Abstract
Background
Mitoxantrone hydrochloride injection for lymph tracing (MHI) is a novel lymphatic tracer for sentinel lymph node (SLN) in patients with early breast cancer but exhibited remarkable liver, kidney, and hematologic toxicities in previous studies. Here, the pharmacokinetics and pharmacodynamics profiles of MHI were evaluated to surmise safety and tolerability.
Methods
Phase 1 open-label, single center, and dose escalation study was performed. Ten patients with invasive breast cancer received 0.5, 1.0, or 2.0 mL of MHI into the breast tissues surrounding the tumor for lymphatic mapping. All of these patients were injected with 2 mCi nuclide-labeled sulfur colloid as a self-control 24 to 48 hours before surgery. Safety was assessed by the incidence of adverse events graded by the National Cancer Institute Common Terminology Criteria, version 4.0.3 (CTCAE4.0.3). Blood samples for pharmacokinetic analyses were collected before and after administration at 15, 30, 60, 120, and 240 min of the injection of MHI.
Results
Up to the cutoff date of the study (Aug 8, 2018), no dose-limiting toxic effects or obvious allergic reactions were observed. Only one case of an adverse event was certainly related to MHI, where it caused blue discoloration of the local skin over the injection site after the operation, but this stain gradually went away. The peak level of MHI was achieved after 15–30 min post injection and completely eliminated from the plasma after 60 min. There were no significant differences in the number of lymph nodes detected by MHI and radioactive colloid. Only one patient with lymph node macrometastases had no SLN detected by either the radioactive colloid or the MHI.
Conclusions
At a dose of up to 2.0 mL, MHI was well tolerated and safe for conducting SLN biopsies in patients with breast cancer. Although there was a case with blue discoloration of the local skin over the injection site after the operation, and remained for a short period of time, but the overall safety was acceptable. Here, we approached a novel SLN tracing slant; however, more investigations of MHI should be performed for further evaluations. (Chinadrugtrials.org.cn number: CXHL1301201, Date of registration: October 12, 2015.)
Keywords: Mitoxantrone hydrochloride, breast cancer, lymphatic mapping, sentinel lymph node biopsy (SLNB)
Introduction
Sentinel lymph node biopsy (SLNB) is the current standard of care for axillary nodal staging in clinically axillary node-negative breast cancer patients (1). SLNB is equivalent to axillary lymph node dissection (ALND) in terms of correct staging, prognosis, and treatment pattern, and it offers advantages of lesser morbidity and fewer complications than ALND (2). Currently, the standard of care for sentinel node localization includes a blue dye, radioactive colloid, or a combination of both (3,4).
Despite high rates of SLN detection with these techniques, the current standard tracers have several limitations. The radioactive colloid is limited by patient radiation exposure, and it cannot be performed in institutes without nuclear medicine facilities. The availability of blue dyes is more common rather than radiocolloids, but their accuracy is highly dependent on the surgeons’ experience and also requires subjective visual detection of the SLNs (5). These limitations encourage the performance of studies on novel methods to guide SLNB, such as indocyanine green (ICG) optical imaging and superparamagnetic iron oxide (SPIO) (6). Research performed by Kitai et al. revealed that the detection rate of SLNs with ICG was 94% (6,7). Superparamagnetic iron oxide is equivalent to the Tc99 radiotracer method for identifying SLNs in breast cancer, as previously demonstrated by Rubio et al. (8). However, the entire procedure, including the SLN biopsy, must be conducted under dim light conditions when using ICG as a lymph tracer. Therefore, there is an unmet need to develop new nonradioactive dyes for SLN tracing and identification in patients with breast cancer.
Mitoxantrone is an antineoplastic antibiotic used to treat acute leukemia, lymphoma, prostate and breast cancer (9). Mitoxantrone is generally administered intravenously at various doses, typically ranging from 12 to 14 mg/m2 at monthly cycles to treat prostate cancer and leukemia. It is mainly metabolized by the biliary tract (10-12). Preclinical pharmacodynamic studies of mitoxantrone hydrochloride have shown a high affinity for the lymphatic system after subcutaneous or subserosal administration (12,13).
Based on the animal studies of Mitoxantrone hydrochloride injection for lymph tracing (MHI) for lymphatic tracing conducted by Shenyang Pharmaceutical University, it was found that 5 mg/mL is the most suitable concentration. In a Japanese big-ear white rabbit VX2 breast cancer model test, the tracking requirements were encountered at five minutes after injection. The deepest staining appeared at 30 min. The staining tended to fade at 180 minutes but still met the tracking requirements. The onset time of MHI was comparable to nanocarbon but faster than methylene blue. The duration of MHI staining was longer than methylene blue, but it did not reflect accumulation phenomena like nanocarbon. In addition, mitoxantrone hydrochloride is an organic substance that can be metabolized completely, reducing the risk of clogging the capillaries that may occur when using a nanocarbon as a lymphatic tracer. Therefore, all the above advantages suggest mitoxantrone hydrochloride as a suitable lymphatic tracer for SLNB in patients with early-stage breast cancer.
Previously several animal studies on MHI revealed no mutagenicity, reproductive toxicity, carcinogenicity, or drug dependence potential (14-17) and declared good safety. However, the long-term toxicity study conducted by Shenyang Pharmaceutical University showed that any toxic reactions, including edema, ulcers, and scabs on the mammary glands, quickly resolved within two weeks after ceasing MHI administration. Moreover, this study also suggested that MHI exhibited liver, kidney, and hematologic toxicity (12). To further evaluate the safety and tolerability of MHI used for lymphatic mapping in humans, we conducted this clinical trial. We present the following article in accordance with the MDAR and CONSORT 2010 reporting checklists (available at http://dx.doi.org/10.21037/gs-20-694).
Methods
Study design
This was a phase I open-label, single-center, first-in-human, dose-escalation study. The study was conducted in compliance with local regulations and with the approval of the Medical Ethics Committee of Fudan University Shanghai Cancer Center (number: 1708175-9-1808C). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and the International Conference on Harmonization Guideline for Good Clinical Practice. The primary objective of this study was the assessment of the safety and tolerability of MHI used for lymphatic mapping in patients with breast cancer and its optimal dose determination for a phase II clinical trial. Secondary objectives included assessment of pharmacokinetic parameters and the therapeutic efficacy of the regimen.
Patient eligibility
Female patients aged 18 to 70 years with preoperative histologically confirmed invasive breast cancer who planned to have a mastectomy were included in this study. Their body mass index (BMI) measured by height and weight data (kg/m2) had to be below 35. They could not have any clear contraindications to surgery discovered during routine preoperative examinations. The patients were required to have an adequate hematological, renal, and hepatic function [hemoglobin ≥90 g/L; absolute neutrophil count (ANC) ≥1.5×109/L; platelet count ≥75×109/L; alanine aminotransferase (ALT) and aspartate aminotransferase (AST) ≤1.5 times the upper limit of normal (ULN); serum creatinine (Cr) ≤1.5×ULN]. The patients needed to be able to communicate well with the researchers and complete the study in accordance with research regulations. All the patients were enrolled voluntarily and provided written informed consent.
Exclusion criteria included pregnant or lactating women, patients with a known allergy to anthraquinones, the presence of alcohol or sedative drug dependence, patients with mental illness, any history of pretreatment with the study medication, and any patients who had participated in any other clinical trials within 3 months prior to the study. Any patients who planned to get pregnant during the trial or within 6 months after the study were also excluded.
Surgical procedure
Ten eligible patients numbered 1–10 were randomly divided into 3 groups. Each patient was injected with 2 mCi nuclide-labeled sulfur colloid as self-control into the breast tissue surrounding the tumor 24 to 48 hours before surgery. MHI (5 mg/mL) was injected into the same site approximately 15 min before dissection. Manual massage and compression of the injected breast were then performed for 5 minutes following the injection.
Based on the animal tolerability tests and pharmacokinetics tests in thyroid cancer stage I clinical trials, we used 0.5 mL as the initial dose in this study. Doses were assigned at registration according to the dose-escalation scheme. Three patients were injected with 0.5 mL mitoxantrone hydrochloride for lymphatic tracing at one site. Four patients were injected with 1.0 mL at two sites because one patient in this group failed the lymphoscintigraphy, and three patients were injected with 2.0 mL at 2 sites.
The SLNs were identified with the guidance from the gamma detector probe and the blue-stained lymph vessels. Any blue-stained node, any node with a blue-stained lymphatic channel directly leading to it, any node with radioactive counts 10% or more of the most radioactive node was removed by the surgeon as an SLN. SLN sectioning and processing for histopathological examination was performed using standard protocols. The pathological status of the detected lymph nodes was determined by intraoperative imprint cytology.
Safety assessment
Safety assessments were performed at each study visit, and they included documentations of treatment-emergent adverse events, vital signs, and standard clinical laboratory parameters, as well as findings from physical, cardiac function, etc. Hematological and chemical laboratory assessments were performed at screening and then at follow-up visit on 7±3, 14±3 and 21±3 days after the operation. Adverse events were graded per the National Cancer Institute Common Terminology Criteria, version 4.0.3 (CTCAE4.0.3).
Dose-limiting toxicity (DLT) was defined as any hematologic or dermatological toxicity, which was grade 3 or worse, according to CTCAE. Three patients were treated at any given dose level. If none of the three experienced DLT, then the dose was escalated to the next dose level. If one of the three experienced DLT, then one additional patient was treated at the same dose level, and escalation to the next dose level continued if no DLT occurred in that patient. If two of three or two of four patients experienced DLT, then we planned to stop the higher dose group trial, 2.0 mL in our study.
Pharmacokinetics and efficacy
Blood samples for pharmacokinetic analyses were collected before administration, and at 15, 30, 60, 120, and 240 min after the administration of MHI. Plasma was analyzed for mitoxantrone using liquid chromatography-tandem mass spectrometry (LC-MS/MS) methods. Pharmacokinetic variables were determined from the plasma concentration-time data of all evaluable patients. Pharmacokinetic parameters of MHI included the area under the curve (AUC) of concentration versus the time curve from time zero to the last measurable concentration, maximum observed concentration (Cmax), and time of observed Cmax (Tmax).
We recorded the time to detection of SLNs and the number of resected SLNs. The identification rate was defined as the sum of successfully tracked SLN cases as a percentage of the total number of participants in the trial. The number of lymph nodes identified by MHI was compared with those determined by radioactive colloid to evaluate the efficacy of the MHI.
Statistical methods
In the current study, we study used Prism 8 software for statistical analysis. Outcome indicators were tested for non-inferiority and analyzed by one-sided testing; other indicators were analyzed by two-sided testing. Continuous variables were expressed as mean values or median values, whereas categorical variables were expressed as frequencies. Furthermore, the paired t-test was used to compare the differences between different individuals or dose groups before and after. Counting data were tested by Chi-square test. Quantitative data between groups were tested by one-way analysis of variance. P values less than or equal to 0.05 were considered statistically significant. In the safety tolerance test, for different dose groups, SAS9.13 software was used to perform a one-way analysis of variance on the vital signs before and after administration, laboratory examinations, and changes in electrocardiogram data to determine the above indicators. Whether the change related to the dose. The safety analysis adopts descriptive statistical methods to analyze the relationship between the degree and duration of adverse events and the outcome of the adverse events on a case-by-case basis. Calculate the incidence of adverse events and adverse reactions, the number and frequency of various adverse events and adverse reactions.
Results
Patient demographics
Between December 2017 and August 2018, ten patients were enrolled in this study. Their median age was 47.5 years (range, 36–58 years). All patients were originally diagnosed with invasive breast cancer and underwent core needle biopsy to establish a tissue diagnosis. Three patients were staged clinically as stage I, and seven patients were stage IIa. All of the patients initially underwent a mastectomy and SLN biopsy. One patient was failed to find the sentinel nodes and underwent a subsequent completion axillary dissection. Table 1 summarizes the patients’ general characteristics. All patients were assessable for safety analysis and response. The vital signs of all patients had no significant differences at baseline. Moreover, the Individual Participant data was sharing at “https://www.trialos.com/login/”, and all data were collected by Electronic Data Capture.
Table 1. Patient characteristics.
| Group | No | Age, years | Height (cm) | Weight (kg) | BMIa | Clinical stage | Histological grade | Tumor sizeb | Histological type | Tumor site | Lymph node-positive/SLNs | LVI | Receptor status (%) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ER | PR | Her2 | Ki-67 | |||||||||||||
| 0.5 mL dose | 1 | 36 | 165 | 52 | 19.10 | I | II | 1.5 | IDC | Behind the nipple | 0/4 | – | 80 | 80 | 1+ | 10 |
| 2 | 53 | 165 | 54 | 19.83 | I | III | 2.5 | IDC | Inner upper quadrant | 0/3 | – | 30 | – | 3+ | 30–40 | |
| 3 | 46 | 150 | 59 | 26.22 | IIa | III | 1.5 | IDC | Outer upper quadrant | 0/9 | – | 0 | 0 | 3+ | 10 | |
| 1.0 mL dose | 4 | 55 | 164 | 65 | 24.17 | I | III | 2 | IDC | Outer upper quadrant | –/– | + | 0 | 0 | 1+ | 30 |
| 5 | 58 | 165 | 60 | 22.04 | IIa | II | 2.5 | IDC | Under the nipple | 0/4 | – | 80 | 60 | 2+ | 15 | |
| 6 | 48 | 158 | 65 | 26.04 | IIa | II | 0.2 | IDC | Outer upper quadrant | 0/4 | – | 80 | 60 | 3+ | <10 | |
| 7 | 47 | 160 | 60 | 23.44 | IIa | II | 4 | IDC | Inner | 0/4 | – | 80 | 80 | 2+ | 10 | |
| 2.0 mL dose | 8 | 51 | 160 | 58 | 22.66 | IIa | III | 3 | IDC | Outer upper quadrant | 0/3 | – | 0 | 0 | 2+ | 60 |
| 9 | 45 | 158 | 57.5 | 23.03 | IIa | III | 1.5 | IDC | Outer upper quadrant | 0/5 | – | 0 | 0 | 0 | 50 | |
| 10 | 53 | 160 | 48 | 18.75 | IIa | – | 3 | ILC | Inner upper quadrant | 0/6 | – | 90 | 15 | 1+ | 20 | |
a, BMI = weight (kg)/height2 (m2). b, tumor size was the maximum diameter determined for the pathological specimen. IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma; SLNs, sentinel lymph nodes; LVI, lymphovascular invasion; ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor; BMI, body mass index.
Safety
No drug-limiting toxic effects were observed through the escalation of the dose to 2.0 mL, which was the planned upper limit dose. Therefore, the maximum tolerated dose could not be reached. No adverse systemic or anaphylactic reactions occurred during this study. No patients withdrew from the trial due to adverse events. A summary of adverse events was enlisted in Table 2. In total, there were 21 adverse effects events that occurred in ten patients. Five adverse events occurred in three patients in the 0.5 mL dose group, seven adverse events occurred in the 1.0 mL dose group, and nine adverse events occurred in the 2.0 mL dose group.
Table 2. Adverse effect events.
| Group | No | Adverse effects | Start date | End date | Relationship with MHI | Outcome |
|---|---|---|---|---|---|---|
| 0.5 mL dose | 1 | Pain (II) | 2017-12-15 | 2017-12-24 | Not Relevant | Disappear |
| 1 | Pain (I) | 2017-12-25 | – | Not Relevant | Continue | |
| 2 | Pain (I) | 2018-01-12 | – | Not Relevant | Continue | |
| 2 | Constipation | 2018-01-13 | 2018-01-20 | Not Relevant | Disappear | |
| 3 | Pain (I) | 2018-01-12 | – | Not Relevant | Continue | |
| 1.0 mL dose | 4 | Pain (I) | 2018-02-24 | – | Not Relevant | Continue |
| 4 | Constipation | 2018-02-25 | 2018-02-25 | Not Relevant | Disappear | |
| 4 | Constipation | 2018-02-27 | 2018-02-27 | Not Relevant | Disappear | |
| 5 | Fatigue | 2018-03-15 | – | Not Relevant | Continue | |
| 5 | Pain (I) | 2018-03-13 | 2018-03-26 | Not Relevant | Disappear | |
| 6 | Pain (I) | 2018-03-14 | 2018-03-26 | Not Relevant | Disappear | |
| 7 | Pain (I) | 2018-03-14 | 2018-03-29 | Not Relevant | Disappear | |
| 2.0 mL dose | 8 | Rash | 2018-04-23 | 2018-04-27 | Not Relevant | Disappear |
| 9 | Hyperchlorhydria | 2018-05-18 | 2018-05-19 | Not Relevant | Disappear | |
| 9 | Hyperchlorhydria | 2018-05-27 | 2018-05-27 | Not Relevant | Disappear | |
| 10 | Cough | 2018-05-12 | 2018-05-20 | Not Relevant | Disappear | |
| 10 | Pain (I) | 2018-05-21 | – | Not Relevant | Continue | |
| 10 | Constipation | 2018-05-11 | 2018-05-11 | Not Relevant | Disappear | |
| 10 | Local staining blue | 2018-05-14 | 2018-08-08 | Relevant | Disappear | |
| 10 | Nausea | 2018-06-27 | – | Not Relevant | Continue | |
| 10 | Poor appetite | 2018-06-27 | – | Not Relevant | Continue |
MHI, mitoxantrone hydrochloride injection for lymph tracing.
The most common adverse events were pain at different levels and mild gastrointestinal events, such as constipation, nausea, or poor appetite. Only one adverse event was definitely related to MHI, and it manifested as a blue stain in the local skin over the injection site after surgery. However, the blue stain gradually went away. The skin stain was first discovered on May 14th and had completely disappeared by August 8th, proof of concept for considerable safety regarding MHI administration.
Efficacy
The identification rate of SLNs in this study was 90% (9/10). A total of 35 SLNs (Table 3) were identified in these ten patients (3.5±1.7 SLNs in each patient; range, 2–6). SLNs in three of four patients (75%) were successfully localized by the novel method in the 1.0 mL dose group. The identification rate of SLNs by MHI in the 0.5 and 2.0 mL dose groups was 100% (3/3 cases each). The identification rate of SLN by radioactive colloid was 90% (9/10). SNLs were not found in one patient (No. 4) by either a radioactive colloid or MHI. No statistically significant difference between the two methods was found for the number of SLNs identified.
Table 3. Mode of detection for discovery of SLNs.
| Group | No | Number of SLN localized by MHI | Number of SLN localized by radioactive colloid | P value | Number of SLNs localized by MHI or radioactive colloid | Number of SLNs localized by MHI and radioactive colloid |
|---|---|---|---|---|---|---|
| 0.5 mL dose | 1 | 2 | 3 | 0.184 | 4 | 1 |
| 2 | 2 | 3 | 3 | 2 | ||
| 3 | 2 | 6 | 6 | 2 | ||
| 1.0 mL dose | 4 | 0 | 0 | 0.092 | 0 | 0 |
| 5 | 4 | 3 | 4 | 3 | ||
| 6 | 1 | 3 | 4 | 1 | ||
| 7 | 3 | 4 | 4 | 3 | ||
| 2.0 mL dose | 8 | 1 | 3 | 0.529 | 3 | 1 |
| 9 | 4 | 3 | 5 | 2 | ||
| 10 | 1 | 2 | 2 | 1 | ||
| Total | 20 | 30 | 35 | 16 |
SLN, sentinel lymph node; MHI, mitoxantrone hydrochloride injection for lymph tracing.
Metastases were found in one patient in the 1.0 mL dose group, and she was the case in which no SNLs were found by either tracer method. This was most likely because all of her lymphatic vessels were blocked by carcinoma cells. The pathological report showed that there were 22 metastasis-positive lymph nodes out of 30 lymph nodes obtained by axillary lymph nodes dissection (ALND).
Pharmacokinetic results
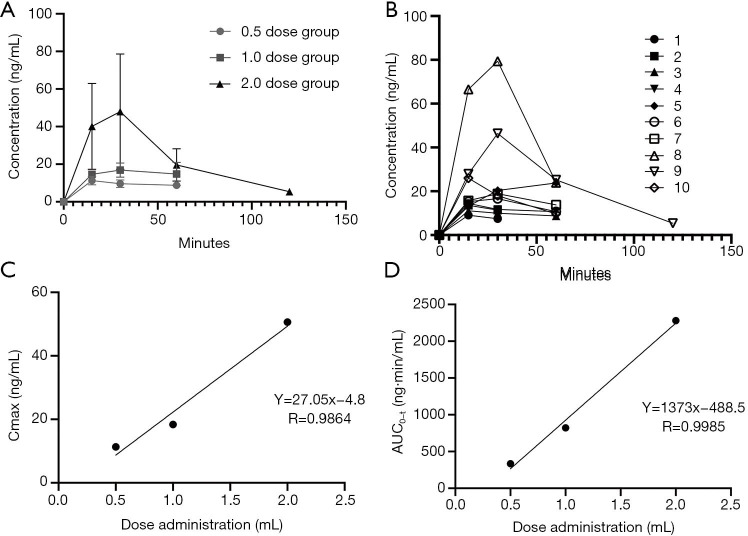
The Cmax detected in the plasma ranged between 9.08 to 13.6 ng/mL for patients receiving the 0.5 mL dose, between 14.4 to 23.8 ng/mL for the 1.0 mL dose group, and between 26 to 79.4 ng/mL for those receiving the 2.0 mL dose of MHI. Results of the individual pharmacokinetic parameters are presented in Table 4. Pharmacokinetic analysis of serum concentration revealed that the Cmax increased with increasing dose (Figure 1). The Cmax of mitoxantrone was reached 15 to 30 min after administration, and mitoxantrone could no longer be detected 60 min after administration. The mean AUC was 335 ng*min/mL in the 0.5 mL dose group, 821 ng*min/mL in the 1.0 mL dose group and 22803 ng*min/mL in the 2.0 mL dose group. These findings suggest that the AUC of the plasma mitoxantrone concentration was generally dose-dependent.
Table 4. Pharmacokinetic parameters.
| Group | No | Tmax (min) | Cmax (ng/mL) | AUC0-t (ng·min/mL) |
|---|---|---|---|---|
| 0.5 mL dose | 1 | 15 | 9.08 | 192 |
| 2 | 15 | 13.6 | 290 | |
| 3 | 15 | 11.1 | 523 | |
| Mean | 15 | 11.3 | 335 | |
| Standard deviation | 0 | 2.3 | 170 | |
| 1.0 mL dose | 4 | 15 | 14.4 | 640 |
| 5 | 60 | 23.8 | 1,014 | |
| 6 | 30 | 16.6 | 764 | |
| 7 | 30 | 18.9 | 868 | |
| Mean | 34 | 18.4 | 821 | |
| Standard deviation | 19 | 4.0 | 159 | |
| 2.0 mL dose | 8 | 30 | 79.4 | 3,143 |
| 9 | 30 | 46.4 | 2,758 | |
| 10 | 15 | 26.0 | 940 | |
| Mean | 25 | 50.6 | 2,280 | |
| Standard deviation | 9 | 26.9 | 1,176 |
Tmax, time when the maximum mitoxantrone concentration was reached; Cmax, maximum concentration; AUC, area under the curve.
Figure 1.
Pharmacokinetic results. (A) The average drug-time curve of the low, medium, and high dose groups after peritumoral injection of mitoxantrone hydrochloride. (B) The average drug-time curve of each subject after peritumoral injection of mitoxantrone hydrochloride. (C) Linear relationship between Cmax and dose administration. (D) Linear relationship between AUC0-t and dose administration. Cmax, the maximum concentrations. AUC, area under the curve.
Discussion
Axillary lymph node status is an important prognostic factor for recurrence and survival in patients with early-stage breast cancer. In recent years, SLNB has become an alternative to ALND. The National Surgical Adjuvant Breast and Bowel Project (NSABP) B32 trial showed that SLNB could achieve the same therapeutic goals as conventional ALND. The overall accuracy of SLN resection in patients with SLNB was 97.1%, and the false-negative rate was 9.8% (18). The use of SLNB instead of ALND can reduce the incidence of complications, such as upper limb lymphedema, dysfunction, and subcutaneous fluid (19).
However, SLNB has not been extensively accepted in the mainland of China. According to a cross-sectional survey of 110 hospitals in China, SLNB was performed in only 63.9% of clinical axillary negative patients. This survey also revealed that 63% (69/110) of the hospitals used methylene blue as a tracer to localize SLNs, and only one hospital used a radioisotope alone to localize SLNs, while 15% (16/110) used a radioisotope combined with methylene blue. The others use fluorescence (5%) or nanocarbon (16%) to localize lymph nodes. The main reason for this is that the radioisotope tracer is not available in many hospitals here and there is also a lack of CFDA-approved dye tracers for SLNB (20,21). Both iso-sulfan blue and patent blue have not been approved by the China Food and Drug Administration (CFDA), and there is also no approved SLN indication for the use of methylene blue in China (22). Therefore, it is an urgent need to develop a novel lymphatic tracer that will be approved by the CFDA.
In the current study, we evaluated the safety and tolerability of MHI used for lymphatic mapping in patients with breast cancer. Preliminary animal experiments showed rapid transit of MHI to the regional nodes and limited systemic biodistribution. The total amount of residual drug in the tissues was only 0.7% of the dose after 24 hours of subcutaneous injection of this product in mice. All patients in the current study underwent a mastectomy and the injection site was removed along with the tumor; theretofore, the amount of drug in the body was extremely low. Compared with the conventional dose used in acute leukemia patients, with a peak concentration of 510±206 ng/mL, the Cmax detected in our study was only 15% of that (23). The maximum tolerated total dose of mitoxantrone intravenous administration for the treatment of ovarian cancer is 75 mg/m2, and the AUC at this dose was 560–1,700 ng/mL, which is 10.7–32.5 times the maximum AUC (3,143 ng min/mL) in our study (24).
Liver, kidney, and hematologic toxicity, which are the dose-limiting toxicities for conventional doses of mitoxantrone, were not observed in this study (24,25). Cady et al. reported that the current blue dyes commonly used, have a risk of allergic reactions in approximately 1% of patients (6,26), and 0.2% have severe reactions, as reported by Krag et al. (18). Allergic reactions ranging from hives and wheals to anaphylactic shock have a 1% to 3% incidence in patients receiving iso-sulfan blue (27). However, these common anaphylactic and allergic reactions to other dyes were not observed in patients using MHI for lymphatic mapping.
A retrospective overview of 3,014 lymphoscintigraphy examinations performed by Coufal et al. revealed that the possible risk factors for failed lymphoscintigraphy include: previous surgery on the breast or the axilla, obstruction of the lymphatic drainage by cancer, and the absence of tracer injection site massage (28). Cox et al. reported that age and BMI had been shown a correlation with an increased incidence of failure in identifying an SLN. They demonstrated that every increase of one year of age or one unit of BMI decreased the odds of success by approximately 5% (29). Fatty tissue around the lymph nodes may cause a decreased flow to the lymphatic basin (30,31). For our patient, her relatively older age (65 years old) and high BMI (15,24) may have contributed to our failure in identifying an SLN. Moreover, excluding possible administration errors, such as using an inadequate volume of injectate, inappropriate timing, and inadequate massage, failed lymphoscintigraphy with MHI and radioactive colloid may be most likely associated with obstruction of the lymphatic channels by tumor cells, since she had 22 positive lymph nodes out of 30 SLNs identified by ALND. In addition, failure may also occur if the injection of either or both dyes enter a biopsy cavity with a mature lining (29). Inflammation around a biopsy site that occludes lymphatic drainage from the area is also a possible reason for failed preoperative lymphoscintigraphy.
This phase I clinical trial still had some limitations. Given that we only enrolled patients undergoing mastectomy, all patients underwent removal of the dyed skin at the site of the MHI. Thus, the assessment of local injury by mitoxantrone, especially any long-term adverse effects, may have some bias and not be accurate enough, and further study is needed to verify its local safety.
Here, we researched an innovative and novel outlook for lymphatic mapping in patients with breast cancer. Compared with the current lymphatic mapping techniques, MHI used for lymph tracking showed good safety and efficacy in patients with breast cancer. A prospective, adequately powered phase II study will be necessary to prove that the identification rate of this novel outlook is equivalent to the current standard of care.
Acknowledgments
Funding: This work was supported by the Shenyang center city hospital emerging frontier technology joint research project (SHDC12015119) and National Key R&D Program of China (2017YFC1311004).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This work has been approved by Medical Ethics Committee of Fudan University Shanghai Cancer Center (No. 1708175-9-1808C). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All patients enrolled voluntarily and provided written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Reporting Checklist: The authors have completed the MDAR and CONSORT 2010 reporting checklists. Available at http://dx.doi.org/10.21037/gs-20-694
Data Sharing Statement: Available at http://dx.doi.org/10.21037/gs-20-694
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-694). The authors have no conflicts of interest to declare.
References
- 1.Veronesi U, Paganelli G, Galimberti V, et al. Sentinel-node biopsy to avoid axillary dissection in breast cancer with clinically negative lymph-nodes. Lancet 1997;349:1864-7. 10.1016/S0140-6736(97)01004-0 [DOI] [PubMed] [Google Scholar]
- 2.Mansel RE, Fallowfield L, Kissin M, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst 2006;98:599-609. 10.1093/jnci/djj158 [DOI] [PubMed] [Google Scholar]
- 3.Lyman GH, Giuliano AE, Somerfield MR, et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol 2005;23:7703-20. 10.1200/JCO.2005.08.001 [DOI] [PubMed] [Google Scholar]
- 4.Ahmed M, Purushotham AD, Douek M. Novel techniques for sentinel lymph node biopsy in breast cancer: a systematic review. Lancet Oncol 2014;15:e351-62. 10.1016/S1470-2045(13)70590-4 [DOI] [PubMed] [Google Scholar]
- 5.Li J, Jia S, Zhang W, et al. Partial axillary lymph node dissection inferior to the intercostobrachial nerves complements sentinel node biopsy in patients with clinically node-negative breast cancer. BMC Surg 2015;15:79. 10.1186/s12893-015-0067-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qiu SQ, Zhang GJ, Jansen L, et al. Evolution in sentinel lymph node biopsy in breast cancer. Crit Rev Oncol Hematol 2018;123:83-94. 10.1016/j.critrevonc.2017.09.010 [DOI] [PubMed] [Google Scholar]
- 7.Kitai T, Inomoto T, Miwa M, et al. Fluorescence navigation with indocyanine green for detecting sentinel lymph nodes in breast cancer. Breast Cancer 2005;12:211-5. 10.2325/jbcs.12.211 [DOI] [PubMed] [Google Scholar]
- 8.Rubio IT, Diaz-Botero S, Esgueva A, et al. The superparamagnetic iron oxide is equivalent to the Tc99 radiotracer method for identifying the sentinel lymph node in breast cancer. Eur J Surg Oncol 2015;41:46-51. 10.1016/j.ejso.2014.11.006 [DOI] [PubMed] [Google Scholar]
- 9.Shenkenberg TD, Von Hoff DD. Mitoxantrone: a new anticancer drug with significant clinical activity. Ann Intern Med 1986;105:67-81. 10.7326/0003-4819-105-1-67 [DOI] [PubMed] [Google Scholar]
- 10.Batra VK, Morrison JA, Woodward DL, et al. Pharmacokinetics of mitoxantrone in man and laboratory animals. Drug Metab Rev 1986;17:311-29. 10.3109/03602538608998294 [DOI] [PubMed] [Google Scholar]
- 11.Ehninger G, Proksch B, Hartmann F, et al. Mitoxantrone metabolism in the isolated perfused rat liver. Cancer Chemother Pharmacol 1984;12:50-2. 10.1007/BF00255910 [DOI] [PubMed] [Google Scholar]
- 12.An G, Morris ME. HPLC analysis of mitoxantrone in mouse plasma and tissues: application in a pharmacokinetic study. J Pharm Biomed Anal 2010;51:750-3. 10.1016/j.jpba.2009.09.027 [DOI] [PubMed] [Google Scholar]
- 13.Subin X, Bin L, Hong Y, et al. Study on the tissue distribution and lymph node targeting of mitoxantrone loaded albumin nanoparticles RP-HPLC method for determination of mitoxantrone in rat plasma and different tissues. Chin J Pharm Anal 2006;26:1043-9. [Google Scholar]
- 14.Bai Y, Wang H, Zhao Q, et al. Security evaluation of mitoxantrone hydrochloride and sodium chloride injection. J Med Pest Control 2011;27:81-2. [Google Scholar]
- 15.Peiling X, Ling H. Development of Anticancer drug Mitoxantrone. Available online: http://g.wanfangdata.com.cn/details/detail.do?_type=perio&id=QK199500808165
- 16.Wang ZD, Ye XL, Yang YX, et al. Comparing study of acute and delayed toxicity of mitoxantrone-polybutycyanoacrylate-nanosphere and mitoxantrone. Sichuan Journal of Physiological Sciences 2009;31:103-4. [Google Scholar]
- 17.Peiling X, Ling H, Bingzhi Q, et al. Development of Anticancer drugs Mitoxantrone. Available online: http://g.wanfangdata.com.cn/details/detail.do?_type=perio&id=QK199500643909
- 18.Krag DN, Anderson SJ, Julian TB, et al. Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III trial. Lancet Oncol 2007;8:881-8. 10.1016/S1470-2045(07)70278-4 [DOI] [PubMed] [Google Scholar]
- 19.Goyal A, Newcombe RG, Chhabra A, et al. Factors affecting failed localisation and false-negative rates of sentinel node biopsy in breast cancer--results of the ALMANAC validation phase. Breast Cancer Res Treat 2006;99:203-8. 10.1007/s10549-006-9192-1 [DOI] [PubMed] [Google Scholar]
- 20.Shen S, Xu Q, Zhou Y, et al. Comparison of sentinel lymph node biopsy guided by blue dye with or without indocyanine green in early breast cancer. J Surg Oncol 2018;117:1841-7. 10.1002/jso.25058 [DOI] [PubMed] [Google Scholar]
- 21.Chen K, Zhu L, Chen L, et al. Circumferential Shaving of the Cavity in Breast-Conserving Surgery: A Randomized Controlled Trial. Ann Surg Oncol 2019;26:4256-63. 10.1245/s10434-019-07725-w [DOI] [PubMed] [Google Scholar]
- 22.Breast Surgery Group, Chinese Medical Association Surgery Branch . Sentinel lymph node biopsy expert consensus and technical operation guidelines for early breast cancer dye method (2018). Chinese Journal of Practical Surgery 2018;38:855-8. [Google Scholar]
- 23.Larson RA, Daly KM, Choi KE, et al. A clinical and pharmacokinetic study of mitoxantrone in acute nonlymphocytic leukemia. J Clin Oncol 1987;5:391-7. 10.1200/JCO.1987.5.3.391 [DOI] [PubMed] [Google Scholar]
- 24.Stiff PJ, McKenzie RS, Alberts DS, et al. Phase I clinical and pharmacokinetic study of high-dose mitoxantrone combined with carboplatin, cyclophosphamide, and autologous bone marrow rescue: high response rate for refractory ovarian carcinoma. J Clin Oncol 1994;12:176-83. 10.1200/JCO.1994.12.1.176 [DOI] [PubMed] [Google Scholar]
- 25.Faulds D, Balfour JA, Chrisp P, et al. Mitoxantrone. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in the chemotherapy of cancer. Drugs 1991;41:400-49. 10.2165/00003495-199141030-00007 [DOI] [PubMed] [Google Scholar]
- 26.Cady B. Consensus on sentinel node biopsy. Breast J 2002;8:123-5. 10.1046/j.1524-4741.2002.08301.x [DOI] [PubMed] [Google Scholar]
- 27.Thevarajah S, Huston TL, Simmons RM. A comparison of the adverse reactions associated with isosulfan blue versus methylene blue dye in sentinel lymph node biopsy for breast cancer. Am J Surg 2005;189:236-9. 10.1016/j.amjsurg.2004.06.042 [DOI] [PubMed] [Google Scholar]
- 28.Coufal O, Zapletal O, Vrtelova P, et al. Failed preoperative lymphoscintigraphy for sentinel lymph node biopsy in breast cancer, possible causes and implications for the surgery - the analysis of 3014 procedures. Rozhl Chir 2015;94:126-30. [PubMed] [Google Scholar]
- 29.Cox CE, Dupont E, Whitehead GF, et al. Age and body mass index may increase the chance of failure in sentinel lymph node biopsy for women with breast cancer. Breast J 2002;8:88-91. 10.1046/j.1524-4741.2002.08203.x [DOI] [PubMed] [Google Scholar]
- 30.Koizumi M, Nomura E, Yamada Y, et al. Sentinel node detection using 99mTc-rhenium sulphide colloid in breast cancer patients: evaluation of 1 day and 2 day protocols, and a dose-finding study. Nucl Med Commun 2003;24:663-70. 10.1097/00006231-200306000-00008 [DOI] [PubMed] [Google Scholar]
- 31.Derossis AM, Fey JV, Cody HS, 3rd, et al. Obesity influences outcome of sentinel lymph node biopsy in early-stage breast cancer. J Am Coll Surg 2003;197:896-901. 10.1016/j.jamcollsurg.2003.08.005 [DOI] [PubMed] [Google Scholar]