Abstract
Attachment insecurity is determined early in life, is a risk factor for psychopathology, and can be measured on two separate continuous dimensions: attachment anxiety and attachment avoidance. Therapeutic changes toward more secure attachment correlate with reduction in psychiatric symptoms. Psilocybin-assisted psychotherapy has demonstrated promise in the treatment of psychopathology, such as treatment-resistant depression and substance use disorders. We hypothesized that psilocybin-assisted psychotherapy would reduce attachment anxiety and attachment avoidance, thus increasing attachment security. We also hypothesized that baseline measures of attachment insecurity, which can reflect a diminished capacity for trust and exploration, would inform the quality of the psilocybin session. Participants were male long-term AIDS survivors with moderate-severe demoralization (n = 18). Using the Experiences in Close Relationships scale, we measured attachment insecurity at baseline as well as immediately, and 3 months, after completion of a brief group therapy course, which included a single midtreatment open-label psilocybin session conducted individually. Clinically important aspects of the psilocybin session were assessed using the revised Mystical Experience Questionnaire and the Challenging Experience Questionnaire the day following psilocybin administration. Self-reported ratings of attachment anxiety decreased significantly from baseline to 3-months post-intervention, t(16) = −2.2; p = 0.045; drm = 0.45; 95% CI 0.01, 0.87. Attachment avoidance did not change significantly. Baseline attachment anxiety was strongly correlated with psilocybin-occasioned mystical-type experiences, r(15) = 0.53, p = 0.029, and baseline attachment avoidance was strongly correlated with psilocybin-related challenging experiences, r(16) = 0.62, p = 0.006. These findings have important implications for the general treatment of psychopathology as well as optimizing psilocybin-assisted psychotherapy as a broadly applicable treatment modality.
Keywords: hallucinogens, psilocybin, object attachment, psychological phenomena, psychotherapy, mysticism
Attachment theory describes how early formative infant-caregiver bonds translate into organized relationship patterns, or working models, in adulthood.1,2 Working models of attachment are influenced by genetic, epigenetic, and environmental factors,3,4 can be reliably measured,5 and link to neural, physiological, and behavioral representations of social approach versus avoidance.6,7 Adult attachment is often categorized into different shorthand “styles”, but is perhaps more precisely described as two separate continuous dimensions—attachment anxiety and attachment avoidance.8Attachment security refers to an ability to seek support from trusted others, who act as a safe haven from distressing stimuli, and to use emotionally intimate relationships as a secure base from which to explore the world.1 Attachment security is associated with low levels of both attachment anxiety and attachment avoidance. Attachment insecurity, on the other hand, reflects high levels of attachment anxiety, attachment avoidance, or both. Elevated attachment anxiety is characterized by worry over the availability of intimate partners and desire for continuous contact and reassurance. Elevated attachment avoidance is characterized by excessive self-reliance and intimacy evasion. Although not considered pathological in and of itself, attachment insecurity predisposes people to various forms of psychopathology, including depression and substance use disorders.9−11 Attachment security, on the other hand, is protective against the development of psychopathology. Finally, working models of attachment are relatively stable;12,13 although they can change over time as a result of significant interpersonal experiences, such as skillfully delivered, typically long-term and intensive, psychotherapy interventions.2,14 Therapeutic changes toward more secure attachment often correlate with reduction in psychiatric symptoms.14 An intervention that could rapidly and durably revise maladaptive working models of attachment are also likely to reduce the symptoms of a broad range of psychiatric disorders.
The past decade has seen a greatly renewed clinical research interest in the therapeutic use of classic psychedelics,15 a group of compounds—including psilocybin, an active component of “magic mushrooms”—that bind at the 5-HT2A serotonin receptor and lead to profound acute changes in consciousness.16 Pure synthetic psilocybin has demonstrated potential for rapidly and durably enhancing psychological flexibility17,18 and has been found to induce long-lasting changes in several domains of otherwise stable personality traits.19 The combination of psychotherapy before, during, and after a psilocybin experience—psilocybin-assisted psychotherapy—has shown promise in treating psychiatric disorders involving inflexibility, such as treatment-resistant depression20 and substance use disorders.21 Bolstering “connectedness” has been proposed as a key component of the therapeutic efficacy of psilocybin-assisted psychotherapy.22−24 “Connectedness” is a somewhat vague concept without a consistent clinical definition. Attachment, however, is a well-researched, evolutionary construct with well-defined mechanisms for connection versus disconnection along with corresponding neural, physiological, and behavioral correlates. We hypothesize that psilocybin-assisted psychotherapy will reduce attachment insecurity. While attachment theory may provide a useful lens through which to better understand the complexities of psilocybin’s effects on connectedness, there is a notable absence in the literature exploring the interaction between psilocybin and attachment theory.
Attachment variables may also help predict important aspects of the psilocybin experience. Therapeutic outcomes are often correlated with the strength of the psilocybin-occasioned ‘mystical-type experience’.16 A critical definitional feature of the mystical experience is a sense of unity, or the experience of interconnectedness with all that exists, which can involve the complete dissolution of the self with loss of all ego boundaries.25 Individuals with high attachment anxiety—given their characteristic overemphasis on proximity maintenance with important others—may be primed to welcome the unity and interconnectedness that can accompany a mystical-type experience, rather than resist or become overwhelmed by its onset. Challenging experiences, another important aspect of psilocybin, might be described colloquially as “bad trips”. Baseline neuroticism has been positively linked to the strength of challenging psilocybin experiences.26 Of note, a strong challenging experience does not necessarily negate therapeutic benefits.27 Individuals with high attachment avoidance, given their inclination to maintain control and remain separate, may have greater challenging experiences with psilocybin. Linking baseline attachment variables to important aspects of the psilocybin experience may help tailor interventions, minimize risk, and contribute to the understanding of underlying mechanisms.
The present study incorporates data from a pilot study28 of psilocybin-assisted psychotherapy with a sample (n = 18) of gay-identified, older, long-term AIDS (acquired immune deficiency syndrome) survivors with moderate to severe demoralization—characterized by poor coping and a sense of helplessness, hopelessness, and a loss of meaning and purpose in life. Treatment involved 4 preparatory group therapy sessions, a single mid-treatment individual psilocybin session (open-label and dosed orally at 0.3–0.36 mg/kg), and 4–6 integrative group therapy sessions. Our previously published clinical findings include notable improvements in demoralization, complicated grief, and post-traumatic stress symptoms.28 Previous research has shown that individuals with greater attachment security adjust better to a diagnosis of HIV (human immunodeficiency virus) or AIDS.29 Collectively, long-term AIDS survivors have experienced a significant history of attachment-related trauma, with loss of loved ones during the early AIDS epidemic as well as rejection by families and communities of origin related to their sexual orientation. Therefore, we felt it was particularly relevant to assess attachment variables in our sample.
Our exploratory analyses assess the following: (1) Does psilocybin-assisted psychotherapy reduce attachment anxiety and attachment avoidance from baseline to 3-month follow-up? (2) Do baseline levels of attachment anxiety and attachment avoidance predict important aspects of the psilocybin experience?
Results and Discussion
Demographics
Table 1. Demographics and Clinical Measurements Demographics.
| demographics | ||
|---|---|---|
| (n = 18) | ||
| age; mean (SD) | 59.2 (4.4) | |
| gender; n (%) | male | 18 (100%) |
| race; n (%) | African American/Black | 1 (5.6%) |
| multiracial | 3 (16.7%) | |
| White | 14 (77.8%) | |
| education; n (%) | some college | 5 (27.8%) |
| college degree | 7 (38.9%) | |
| some grad school | 2 (11.1%) | |
| graduate degree | 4 (22.2%) | |
| religion; n (%) | Agnostic | 1 (5.6%) |
| Buddhist | 3 (16.7%) | |
| Christian | 1 (5.6%) | |
| Jewish | 1 (5.6%) | |
| none/atheist | 12 (66.7%) | |
| previous classic psychedelic use; n (%) | 16 (88.9%) | |
| years since last used a classic psychedelic; median (IQR) | 20 (1–32) | |
| clinical measurements | ||||
|---|---|---|---|---|
| baseline | immediately post-psilocybin | 3-weeks post-psilocybin | 3-months after last group therapy session | |
| attachment anxietya; mean (SD) | 33.0 (9.0) | 32.2 (9.1) | 29.0 (9.0) | |
| attachment avoidance; mean (SD) | 27.4 (10.4) | 24.7 (9.2) | 25.6 (9.0) | |
| MEQ30; mean (SD) | 104.7 (26.6) | |||
| ChEQ; mean (SD) | 37.1 (26.0) | |||
n = 17 due to outlier removal.
Change in Attachment Insecurity
See Table 1 for baseline characteristics and clinical outcomes. One outlier was detected and removed for attachment anxiety.
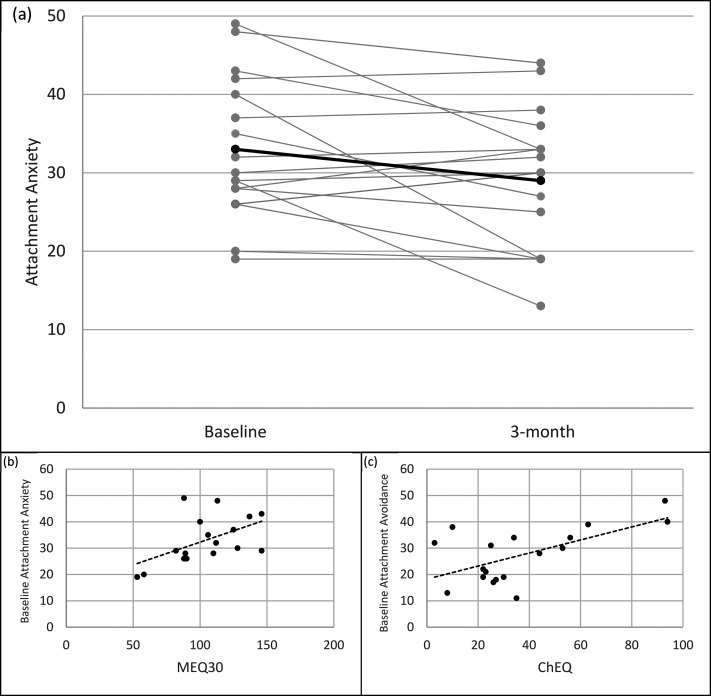
Attachment anxiety decreased from baseline to 3-months post-intervention by 4 points, t(16) = −2.2; p = 0.045; drm = 0.45; 95% CI 0.01, 0.87 (see Figure 1a). Attachment avoidance decreased during this time by 1.83 points, t(17) = −0.9; p = 0.367; drm = 0.19; 95% CI −0.22, 0.59 (see Figure S-1).
Figure 1.
(a) Experiences in Close Relationships (ECR-M16) subscale for attachment anxiety at baseline and 3-month follow-up. Bold line is average. (b) y-axis, baseline ECR-M16 subscale for attachment anxiety; x-axis, Mystical Experience Questionnaire (MEQ30) total score. (c) y-axis, baseline ECR-M16 subscale for attachment avoidance; x-axis, Challenging Experience Questionnaire (ChEQ) total score.
Attachment Insecurity as Predictor of MEQ30 and ChEQ
Baseline attachment anxiety and MEQ30 were found to be strongly correlated, r(15) = 0.53, p = 0.029 (see Figure 1b). Baseline attachment avoidance and MEQ30 had a small negative correlation that was not statistically significant, r(16) = −0.10, p = 0.693.
Baseline attachment avoidance was found to be strongly correlated with ChEQ, r(16) = 0.62, p = 0.006 (see Figure 1c). The relationship between baseline attachment anxiety and ChEQ was small and not statistically significant, r(15) = 0.18, p = 0.489.
The primary aims of our exploratory analyses were (1) to investigate the effect of psilocybin-assisted psychotherapy on attachment anxiety and attachment avoidance and (2) to investigate the effects of baseline attachment anxiety and avoidance on the psilocybin experience. We found a significant reduction in attachment anxiety at 3 months post-intervention compared to baseline. There was no notable change in attachment avoidance. We also found that higher baseline attachment anxiety was strongly associated with higher intensity of psilocybin-induced mystical-type experiences, and higher baseline attachment avoidance was strongly associated with higher intensity of challenging psilocybin experiences. Thus, our intervention reduced attachment anxiety, and baseline attachment insecurity predicted the quality of the psilocybin experience itself. These findings have important implications for the general treatment of psychiatric disorders as well as optimizing psilocybin-assisted psychotherapy as a broadly applicable treatment modality.
Further exploration is required in order to better understand the mechanisms underlying our finding of reduced attachment anxiety (e.g., it is unclear why some participants had a greater reduction in attachment anxiety than others). Preller et al. demonstrated that psilocybin, compared to placebo, acutely reduced subjective and neural reactivity to a laboratory-based social exclusion task, a marker of rejection sensitivity;30 while we found a significant reduction in attachment anxiety months after our intervention had ended. One possible explanation for our finding may involve psilocybin-induced plasticity31 triggering change in otherwise stable attachment-related neural pathways. Psychologically, our finding may reflect mitigation of hyperactivating strategies of the attachment motivation system (i.e., cognitive and behavioral efforts to minimize distance from intimate others that define individuals with high attachment anxiety).14 Theoretically, profound experiences of unity or interconnectedness with all that exists—a defining component of mystical experiences—may decrease an individual’s need for using hyperactivating strategies for some amount of time after the unity experience. In other words, perhaps ingrained working models resulting from inconsistent or intrusive early caretakers are transformed, and a more cohesive sense of self32 is able to emerge in the face of the numinous. Mystical unity has been interpreted as unity with entities beyond the interpersonal, such as “God”, “Nature”, or the “Cosmos”.33 Bill Wilson compared the effects of classic psychedelics to the “spiritual awakening” that inspired his recovery from alcoholism and subsequent cofounding of Alcoholics Anonymous34—which centers around a belief in “a Power greater than ourselves”. Psilocybin has been found to increase connection to nature,35 and psilocybin experiences were rated by research participants as among the most spiritually significant occurrences of their lives.36 Typically, self-reported attachment to intimate others corresponds to attachment to “God” (i.e., if one involves high attachment anxiety, the other tends to as well).37 However, psilocybin-induced neural plasticity along with an experience of mystical unity may lead to overall reduced attachment anxiety by establishing a more secure connection to something greater than, or beyond, the self, a connection that endures after the intervention has concluded (in our case, almost 4 months after a single psilocybin session). As William James38 put it, “···we can experience union with something larger than ourselves and in that union find our greatest peace.”38
On the other hand, we did not see a significant reduction in attachment avoidance. This finding echoes previous patterns in the literature of significant reductions in attachment anxiety, but not attachment avoidance, after receiving psychotherapy.39,40 One explanation may be that attachment anxiety, as opposed to attachment avoidance, is more tightly linked to the symptoms being targeted in our intervention. For example, Fraley and Bonanno found that, in a study of bereaved individuals, attachment anxiety was significantly associated with bereavement-related anxiety, depression, grief, and post-traumatic stress;41 however, attachment avoidance was not significantly associated with any of these symptoms. This may help explain why our participants—who experienced notable reductions in demoralization, complicated grief, and post-traumatic stress after psilocybin administration—demonstrated a significant reduction in attachment anxiety but not in attachment avoidance. It is important to remember that, while attachment insecurity may be contributing to psychiatric symptoms through rigid reenactments of maladaptive working models applied inflexibly in new situations, attachment insecurity is not itself pathological and may be serving an adaptive function by keeping individuals safe from ongoing interpersonal harm.
The observed link between baseline attachment anxiety and strength of the mystical-type experience is another interesting finding requiring further exploration. An alternative hypothesis might have assumed the opposite: that attachment anxiety would dampen mystical-type experiences due to elevated proximity-seeking toward the therapist(s) and an aversion to inward exploration distracting from a deeper internal experience—which would have essentially linked higher baseline attachment anxiety to less intense mystical-type experiences. Conversely, our finding suggests that hyperactivating strategies used among those with high attachment anxiety might somehow prime an individual for extreme interconnectedness, thus enhancing mystical-type experiences in this context.
On a related note, Granqvist et al. found that attachment disorganization is associated with a greater propensity for nonpsychedelic mystical experiences among spiritually oriented individuals.33 Individuals with attachment disorganization—often related to childhood abuse or neglect and linked with a high psychopathology risk—employ both hyperactivating and deactivating strategies in a dysregulated, often contradictory, manner with high scores on both attachment anxiety and attachment avoidance dimensions. The ECR-M16 does not measure attachment disorganization, perhaps a third dimension of attachment insecurity, so we were unable to investigate this relationship in our analyses; however, we feel that it is important to reference attachment disorganization in the discussion of our findings. Attachment disorganization is linked with dissociation—or a trance-like state representing discontinuity between thoughts, actions, memories, surroundings, and sense of self. Dissociation is often formulated as a clinical problem. Curiously, similar to attachment anxiety, the capacity for dissociation might actually prime an individual for the healing potential of nonordinary states of consciousness. Something similar is suggested by the literature on both medical hypnosis42 and Spiritist mediumship.43 It is likely that a highly structured set and setting along with a strong therapeutic alliance and integrative psychotherapy (i.e., adequate safety and support) are required to transform extreme interpersonal coping strategies into mechanisms for healing. In future work that replicates and extends our findings, we strongly advise advanced clinical judgment—including a thorough assessment of a participant’s attachment relationships, a therapist’s understanding of their own attachment patterns, and strong co-therapy teams—when constructing attachment-based formulations and treatment plans with vulnerable individuals in the context of psilocybin-assisted psychotherapy.
Finally, we found that higher attachment avoidance predicted greater challenge during the psilocybin experience. Individuals with high attachment avoidance have a characteristic aversion to emotional vulnerability and can have difficulty tolerating novel experiences. Clinically, it is thought that participants who can “surrender” to the psilocybin experience and trust their therapists to care for them (when they can no longer care for themselves in a usual manner) have less challenging experiences. It makes sense, therefore, that participants who tend to resist relying on others would have more challenging experiences with the concentrated attention of two therapists for an extended period of time. Interestingly, our findings also suggest that more securely attached individuals, or those with lower attachment anxiety and attachment avoidance, would have milder mystical-type experiences as well as less challenging experiences. Further work is needed to explore these hypotheses.
There are several obvious limitations to our analyses. Because of our lack of a control group, we are not able to state that these changes in attachment insecurity are psilocybin-induced versus induced by other aspects of the intervention, such as participants’ expectations or the group psychotherapy intervention44—which is a unique component of our study compared to other modern-day psilocybin trials. Our findings may not be generalizable beyond older, gay-identified men who are largely white, atheist, and college-educated. We used the self-report ECR-M16 for efficiency and simple quantitative analyses;5 however, future studies might incorporate the Adult Attachment Interview45 in order to consider a broader representation of attachment (e.g., attachment disorganization). Attachment insecurity is more often used as a baseline characteristic or moderating variable, rather than a clinical outcome, which presents a challenge in defining and conceptualizing a clinically significant change. Furthermore, levels of attachment anxiety and attachment avoidance in our sample may not generalize to a larger population of long-term AIDS survivors or other clinical populations due to selection bias or other factors related to our limited sample size. While our data are preliminary, we feel it is important to publish effect sizes in order to inform the design and a priori hypotheses of larger confirmatory trials.
The suggestion that a brief intervention—psilocybin-assisted group psychotherapy—might aide in the development of a greater sense of attachment security is clinically intriguing. If replicated, these findings could affect treatment for a wide range of psychiatric disorders, against which attachment security is protective. There are also implications for improving attachment-related supra-diagnostic issues, such as interpersonal problems, difficulty with emotion regulation, and overall adaptive functioning. Attachment theory potentially expands and deepens mechanistic theories of increased connectedness in psychedelic medicine.22−24 Larger controlled trials are needed to confirm our findings and to further explore the complex interplay between attachment theory and psilocybin-assisted psychotherapy.
Methods
Study Design and Population
These exploratory analyses use data from an open-label clinical trial of psilocybin-assisted psychotherapy for demoralization in older long-term AIDS survivor men (n = 18) (NCT02950467). The main outcomes have been published separately.28
Outcome Measures
The 16-item, self-report, modified Experiences in Close Relationships scale (ECR-M16)46 was collected at baseline, during the final week of group therapy sessions (3-weeks post psilocybin), and 3-months after the final group therapy session. The ECR-M16, a version of the scale developed for older populations with chronic medical illness, rephrases relevant items to refer generally to people with whom one feels close (rather than specifically romantic partners). Half of the questions measure attachment anxiety (e.g., “I resent it when people with whom I feel close spend time away from me.”), and half attachment avoidance (e.g., “I get uncomfortable when other people want to be very close to me.”), using a 7-point Likert scale.
Participants completed the 30-item revised Mystical Experience Questionnaire (MEQ30)47 and the 26-item Challenging Experience Questionnaire (ChEQ)48 the day after their psilocybin session. We used the MEQ30 total score, which comprises four factors: mystical (internal and external unity, noetic quality, and sacredness), positive mood, transcendence of time/space, and ineffability. We also used the ChEQ total score, which comprises seven factors: grief, fear, death, insanity, isolation, physical distress, and paranoia.
Statistical Analysis
We used the interquartile range (IQR) rule for identifying outliers: anything outside of [median – (1.5 × IQR)] to [median + (1.5 × IQR)]. Two missing values for each of attachment anxiety and attachment avoidance at 3-month follow-up were replaced with the value from the 3-week post-psilocybin assessment (i.e., last observation carried forward). Standard descriptive tests were used to report baseline and follow-up characteristics. A paired sample t-test was used to compare attachment insecurity at baseline and 3-month follow-up. We reported standardized effect sizes for pre to post repeated measures (drm) with 95% confidence intervals, which were calculated using exploratory software for confidence intervals.49 Pearson correlations compared baseline attachment anxiety and attachment avoidance with MEQ30 and ChEQ. Finally, we reported p-values for all outcomes using α = 0.05. Given the exploratory nature of our analyses, we did not account for the nested nature of our data, and no mathematical correction was made for multiple comparisons. Unless stated otherwise, analyses were calculated using SPSS Statistics, version 26.0 (IBM Corp., Armonk, NY).
Supporting Information Available
The Supporting Information is available free of charge at https://pubs.acs.org/doi/10.1021/acsptsci.0c00169.
Figure showing change in ECR-M16 subscale for attachment avoidance from baseline to 3-month follow-up (PDF)
Author Contributions
C.S.S. conceptualized and conducted this analysis, drafted this manuscript, and contributed to the design and implementation of the psilocybin-assisted group therapy intervention. B.T.A. designed and coordinated the parent trial and collected and analyzed data for this analysis. K.M.O. provided guidance and clarity on attachment constructs. J.W. contributed to the design of the parent trial. All authors contributed to the final version of this manuscript.
Salary support for C.S.S.: Department of Veterans Affairs Clinical Science Research & Development, Federal Award Identification Number IK2CX001495. Salary support for B.T.A.: NIMH R25 MH060482 and San Francisco VA Advanced Neuroscience Fellowship. Support for the parent trial: Carey Turnbull, Heffter Research Institute, River Styx Foundation, Saisei Foundation, Sarlo Foundation, Stupski Foundation, and Usona Institute.
The authors declare the following competing financial interest(s): B.T.A. is a consultant with Consciousness Healing. J.W. is a consultant for Silli Pharmaceutical.
Supplementary Material
References
- Bowlby J. (1969) Attachment and loss, Basic Books, New York, NY. [Google Scholar]
- Mikulincer M., and Shaver P. R. (2016) Attachment in adulthood: structure, dynamics, and change, 2nd ed., p 1 online resource (706 pages), The Guilford Press, New York. [Google Scholar]
- Gervai J. (2009) Environmental and genetic influences on early attachment. Child Adolesc Psychiatry Ment Health 3, 25. 10.1186/1753-2000-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen P.; Storebo O. J. (2020) Attachment and Epigenetics: A Scoping Review of Recent Research and Current Knowledge. Psychol Rep 33294120901846. 10.1177/0033294120901846. [DOI] [PubMed] [Google Scholar]
- Ravitz P.; Maunder R.; Hunter J.; Sthankiya B.; Lancee W. (2010) Adult attachment measures: a 25-year review. J. Psychosom. Res. 69, 419–432. 10.1016/j.jpsychores.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Vrticka P.; Vuilleumier P. (2012) Neuroscience of human social interactions and adult attachment style. Front. Hum. Neurosci. 6, 212. 10.3389/fnhum.2012.00212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman R. (2017) The Neurobiology of Human Attachments. Trends Cognit. Sci. 21, 80–99. 10.1016/j.tics.2016.11.007. [DOI] [PubMed] [Google Scholar]
- Brennan K. A., Clark C. L., and Shaver P. R. (1998) Self-report measurement of adult attachment: An integrative overview in Attachment theory and close relationships (Rholes W. S., and Simpson J. A., Eds.), pp 46–76, The Guilford Press, New York. [Google Scholar]
- Mikulincer M.; Shaver P. R. (2012) An attachment perspective on psychopathology. World Psychiatry 11, 11–15. 10.1016/j.wpsyc.2012.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miniati M.; Callari A.; Pini S. (2017) Adult Attachment Style and Suicidality. Psychiatr. Danubina 29, 250–259. 10.24869/psyd.2017.250. [DOI] [PubMed] [Google Scholar]
- Schindler A. (2019) Attachment and Substance Use Disorders-Theoretical Models, Empirical Evidence, and Implications for Treatment. Front Psychiatry 10, 727. 10.3389/fpsyt.2019.00727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley R. C. (2002) Attachment stability from infancy to adulthood: Meta-analysis and dynamic modeling of developmental mechanisms. Personality and Social Psychology Review 6, 123–151. 10.1207/S15327957PSPR0602_03. [DOI] [Google Scholar]
- Pinquart M.; Feussner C.; Ahnert L. (2013) Meta-analytic evidence for stability in attachments from infancy to early adulthood. Attach Hum Dev 15, 189–218. 10.1080/14616734.2013.746257. [DOI] [PubMed] [Google Scholar]
- Mikulincer M., and Shaver P. (2007) Attachment in Adulthood: Structure, Dynamics, and Change, Guilford Press, New York, NY. [Google Scholar]
- Reiff C. M.; Richman E. E.; Nemeroff C. B.; Carpenter L. L.; Widge A. S.; Rodriguez C. I.; Kalin N. H.; McDonald W. M. (2020) Psychedelics and Psychedelic-Assisted Psychotherapy. Am. J. Psychiatry 177, 391–410. 10.1176/appi.ajp.2019.19010035. [DOI] [PubMed] [Google Scholar]
- Johnson M. W.; Hendricks P. S.; Barrett F. S.; Griffiths R. R. (2019) Classic psychedelics: An integrative review of epidemiology, therapeutics, mystical experience, and brain network function. Pharmacol. Ther. 197, 83–102. 10.1016/j.pharmthera.2018.11.010. [DOI] [PubMed] [Google Scholar]
- Moreno F. A.; Wiegand C. B.; Taitano E. K.; Delgado P. L. (2006) Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder. J. Clin. Psychiatry 67, 1735–1740. 10.4088/JCP.v67n1110. [DOI] [PubMed] [Google Scholar]
- Watts R.; Luoma J. B. (2020) The use of the psychological flexibility model to support psychedelic assisted therapy. Journal of Contextual Behavioral Science 15, 92–102. 10.1016/j.jcbs.2019.12.004. [DOI] [Google Scholar]
- Erritzoe D.; Roseman L.; Nour M. M.; MacLean K.; Kaelen M.; Nutt D. J.; Carhart-Harris R. L. (2018) Effects of psilocybin therapy on personality structure. Acta Psychiatr. Scand. 138, 368–378. 10.1111/acps.12904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carhart-Harris R. L.; Bolstridge M.; Day C. M. J.; Rucker J.; Watts R.; Erritzoe D. E.; Kaelen M.; Giribaldi B.; Bloomfield M.; Pilling S.; Rickard J. A.; Forbes B.; Feilding A.; Taylor D.; Curran H. V.; Nutt D. J. (2018) Psilocybin with psychological support for treatment-resistant depression: six-month follow-up. Psychopharmacology (Berl) 235, 399–408. 10.1007/s00213-017-4771-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogenschutz M. P. (2017) It’s time to take psilocybin seriously as a possible treatment for substance use disorders. Am. J. Drug Alcohol Abuse 43, 4–6. 10.1080/00952990.2016.1200060. [DOI] [PubMed] [Google Scholar]
- Carhart-Harris R. L.; Erritzoe D.; Haijen E.; Kaelen M.; Watts R. (2018) Psychedelics and connectedness. Psychopharmacology (Berl) 235, 547–550. 10.1007/s00213-017-4701-y. [DOI] [PubMed] [Google Scholar]
- Holland J. (2020) Good chemistry: the science of connection, from soul to psychedelics, 1st ed., Harper Wave, New York, NY. [Google Scholar]
- Forstmann M.; Yudkin D. A.; Prosser A. M. B.; Heller S. M.; Crockett M. J. (2020) Transformative experience and social connectedness mediate the mood-enhancing effects of psychedelic use in naturalistic settings. Proc. Natl. Acad. Sci. U. S. A. 117, 2338–2346. 10.1073/pnas.1918477117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett F. S.; Griffiths R. R. (2017) Classic Hallucinogens and Mystical Experiences: Phenomenology and Neural Correlates. Curr. Top. Behav. Neurosci. 36, 393–430. 10.1007/7854_2017_474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett F. S.; Johnson M. W.; Griffiths R. R. (2017) Neuroticism is associated with challenging experiences with psilocybin mushrooms. Pers Individ Dif 117, 155–160. 10.1016/j.paid.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonaro T. M.; Bradstreet M. P.; Barrett F. S.; MacLean K. A.; Jesse R.; Johnson M. W.; Griffiths R. R. (2016) Survey study of challenging experiences after ingesting psilocybin mushrooms: Acute and enduring positive and negative consequences. J. Psychopharmacol. 30, 1268–1278. 10.1177/0269881116662634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson B. T.; Danforth A.; Daroff R.; Stauffer C.; Ekman E.; Agin-Liebes G.; Trope A.; Boden M. T.; Dilley J.; Mitchell J.; Woolley J. (2020) Psilocybin-assisted group therapy for demoralized older long-term AIDS survivor men: An open-label safety and feasibility pilot study. EClinicalMedicine. 27, 100538. 10.1016/j.eclinm.2020.100538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-Cobb J. M.; Gore-Felton C.; Marouf F.; Koopman C.; Kim P.; Israelski D.; Spiegel D. (2002) Coping, social support, and attachment style as psychosocial correlates of adjustment in men and women with HIV/AIDS. J. Behav Med. 25, 337–353. 10.1023/A:1015814431481. [DOI] [PubMed] [Google Scholar]
- Preller K. H.; Pokorny T.; Hock A.; Kraehenmann R.; Stämpfli P.; Seifritz E.; Scheidegger M.; Vollenweider F. X. (2016) Effects of serotonin 2A/1A receptor stimulation on social exclusion processing. Proc. Natl. Acad. Sci. U. S. A. 113, 5119–5124. 10.1073/pnas.1524187113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ly C.; Greb A. C.; Cameron L. P.; Wong J. M.; Barragan E. V.; Wilson P. C.; Burbach K. F.; Soltanzadeh Zarandi S.; Sood A.; Paddy M. R.; Duim W. C.; Dennis M. Y.; McAllister A. K.; Ori-McKenney K. M.; Gray J. A.; Olson D. E. (2018) Psychedelics Promote Structural and Functional Neural Plasticity. Cell Rep. 23, 3170–3182. 10.1016/j.celrep.2018.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenberg J. D. (1980) Clinical application of the concept of a cohesive sense of self. Int. J. Psychoanal Psychother 8, 85–114. PMID: 7429741. [PubMed] [Google Scholar]
- Granqvist P.; Hagekull B.; Ivarsson T. (2012) Disorganized Attachment Promotes Mystical Experiences via a Propensity for Alterations in Consciousness (Absorption). International Journal for the Psychology of Religion 22, 180–197. 10.1080/10508619.2012.670012. [DOI] [Google Scholar]
- Kurtz E. (2008) Drugs and the spiritual: Bill W. takes LSD in The Collected Ernie Kurtz, Authors Choice, New York, NY. [Google Scholar]
- Lyons T.; Carhart-Harris R. L. (2018) Increased nature relatedness and decreased authoritarian political views after psilocybin for treatment-resistant depression. J. Psychopharmacol. 32, 811–819. 10.1177/0269881117748902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths R.; Richards W.; Johnson M.; McCann U.; Jesse R. (2008) Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later. J. Psychopharmacol. 22, 621–632. 10.1177/0269881108094300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall T. W.; Fujikawa A.; Halcrow S. R.; Hill P. C.; Delaney H. (2009) Attachment to God and implicit spirituality: Clarifying correspondence and compensation models. Journal of Psychology and Theology 37, 227–244. 10.1177/009164710903700401. [DOI] [Google Scholar]
- James W. (1903) The Varieties of Religious Experience: A Study in Human Nature, Longmans, Green and Company, London, England. [Google Scholar]
- Taylor P.; Rietzschel J.; Danquah A.; Berry K. (2015) Changes in attachment representations during psychological therapy. Psychother Res. 25, 222–238. 10.1080/10503307.2014.886791. [DOI] [PubMed] [Google Scholar]
- Johnson L. N.; Tambling R. B.; Mennenga K. D.; Ketring S. A.; Oka M.; Anderson S. R.; Huff S. C.; Miller R. B. (2016) Examining Attachment Avoidance and Attachment Anxiety Across Eight Sessions of Couple Therapy. J. Marital Fam Ther 42, 195–212. 10.1111/jmft.12136. [DOI] [PubMed] [Google Scholar]
- Fraley R. C.; Bonanno G. A. (2004) Attachment and loss: a test of three competing models on the association between attachment-related avoidance and adaptation to bereavement. Pers Soc. Psychol Bull. 30, 878–890. 10.1177/0146167204264289. [DOI] [PubMed] [Google Scholar]
- Spiegel D. (2013) Tranceformations: hypnosis in brain and body. Depression Anxiety 30, 342–352. 10.1002/da.22046. [DOI] [PubMed] [Google Scholar]
- Moreira-Almeida A.; Neto F. L.; Cardeña E. (2008) Comparison of brazilian spiritist mediumship and dissociative identity disorder. J. Nerv. Ment. Dis. 196, 420–424. 10.1097/NMD.0b013e31816ff3a1. [DOI] [PubMed] [Google Scholar]
- Marmarosh C. L., Markin R. D., and Spiegel E. B. (2013) Attachment in Group Psychotherapy, American Psychological Association, Washington, DC. 10.1037/14186-000. [DOI] [Google Scholar]
- Hesse E. (2008) The Adult Attachment Interview: Protocol, Method of Analysis, and Empirical Studies in Handbook of Attachment: Theory, Research, and Clinical Applications (Cassidy J., and Shaver P. R., Eds.) 2nd ed., pp 552–598, Guilford Press, New York, NY. [Google Scholar]
- Lo C.; Walsh A.; Mikulincer M.; Gagliese L.; Zimmermann C.; Rodin G. (2009) Measuring attachment security in patients with advanced cancer: psychometric properties of a modified and brief Experiences in Close Relationships scale. Psycho-Oncology 18, 490–499. 10.1002/pon.1417. [DOI] [PubMed] [Google Scholar]
- Barrett F. S.; Johnson M. W.; Griffiths R. R. (2015) Validation of the revised Mystical Experience Questionnaire in experimental sessions with psilocybin. J. Psychopharmacol. 29, 1182–1190. 10.1177/0269881115609019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett F. S.; Bradstreet M. P.; Leoutsakos J. S.; Johnson M. W.; Griffiths R. R. (2016) The Challenging Experience Questionnaire: Characterization of challenging experiences with psilocybin mushrooms. J. Psychopharmacol. 30, 1279–1295. 10.1177/0269881116678781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming G. (2016) Exploratory software for confidence intervals; Routledge. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.