Abstract
Fear of COVID-19 is associated with public health compliance but also with negative well-being; however, no articles have reported associations of such fear with perceived benefits and harms. We assessed the level of fear of COVID-19 in Hong Kong adults and its associations with sociodemographic factors and perceived benefits and harms of COVID-19. In a 6-day population-based cross-sectional online survey in May 2020, 4,890 adults provided data on fear and perceived benefits and harms, personal happiness and family well-being, and sociodemographic characteristics. Linear regression was used to analyze associations. The level of fear was moderate (mean score 6.3/10). Fewer respondents reported perceived benefits (10.6%–21.7%) than harms (13.4%–43.5%). Females, younger age groups, and respondents with lower education or more cohabitants had greater fear. Fear was associated with perceived personal (increased knowledge of personal epidemic prevention) and family benefits (improved family hygiene), both with a very small effect size (Cohen’s d = 0.03). Fear was also associated with lower personal happiness and perceived personal (increased negative emotions, feeling depressed and anxious, decreased income, and decreased work efficiency) and family harms (increased conflicts and negative emotions among family members), with small effect sizes (0.08–0.37). We have first shown sociodemographic differences in the fear of COVID-19 and such fear was associated with both perceived personal and family benefits and harms of COVID-19. Our findings may guide the management of fear to reduce sociodemographic differences, and maximize benefits and minimize harms.
Keywords: COVID-19, Fear, Mental health, Perceived benefits and harms, Family, Well-being
Females, younger people, those with lower education or more cohabitants had greater fear of COVID-19. Such fear was associated with both perceived personal and family benefits and harms.
Implications.
Practice: More understanding and support are needed for individuals and groups with risk of greater COVID-19-related fear.
Policy: Policymakers who want to utilize the positive impact of fear to increase public health compliance should take note that such fear can also have negative effects on well-being.
Research: More research on the nature, role, and impact of fear are needed to guide the management of fear to reduce sociodemographic differences, and maximize benefits and minimize harms.
INTRODUCTION
Fear, a natural response triggered in situations such as disease outbreaks and epidemics, serves to keep people away from danger and risky behaviors [1, 2]. Previous reports suggested higher levels of COVID-19-related fear associated with public health compliance and engagement in preventive behaviors such as frequent handwashing [1, 3]. One survey also found fear associated with higher number of workplace infection control measures in response to recent outbreaks [4]. However, chronic or excessive fear can also lead to various psychological disorders [5, 6], whereas widespread public fear can manifest into discrimination and stigmatization of individuals and groups [7, 8]. Several surveys reported the relations of fear of COVID-19 with negative emotions, anxiety, and depression [1, 9–14]. Our search of PubMed and Cochrane Library on October 30, 2020 using keywords including “COVID-19,” “coronavirus,” “fear,” “mental health,” and “well-being” found no articles that reported associations of fear of COVID-19 with both benefits and harms related to personal and family well-being including happiness, hygiene, work-related impacts, and family relationships.
Hong Kong is one of the most westernized and developed cities in China with a population of over 7 million. Despite its close connections with mainland China (and Wuhan, the epicenter of COVID-19), Hong Kong had fewer than 100 confirmed cases from the first case on January 23, 2020 through the end of February [15]. Without any lockdown, such a small first wave could be attributed to social distancing measures and almost 100% voluntary masking [16]. An influx of imported cases from abroad in early March started the “second wave.” Although the local outbreaks were under control with about 1,100 cases by the end of May 2020 (around the end of the second wave) [17], poor emotional well-being such as anxiety and depression in the population were reported [18, 19]. Therefore, assessing and managing fear is a crucial component of outbreak control and health promotion [20, 21].
Under the Hong Kong Jockey Club SMART Family-Link Project (https://www.jcsmartfamilylink.hk/), we conducted the Family Amidst COVID-19 (FamCov) survey in May 2020, after the second wave was under control. This paper aimed to (i) assess the level of fear of COVID-19 in Hong Kong adults after the second wave of the pandemic in May 2020; (ii) examine fear of COVID-19 by different sociodemographic factors; and (iii) analyze the associations of fear of COVID-19 with perceived benefits and harms from COVID-19 and personal and family well-being.
METHODS
Study design and procedures
We conducted FamCov, a population-based cross-sectional online survey, to assess the impact of COVID-19 on families in Hong Kong from May 26–31, 2020 (6 days). We aimed to recruit as many respondents as possible when the second wave was under control as we anticipated another wave could start at any time (which did in early July). The target population was Hong Kong residents aged 18 years and above with one or more family members.
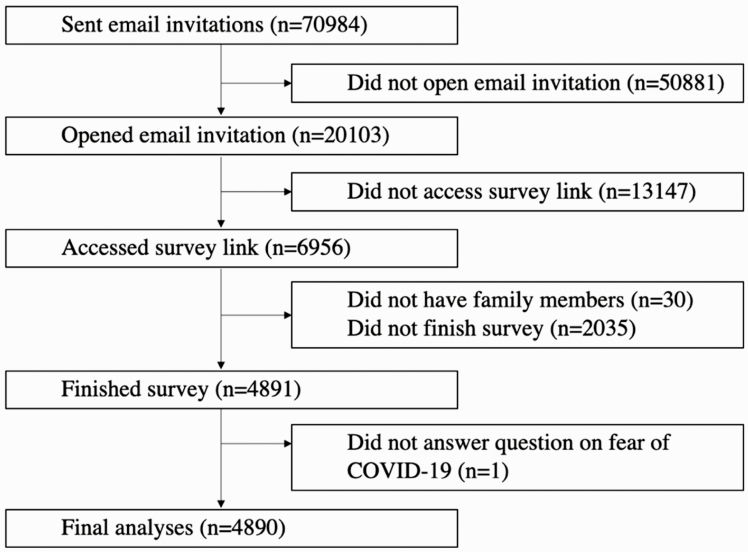
The online survey was distributed through PopPanel, a panel of the general public, both probability and non-probability based, established by the Hong Kong Public Opinion Research Institute (HKPORI), a well-known local survey agency. The probability-based panel included randomly selected individuals who were recruited through telephone surveys and representative of the Hong Kong population, whereas the non-probability-based panel included volunteers who joined through online registration [22]. Panel members are occasionally invited to express their views on different survey topics (https://www.pori.hk/eng/hkpop-panel). All data of the present survey were collected on an online platform constructed and maintained by the University of Hong Kong IT team. The online survey was sent via email invitations to a total of 70,984 adults aged 18 years and above with valid email addresses from the panels. As the email invitations might have been classified as spam and redirected as junk mail, only 20,103 invitation emails were opened and 6,596 survey links were accessed within the 6-day data collection period. A total of 4,891 respondents who fit the inclusion criteria completed the survey. One respondent who did not answer the survey question on fear of COVID-19 was excluded, leaving 4,890 for the final analyses. Figure 1 shows the flow diagram of the survey recruitment process. Ethics approval was obtained from the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (IRB reference no.: UW20-238).
Fig 1.
Flow diagram of the survey recruitment and exclusion process.
Measurements
Fear of COVID-19 was assessed by the question, “Has COVID-19 caused you fear?” on a scale of 0 (no fear at all) to 10 (very fearful). Perceived benefits and harms of COVID-19, both personal and family, were separately assessed by four questions: “What benefits/harms have COVID-19 brought you?” and “What benefits/harms have COVID-19 brought your family?” A list of choices of benefits and harms were provided, and one or more could be selected. Benefits of COVID-19 in the present analyses included increase in knowledge of personal epidemic prevention, improved hygiene, and enhanced resilience. Harms of COVID-19 included decrease in work efficiency and personal income, increase in negative emotions, feeling anxious or depressed, and increase in family conflicts.
Personal and family happiness was assessed by two separate questions, “How happy do you think you are?” and “How happy do you think your family is?” on a scale of 0 (very unhappy) to 10 (very happy). Family health was assessed by asking, “How healthy do you think your family is?” on a scale of 0 (very unhealthy) to 10 (very healthy). Family harmony was also assessed by asking, “How harmonious do you think your family is?” on a scale of 0 (very unharmonious) to 10 (very harmonious). We have used the three family well-being questions in previous papers [23–26], and have also shown that the family happiness question is a reliable and valid measurement tool [24].
Information on six sociodemographic characteristics was collected: sex, age group (18–24 years, 25–34 years, 35–44 years, 45–54 years, 55–64 years, and 65 years and above), education (primary school or lower, secondary, diploma or certificate, associate degree, bachelor’s degree or higher), housing (public housing, subsidized housing [owned], private housing [rented] and private housing [owned]), number of cohabitants (analyzed as both continuous and categorical), and household monthly income (no income, less than HK$4,000, $4,000 to 9,999, $10,000 to 19,999, $20,000 to 29,999, $30,000 to 39,999, and $40,000 or higher; HK$7.8 = US$1). Several variables were recoded: age group (18–34, 35–44, 45–54, 55–64, and 65 years and above), education (secondary or below and post-secondary), and housing (public housing, rented, and owned). Household monthly income per person (income divided by household size) was derived and dichotomized with reference to official median monthly household income figures from the Hong Kong Census and Statistics Department (e.g., HK$28,900 and HK$43,500 for a 2-person and 4-person household in 2019, respectively) into “lower” (less than or equal to the median) or “higher” [27].
Statistical analysis
All statistical analyses were performed using Stata 15.1 for Windows. Results on respondent characteristics, presented as mean and standard deviation or number and percentage, were weighted by sex, age group, and education of the Hong Kong general population to improve their representativeness [28]. Statistical significance was indicated by p < .05.
Linear regression was used to examine the level of fear associated with different variables. We first examined the differences in fear by each of the six sociodemographic variables (sex, age group, education, housing, number of cohabitants, and household monthly income per person) with mutual adjustment. Since fear did not differ by housing and income, only sex, age group, education level, and number of cohabitants were considered potential confounders. Interaction effects between potential confounders were examined by including one interaction term (sex by age/sex by education/sex by number of cohabitants/age by education/age by number of cohabitants/education by number of cohabitants) into the regression model at a time.
Linear regression was also used to examine the differences in the level of fear by a set of dichotomous variables of perceived benefits and harms of COVID-19, and examine the linear association of fear with personal and family well-being, with and without adjusting for potential confounders. Owing to the cross-sectional design of the survey, we focused on the associations of fear with other variables, and not on examining causal relationships between variables or exploring the prediction of perceived harms and benefits in relation to COVID-19. Thus, fear was treated as a dependent variable in the regression analyses for ease of interpretation.
Effect size (Cohen’s d) was computed to quantify the size of differences between two groups, with values of 0.2 to <0.5 considered as small, 0.5 to <0.8 as medium, and 0.8 or above as large [29]. A positive effect size indicated an increase in the level of fear, while a negative effect size indicated a decrease.
RESULTS
Characteristics of survey sample
Table 1 shows that of the 4,890 respondents, after weighting, 47.0% were male, 78.5% were aged 18–64 years, 34.3% had attained secondary or higher education, and 63.4% lived in owned housing. The mean (±standard deviation) number of cohabitants was 2.31 ± 1.31 and 47.4% had higher household monthly income per person. The mean score of fear of COVID-19 was 6.31 ± 2.29. Of the four well-being questions, personal happiness was the lowest (mean: 6.01 ± 2.12). Family health (7.26 ± 1.72) and family harmony (7.26 ± 1.82) scores were the highest, followed by family happiness (6.84 ± 1.83).
Table 1.
Characteristics of the survey sample (N = 4,890)
| Unweighted | Weighteda | |
|---|---|---|
| Sociodemographics | n (%) | n (%) |
| Sex | ||
| Male | 2,137 (43.7) | 2,290 (47.0) |
| Female | 2,753 (56.3) | 2,583 (53.0) |
| Age group, years | ||
| 18–34 | 1,309 (26.8) | 1,167 (23.9) |
| 35–44 | 1,359 (27.8) | 831 (17.0) |
| 45–54 | 1,204 (24.6) | 883 (18.1) |
| 55–64 | 808 (16.5) | 952 (19.5) |
| ≥65 | 210 (4.3) | 1,041 (21.4) |
| Education | ||
| Secondary or below | 658 (13.5) | 3,178 (65.7) |
| Post-secondary | 4,199 (86.5) | 1,662 (34.3) |
| Housing | ||
| Public housing | 771 (16.3) | 1,056 (22.2) |
| Rented | 832 (17.6) | 688 (14.4) |
| Owned | 3,119 (66.1) | 3,021 (63.4) |
| Number of cohabitants (mean ± SD) | 2.33 ± 1.33 | 2.31 ± 1.31 |
| Household monthly income per personb | ||
| Lower | 1,270 (29.8) | 2,201 (52.6) |
| Higher | 2,986 (70.2) | 1,986 (47.4) |
| Well-being | Mean ± SD | Mean ± SD |
| Personal | ||
| Fear of COVID-19c | 6.34 ± 2.20 | 6.31 ± 2.29 |
| Personal happinessd | 5.95 ± 2.11 | 6.01 ± 2.12 |
| Family | ||
| Family happinesse | 6.74 ± 1.92 | 6.84 ± 1.83 |
| Family healthf | 7.15 ± 1.74 | 7.26 ± 1.72 |
| Family harmonyg | 7.10 ± 1.92 | 7.26 ± 1.82 |
| Perceived benefits of COVID-19 | n (%) | n (%) |
| Personal | ||
| Increased knowledge of personal epidemic prevention | 1,259 (26.6) | 1,023 (21.7) |
| Improved personal hygiene | 1,128 (23.9) | 973 (20.7) |
| Enhanced personal resilience | 649 (13.7) | 557 (11.8) |
| Family | ||
| Improved family hygiene | 934 (20.4) | 820 (17.9) |
| Enhanced family resilience | 556 (12.2) | 486 (10.6) |
| Perceived harms of COVID-19 | n (%) | n (%) |
| Personal | ||
| Decreased work efficiency | 1,057 (22.6) | 775 (16.7) |
| Decreased personal income | 1,388 (29.5) | 1,622 (34.9) |
| Increased negative emotions | 2,067 (44.2) | 2,008 (43.5) |
| Feeling anxious | 1,715 (36.4) | 1,613 (34.6) |
| Feeling depressed | 667 (14.2) | 675 (14.5) |
| Family | ||
| Increased family conflicts | 677 (15.3) | 594 (13.4) |
| Increased negative emotions among family members | 1,437 (32.6) | 1,465 (33.3) |
Missing data were excluded.
aData were weighted by sex, age group, and education of the 2019 Hong Kong population.
bIncome divided by household size dichotomized into “lower” (less than or equal to median monthly household income) and “higher.”
cFear of COVID-19: scale of 0 (no fear at all) to 10 (very fearful).
dPersonal happiness: scale of 0 (very unhappy) to 10 (very happy).
eFamily happiness: scale of 0 (very unhappy) to 10 (very happy).
fFamily health: scale of 0 (very unhealthy) to 10 (very healthy).
gFamily harmony: scale of 0 (very unharmonious) to 10 (very harmonious).
More perceived harms (13.4%–43.5%) than benefits (10.6%–21.7%) were reported. Personal benefits reported included increased knowledge of personal epidemic prevention (21.7%), improved personal hygiene (20.7%), and enhanced personal resilience (11.8%). Family benefits were improved family hygiene (17.9%) and enhanced family resilience (10.6%). Personal harms reported included decreased work efficiency (16.7%) and personal income (34.9%), increase in negative emotions (43.5%), and feeling anxious (34.6%) and depressed (14.5%), and family harms included increased family conflicts (13.4%) and negative emotions among family members (33.3%).
Associations with sociodemographic factors
Table 2 shows that females reported greater fear of COVID-19 than males with a very small effect size (6.53 ± 2.11 vs. 6.09 ± 2.29, p < .001, Cohen’s d = 0.09). Fear decreased with age (p for trend < .001). Effect sizes for fear in older age groups compared with the youngest group (18–34 years) ranged from 0.02 to 0.08. Respondents with secondary or below education had greater fear than those with post-secondary education with a very small effect size (6.39 ± 2.33 vs. 6.33 ± 2.18, p = .01, Cohen’s d = 0.09). Fear increased with the number of cohabitants (p for trend < .001). No difference was found for housing and household income. All interaction terms tested between sociodemographic factors were nonsignificant: sex by age (p = .09), sex by education (p = .55), sex by number of cohabitants (p = .45), age by education (p = .39), age by number of cohabitants (p = .38), and education by number of cohabitants (p = .30).
Table 2.
Associations of fear of COVID-19 with sociodemographic factors
| Fear of COVID-19a | ||||
|---|---|---|---|---|
| Adjustedb | ||||
| Mean ± SD | β (95% CI) | p value | Effect sizec | |
| Sex | ||||
| Male | 6.09 ± 2.29 | – | ||
| Female | 6.53 ± 2.11 | 0.42 (0.29, 0.55) | <.001 | 0.09 |
| Age group | ||||
| 18–34 years | 6.55 ± 2.15 | – | ||
| 35–44 years | 6.60 ± 2.08 | 0.13 (−0.05, 0.31) | .17 | 0.02 |
| 45–54 years | 6.21 ± 2.22 | −0.29 (−0.48, −0.09) | .004** | −0.04 |
| 55–64 years | 5.89 ± 2.32 | −0.61 (−0.83, −0.39) | <.001*** | −0.08 |
| ≥65 years | 5.73 ± 2.13 | −0.68 (−1.03, −0.33) | <.001*** | −0.05 |
| p for trend | <.001*** | |||
| Education | ||||
| Secondary or below | 6.39 ± 2.33 | – | ||
| Post-secondary | 6.33 ± 2.18 | −0.27 (−0.48, −0.07) | .01* | −0.04 |
| Housing | ||||
| Public housing | 6.48 ± 2.24 | – | ||
| Rented | 6.42 ± 2.14 | 0.09 (−0.15, 0.33) | .47 | 0.01 |
| Owned | 6.26 ± 2.20 | −0.05 (−0.24, 0.15) | .63 | −0.01 |
| p for trend | .44 | |||
| Number of cohabitants | ||||
| 0 (living alone) | 5.69 ± 2.38 | – | ||
| 1–3 | 6.34 ± 2.19 | 0.57 (0.28, 0.86) | <.001 | 0.05 |
| 4 or more | 6.47 ± 2.17 | 0.66 (0.33, 0.98) | <.001 | 0.06 |
| p for trend | <.001 | |||
| Household monthly income per person | ||||
| Lower | 6.40 ± 2.26 | – | ||
| Higher | 6.28 ± 2.18 | −0.13 (−0.29, 0.02) | .10 | −0.02 |
Missing data were excluded.
aFear of COVID-19: scale of 0 (no fear at all) to 10 (very fearful).
bMutually adjusted by all other sociodemographic factors.
cEffect size (Cohen’s d): small = 0.2 to <0.5, medium = 0.5 to <0.8, large = ≥0.8.
*p < .05, **p < .01, ***p < .001.
Perceived benefits of COVID-19
Table 3 shows greater fear in respondents who reported COVID-19 benefits of increased knowledge of personal epidemic prevention (6.49 ± 2.08 vs. 6.31 ± 2.24, β (95% CI): 0.15 (0.01, 0.29), p = .04), and improved family hygiene (6.50 ± 2.05 vs. 6.32 ± 2.25, β (95% CI): 0.18 (0.02, 0.33), p = .03), with small effect sizes. However, greater fear showed no association with improved personal hygiene, and personal and family resilience.
Table 3.
Associations of fear of COVID-19 with perceived benefits and harms
| Fear of COVID-19a | ||||
|---|---|---|---|---|
| Adjustedb | ||||
| Mean ± SD | β (95% CI) | p value | Effect sizec | |
| Perceived benefits of COVID-19 | ||||
| Personal | ||||
| Increased knowledge of personal epidemic prevention | ||||
| No | 6.31 ± 2.24 | – | ||
| Yes | 6.49 ± 2.08 | 0.15 (0.01, 0.29) | .04* | 0.03 |
| Improved personal hygiene | ||||
| No | 6.33 ± 2.25 | – | ||
| Yes | 6.44 ± 2.05 | 0.10 (−0.05, 0.25) | .19 | 0.02 |
| Enhanced personal resilience | ||||
| No | 6.35 ± 2.22 | – | ||
| Yes | 6.41 ± 2.06 | 0.06 (−0.12, 0.24) | .51 | 0.01 |
| Family | ||||
| Improved family hygiene | ||||
| No | 6.32 ± 2.25 | – | ||
| Yes | 6.50 ± 2.05 | 0.18 (0.02, 0.33) | .03* | 0.03 |
| Enhanced family resilience | ||||
| No | 6.34 ± 2.24 | – | ||
| Yes | 6.45 ± 2.00 | 0.14 (−0.05, 0.34) | .15 | 0.02 |
| Perceived harms of COVID-19 | ||||
| Personal | ||||
| Decreased work efficiency | ||||
| No | 6.22 ± 2.23 | – | ||
| Yes | 6.80 ± 2.07 | 0.51 (0.36, 0.66) | <.001*** | 0.10 |
| Decreased personal income | ||||
| No | 6.25 ± 2.20 | – | ||
| Yes | 6.60 ± 2.20 | 0.37 (0.23, 0.51) | <.001*** | 0.08 |
| Increased negative emotions | ||||
| No | 5.76 ± 2.26 | – | ||
| Yes | 7.07 ± 1.89 | 1.28 (1.16, 1.40) | <.001*** | 0.30 |
| Feeling anxious | ||||
| No | 5.75 ± 2.19 | – | ||
| Yes | 7.39 ± 1.82 | 1.61 (1.49, 1.73) | <.001*** | 0.37 |
| Feeling depressed | ||||
| No | 6.15 ± 2.18 | – | ||
| Yes | 7.55 ± 1.96 | 1.37 (1.20, 1.55) | <.001*** | 0.22 |
| Family | ||||
| Increased family conflicts | ||||
| No | 6.21 ± 2.21 | – | ||
| Yes | 7.12 ± 2.04 | 0.75 (0.57, 0.93) | <.001*** | 0.12 |
| Increased negative emotions among family members | ||||
| No | 6.03 ± 2.21 | – | ||
| Yes | 7.06 ± 1.99 | 1.05 (0.92, 1.19) | <.001*** | 0.22 |
Missing data were excluded.
aFear of COVID-19: scale of 0 (no fear at all) to 10 (very fearful).
bAdjusted for sex, age group, education, and number of cohabitants.
cEffect size (Cohen’s d): small = 0.2 to <0.5, medium = 0.5 to <0.8, large = ≥0.8.
*p < .05, ***p < .001.
Perceived harms of COVID-19
Table 3 also shows that, for personal work-related impacts, fear was greater among respondents who reported decreased work efficiency (6.80 ± 2.07 vs. 6.22 ± 2.22, β (95% CI): 0.51 (0.36, 0.66), p < .001), and decreased personal income (6.60 ± 2.20 vs. 6.25 ± 2.20, β (95% CI): 0.37 (0.23, 0.51), p < .001). For personal psychological impacts, fear was greater in respondents who reported COVID-19 harms of feeling depressed (7.55 ± 1.96 vs. 6.15 ± 2.18, β (95% CI): 1.37 (1.20, 1.55), p < .001, Cohen’s d = 0.22), anxious (7.39 ± 1.82 vs. 5.75 ± 2.19, β (95% CI): 1.61 (1.49, 1.73), p < .001, Cohen’s d = 0.37), and increased negative emotions (7.07 ± 1.89 vs. 5.76 ± 2.26, β (95% CI): 1.28 (1.16, 1.40), p < .001, Cohen’s d = 0.30). For family harms, fear was greater in respondents who reported increased family conflicts (7.12 ± 2.04 vs. 6.21 ± 2.20, β (95% CI): 0.75 (0.57, 0.93), p < .001, Cohen’s d = 0.12) and increased negative emotions among family members (7.06 ± 1.99 vs. 6.03 ± 2.21, β (95% CI): 1.05 (0.92, 1.19), p < .001, Cohen’s d = 0.22).
Similar findings were found in the analyses without adjusting for potential confounders and are not shown.
Personal and family well-being
Table 4 shows that fear of COVID-19 was negatively associated with personal happiness scores (β (95% CI): −0.10 (−0.13, −0.07), p < .001). Fear was also negatively associated with lower family happiness (β (95% CI): −0.04 (−0.07, −0.01), p = .01) and family health (β (95% CI): −0.07 (−0.10, −0.03), p < .001) scores in the crude analyses, but the associations became nonsignificant in the adjusted models. No association was found for family harmony.
Table 4.
Associations of fear of COVID-19 with personal and family well-being
| Fear of COVID-19a | ||
|---|---|---|
| Adjustedf | ||
| β (95% CI) | p value | |
| Personal and family well-being | ||
| Personal happinessb | −0.10 (−0.13, −0.07) | <.001*** |
| Family happinessc | −0.02 (−0.06, 0.01) | .18 |
| Family healthd | −0.03 (−0.07, 0.003) | .07 |
| Family harmonye | 0.01 (−0.02, 0.04) | .51 |
Missing data were excluded.
aFear of COVID-19: scale of 0 (no fear at all) to 10 (very fearful).
bPersonal happiness: scale of 0 (very unhappy) to 10 (very happy).
cFamily happiness: scale of 0 (very unhappy) to 10 (very happy).
dFamily health: scale of 0 (very unhealthy) to 10 (very healthy).
eFamily harmony: scale of 0 (very unharmonious) to 10 (very harmonious).
fAdjusted for sex, age group, education, and number of cohabitants.
***p < .001.
Discussion
This is the first report showing sociodemographic differences in the fear of COVID-19 and that such fear was associated with both perceived personal and family benefits and harms of COVID-19, with greater effect sizes for harms than benefits. Our survey found a moderate level of fear of COVID-19 with a mean score of 6.3 out of 10 when the second wave of COVID-19 in Hong Kong was under control at about 4 months after the first confirmed case was reported.
Females, younger age groups, and respondents with lower education had greater fear of COVID-19. Our results are corroborated by other COVID-19-related reports [10, 11]. Females are more prone to phobic fears, and they perceive greater threats than men [30]. Sex differences in fear can be seen in childhood and may be explained by heightened biological responses in females [31]. We expected older adults would have greater fear of COVID-19 due to increased vulnerability and mortality risk, but conversely, they showed the least fear. Unlike residents of nursing homes at risk of cross infections, our older respondents were home-dwelling with physical and mental health conditions good enough to complete an online questionnaire. Instead, respondents aged 35–44 years showed the greatest fear. This age group most likely consisted of young working parents who needed to care for small children and elderly parents. The 18- to 34-year age group had the second greatest fear, probably because social distancing and isolation might seriously disrupt their normal socializing activities for extended periods of time, and being children then in 2003, they lacked the successful experience of overcoming the SARS epidemic in Hong Kong. Respondents with lower education had greater fear, which was also found in a previous survey [32], most likely due to less knowledge and limited understanding about the virus. Those living with others had greater fear than those living alone, probably from fear of infecting others with COVID-19 and vice versa. However, the differences were very small probably because the two waves of the outbreak in Hong Kong were small and under control with almost 100% voluntary masking and no lockdown [16]. We were surprised to find no differences in fear among respondents living in different types of housing. As Hong Kong is a very densely populated city with an average household median accommodation size in 2016 of 40 square meters (equivalent to around 430 square feet) [33], public housing, rented, and owned properties are all similarly small. More understanding and support are needed for individuals and groups with risk of greater COVID-19-related fear.
Our results further support previous COVID-19 study findings regarding the dichotomous role of fear with positive and negative impacts on emotions and behaviors. For perceived benefits, we found that respondents with greater fear reported increased knowledge of epidemic prevention and improved personal hygiene, but with very small effect sizes. Previous studies found that higher levels of COVID-19-related fear were associated with higher public health compliance and engagement in preventive behaviors such as frequent handwashing, social distancing, and avoidance of public transportation [1, 3]. Our weak associations were probably due to ubiquitous anti-epidemic behaviors in the whole population [15].
For perceived harms, our findings on the associations between fear of COVID-19 and poor personal well-being are consistent with recent reports showing associations of fear of COVID-19 with increased anxiety and depression [1, 10, 11, 14], negative emotions, and overall decreased physical well-being and quality of life [1, 9, 10]. Though happiness was shown to decrease with increase in perceived risk of COVID-19 [21], we further showed that higher levels of fear of COVID-19 were associated with lower personal happiness. We also showed higher levels of fear in respondents with decreased personal income and work efficiency during the pandemic. Previous reports found an association between fear and job insecurity [34], and interaction between fear of COVID-19 and perceived job insecurity in affecting depressive symptoms [35]. We are also the first to show that respondents with more fear reported increased family conflicts and negative emotions among family members. More support for families is needed. Policymakers who want to utilize the positive impact of fear to increase public health compliance should take note that such fear can also have negative effects on well-being.
Overall, the effect sizes of the association of fear of COVID-19 with perceived harms, though small, were much greater than those with perceived benefits. As the prevalence of masking, hand hygiene, and other preventive behaviors were already very high [15], instilling more fear would not motivate more engagement, but could be important to encourage perseverance to counteract “anti-epidemic fatigue” when the pandemic drags on for much longer than expected. Further studies are needed on the nature, role, and impact of fear, on a sensible or appropriate level of fear to reduce sociodemographic differences and motivate positive behaviors without causing excessive harms, and the types of fear that can lead to different positive and negative outcomes. How fear should be measured, monitored, and managed must be considered as an integral part of pandemic control policies.
Limitations
Our study had a few limitations. First, causal relationships cannot be inferred from the cross-sectional design of the survey. Second, all outcomes were self-reported, which might lead to recall bias. However, the use of self-reported questions to collect information from the public is common because of its convenience and low cost. Third, we did not use a validated scale to assess fear of COVID-19 as it was not yet available when the survey was developed. However, our simple 1-item scale did yield useful results. Fourth, we did not ask about the specific aspects of COVID-19 that caused fear. Fifth, although the low response rate would limit the generalizability of our results, the large sample size within 6 days would reduce changes of the variables due to the ups and downs of the outbreaks and allowed us to detect associations of smaller effect sizes. Finally, because the online survey had under-sampled people who were older, had lower education and income, generalizability of our results might be limited. However, despite the sociodemographic differences between our sample when unweighted and weighted, the results of the key variables were similar.
CONCLUSIONS
The COVID-19 pandemic led to a moderate level of fear in Hong Kong adults, even after the first two waves of outbreak were controlled and contained. Using simple questions on fear and perceived benefits and harms, we have first shown sociodemographic differences in the fear of COVID-19 and that such fear was associated with both perceived personal and family benefits and harms, and the effect sizes of associations were greater for harms than benefits. Females, younger age groups, and those with lower education or more cohabitants had greater fear. Amidst the growing uncertainty of the pandemic and its impact on daily life, more research on the nature, role, and impact of fear are needed to guide the management of fear to reduce sociodemographic disparities, and maximize benefits and minimize harms.
Acknowledgments
We would like to thank all community participants of the survey and the Jockey Club SMART Family-Link Project team.
Funding: This study was funded by the Hong Kong Jockey Club Charities Trust.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Human Rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author Contributions: S.M.-M.S., T.-H.L., A.Y.-K.L., B.Y.-M.W., M.-P.W., and S.-Y.H. contributed to the conception and design of the study. S.M.-M.S. and A.Y.-K.L. analyzed the data. S.M.-M.S., T.-H.L., and A.Y.-K.L. interpreted the results. S.M.-M.S. wrote the first draft. All authors critically reviewed and approved the final manuscript.
Ethical Approval: Ethical approval was obtained from the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (IRB reference no.: UW20-238).
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
Study registration: This study was not formally registered.
Analytic plan preregistration: The analysis plan was not formally preregistered.
Data availability:
De-identified data from this study are not available in a public archive. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author.
Analytic code availability: Analytic code used to conduct the analyses presented in this study is not available in a public archive. They may be available by emailing the corresponding author.
Materials availability: Materials used to conduct the study are not publicly available.
References
- 1. Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2020:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kok G, Bartholomew LK, Parcel GS, Gottlieb NH, Fernández ME. Finding theory- and evidence-based alternatives to fear appeals: intervention mapping. Int J Psychol. 2014;49(2):98–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yıldırım M, Geçer E, Akgül Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol Health Med. 2021;26(1):35–43. [DOI] [PubMed] [Google Scholar]
- 4. Sasaki N, Kuroda R, Tsuno K, Kawakami N. Workplace responses to COVID-19 associated with mental health and work performance of employees in Japan. J Occup Health. 2020;62(1):e12134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ornell F, Schuch JB, Sordi AO, Kessler FHP. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020;42(3):232–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shin LM, Liberzon I. The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology. 2010;35(1):169–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74(4):281–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yadav S, Rawal G. The current mental health status of Ebola survivors in Western Africa. J Clin Diagn Res. 2015;9(10):LA01–LA02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Satici B, Saricali M, Satici SA, Griffiths MD. Intolerance of uncertainty and mental wellbeing: serial mediation by Rumination and fear of COVID-19. Int J Ment Health Addict. 2020:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bakioğlu F, Korkmaz O, Ercan H. Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int J Ment Health Addict. 2020:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol Trauma. 2020;12(S1):S17–S21. [DOI] [PubMed] [Google Scholar]
- 12. Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ahorsu DK, Lin C-Y, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fitzpatrick KM, Harris C, Drawve G. Living in the midst of fear: depressive symptomatology among US adults during the COVID‐19 pandemic. Depress Anxiety. 2020;37:957–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cheng KK, Lam TH, Leung CC. Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. Lancet. 2020. doi: 10.1016/S0140-6736(20)30918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centre for Health Protection. Latest Situation of Cases of COVID-19 (as of 29 June 2020). Hong Kong. Available at https://www.chp.gov.hk/files/pdf/local_situation_covid19_en_20200629.pdf. Accessibility verified November 7, 2020. [Google Scholar]
- 18. Lee D. Hong Kong third wave: with Covid-19 upending daily life, residents at greater risk of mental health problems, charity warns. South China Morning Post. 2020. Available at https://www.scmp.com/news/hong-kong/society/article/3094695/hong-kong-third-wave-covid-19-upending-daily-life-residents. Accessibility verified November 7, 2020. [Google Scholar]
- 19. Choi EPH, Hui BPH, Wan EYF. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020;17(10):3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Person B, Sy F, Holton K, Govert B, Liang A; National Center for Infectious Diseases/SARS Community Outreach Team . Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis. 2004;10(2):358–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yıldırım M, Güler A. Positivity explains how COVID-19 perceived risk increases death distress and reduces happiness. Pers Individ Dif. 2021;168:110347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hong Kong Public Opinion Research Institute. HKPOP Panel. Available at https://www.pori.hk/eng/hkpop-panel. Accessibility verified November 7, 2020.
- 23. Lai AYK, Lam EYW, Fabrizo C, et al. A community-based lifestyle-integrated physical activity intervention to enhance physical activity, positive family communication, and perceived health in deprived families: a cluster randomized controlled trial. Front Public Health. 2020;8:434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chen S, Wang MP, Ho HCY, et al. Test–retest reliability and validity of a single-item Self-reported Family Happiness Scale in Hong Kong Chinese: findings from Hong Kong Jockey Club FAMILY Project. Quality of Life Research. 2019;28(2):535–543. [DOI] [PubMed] [Google Scholar]
- 25. Ho HC, Mui M, Wan A, et al. Happy family kitchen: a community-based research for enhancing family communication and well-being in Hong Kong. J Fam Psychol. 2016;30(6):752–762. [DOI] [PubMed] [Google Scholar]
- 26. Ho HC, Mui M, Wan A, et al. Happy family kitchen II: a cluster randomized controlled trial of a community-based family intervention for enhancing family communication and well-being in Hong Kong. Front Psychol. 2016;7:638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hong Kong Census and Statistics Department. 2019 Census. Available at https://www.censtatd.gov.hk/hkstat/sub/sp150.jsp?productCode=D5250038. Accessibility verified November 7, 2020.
- 28. Hong Kong Census and Statistics Department. Table 002: population by age group and sex 2019. 2019. Available at https://www.censtatd.gov.hk/hkstat/sub/sp150.jsp?tableID=002&ID=0&productType=8. Accessibility verified November 7, 2020.
- 29. Sullivan GM, Feinn R. Using effect size - or why the P value is not enough. J Grad Med Educ. 2012;4(3):279–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Campbell A. The evolutionary psychology of women’s aggression. Philos Trans R Soc Lond B Biol Sci. 2013;368(1631):20130078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Else-Quest NM, Hyde JS, Goldsmith HH, Van Hulle CA. Gender differences in temperament: a meta-analysis. Psychol Bull. 2006;132(1):33–72. [DOI] [PubMed] [Google Scholar]
- 32. Reznik A, Gritsenko V, Konstantinov V, Khamenka N, Isralowitz R. COVID-19 fear in Eastern Europe: validation of the fear of COVIDs9 scale. Int J Ment Health Addict. 2020:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hong Kong Population By-census. Summary results of 2016 population by-census: e129b. median floor area of accommodation by area of residence, year and household size. 2016. Available at https://www.bycensus2016.gov.hk/en/bc-mt.html?search=E129a. Accessibility verified December 1, 2020.
- 34. Nella D, Panagopoulou E, Galanis N, Montgomery A, Benos A. Consequences of job insecurity on the psychological and physical health of Greek civil servants. Biomed Res Int. 2015;2015:673623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gasparro R, Scandurra C, Maldonato NM, et al. Perceived job insecurity and depressive symptoms among Italian Dentists: the moderating role of fear of COVID-19. Int J Environ Res Public Health. 2020;17(15):5338. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified data from this study are not available in a public archive. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author.
Analytic code availability: Analytic code used to conduct the analyses presented in this study is not available in a public archive. They may be available by emailing the corresponding author.
Materials availability: Materials used to conduct the study are not publicly available.