Abstract
There are limited data in the literature comparing two simultaneously worn ambulatory blood pressure (BP) monitoring (ABPM) devices. The authors compared BPs from two monitors (Mobil‐O‐Graph [I.E.M., Stolberg, Germany] and Spacelabs 90207 [Spacelabs Medical, Issequah, WA]). In the nonrandomized component of the study, simultaneous 8‐hour BP and heart rate data were measured by Mobil‐O‐Graph, consistently applied to the nondominant arm, and Spacelabs to the dominant arm on 12 untreated adults. Simultaneous 8‐hour BP and heart data were obtained by the same monitors randomly assigned to a dominant or nondominant arm on 12 other untreated adults. Oscillometric BP profiles were obtained in the dominant and nondominant arms of the above 24 patients using an Accutorr (Datascope, Mahwah, NJ) device. The Spacelabs monitor recorded a 10.2‐mm Hg higher systolic pressure in the nonrandomized (P=.0016) and a 7.9‐mm Hg higher systolic pressure in the randomized studies (P=.00008) compared with the Mobil‐O‐Graph. The mean arterial pressures were 1 mm Hg to 2 mm Hg different between monitors in the two studies, and heart rates were nearly identical. Our observations, if confirmed in larger cohorts, support the concern that ABPM device manufacturers consider developing normative databases for their devices.
Ambulatory blood pressure (BP) monitoring (ABPM) is an effective way to characterize BP‐related cardiovascular risk since it performs repeated measurements over 24 hours, providing a superior estimation of hemodynamic load when compared with office‐based BP.1, 2 Most ABPM devices measure brachial BP through a proprietary algorithm using oscillometry. However, there is no uniform methodology or current national standard for this process and different brands of oscillometric monitors use different techniques.3, 4 Unlike mercury‐based sphygmomanometry, oscillometric monitors often estimate systolic and diastolic pressures.
The British Hypertension Society4 and the Association for the Advancement of Medical Instrumentation5 recommends validation of oscillometric monitors by comparison to a mercury manometer, allowing up to 5‐mm Hg differences in systolic readings. With the disappearance of mercury from health care settings, and the ubiquitous use of automated BP devices, diagnostic and treatment decisions are increasingly based on oscillometric BP monitor data and publications using ABPM sometimes combine data from multiple ABPM devices.6 Our review of the literature found only two publications comparing two ABPM devices worn simultaneously,7, 8 and only one was outside of the office setting. Consequently, we conducted a study comparing 8‐hour ABPM using two monitors worn simultaneously by adult patients.
Methods
Nonrandomized Study
In this single‐center study, we recruited 12 adult healthy volunteers at the Hospital of University of Pennsylvania over a period of 2 months. This study was approved by the institutional review board (IRB) of the University of Pennsylvania and written informed consent was obtained from all patients.
BP and heart rate (HR) data were collected over 8 hours beginning at 8:30 am ± 60 minutes. Demographic data, including date of birth, sex, and ethnicity as well as the height and weight of each participant were recorded. Standard seated BPs were obtained in triplicate at the beginning and end of the 8‐hour monitoring period using an Accutorr (Datascope, Mahwah, NJ) device.
Ambulatory BP (ABP) and HR data were recorded at 15‐minute intervals using the validated Mobil‐O‐Graph (I.E.M. Stolberg, Germany)9 (nondominant arm) and the Spacelabs 90207 (Spacelabs Medical, Issequah, WA)10 (dominant arm). The Mobil‐O‐Graph was worn for a total of 24 hours as part of a separate study protocol that prespecified application to the nondominant arm.
Oscillometric BP Recording From Both Arms of Each Patient in the Nonrandomized Study
On a separate occasion, we measured seated BPs using the Accutorr device in every patient with ABPM. After 5 minutes of rest, 3 BPs were obtained in each arm at 1‐minute intervals, recorded, and averaged for each arm. A coin flip determined whether the dominant arm or the nondominant arm was used first (dominant arm for heads).
Randomized Study
In a different cohort, also IRB‐approved and for which written informed consent was obtained, we measured baseline BPs using the Accutorr and used the same ABP monitors for 8 hours. However, the arm to which each monitor was applied was randomly determined by a coin flip at the time of application (eg, heads for the Mobil‐O‐Graph on the dominant arm).
In all studies, cuff sizes used for measuring BP were appropriate for the mid‐arm circumference.
Data
The average BP readings for systolic BP (SBP), diastolic BP (DBP), and mean arterial pressure (MAP) for all studies is reported as mean (standard error of the mean [SEM]) calculated for 8 hours. The average HR is reported as mean (SEM) beats per minute. Paired t testing was performed to determine the statistical significance of differences within the patients.
Results
Baseline characteristics for all patients are presented in Table 1. Figure 1 (left panel) shows SBP, MAP, and DBP from each ambulatory monitor as an hourly average in the nonrandomized cohort. The Spacelabs device read higher systolic (134.2 [3.2] mm Hg) and diastolic (84.9 [2.6] mm Hg) BP throughout the 8 hours compared with the systolic (123.9 [2.8] mm Hg) and diastolic (82.1 [2.2] mm Hg) values of Mobil‐O‐Graph. There was, however, close agreement between the devices in measured MAP: Mobil‐O‐Graph (101.4 [2.0] mm Hg) and Spacelabs (100.6 [2.4] mm Hg). Measured HR also correlated well: 82.4 (4.1) beats per minute for Mobil‐O‐Graph compared with 81.7 (4.0) beats per minute for Spacelabs.
Table 1.
Baseline Characteristics
| Demographics | Nonrandomized, No. (%)(n=12) | Randomized, No. (%)(n=12) |
|---|---|---|
| Sex | ||
| Male | 7 (58.3) | 6 (50) |
| Female | 5 (41.7) | 6 (50) |
| Race | ||
| Caucasian | 9 (75) | 5 (41.7) |
| Asian | 3 (25) | 5 (41.7) |
| African American | 0 (0) | 2 (16.6) |
| Age, y | 38 | 38 |
| Height, cm | 175.75 | 166.1 |
| Weight, kg | 84.4 | 70.9 |
| Body mass index, kg/m2 | 27.39 | 25.5 |
Figure 1.
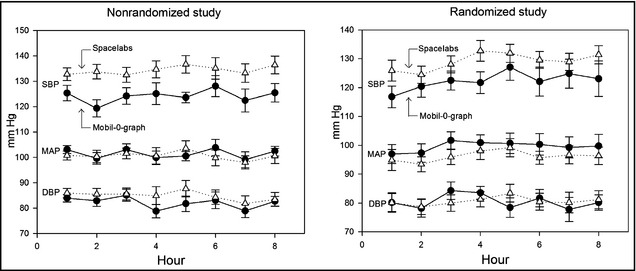
Left and right insets show systolic blood pressure (SBP), mean arterial pressure (MAP), and diastolic blood pressure (DBP) averaged (with standard errors) for the 8 hours that the Mobil‐O‐Graph (black lines and filled circles) and Spacelabs (dotted lines and triangles) devices were worn in the nonrandomized and randomized studies, respectively.
For the seated Accutorr measurements performed in all patients, the BP was done on the dominant arm first in 14 of the 24 patients. The SBP in the dominant arm was significantly higher (2.6 mm Hg; P=.03) compared with the nondominant arm (Table 2). As with the ABPM, there was close agreement in the MAP measurements.
Table 2.
Comparison of Oscillometric Blood Pressure of Dominant and Nondominant Arm Using the Accutorr Device
| Dom SBP, mm Hg | Non‐Dom SBP, mm Hg | Dom DBP, mm Hg | Non‐DOM DBP, mm Hg | Dom MAP, mm Hg | Non‐Dom MAP, mm Hg | Dom HR, beats per min | Non‐Dom HR, beats per min | |
|---|---|---|---|---|---|---|---|---|
| N=24 | 118.6 | 115.9 | 69.9 | 70.3 | 88.2 | 87.1 | 75.8 | 75.5 |
| SEM | (3.6) | (3.6) | (2.5) | (2.5) | (2.8) | (3.0) | (3.4) | (3.5) |
| P value | – | .033 | – | .712 | – | .052 | – | .563 |
Abbreviations: Dom, dominant arm; DBP, diastolic blood pressure; HR, heart rate; MAP, mean arterial pressure; Non‐Dom, nondominant arm; SBP, systolic blood pressure; SEM, standard error of the mean. P value <.05 implies statistically significant difference in the measured values between dominant and nondominant arms.
Bland‐Altman plots were constructed for MAP, and SBP comparing the two ABP monitors is shown in Figures 2 and 3. In Figure 2, the SBP readings are 10.2 mm Hg higher on the Spacelabs compared with the Mobil‐O‐Graph with no evidence of bias in the range of readings (P=.001). As shown in Figure 3, MAP was similar between the two monitors (P=.61). The HRs measured by the two devices were similar (P=.26), and the DBP showed a nonsignificant trend to a higher value in Spacelabs (P=.15) (data not shown for HR or DBP).
Figure 2.
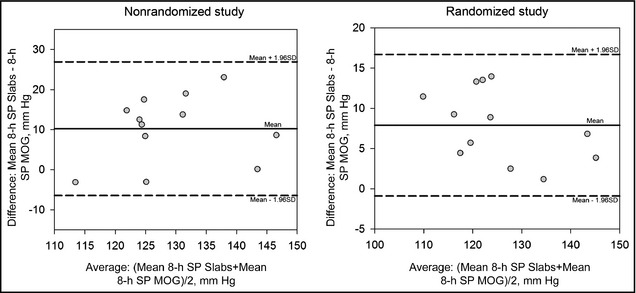
Left and right insets show Bland‐Altman plots of the mean systolic pressures (SPs) of Mobil‐O‐Graph (MOG) and Spacelabs (Slabs) monitors, averaged over 8 hours for each data point for nonrandomized and randomized studies, respectively. Central solid lines indicate the mean of the differences (bias) at 10.2 mm Hg for nonrandomized study and 7.7 mm Hg for the randomized study. Dotted lines on either side of the mean indicate the confidence intervals of agreement between the two monitors' SP measurements, with a standard deviation difference of 8.5 mm Hg for nonrandomized study and 4.5 mm Hg for randomized study for all values.
Figure 3.
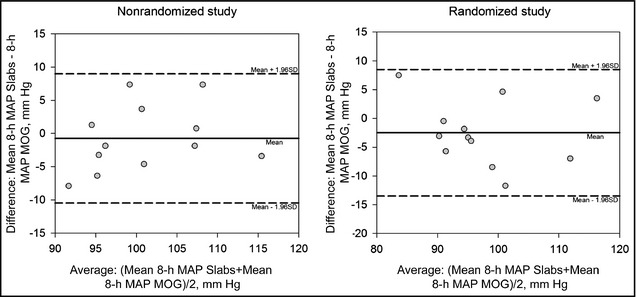
Left and right insets show Bland‐Altman plots of the mean arterial pressures (MAPs) of Mobil‐O‐Graph (MOG) and Spacelabs (Slabs) monitors, averaged over 8 hours for each data point for nonrandomized and randomized studies, respectively. Central solid lines indicate the mean of the differences (bias) at −.7 mm Hg for nonrandomized study and −2.5 mm Hg for the randomized study. Dotted lines on either side of the mean indicate the confidence intervals of agreement between the two monitors' SP measurements, with a standard deviation difference of 5 mm Hg for nonrandomized study and 5.6 mm Hg for randomized study for all values.
In the randomized study, the Spacelabs device was applied to the dominant arms in 5 of the 12 patients. The average SBP reading for these patients using the Mobil‐O‐Graph was 121.4 (3.4) mm Hg, compared with 129.2 (2.8) mm Hg using the Spacelabs device (P=.00008). These results are shown in Figure 1 (right panel). Whether the Mobil‐O‐Graph was applied to the dominant or the nondominant arm, its SBP readings remained significantly lower than those obtained with the Spacelabs device, while the MAP, again, was not significantly different.
Discussion
Oscillometric BP devices generally determine the MAP and estimate the systolic and diastolic values based on internal algorithms. Our 8‐hour data show high concordance of MAPs despite the few minutes in time difference between device inflations. Our data also demonstrate an 8‐ to 10‐mm Hg higher SBP with the Spacelabs monitor compared with the Mobil‐O‐Graph monitor. Our hospital no longer measures BP using mercury‐based devices, and relies on oscillometric BP equipment to perform all vital signs (BP, HR, temperature, and oxygen saturation). Thus, from a calibration standpoint, it is difficult to decide which ABPM monitor more closely approximates the true brachial arterial pressure when measured in a manner recommended by accepted mercury‐based industry standards.5
We undertook these studies anticipating there would be only a small difference between the ambulatory monitors, but our results suggest otherwise. Although it could be argued that the findings from our nonrandomized study were mainly due to nondominant vs dominant arm monitor application, we found nearly identical differences in ABPM systolic data irrespective of which ABP monitor was applied to the dominant or the nondominant arm.
We found only two studies comparing two simultaneously worn ABPM devices. In one study the monitoring period was short—only long enough to obtain 6 readings in a research setting.7 They demonstrated reasonably close agreement in aggregate between monitors but there was no “ambulatory” component. A careful read of their data revealed that <50% of the systolic readings on the two monitors (Del Mar Avionics' Pressurometer IV [Irvine, CA] compared with Spacelabs 90202) were within 5 mm Hg of each other. In the other study, the same type of monitor, a Tycos Quiet‐Trak device [Tycos‐Welch‐Allyn, Arden, NC], was worn on each arm for 24 hours.8 The 10 patients were all hypertensive and were recruited because of a minimum 10‐mm Hg difference in SBP between their arms on screening. An average of 8‐mm Hg difference in SBP over the 24 hour period, with higher readings in the right arm was observed, as in our study. The difference in the SBP they noted using the same model ABPM comparing arms was about half of the difference reported in their screening clinic BP values, while our study showed the opposite. Moreover, they studied a population selected for a pre‐existing difference in SBP.
When we measured SBP using the same oscillometric monitor (Accutorr) on each arm, we observed a significant 2.6‐mm Hg (P=.03) higher SBP in the dominant arm (Table 2), consistent with other studies.11 This partially explains the higher SBP using Spacelabs due to its placement on the dominant arm in the nonrandomized study. Although factors such as the presence of cardiovascular comorbidities12 with increasing age13 could account for the interarm BP difference we noted, the relatively younger age and absence of hypertension in our cohort makes it less likely. However, such a systematic bias (2.6 mm Hg) explains less than one third of the difference we noted between the two ambulatory units in either our nonrandomized (10.2 mm Hg) or our randomized cohorts (7.9 mm Hg). Interestingly the difference in SBP between monitors in the nonrandomized study compared with the randomized study is almost entirely explained by the differences in SBP between the dominant and nondominant arms obtained by the Accutorr device, further supporting our observation of a difference in the SBP between the ABPM devices.
Differences in bleed down rates (the Mobil‐O‐Graph has a variable bleed down rate; the Spacelabs has an 8‐mm Hg bleed down rate) could account for some of the variation in SBP, but we speculate that differences in the internal algorithms are responsible, as the MAP measured by each device was similar in both cohorts.
Study Limitations
Our study has limitations. The numbers are small, and we cannot say which monitor is “better” since we have no mercury standard or direct (intra‐arterial) pressure measurements. Our patients were healthy and un‐medicated; thus, our observations may not apply to populations with comorbidities or taking medications such as treated hypertensives. The detection of interarm differences in BP was only done by oscillometry, which we think reduces human ascertainment bias, but we acknowledge that auscultatory BP would also have been useful, had we performed it, to verify the interarm BP differences.
Conclusions
We observed significant differences in SBP during a period of 8 hours using two different ABPM devices. According to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, a 14%, 9%, and 7% reduction in mortality rates due to stroke, coronary heart disease, and all‐cause mortality, respectively, can be achieved by an SBP reduction of 5 mm Hg.14 An 8‐ to 10‐mm Hg ABP difference, if replicated in other studies, has important public health consequences, and raises questions about the wisdom of pooling ABPM data obtained from different ambulatory devices.15 Without more studies like ours, on a larger scale, it is challenging to place confidence in the SBP (particularly in patients older than 59 years16) values reported in studies using different ABP monitors. Replication of our results would support a recommendation that each ABPM manufacturer develop device‐specific normative databases to help a practitioner interpret the ABPM data obtained with their device. The growing use of home oscillometric BP17 represents an additional area where similar differences as those we noted in our report could exist.
Conflict of Interest
The authors report no financial conflicts of interest.
Source of Funding
These studies were conducted in the Clinical and Translational Research Center, which is funded by grant number UL1RR024134 from the National Center for Research Resources.
J Clin Hypertens (Greenwich). 2013;15:321–325. ©2013 Wiley Periodicals, Inc.23614845
References
- 1. O'Brien E, Turner JR. Assessing blood pressure responses to noncardiovascular drugs: the beneficial role of ambulatory blood pressure monitoring. J Clin Hypertens (Greenwich). 2013;15:55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension 2005;46:156–161. [DOI] [PubMed] [Google Scholar]
- 3. Ogedegbe G, Pickering T. Principles and techniques of blood pressure measurement. Cardiol Clin 2010;28:571–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005;111:697–716. [DOI] [PubMed] [Google Scholar]
- 5. Weiss BM, Pasch T. Measurement of systemic arterial pressure. Curr Opin Anaesthesiol. 1997;10:459–466. [Google Scholar]
- 6. Hansen TW, Kikuya M, Thijs L, et al. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta‐analysis of 7,030 individuals. J Hypertens 2007;25:1554–1564. [DOI] [PubMed] [Google Scholar]
- 7. Santucci S, Cates EM, James GD, et al. A comparison of two ambulatory blood pressure monitors, the Del Mar Avionics Pressurometer IV and the Spacelabs 90202. Am J Hypertens 1989;2:797–799. [DOI] [PubMed] [Google Scholar]
- 8. O'Shea JC, Murphy MB. Ambulatory blood pressure monitoring: which arm? J Hum Hypertens 2000;14:227–230. [DOI] [PubMed] [Google Scholar]
- 9. Wei W, Tölle M, Zidek W, van der Giet M. Validation of the Mobil‐O‐Graph: 24 h‐blood pressure measurement device. Blood Press Monit. 2010;15:225–228. [DOI] [PubMed] [Google Scholar]
- 10. Groppelli A, Omboni S, Ravogli A, et al. Validation of the SpaceLabs 90202 and 90207 devices for ambulatory blood pressure monitoring by comparison with intra‐arterial resting and ambulatory measurements. J Hypertens Suppl 1991;9:S334–S335. [PubMed] [Google Scholar]
- 11. Swallow RA. Letter: hypertension–which arm? Br Med J. 1975;3:370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Clark CE, Campbell JL, Evans PH, Millward A. Prevalence and clinical implications of the inter‐arm blood pressure difference: a systematic review. J Hum Hypertens 2006;20:923–931. [DOI] [PubMed] [Google Scholar]
- 13. Arnett DK, Tang W, Province MA, et al. Interarm differences in seated systolic and diastolic blood pressure: the hypertension genetic epidemiology network study. J Hypertens 2005;23:1141–1147. [DOI] [PubMed] [Google Scholar]
- 14. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 15. Kikuya M, Hansen TW, Thijs L, et al. Diagnostic thresholds for ambulatory blood pressure monitoring based on 10‐year cardiovascular risk. Circulation 2007;115:2145–2152. [DOI] [PubMed] [Google Scholar]
- 16. Izzo JL Jr, Levy D, Black HR. Clinical Advisory Statement. Importance of systolic blood pressure in older Americans. Hypertension 2000;35:1021–1024. [DOI] [PubMed] [Google Scholar]
- 17. Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: executive summary. A joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. J Clin Hypertens (Greenwich). 2008;10:467–476. [DOI] [PMC free article] [PubMed] [Google Scholar]


