Abstract
Child care-based interventions offer an opportunity to reach children at a young and impressionable age to support healthy eating and physical activity behaviors. Ideally, these interventions engage caregivers, including both childcare providers and parents, in united effort. This study evaluated the impact of the Healthy Me, Healthy We intervention on children’s diet quality and physical activity. A sample of 853 three- to four-year-old children from 92 childcare centers were enrolled in this cluster-randomized control trial. Healthy Me, Healthy We was an 8-month, social marketing intervention delivered through childcare that encouraged caregivers (childcare providers and parents) to use practices that supported children’s healthy eating and physical activity behaviors. Outcome measures, collected at baseline and post-intervention, assessed children’s diet quality, physical activity, and BMI as well as caregivers’ feeding and physical activity practices. Generalized Linear Mixed Models were used to assess change from baseline to post-intervention between intervention and control arms. No significant changes were noted in any of the outcome measures except for small improvements in children’s sodium intake and select parent practices. Despite the negative findings, this study offers many lessons about the importance and challenges of effective parent engagement which is critical for meaningful changes in children’s health behaviors.
Keywords: Intervention, Early care and education, Nutrition, Feeding practices, Physical activity practices
Implications.
Practice: ECE providers need strategies, resources, and simple messages to help them work collaboratively with parents to support healthy eating and physical activity in children.
Policy: Policymakers who wish to support healthy eating and physical activity in children should promote consistent messaging through guidelines and standards that encourage better partnership and collaboration between ECE providers and parents.
Research: Future researchers should not disregard the usefulness of the social marketing approach within ECE settings based on these null findings, but instead consider how the lessons learned could be used to improve the application of this approach, including how to facilitate ECE provider-parent partnerships and to understand the intensity of intervention needed to impact the downstream audience of children and support their healthy eating and physical activity.
Background
Children undergo rapid growth and development in the first 5 years of life, and behaviors learned during these years have a lasting impact on health habits and outcomes [1]. Diet and physical activity in early childhood predict food preferences and physical activity behaviors in adolescence and adulthood as well as physical and mental health (e.g., obesity, aggression, attention problems) [2–5]. Establishing healthy behaviors early is imperative for health across the lifespan [6]. Sadly, young children fall short of key recommendations [7, 8], consuming few vegetables and whole grains and excessive refined grains and empty calories [9], while also getting insufficient physical activity [10] and excessive sedentary time [11].
Early care and education (ECE) programs are a valuable setting for public health initiatives targeting young children’s diet and physical activity behaviors. Two thirds of 3–5-year-olds in the USA are enrolled in childcare [12], and participation exceeds 95% in countries with universal pre-kindergarten (e.g., France, Belgium, Denmark) [13]. ECE programs are where children spend many of their waking hours [14], eat most of their meals/snacks [15, 16], and get most of their physical activity [17, 18]. ECE program standards recommend serving healthy food, providing active opportunities, using appropriate feeding and physical activity practices, educating children, staff, and families, and using policy to institutionalize these practices [16, 19]. However, compliance with standards is low [20].
ECE programs also provide a conduit to parents, essential partners in interventions to improve children’s diet and physical activity behaviors [21]. Family events, phone calls, home activities, and brochures are among the strategies used, but meaningful engagement has often been elusive [22].
Social marketing [23] provides a systematic approach to intervention development that may improve engagement of ECE providers and parents in support of children’s healthy eating and physical activity. This approach uses commercial marketing principles to create interventions that persuade target audiences to voluntarily adopt desired health behaviors [24]. It requires understanding the perspectives of all target audiences and what drives their behaviors [25]. The National Social Marketing Centre put forward Social Marketing Benchmark Criteria (SMBC) to improve the impact of social marketing interventions, encouraging attention to behavior, customer orientation, theory, insight, exchange, competition, segmentation, and methods mix (i.e., product, price, place, promotion) [25]. Social marketing has been an effective approach in school-based obesity prevention initiatives [26], but its use in ECE settings has been limited [27].
The Healthy Me, Healthy We (HMHW) study [28] is the first randomized control trial to test the effectiveness of a ECE-based nutrition and physical activity social marketing intervention. Participation in the HMHW campaign was hypothesized to improve children’s diet and physical activity behaviors (primary outcomes) and to accomplish this by improving caregivers’ (ECE providers, parents) feeding and physical activity practices.
METHODS
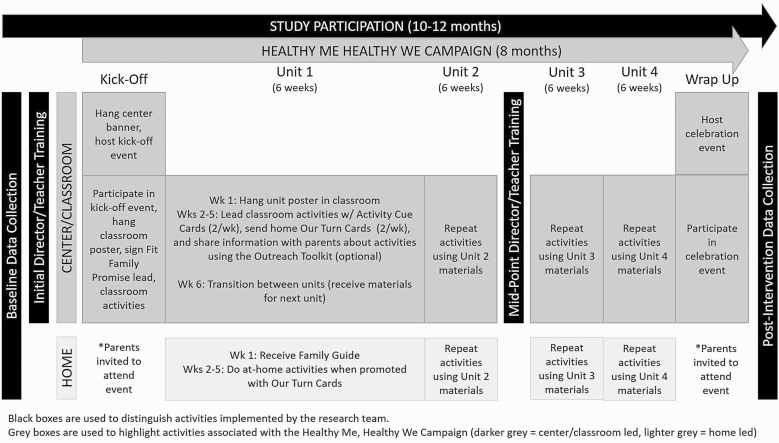
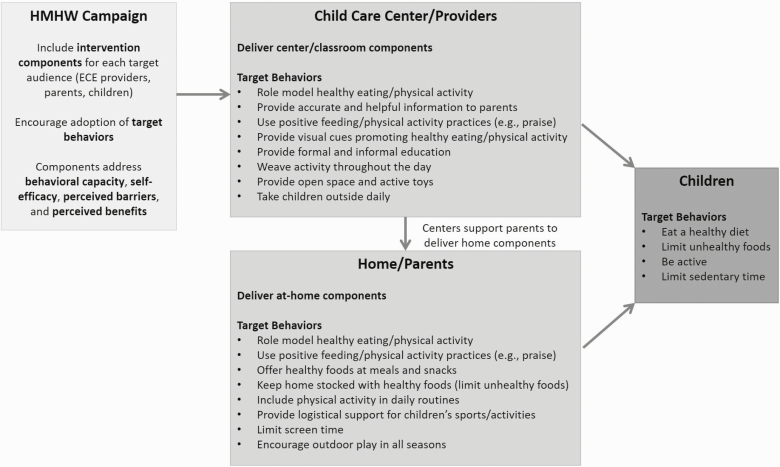
The HMHW study (conducted between 2015 and 2017) used a two-arm cluster-randomized trial to test the effectiveness of the HMHW campaign in increasing children’s diet quality and physical activity compared to control (delayed access). Descriptions of the study design, protocol, formative work, and intervention have been published [28–30]. The study timeline and conceptual model are shown in Figs. 1 and 2, respectively. Protocols were approved by the Institutional Review Board and registered at ClinicalTrials.gov (NCT02330354).
Fig 1.
Healthy Me, Healthy We study timeline including intervention delivery.
Fig 2.
Healthy Me, Healthy We conceptual model.
Participants
Participants included 853 children aged 3–4 years and their parents from 92 childcare centers in North Carolina. Participants were recruited in two waves. Community organizations shared information about the study with local center directors and endorsed participation. Research staff followed-up by phone to gauge initial interest and eligibility (i.e., having a 3–4-year-old classroom, having a 3–5-star quality rating or being exempt from rating, providing lunch, not exclusively serving children with special needs), and then in-person to verify interest and obtain a Memorandum of Understanding.
Information packets were shared with eligible classroom teachers (i.e., 3–4-year-old teacher, able to write/speak English). At least one teacher had to sign consent for the center to remain eligible. Research staff worked with participating teachers to distribute similar packets to eligible parents (i.e., parent of a 3–4-year-old, able to write/speak English) and conduct in-person visits to answer questions and collect written consent. At least seven parents had to sign consent for the center to remain eligible.
Randomization
Centers served as the unit of randomization as the intervention was delivered center wide. Randomization occurred on a rolling basis once baseline measures were collected and sufficient data had been confirmed (i.e., at least 7 children/center with usable diet and physical activity data). Centers were stratified by county, and the study statistician created randomization tables using a permuted block approach (with blocks of two and four). The project manager used these tables to assign centers to the intervention or control arm and informed centers of their arm assignment. Only these team members and those delivering the intervention knew arm assignments; investigators and data collectors remained blinded.
Intervention
The HMHW campaign has been described in detail elsewhere according to TIDieR guidelines [29, 30]. Its development was guided by the social marketing approach, and therefore included a multi-phase process that involved identification of behavioral targets and drivers, formative research, concept development and testing, program development and pilot testing, program refinement, and implementation planning. The 8-month campaign was designed to increase children’s diet quality and physical activity. Development was guided by the Social Marketing Approach [23] and informed by the Social Ecological Framework [31], Exchange Theory [24], and Social Cognitive Theory [32]. While children were the main downstream target audience, ECE providers and parents were recognized as important midstream target audiences that influenced children’s diet and physical activity.
The campaign began with a kick-off event that included hanging the HMHW center banner and classroom posters (1 per classroom), sending invitations to parents, signing the Fit Family Promise (at school and at home), and doing a classroom activity with the HMHW theme song and dance. A welcome letter from Dr. Fitbodi (HMHW mascot) was added in wave 2 to help teachers introduce the campaign.
The kick-off was followed by four 6-week units. During each unit, teachers hung the classroom poster as a visual reminder of unit goals and a prompt for classroom activities. Teachers used activity cue cards (n = 16) to lead eight classroom activities to build children’s knowledge and skills. They also distributed Our Turn cards to prompt parents to do corresponding at-home activities. Parents received a Family Guide magazine at the start of each unit that introduced unit goals, presented benefits of healthier behaviors, encouraged practices to support healthier behaviors, and offered at-home activities. Parents received an activity tracker to log at-home activities. In wave 2, teachers received an outreach toolkit with resources to boost parent engagement (e.g., social media posts about classroom activities).
The campaign concluded with a celebration event which included promoting the event to parents, displaying a certificate of completion, having teachers wear HMHW buttons, posting pictures of activities, having children perform the HMHW song, and awarding children HMHW ribbons.
To support centers’ ability to deliver the campaign, directors and teachers received two trainings and three check-ins by the study interventionist. The first training, delivered prior to the campaign launch, lasted 3 hr, and the second training, delivered halfway through the campaign, lasted 2 hr. Trainings provided general information about childcare’s role in shaping healthy behaviors, introduction to unit themes and campaign components, and skill building (e.g., practice with classroom activities). In wave 2, content was added about boosting parent engagement. Informal check-ins (generally <60 min) occurred after the first training and at the end of units one and three and allowed the interventionist to deliver program materials, offer technical assistance (e.g., assess progress and challenges, offer advice), and inquire about event planning.
Outcome measures
Measures were collected at baseline and post-intervention (about 8–10 months later). Data collection required a 3-day visit to each center to distribute surveys and accelerometers, conduct observations, and collect physical measurements. Visits were conducted by research staff trained and certified on all protocols and blinded to randomization assignment. The study included two primary outcomes—children’s diet quality and minutes of non-sedentary activity—and several secondary outcomes—children’s body mass index (BMI), and caregivers’ nutrition and physical activity practices.
Children’s diet quality
Children’s dietary intakes on two weekdays and one weekend day were assessed using a combination of observation and parent-completed food diaries. Weekday intake at childcare was assessed on days 2 and 3 of the visit using the Diet Observation in Child Care protocol [33]. Weekday intake outside of childcare and weekend intake was assessed by parent-completed food diaries. Parents received food diaries on day 1 and used to record food and beverages consumed outside of childcare on days 2 and 3 of the measurement visit as well as one weekend day. The food diary instructions included a sample day and guidance on estimating serving sizes. When diaries were returned with inadequate information (e.g., incomplete days, missing serving sizes, missing food details), parents were contacted by phone to fill in missing information. Combined diet data were entered into the Nutrition Data System for Research (NDSR, University of Minnesota, Minneapolis) to estimate intakes of energy, macro- and micronutrients, and food group servings. NDSR output data were then used to calculate 2015 Healthy Eating Index (HEI) total score [34], which rates current diet intake against national dietary guidelines on a scale of 0–100. HEI total score was a primary outcome but HEI component scores were also calculated.
Children’s physical activity
Children’s physical activity was assessed with ActiGraph GT3X+ accelerometers (ActiGraph, Pensacola, FL) worn over their right hip for seven days, starting with day 2 of the visit. Parents were provided with an instruction page about the ActiGraph which reminded them to take the monitor off at night but replace it in the morning. Data were downloaded using ActiLife software (ActiGraph, Pensacola, FL). SAS (v9.4) macros were applied to identify sufficient wear (i.e., 6+ hours of waking wear and 3+ wear days) and calculate minutes of sedentary (<25 counts/15 s), light (25–419 counts/15 seconds), moderate (420–841 counts/15 s), and vigorous (≥842 counts/15 s) physical activity using age-appropriate cut points [35–37]. Most children (99%) had 8+ hours of waking wear per day, and 84% had 4+ days of good wear. Given variations in wear time, physical activity outcomes were standardized to average waking wear for the sample (11.5 hr/day). Non-sedentary time was a primary outcome; however, minutes of light/moderate/vigorous activity, counts per minute, and steps were also calculated.
Children’s anthropometrics
Research staff measured children’s standing height to the nearest 1/8 inch with a Seca 123 stadiometer (Seca Corp., Columbia, MD), weight to the nearest 0.1 pound with a Seca 874 electronic scale (Seca Corp., Columbia, MD), and waist circumference to the nearest 0.1 cm with a Gulick II measuring tape. Height and weight were used to calculate BMI; Centers for Disease Control and Prevention’s SAS code and growth charts [38] were used to calculate BMI z-score.
Parent practices
Self-administered surveys were used to assess parents’ feeding and physical activity practices. Existing feeding practice scales were used to assess food availability and preparation [39], encouraging balance and variety [40], modeling [40], nutrition environment [40], and positive family meal patterns [41]. Drawing on existing physical activity practice surveys [42–45], scales were developed for this study to assess facilitation of sports and lessons (2 items, α = 0.842), support for physical activity (11 items, α = 0.887), and weather-related restriction of outdoor play (3 items, α = 0.806).
Child care center practices
The Environment and Policy Assessment and Observation (EPAO) [46] was used to assess child care centers’ nutrition and physical activity practices. This observation and document review were completed during days 2 and 3 of the visit to capture center provisions, teacher practices, professional development, and written policies. Data were collected by trained and certified research staff per EPAO protocols (e.g., instrument overview, in-center observation and practice, certification against gold standard). Data were used to calculate total nutrition environment and total physical activity environment scores as well as 20 component scores.
Additional measures
Self-administered demographic surveys were completed by parents and center directors. Parent demographic surveys captured age, sex, and race/ethnicity of child and parent as well as household income, employment status, and education. The director demographic survey captured information about their center’s quality rating (1–5 stars, increasing stars = increasing quality), national accreditation, acceptance of childcare subsidies, and participation in the Child and Adult Care Food Program (CACFP, federal reimbursement program for food served to low-income children).
Statistical analysis
For each of the two primary outcomes, HEI score and non-sedentary physical activity, the difference in mean change at follow-up between intervention and control arms was compared to assess whether children in the intervention arm improved their HEI score and increased their non-sedentary physical activity more than the children in the control arm. Hypotheses were tested under the intent-to-treat (ITT) principle using Generalized Linear Mixed Models (GLMM) that accounted for the correlation induced by the clustering of children within the childcare centers. Models did not account for clustering of children within classrooms as it is common for children to move between classrooms; hence, this level of clustering was not tracked. Initially, GLMMs were adjusted for child age and sex. Additional baseline variables, identified a priori based on relevancy to change in HEI score and minutes of non-sedentary activity (primary outcomes), were examined and, if significantly different between intervention and control children (i.e., Latino, income), were incorporated as covariates in fully adjusted GLMMs. Differences in secondary outcomes, including child BMI and caregiver feeding and physical activity practices, were analyzed in a parallel fashion.
Power calculation
The final power calculation suggested a sample of 768 children from 96 centers. This sample size provided 80% power to detect a 4-point change in HEI score and 94% power to detect a 1 min/h change in non-sedentary physical activity at a significance level of 0.025 (keeping overall Type 1 error rate at 0.05). Sample size was calculated using a formula from Donner and Klar [47, 48] assuming cluster sizes of 7–9, intra-class correlations (ICC) of 0.15 for HEI score and 0.035 for non-sedentary physical activity (based on previous work in ECEs and the literature [46, 49, 50]), and 20% attrition.
Process evaluation
The process evaluation plan assessed delivery of the intended training and technical assistance by the study interventionist to support center implementation (implementation fidelity). The implementation tracking database captured delivery (and receipt) of intervention components including trainings (e.g., dates offered, lists of participating centers and teachers), technical assistance visits (e.g., dates completed, teachers seen), and provision of program material (e.g., classroom and home materials for all units). Self-administered surveys completed by teachers and parents captured how well the program addressed determinants of targeted behaviors (e.g., “The program helped me [teacher] feel more confident when sharing information with families about healthy eating habits in children”).
RESULTS
Characteristics of study participants are provided in Table 1. The 853 children were, on average, 47.9 months old and included roughly equal numbers of boys and girls (51% vs. 49%). Children were predominantly white (46%) or African American (36%). The 853 parents were, on average, 33.5 years old and most were female (85%). Like children, parents were predominantly white (53%) or African American (37%). Of the 92 centers, most had a quality rating of 4 or 5 stars (out of 5, 78%), accepted subsidies (93%), and participated in the Child and Adult Care Food Program (72%). There were slight differences between arms in terms of children’s Latino ethnicity (p = .02), family income (p = .03), and parents’ marital status (p = .04).
Table 1.
Participant characteristics
| Demographic | Overall | Intervention | Control |
|---|---|---|---|
| Children | (n = 853) | (n = 446) | (n = 407) |
| Age in months, Mean (SD) | 47.93 (6.96) | 48.27 (6.99) | 47.55 (6.92) |
| Female, No. (%) | 420 (49.2%) | 211 (47.3%) | 209 (51.4%) |
| Race, No. (%) | |||
| White | 377 (46.4%) | 183 (43.2%) | 194 (49.9%) |
| Black or African American | 295 (36.3%) | 163 (38.4%) | 132 (33.9%) |
| Othera | 141 (17.4%) | 78 (18.4%) | 63 (16.2%) |
| Latino ethnicity, No. (%) | 70 (8.6%) | 48 (11.2%) | 22 (5.7%) |
| BMI (kg/m2), Mean (SD) | 16.26 (1.60) | 16.25 (1.65) | 16.26 (1.54) |
| Parents | (n = 853) | (n = 446) | (n = 407) |
| Age in years, Mean (SD) | 33.46 (7.82) | 32.67 (8.05) | 34.32 (7.48) |
| Female, No. (%) | 702 (85.3%) | 368 (85.2%) | 334 (85.4%) |
| Race, No. (%) | |||
| White | 434 (53.3%) | 217 (51.1%) | 217 (55.8%) |
| Black or African American | 300 (36.9%) | 168 (39.5%) | 132 (33.9%) |
| Othera | 80 (9.8%) | 40 (10.3%) | 40 (9.4%) |
| Latino ethnicity, No. (%) | 51 (6.2%) | 32 (7.5%) | 19 (4.9%) |
| BMI (kg/m2), Mean (SD) | 28.72 (7.29) | 28.29 (7.01) | 29.19 (7.56) |
| Family income, No. (%) | |||
| Under $30,000 | 240 (28.1%) | 144 (32.3%) | 96 (23.6%) |
| $30,000–$59,999 | 156 (18.3%) | 83 (18.6%) | 73 (17.9%) |
| $60,000 | 323 (37.9%) | 156 (35.0%) | 167 (41.0%) |
| Prefer not to answer | 134 (15.7%) | 63 (14.1%) | 71 (17.4%) |
| Marital status, No. (%) | |||
| Single, never married | 261 (31.9%) | 153 (35.7%) | 108 (27.7%) |
| Married or domestic partnership | 477 (58.3%) | 232 (54.2%) | 245 (62.8%) |
| Education, No. (%) | |||
| Some college or less | 326 (38.2%) | 186 (41.7%) | 140 (34.4%) |
| Associate degree | 104 (12.2%) | 53 (11.9%) | 51 (12.5%) |
| College degree or higher | 379 (44.4%) | 183 (41.0%) | 196 (48.2%) |
| Centers | (n = 92) | (n = 48) | (n = 44) |
| Star rating, No. (%) | |||
| 3 stars | 16 (17.4%) | 7 (14.6%) | 9 (20.5%) |
| 4 stars | 22 (23.9%) | 16 (33.3%) | 6 (13.6%) |
| 5 stars | 50 (54.3%) | 24 (50.0%) | 26 (59.1%) |
| Exempt | 4 (4.3%) | 1 (2.1%) | 3 (6.8%) |
| NAEYC accreditation, No. (%) | 21 (23.6%) | 13 (27.7%) | 8 (19.0%) |
| Accepts childcare subsidies, No. (%) | 84 (93.3%) | 42 (91.3%) | 42 (95.5%) |
| Participates in CACFP, No. (%) | 66 (71.1%) | 38 (79.2%) | 28 (63.6%) |
aOther includes American Indian, Alaskan Native, Asian, more than one race, other (write in), and prefer not to answer.
There was no significant difference in change from baseline to post-intervention in children’s HEI score or non-sedentary physical activity between intervention and control arms (Table 2). The observed ICC for change was 0.10 for HEI score (lower than anticipated) and 0.15 for non-sedentary physical activity (higher than anticipated). When HEI component scores were examined, there appeared to be a significant increase in the sodium component score in favor of the intervention arm (difference in mean change = 0.52, p = .029). None of the secondary physical activity outcomes showed statistically significant change. Children’s BMI did not change significantly either.
Table 2 .
Change in children’s nutrition and physical activity behaviors and caregivers’ practices
| Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|
| Baseline mean (SD) | Follow-up mean (SD) | Baseline mean (SD) | Follow-up mean (SD) | Diff in mean change (SE)a | Effect sizea,b | p a | |
| Children | (n = 446) | (n = 407) | |||||
| HEI score | 57.72 (9.73) | 58.33 (10.14) | 57.80 (10.82) | 58.30 (10.19) | 0.22 (0.90) | 0.03 | .808 |
| Non-sed min/day | 323.2 (42.04) | 320.8 (41.74) | 312.6 (41.54) | 311.0 (39.98) | –2.50 (3.23) | 0.09 | .439 |
| BMI | 16.25 (1.65) | 16.27 (1.96) | 16.26 (1.54) | 16.22 (1.70) | 0.06 (0.06) | 0.13 | .270 |
| BMI z-score | 0.40 (1.01) | 0.44 (1.06) | 0.42 (1.00) | 0.45 (1.00) | 0.01 (0.04) | 0.05 | .679 |
| Parents | (n = 446) | (n = 407) | |||||
| Nutrition practices c | |||||||
| Availability and preparation | 4.14 (0.55) | 4.15 (0.61) | 4.14 (0.55) | 4.14 (0.52) | 0.00 (0.04) | 0.00 | .984 |
| Encourage balance/variety | 4.53 (0.53) | 4.59 (0.48) | 4.60 (0.45) | 4.60 (0.44) | 0.09 (0.04) | 0.11 | .018 |
| Modeling nutrition | 4.25 (0.75) | 4.30 (0.73) | 4.32 (0.76) | 4.32 (0.73) | 0.09 (0.06) | 0.08 | .104 |
| Nutrition environment | 3.74 (0.68) | 3.80 (0.72) | 3.78 (0.75) | 3.83 (0.70) | 0.01 (0.05) | 0.01 | .763 |
| Positive family meal patterns | 4.11 (1.28) | 4.16 (1.31) | 4.09 (1.30) | 4.17 (1.34) | –0.01 (0.12) | 0.00 | .962 |
| Physical activity practices d | |||||||
| Facilitation of sports/lessons | 1.61 (1.96) | 1.84 (1.72) | 1.41 (1.85) | 1.65 (1.83) | 0.12 (0.21) | 0.03 | .581 |
| Support for physical activity | 4.10 (0.72) | 4.25 (0.65) | 4.04 (0.68) | 4.12 (0.66) | 0.05 (0.05) | 0.05 | .308 |
| Weather-related restriction of outdoor play | 4.33 (1.06) | 4.23 (1.09) | 4.25 (1.14) | 4.22 (1.11) | –0.16 (0.08) | 0.10 | .040 |
| Child care centers | (n = 48) | (n = 44) | |||||
| Overall nutrition score | 9.66 (2.21) | 9.55 (2.03) | 8.98 (2.13) | 9.02 (1.72) | 0.02 (0.44) | 0.01 | .961 |
| Overall physical activity score | 9.12 (1.78) | 10.61 (1.40) | 9.53 (1.72) | 9.92 (1.93) | 0.75 (0.49) | 0.16 | .133 |
a For child outcomes, the difference in mean change (SE), effect size, and p-value reflect the fully adjusted ITT model, which controls for age sex, family income category, and Latin decent. For parent and center outcomes, the difference in mean change (SE), effect size, and p-value reflect the fully adjusted completers model, which controls for baseline values (when significantly different at baseline) as well as covariates. For parent outcomes, this includes education, race/ethnicity, and BMI. For center outcomes, this includes star rating and participation in CACFP.
bEffect sizes for HEI score and non-sed min/day calculated using Cohen’s d.
cScale scores have potential ranges as follows: availability and preparation (range 1–5.4), encourage balance/variety (1–5), modeling nutrition (1–5), nutrition environment (1–5), and positive family meal patterns (1–11).
dScale scores have potential ranges as follows: facilitation of sports/lessons (0–7), support for physical activity (1–5.45), weather-related restriction of outdoor play (1–6).
The analyses of change in parent practices indicated a significant increase in favor of the intervention arm in encourage balance and variety (diff in mean change = 0.09, p = .018), meaning parents were more likely to encourage their child to eat a variety of healthy foods over unhealthy ones, and weather-related rules for outdoor play (diff in mean change = –0.16, p = .04), meaning parents were more likely to allow outdoor play on wet, rainy, or cold days. No other parent feeding or physical activity practices changed significantly. Analyses of change in center nutrition and physical activity environments also failed to show any significant change in the overall nutrition and physical activity environment score or in any of the component scores.
Process data showed that every center participated in the two prescribed trainings, received the three planned technical assistance visits, and were provided with all campaign materials. Over the two waves, this required 35 trainings and 144 technical assistance visits (45–60 min each). Teacher surveys highlighted some potential deficiencies. There was lower agreement to items about the program helping them (a) find time to support healthy habits despite competing priorities (only 30% and 37% strongly agreed for healthy eating and physical activity, respectively); (b) feel more confident sharing information with parents (only 35% strongly agreed, same for both healthy eating and physical activity); and (c) feel like efforts in the classroom were reinforced at home (only 29% strongly agreed, asked about healthy eating only). Our Turn cards were among the lowest rated components with 37% of teachers noting they needed some or a lot of improvement. Parent surveys confirmed the disconnect between classroom and home. Generally, less than half of parents received the Family Guides (66% for unit 1, 48% for unit 2, 45% for unit 3, 50% for unit 4). Similarly, 55% did not remember receiving any Our Turn Cards, and another 9% reported receiving four or less. Not surprisingly, parents had consistently low agreement about the program helping them change targeted behaviors (<30% of parents strongly agreed with any of these statements).
Discussion
The HMHW study is unique from most other ECE-based child obesity prevention interventions in its rigorous application of the social marketing approach, as most other studies have used only specific elements (e.g., behavior, methods mix, audience segments) [27]. The use of the social marketing approach has advanced the field in terms of understanding challenges to ECE provider-parent partnerships (e.g., ECE providers’ discomfort approaching parents, parents’ discomfort with being approached) [29] and the importance of assessing ECE provider and parent perspectives when developing interventions requiring change in their own behaviors [27]. Real-world interventions like HMHW are very complex as they rely on existing structures and personnel for delivery, which warrants further evaluation of the process data to fully understand the null findings. Despite the lack of significant improvement in either children’s diet quality or physical activity, this study offers many useful lessons for future interventions.
Most ECE-based child obesity prevention interventions to date have used research staff or health experts to deliver the intervention and evaluated the efficacy of the intervention [51]. In contrast, the HMHW study evaluated the effectiveness of a campaign whose components were delivered by ECE providers and parents. Further examination of process evaluation data is warranted to understand whether results represent an ineffective intervention, inadequate implementation, or some combination of both. As noted in recent reviews of implementation strategies employed for ECE-based interventions, such information is critical to understanding how to effectively leverage the ECE setting to support children’s health [52].
One of the major lessons learned is the need for effective parent engagement strategies. Reviews of ECE-based child obesity prevention interventions emphasize its importance and the substantial investment required to make any headway [21, 22]. Previous efforts have relied largely on sending materials home (e.g., newsletter, brochures, posters, cards) [22] which have been described as low-impact strategies [21]. Even when more intense and impactful strategies are used, like family functions and parent trainings, participation is low [21, 22]. The challenge of parent engagement was a consistent theme throughout the HMHW study, arising first during the formative work [29]. Campaign materials offered a variety of resources to support parent engagement, including invitations to the HMHW kick-off event, attractive Family Guide magazines with educational material, Our Turn cards prompting at-home activities, announcements at the start of each new unit, and sample social media posts about classroom activities. In wave 2, trainings were modified to include more time to discuss and practice parent engagement strategies. Even with this multitude of options and training efforts, at-home components failed to make it home or have an impact on parents. These failures may have occurred due to the lack of parent engagement strategies encouraging two-way communication. While many strategies were offered, most were passive (e.g., relying on handouts to parents). Parent engagement remains an area that needs greater research.
Another major lesson learned was the need to streamline the target behaviors and associated messages. In efforts to address the many contributors to children’s poor diet quality and inactivity, target audiences may be overwhelmed with behaviors targeted, none getting sufficient time or attention to support change. HMHW campaign messages tried to address 11 child eating and physical activity behaviors, 18 ECE provider practices, and 14 parent practices. Each campaign promoted diet and physical activity goals; hence, each included a mix of these messages. Given that so few of the intervention components appeared to make it home, messages needed to be repeated in each unit to have any chance of impact, which may explain the improvements observed in the parent practices encourage balance and variety and weather-related rules for outdoor play. For example, each Family Guides included a 2-page spread on accommodating outdoor play given the season and weather. Social marketing campaigns with focused behavioral targets and messages may be more effective, as in Food Friends: Fun with New Foods, which focuses specifically on children’s willingness to try new foods [53].
Conclusions
The HMHW study did not show significant improvements in children’s diet quality or physical activity; however, its application of the social marketing approach helped call attention to the need for strengthening partnerships between ECE providers and parents so they can work together to support healthy behaviors in children. Closer examination of the implementation of HMHW is warranted to understand where implementation may have failed in supporting centers’ and ECE providers’ delivery of the campaign and engagement of parents and children.
Acknowledgements
This study was funded by the National Heart, Lung and Blood Institute [R01HL120969]. Support was also received from the Center for Disease Control and Prevention [U48DP005017] and National Institute of Diabetes and Digestive and Kidney Diseases [P30DK056350].
Compliance with Ethical Standards
Conflicts of Interest: AEV, HHK, RM, RB, JLC, PP, CTL, DH, and DSW declare no conflicts of interest.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Study protocols were approved by the Institutional Review Board at the University of North Carolina at Chapel Hill (13–2379). This article does not contain any studies with animals.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. National Research Council and Institute of Medicine. From Neurons to Neighborhoods: The Science of Child Development. Washington, DC: Board on Children, Youth, and Families, Commission on Behavioral and Social Sciences and Education; 2000. [Google Scholar]
- 2. Nicklaus S. Development of food variety in children. Appetite. 2009; 52(1): 253–255. [DOI] [PubMed] [Google Scholar]
- 3. Jones RA, Hinkley T, Okely AD, Salmon J. Tracking physical activity and sedentary behavior in childhood: a systematic review. Am J Prev Med. 2013; 44(6): 651–658. [DOI] [PubMed] [Google Scholar]
- 4. Funtikova AN, Navarro E, Bawaked RA, Fíto M, Schröder H. Impact of diet on cardiometabolic health in children and adolescents. Nutr J. 2015; 14: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hinkley T, Teychenne M, Downing KL, Ball K, Salmon J, Hesketh KD. Early childhood physical activity, sedentary behaviors and psychosocial well-being: a systematic review. Prev Med. 2014; 62: 182–192. [DOI] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. Vital signs: obesity among low-income, preschool-aged children—United States, 2008–2011. MMWR. 2013; 62(31): 629–634. [PMC free article] [PubMed] [Google Scholar]
- 7. U.S. Department of Health and Human Services, U.S. Department of Agriculture. 2015–2020 dietary guidelines for Americans 2015. Available at http://health.gov/dietaryguidelines/2015/guidelines. Accessibility verified February 10, 2020.
- 8. National Association for Sport and Physical Education. Active Start: A Statement of Physical Activity Guidelines for Children Birth to Five Years. 2nd ed.Reston, VA: NASPE Publications; 2009. [Google Scholar]
- 9. Banfield EC, Liu Y, Davis JS, Chang S, Frazier-Wood AC. Poor adherence to US dietary guidelines for children and adolescents in the national health and nutrition examination survey population. J Acad Nutr Diet. 2016; 116(1): 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Beets MW, Bornstein D, Dowda M, Pate RR. Compliance with national guidelines for physical activity in U.S. preschoolers: measurement and interpretation. Pediatrics. 2011; 127(4): 658–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tandon PS, Zhou C, Lozano P, Christakis DA. Preschoolers’ total daily screen time at home and by type of child care. J Pediatr. 2011; 158(2): 297–300. [DOI] [PubMed] [Google Scholar]
- 12. National Center for Education Statistics. Percentage of 3-, 4-, and 5-year-old children enrolled in preprimary programs, by level of program, attendance status, and selected child and family characteristics: 2016;2017. Available from: https://nces.ed.gov/programs/digest/d17/tables/dt17_202.20.asp. Accessibility verified May 8, 2019.
- 13. Bos JM, Phillips-Fain G, Rein E, Weinberg E, Chavez S.. Connecting All Children to High-Quality Early Care and Education: Promising Strategies from the International Community. Washington, DC: American Institutes for Research; 2016. October. [Google Scholar]
- 14. National Center for Education Statistics. Number of children under 6 years old and not yet enrolled in kindergarten, percentage in center-based programs, average weekly hours in nonparental care, and percentage in various types of primary care arrangements, by selected child and family characteristics: 2016.2017. Available at https://nces.ed.gov/programs/digest/d17/tables/dt17_202.30.asp. Accessibility verified April 3, 2019.
- 15. Benjamin-Neelon SE. Position of the academy of nutrition and dietetics: benchmarks for nutrition in child care. J Acad Nutr Diet. 2018; 118(7): 1291–1300. [DOI] [PubMed] [Google Scholar]
- 16. American Academy of Pediatrics, American Public Health Association, National Resource Center for Health, Safety in Child Care and Early Education. Caring for Our Children: National Health and Safety Performance Standards; Guidelines for Early Care and Education Programs. 3rd ed: Elk Grove Village, IL: American Academy of Pediatrics; Washington, DC: American Public Health Association; 2011. [Google Scholar]
- 17. Hesketh KR, Griffin SJ, van Sluijs EM. UK Preschool-aged children’s physical activity levels in childcare and at home: a cross-sectional exploration. Int J Behav Nutr Phys Act. 2015; 12: 123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Møller NC, Christensen LB, Mølgaard C, Ejlerskov KT, Pfeiffer KA, Michaelsen KF. Descriptive analysis of preschool physical activity and sedentary behaviors - a cross sectional study of 3-year-olds nested in the SKOT cohort. BMC Public Health. 2017; 17(1): 613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Institute of Medicine. Early Childhood Obesity Prevention Policies. Washington, DC: The National Academies Press; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Larson N, Ayers Looby A, Frost N, Nanney MS, Story M. What can be learned from existing investigations of weight-related practices and policies with the potential to impact disparities in US child-care settings? A narrative review and call for surveillance and evaluation efforts. J Acad Nutr Diet. 2017; 117(10): 1554–1577. [DOI] [PubMed] [Google Scholar]
- 21. Ward DS, Welker E, Choate A, et al. Strength of obesity prevention interventions in early care and education settings: a systematic review. Prev Med. 2017; 95(Suppl): S37–S52. [DOI] [PubMed] [Google Scholar]
- 22. Morris H, Skouteris H, Edwards S, Rutherford L. Obesity prevention interventions in early childhood education and care settings with parental involvement: a systematic review. Early Child Dev Care. 2015; 185(8): 1283–1313. [Google Scholar]
- 23. Grier S, Bryant CA. Social marketing in public health. Annu Rev Public Health. 2005; 26: 319–339. [DOI] [PubMed] [Google Scholar]
- 24. Lee N, Kotler P.. Social Marketing: Changing Behaviors for Good. 5th ed.Thousand Oaks, CA: Sage Publications, Inc.; 2015. [Google Scholar]
- 25. National Social Marketing Centre. Social marketing benchmark criteria. Available at file:///C:/Users/avaughn/Downloads/benchmark-criteria-090910%20(2).pdf. Accessibility verified September 25, 2017.
- 26. Aceves-Martins M, Llauradó E, Tarro L, et al. Effectiveness of social marketing strategies to reduce youth obesity in European school-based interventions: a systematic review and meta-analysis. Nutr Rev. 2016; 74(5): 337–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Luecking CT, Hennink-Kaminski H, Ihekweazu C, Vaughn A, Mazzucca S, Ward DS. Social marketing approaches to nutrition and physical activity interventions in early care and education centres: a systematic review. Obes Rev. 2017; 18(12): 1425–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hennink-Kaminski H, Vaughn AE, Hales D, Moore RH, Luecking CT, Ward DS. Parent and child care provider partnerships: protocol for the Healthy Me, Healthy We (HMHW) cluster randomized control trial. Contemp Clin Trials. 2018; 64: 49–57. [DOI] [PubMed] [Google Scholar]
- 29. Hennink-Kaminski H, Ihekweazu C, Vaughn A, Ward DS. Using formative research to develop the healthy me, healthy we campaign: partnering child care and home to promote healthy eating and physical activity behaviors in preschool children. Soc Mar Q. 2018; 24(3): 194–215. [Google Scholar]
- 30. Vaughn AE, Bartlett R, Luecking CT, Hennink-Kaminski H, Ward DS. Using a social marketing approach to develop Healthy Me, Healthy We: a nutrition and physical activity intervention in early care and education. Transl Behav Med. 2019; 9(4): 669–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988; 15(4): 351–377. [DOI] [PubMed] [Google Scholar]
- 32. Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004; 31(2): 143–164. [DOI] [PubMed] [Google Scholar]
- 33. Ball SC, Benjamin SE, Ward DS. Development and reliability of an observation method to assess food intake of young children in child care. J Am Diet Assoc. 2007; 107(4): 656–661. [DOI] [PubMed] [Google Scholar]
- 34. Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the healthy eating index: HEI-2015. J Acad Nutr Diet. 2018; 118(9): 1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring). 2006; 14(11): 2000–2006. [DOI] [PubMed] [Google Scholar]
- 36. Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008; 26(14): 1557–1565. [DOI] [PubMed] [Google Scholar]
- 37. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008; 40(1): 181–188. [DOI] [PubMed] [Google Scholar]
- 38. Centers for Disease Control and Prevention. A SAS Program for the 2000 CDC growth charts (ages 0 to <20 years). Atlanta, GA; 2019. Available at https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessibility verified October 2, 2019.
- 39. Vaughn AE, Dearth-Wesley T, Tabak RG, Bryant M, Ward DS. Development of a comprehensive assessment of food parenting practices: the home self-administered tool for environmental assessment of activity and diet family food practices survey. J Acad Nutr Diet. 2017; 117(2): 214–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Musher-Eizenman D, Holub S. Comprehensive feeding practices questionnaire: validation of a new measure of parental feeding practices. J Pediatr Psychol. 2007; 32(8): 960–972. [DOI] [PubMed] [Google Scholar]
- 41. Lytle LA, Hearst MO, Fulkerson J, et al. Examining the relationships between family meal practices, family stressors, and the weight of youth in the family. Ann Behav Med. 2011; 41(3): 353–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gattshall ML, Shoup JA, Marshall JA, Crane LA, Estabrooks PA. Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. Int J Behav Nutr Phys Act. 2008; 5: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. O’Connor TM, Chen TA, del Rio Rodriguez B, Hughes SO. Psychometric validity of the parent’s outcome expectations for children’s television viewing (POETV) scale. BMC Public Health. 2014; 14: 894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Timperio A, Salmon J, Ball K, et al. Family physical activity and sedentary environments and weight change in children. Int J Pediatr Obes. 2008; 3(3): 160–167. [DOI] [PubMed] [Google Scholar]
- 45. Vaughn AE, Hales DP, Neshteruk CD, Ward DS. Home STEAD’s physical activity and screen media practices and beliefs survey: instrument development and integrated conceptual model. PLoS One. 2019; 14(12): e0226984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ward D, Hales D, Haverly K, et al. An instrument to assess the obesogenic environment of child care centers. Am J Health Behav. 2008; 32(4): 380–386. [DOI] [PubMed] [Google Scholar]
- 47. Donner A, Klar N. Statistical considerations in the design and analysis of community intervention trials. J Clin Epidemiol. 1996; 49(4): 435–439. [DOI] [PubMed] [Google Scholar]
- 48. Donner A, Klar N.. Design and Analysis of Cluster Randomization Trials in Health Research. London, UK: Arnold; 2000. [Google Scholar]
- 49. Ward DS, Vaughn AE, Bangdiwala KI, et al. Integrating a family-focused approach into child obesity prevention: rationale and design for the My Parenting SOS study randomized control trial. BMC Public Health. 2011; 11: 431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Vitolo MR, Rauber F, Campagnolo PD, Feldens CA, Hoffman DJ. Maternal dietary counseling in the first year of life is associated with a higher healthy eating index in childhood. J Nutr. 2010; 140(11): 2002–2007. [DOI] [PubMed] [Google Scholar]
- 51. Matwiejczyk L, Mehta K, Scott J, Tonkin E, Coveney J. Characteristics of effective interventions promoting healthy eating for pre-schoolers in childcare settings: an umbrella review. Nutrients. 2018; 10(3): 293–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Wolfenden L, Barnes C, Jones J, et al. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database Syst Rev. 2020; 2: CD011779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Johnson SL, Bellows L, Beckstrom L, Anderson J. Evaluation of a social marketing campaign targeting preschool children. Am J Health Behav. 2007; 31(1): 44–55. [DOI] [PubMed] [Google Scholar]