The thoraco-abdominal CT-scan showed splenic and left renal infarcts of probable embolic origin (Fig. 3). Treatment consisted in subcutaneous enoxaparin 100 IU/kg bid. Evolution was marked by partial neurological recovery. A control brain MRI showed no new lesions 10 days after anticoagulation was initiated. However, tumor markers had risen steeply with a CEA of 6.9 µg/L and a CA 19.9 of 15,382 kU/L compared to initial dosing at diagnosis 6 weeks before (1.3 µg/L and 205 kU/L, respectively), reflecting the disease aggressiveness. The specific oncologic treatment could not be initiated because of a persistent poor performance status and the patient opted for supportive care. Unfortunately, in the setting of probable rapid oncologic progression, she passed away 3 weeks after NBTE diagnosis and her family declined autopsy. Figure 4 synthesizes the timeline of the above-described events.
Fig. 1.
Brain MRI, axial section, T2/FLAIR and DWI: multifocal and bilateral acute ischemic strokes
Fig. 2.
Transoesophageal echocardiography: hyperechogenic rounded vegetation of 6 mm on the posterior leaflet of the mitral valve
Fig. 3.
Abdominal CT-scan, axial sections, arterial phase: splenic and left renal infarcts
Fig. 4.
Timeline of events. Please note that the patient underwent a staging workup during the first month after initial upper gastro-intestinal endoscopy, including diagnostic laparoscopy showing peritoneal carcinomatosis. D day, LMWH low-molecular-weight heparin
Discussion
The patient’s medical history is remarkable for a colon cancer 20 years before, which was treated by right hemicolectomy. Back then, because she met the Amsterdam criteria [4], she underwent genetic testing on a blood sample that showed a causal mutation in MLH1 and confirmed the diagnosis of HNPCC (Lynch syndrome). Unfortunately, she was lost to follow-up and escaped from advised clinical and endoscopic follow-up. In December 2020, when encountering the antral tumor on endoscopy in the workup of abdominal pain and emesis, we expected the tumor to present microsatellite instability (MSI). However, pathologists report a gastric signet ring cell adenocarcinoma, little cohesive, largely ulcerated, without HER2/neu overexpression and without argument for a MSI-high tumor on immunohistochemistry (nuclear staining of cancer cells with each of the following antigens: MLH1, MSH2, MSH6 and PMS2) nor PCR. This reminds us that not all tumors that arise in patients with Lynch syndrome are secondary to an underlying germline mutation, as mismatch repair (MMR) deficiency and the subsequent accumulation of genetic alterations that eventually leads to carcinoma require loss of function of both alleles of a given gene [5]. In other words, despite carrying one MMR-mutated allele, the MLH1 gene function was not lost by alteration of the second wild-type allele during the carcinogenesis of her gastric cancer.
NBTE is usually diagnosed postmortem and is most commonly associated with malignancy, occurring in 1.2% of all cancer patients (mostly end-stage) in autopsy series [6].
The instigating factor causing NBTE remains unclear, but involves endothelial cell injury in the setting of a hypercoagulable state. The acute injury results in platelet deposition and migration of inflammatory mononuclear cells to form thrombi interwoven with fibrin and immune complexes [7]. In contrast to infective endocarditis, NBTE lesions are sterile, more friable and more prone to systemic embolization. NBTE vegetations commonly involve the mitral and aortic valves and can affect both undamaged and damaged cardiac valves, as well as the chordae tendineae or the endocardium [8].
In malignancy, macrophages interact with malignant cells to release cytokines (tumor necrosis factor, interleukin-1 and 6), which damage endothelium and promote platelet deposition, ultimately forming friable thrombi. Macrophages also interact with tumor cells to over-activate the coagulation cascade, hence, worsening the hypercoagulable state [7].
In COVID-19, other potential causal factors can be identified such as unrestricted angiotensin II action, an increased production of adhesion molecules able to induce vascular inflammation and endothelial activation, complement stimulation, excessive production of neutrophil extracellular traps (NETs), and increased platelet count [3].
Dehydration, acute inflammatory condition, prolonged immobilization, existence of multiple cardiovascular risk factors such as diabetes or hypertension are frequent comorbidities in cancer and in SARS-CoV-2 hospitalized subjects, which might further rise thromboembolic risk.
We, therefore, make the hypothesis that acute SARS-CoV-2 infection, alongside advanced malignancy, might have played a role in the pathogenesis of NBTE in our patient.
Cancer patients are more vulnerable to COVID-19 infection and their disease course is likely to be more aggressive. Risk, clinical features and management of COVID-19 in cancer patients have been discussed in a review by Liu et al. [10]. A retrospective cohort study by Patell et al. (353 patients without cancer and 45 with active cancer) found a similarly high incidence of thrombosis and bleeding among patients admitted with COVID-19 with or without active cancer [11], but the confidence intervals were particularly large and further studies should continue to explore the thrombotic risk in this particular population. Indeed, prothrombotic mechanisms differ in malignancy and COVID-19, and could, therefore, confer additional risk. The latest data about thrombosis and hemostasis issues in cancer patients with COVID-19 state that, as a rule, patients should receive pharmacological venous thromboembolism prophylaxis [12]. Prophylactic daily low-molecular-weight heparins (LMWHs) or twice daily subcutaneous unfractionated heparin (UFH) are recommended by the World Health Organisation [13]. It could be argued that due to very high thrombotic risk, patients with active cancer and severe COVID-19 may need intermediate doses of LMWH [14] and that monitoring anti-Xa levels could be of help to optimize anticoagulation. In case there are contraindications to anticoagulation, mechanical deep-vein thrombosis prophylaxis by intermittent pneumatic compression should be considered [13]. On the basis that SARS-CoV-2 infection activates platelet physiology and that platelets could play a role in multiple stages of cancer progression [15], some teams made the assumption that hyperactive platelets may provide detrimental features for thrombotic and inflammatory conditions in COVID-19-positive patients with malignancy [16]. The efficacy of antiplatelet agents like aspirin, which are effective in blocking the formation of microthrombi and showed to be promising in ongoing COVID-19 studies [17], should also be explored in the treatment of patients with cancer infected with COVID-19. All in all, our observation supports the need for larger studies in the COVID-19-positive cancer population. Rapidly emerging data will hopefully foster management regimens for these patients.
In conclusion, NBTE is a rare entity that should be suspected in every patient with multiple thromboembolic events in the setting of a hypercoagulable state such as cancer or COVID-19 and with sterile microbiologic samples. Early diagnosis is crucial for establishing rapid treatment to prevent further valvular damage and systemic embolization.
Abbreviations
- COVID-19
SARS-CoV-2 disease
- CT
Computed tomography
- DNA
Deoxyribonucleic acid
- DWI
Diffusion-weighed imaging
- HNPCC
Hereditary nonpolyposis colorectal cancer
- LMWH
Low-molecular-weight heparin
- MMR
DNA mismatch repair
- MRI
Magnetic resonance imaging
- MSI
Microsatellite instability
- MSS
Microsatellite stability
- NBTE
Nonbacterial thrombotic endocarditis
- NETs
Neutrophil extracellular traps
- SARS-CoV-2
Severe Acute Respiratory Syndrome Coronavirus 2
- UFH
Unfractionated heparin
Declarations
Conflict of interest
Quentin Binet, Celine Goffinet, Frederique-Estelle Etogo-Asse and Leila Shaza declare that they have no conflict of interest.
Human rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from the patient for being included in this case report.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liu J, Frishman WH. Nonbacterial thrombotic endocarditis: pathogenesis, diagnosis, and management. Cardiol Rev. 2016;24:244–247. doi: 10.1097/CRD.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 2.Balata D, Mellergård J, Ekqvist D, et al. Non-bacterial thrombotic endocarditis: a presentation of COVID-19. Eur J Case Rep Intern Med. 2020;7:001811. doi: 10.12890/2020_001811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allegra A, Innao V, Allegra AG, et al. Coagulopathy and thromboembolic events in patients with SARS-CoV-2 infection: pathogenesis and management strategies. Ann Hematol. 2020;99:1953–1965. doi: 10.1007/s00277-020-04182-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park JG, Vasen HF, Park KJ, et al. Suspected hereditary nonpolyposis colorectal cancer: International Collaborative Group on Hereditary Non-Polyposis Colorectal Cancer (ICG-HNPCC) criteria and results of genetic diagnosis. Dis Colon Rectum. 1999;42:710–715. doi: 10.1007/BF02236922. [DOI] [PubMed] [Google Scholar]
- 5.Hissong E, Baek I, Costa V, et al. Identification of a microsatellite stable, EGFR-mutant lung adenocarcinoma developing in a patient with lynch syndrome. JCO Precis Oncol. 2020;4:818–822. doi: 10.1200/PO.20.00074. [DOI] [PubMed] [Google Scholar]
- 6.González Quintela A, Candela MJ, Vidal C, et al. Non-bacterial thrombotic endocarditis in cancer patients. Acta Cardiol. 1991;46:1–9. [PubMed] [Google Scholar]
- 7.Eiken PW, Edwards WD, Tazelaar HD, et al. Surgical pathology of nonbacterial thrombotic endocarditis in 30 patients, 1985–2000. Mayo Clin Proc. 2001;76:1204. doi: 10.4065/76.12.1204. [DOI] [PubMed] [Google Scholar]
- 8.Roldan CA, Sibbitt WL, Jr, Qualls CR, et al. Libman-Sacks endocarditis and embolic cerebrovascular disease. JACC Cardiovasc Imaging. 2013;6:973–983. doi: 10.1016/j.jcmg.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smeglin A, Ansari M, Skali H, et al. Marantic endocarditis and disseminated intravascular coagulation with systemic emboli in presentation of pancreatic cancer. J Clin Oncol. 2008;26:1383–1385. doi: 10.1200/JCO.2007.12.9148. [DOI] [PubMed] [Google Scholar]
- 10.Liu C, Zhao Y, Okwan-Duodu D, et al. COVID-19 in cancer patients: risk, clinical features, and management. Cancer Biol Med. 2020;17:519–527. doi: 10.20892/j.issn.2095-3941.2020.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patell R, Bogue T, Bindal P, et al. Incidence of thrombosis and hemorrhage in hospitalized cancer patients with COVID-19. J Thromb Haemost. 2020;18:2349–2357. doi: 10.1111/jth.15018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horowitz NA, Brenner B. Thrombosis and hemostasis issues in cancer patients with COVID-19. Semin Thromb Hemost. 2020;46:785–788. doi: 10.1055/s-0040-1714275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. Clinical management of severe acute respiratory infection (SARI) when COVID-19 is suspected. Interim guidance. Available at: https://www.who.int/publications/i/item/clinical-management-of-covid-19. Accessed 25 Mar 2021.
- 14.Eck RJ, Bult W, Wetterslev J, et al. Intermediate dose low-molecular-weight heparin for thrombosis prophylaxis: systematic re-view with meta-analysis and trial sequential analysis. Semin Thromb Hemost. 2019;45:810–824. doi: 10.1055/s-0039-1696965. [DOI] [PubMed] [Google Scholar]
- 15.Lichtenberger LM, Vijayan KV. Are platelets the primary target of aspirin's remarkable anticancer activity? Cancer Res. 2019;79:3820–3823. doi: 10.1158/0008-5472.CAN-19-0762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lichtenberger LM, Vijayan KV. Is COVID-19–induced platelet activation a cause of concern for cancer patients? Cancer Res. 2020;81(5):1209–1211. doi: 10.1158/0008-5472.CAN-20-3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chow JH, Khanna AK, Kethireddy S, et al. Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19. Anesth Analg. 2021;132:930–941. doi: 10.1213/ANE.0000000000005292. [DOI] [PubMed] [Google Scholar]