Abstract
Limited data exist on the comparison of blood pressure (BP) measurements using aneroid and oscillometric devices. The purpose of the study was to investigate the difference in BP obtained using oscillometric and aneroid BP monitors in 9‐ to 10‐year‐old children. A total of 979 children were divided into group O, which underwent two oscillometric BP readings followed by two aneroid readings, and group A, which had BP measured in the reverse order. No significant difference was found between the mean (±standard deviation) of the two systolic BP readings obtained using the oscillometric and aneroid devices (111.5±8.6 vs 111.3±8.1 mm Hg; P=.39), whereas the mean diastolic BP was lower with the oscillometric monitor (61.5±8.0 vs 64.5±6.8 mm Hg; P<.001). A significant downward trend in BP was observed with each consecutive measurement, and agreement between the two monitors was limited. Multiple BP measurements are, therefore, recommended before the diagnosis of elevated BP or hypertension is made with either method.
Measurement of blood pressure (BP) is an essential component of physical examination in both children and adults. In spite of a low prevalence of hypertension in children,1, 2, 3, 4 early and accurate detection of elevated BP is nonetheless very important for preventing future end‐organ damage.5, 6, 7
While normative data on BP in children are based on manual BP readings using mercury sphygmomanometer, automated oscillometric BP monitors are now widely used in pediatric clinics and hospitals.8 Studies comparing oscillometric and mercury BP monitors have yielded inconsistent findings where the oscillometric method has been found to either overestimate or underestimate the BP.9, 10, 11, 12, 13
Two recent US studies14, 15 have investigated the difference between BP measurements obtained by aneroid and mercury sphygmomanometers in children and found no or minimal difference between these measurement methods. To date, the only published study comparing an aneroid sphygmomanometer with an oscillometric BP monitor was carried out in a population of 235 children with chronic kidney disease (CKD).16 The oscillometric monitor was found to overestimate both the systolic and diastolic BP and limited agreement was found between the two methods in classification of BP status.
Although mercury sphygmomanometers have been widely replaced with aneroid BP devices, no studies have compared aneroid sphygmomanometers and automated oscillometric BP monitors in population‐based samples. The aim of this study was to compare BP measurements obtained using aneroid sphygmomanometer and automated oscillometric device and to analyze factors contributing to the differences between these two methods in 9‐ to 10‐year‐old Icelandic school children.
Methods
The study was a part of a population‐based, cross‐sectional study of BP in healthy 9‐ to 10‐year‐old Icelandic school children carried out in the year 2009.4 Of the 1472 children invited to participate, the parents of 1071 children gave their written informed consent for participation. The study was approved by The National Bioethics Committee (NBC 08‐138) and The Icelandic Data Protection Authority.
The aneroid BP monitor used in the study was the Accoson Green Light 300 Sphygmomanometer (Accoson, Harlow, Essex, UK), which has been validated in adults but not in children.17 The oscillometric blood pressor monitor was the IntelliVue MP50 Patient Monitor (Philips, Andover, MA). The aneroid sphygmomanometer was already being used in our pediatric hypertension clinic at the initiation of the study and the oscillometric monitor was available to our research group without cost at the time of the study.
Each child underwent a total of four seated BP measurements in a quiet room close to the classroom, of which two measurements were performed using the manual aneroid sphygmomanometer and two measurements with the automated oscillometric monitor. The BP measurements were carried out between 8 am and 2 pm, at least 30 seconds apart following a minimum of 2 minutes of rest. Two trained physicians wearing casual clothing performed all BP measurements and all aneroid readings were obtained by the same physician. The BP cuffs had a bladder width of at least 40% and a bladder length of 80% to 100% of the child's upper arm circumference at a point midway between the olecranon and the acromion.18 When the aneroid BP monitor was used, systolic BP was determined by the auscultatory appearance of the first Korotkoff sound and diastolic BP by the fifth Korotkoff sound, rounded to the nearest 2 mm Hg.
The children were divided into two groups designated as O and A, based on the order by which their BP was measured. Children in group O first underwent two oscillometric and then two aneroid BP measurements, while children in group A had their BP measured in the reverse order. This approach was chosen to reduce the confounding effect of the first reading, which is frequently higher than subsequent readings.11 The order by which the children were brought from the classroom to the examination room was left to the discretion of the individual teachers. The first child was assigned to group O and the second child to group A and the remainder of the children were assigned to two groups in an alternating order. Normative BP data published by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents were used to define BP percentiles.18 Elevated BP was defined as BP ≥95th age‐, sex‐, and height‐specific percentile.
Measurements of height and weight were obtained by school nurses and the body mass index (BMI) calculated. Anthropometric reference data for sex and age from the Centers for Disease Control and Prevention were used to establish height and weight percentiles and to calculate BMI percentile.
Statistical Considerations
Data are presented as percentage or mean±standard deviation. The two groups of children were compared using the two‐sample t test and chi‐square analysis. Three strategies were employed to compare BP readings obtained by the aneroid and oscillometric techniques. First, each child served as its own control and a paired t test was used to compare the first BP reading obtained by each method, then the second reading by each method, and finally the mean of the two readings obtained by each method. Second, we compared each of the two oscillometric measurements for one group with the corresponding aneroid measurements for the other group, using two‐sample t test. Finally, we performed a repeated measures analysis of variance (rmANOVA) to better characterize the decline in BP readings with repeated measurements and to test for a potential effect of method and method order, controlling for BMI and sex. The frequency of elevated BP (≥95th percentile) observed by each method was compared using McNemar's test and the agreement between the methods in detecting elevated BP examined using the κ statistic (>0.7 good agreement, 0.4–0.7 fair agreement, <0.4 limited agreement). Correlation between BP readings was examined using Pearson′s correlation coefficient. To further investigate the difference in BP readings by the two methods, we plotted Bland‐Altman graphs and applied Pearson′s correlation coefficient to examine the relationship between body composition parameters and the BP difference. Sex variability in BP difference between the measurement methods was assessed by the two‐sample t test. Statistical significance was set at a P value of <.05. Statistical analysis was performed with SPSS 17.0 (SPSS, IBM Corporation, Armonk, NY).
Results
Of the 1071 participating children, 92 had missing data, leaving 979 patients with complete data for BP, height, weight, BMI, and BMI percentile. The mean age was 9.6±0.3 years and 50.4% were female. The mean height was 139±6 cm and the mean weight 34±7 kg, yielding an average BMI of 17.6±2.8 (BMI percentile 56.9±28.2). Obesity was present in 7.2% of the children and 20.1% were either overweight or obese. A total of 459 children were assigned to group O and 520 children to group A. There was no difference between the two groups with respect to age, sex, height, weight, BMI, and BMI percentile or the frequency of overweight and obesity. The mean BP for each of the four measurements is presented in Table 1 and the comparison of BP measurements, with each child serving as its own control, is displayed in Table 2. The first systolic BP measurement obtained using the oscillometric method was significantly higher than the first aneroid reading (113.0±9.3 mm Hg vs 112.3±8.3 mm Hg; P=.003). No significant difference was found between the two methods for the second systolic BP readings (110.0±8.7 mm Hg vs 110.4±8.4 mm Hg; P=.11) or for the mean of the two readings obtained by each method (111.5±8.6 mm Hg vs 111.3±8.1 mm Hg; P=.39). For diastolic BP, the first and second measurement and the average of the two measurements were significantly lower with the oscillometric monitor (62.5±7.9 mm Hg vs 64.8±7.0 mm Hg [P<.001]; 60.5±7.7 mm Hg vs 65±7 mm Hg [P<.001]; and 61.5±8.0 mm Hg vs 64.5±6.8 mm Hg [P<.001], respectively).
Table 1.
The Mean Systolic and Diastolic Blood Pressure by Each Consecutive Measurement
| Measurement number | mm Hg |
|---|---|
| Systolic blood pressure | |
| 1 | 113.7±0.3 |
| 2 | 111.1±0.3 |
| 3 | 111.5±0.3 |
| 4 | 109.1±0.3 |
| Diastolic blood pressure | |
| 1 | 64.2±0.2 |
| 2 | 63.0±0.2 |
| 3 | 63.1±0.2 |
| 4 | 62.0±0.2 |
Data are presented as mean±standard error of the mean.
Table 2.
Difference Between Blood Pressure Readings Obtained Using the Oscillometric and Aneroid Monitors With Each Child Serving as Their Own Control
| Oscillometric Monitor, mm Hg | Aneroid Monitor, mm Hg | Mean Difference, mm Hg | P Value | |
|---|---|---|---|---|
| Systolic blood pressure | ||||
| First | 113.0±9 | 112.3±8 | 0.74±8 | .003 |
| Second | 110.0±9 | 110.4±8 | −0.38±7 | .11 |
| Mean | 111.5±9 | 111.3±8 | 0.18±7 | .39 |
| Diastolic blood pressure | ||||
| First | 62.5±8 | 64.8±7 | −2.3±9 | <.001 |
| Second | 60.5±8 | 64.5±7 | −4.0±9 | <.001 |
| Mean | 61.5±8 | 64.6±7 | −3.15±8 | <.001 |
Bold values indicate significance.
A scatter plot showing the correlation between each of the oscillometric and the aneroid measurements yielded a correlation coefficient (r) of 0.62 (P<.001) and 0.64 (P<.001) for the systolic BP readings and only 0.29 (P<.001) and 0.25 (P<.001) for the diastolic BP readings, respectively (Figure 1). The mean of the two oscillometric systolic BP readings was on average 0.18±7 mm Hg higher than the mean of the two aneroid readings (P=.39), with a difference ranging from −21 mm Hg to 21 mm Hg. The mean diastolic BP readings by the aneroid sphygmomanometer were on average 3.1±8.0 mm Hg higher than the oscillometric readings, with the difference ranging from −33 mm Hg to 35 mm Hg. The difference between the mean of the oscillometric and aneroid systolic BP readings obtained in all study subjects was within 5 mm Hg in 55%, 10 mm Hg in 88%, and within 15 mm Hg in 97% of participants. The difference between the mean of all oscillometric and aneroid diastolic BP readings was within 5 mm Hg in 46%, 10 mm Hg in 77%, and within 15 mm Hg in 92% of participants. Bland‐Altman analysis showed that the magnitude of the difference in systolic and diastolic BP between the two measurement methods was unrelated to the BP level (Figure 2).
Figure 1.
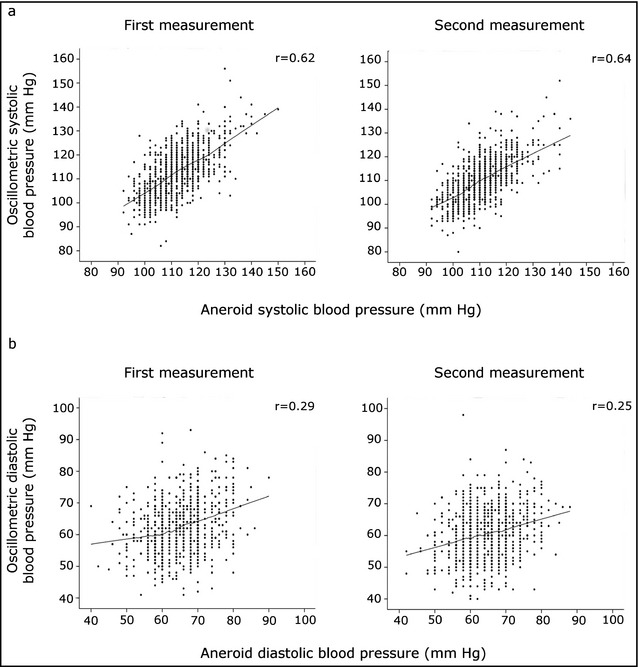
Correlation between each of the first two oscillometric and aneroid blood pressure readings. (a) Systolic blood pressure. (b) Diastolic blood pressure. P<.001 for all coefficients (Pearson′s r). Smoother lines are created with local regression.
Figure 2.
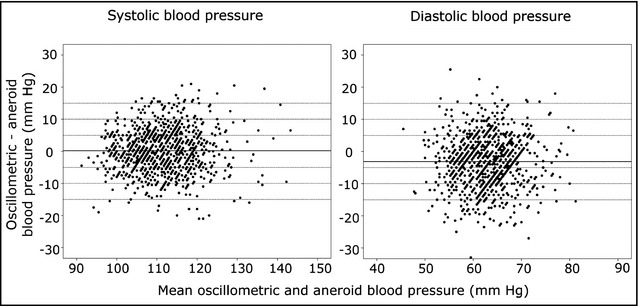
Bland‐Altman plot showing the magnitude of difference in systolic and diastolic blood pressure readings between the oscillometric and aneroid blood pressure monitors plotted against the mean of blood pressure readings with the two techniques. The solid horizontal line represents the mean blood pressure difference between the measurement methods.
There was a significant correlation between the difference in systolic BP obtained by the two methods and BMI (r=0.077, P=.013), while the correlation with BMI percentile, height, and weight did not reach statistical significance. The difference in diastolic BP obtained using the two methods correlated significantly with height (r=−0.10, P=.001) but not with weight, BMI, or BMI percentile. No sex variability was observed for the difference in BP values obtained by the two measurement methods (P=.2 for systolic BP and P=.4 for diastolic BP).
The mean of the two oscillometric systolic BP readings was elevated (≥95th percentile) in 15.7% of the children and the mean of the two aneroid systolic BP readings in 14.1% (P=.23). Although the frequency of elevated BP did not differ significantly between the two measurement methods, the agreement between the oscillometric and aneroid monitors in detecting elevated systolic BP was limited (κ statistic = 0.39), as is shown in Table 3. The agreement in the diagnosis of elevated diastolic BP was not calculated as it was present in only very few children. Of the 154 patients (15.7%) who had elevated oscillometric systolic BP, only 69 (44.8%) had elevated BP using the aneroid monitor and an additional 34 (22.1%) had BP in the prehypertension range (90th–95th percentile). Among the 138 patients (14.1%) with elevated BP detected by the aneroid device, only 69 (50%) had elevated BP using the automated oscillometric monitor and an additional 35 (25.4%) had BP in the prehypertension range.
Table 3.
Agreement Between the Mean of Oscillometric and Aneroid Blood Pressure Measurements for the Whole Group of Children in the Diagnosis of Elevated Systolic Blood Pressure (SBP)
| Aneroid SBP | ||
|---|---|---|
| ≥95% | <95% | |
| Oscillometric SBP | ||
| ≥95% | 7.0% | 8.7% |
| <95% | 7.0% | 77.2% |
κ statistic is 0.39, limited agreement (>0.7 = good, 0.4–0.7 = medium, <0.4 = limited agreement).
Regardless of the BP measurement technique applied, the first systolic and diastolic BP measurements were significantly higher than each of the subsequent readings (Table 1). The rmANOVA showed the changes between consecutive BP measurements to be significant, except between the second and the third measurements of both systolic and diastolic BP. The interaction between systolic BP and the measurement order was significant (P=.002) and the systolic BP was significantly higher with the oscillometric monitor during the first measurement (adjusted mean±standard error of the mean 114.8±0.40 vs 112.7±0.38 mm Hg, P<.001) but lower when the fourth measurement was carried out (108.3±0.37 mm Hg vs 109.9±0.40 mm Hg, P=.004). No difference was noted between the two monitors for the second and the third measurements (Figure 3). The interaction between diastolic BP and the measurement order was also significant (P<.001), with no statistical difference noted for the first diastolic BP reading obtained by the two monitors, while the second, third, and fourth readings were significantly lower with the oscillometric method (adjusted means, 61.3±0.33 vs 64.4±0.31 mm Hg [P<.001]; 61.4±0.32 vs 65.0±0.34 mm Hg [P<.001]; and 59.8±0.32 vs 64.6±0.34 mm Hg [P<.001], respectively) (Figure 3).
Figure 3.
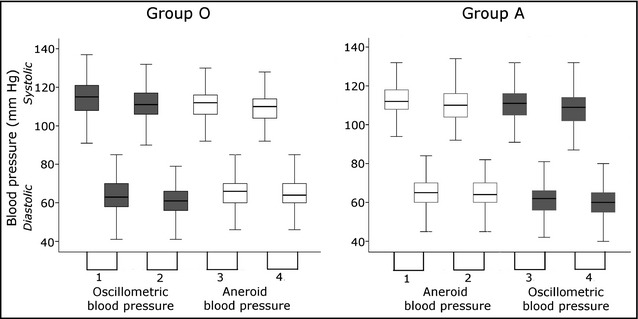
Boxplot showing the four sequential systolic and diastolic blood pressure readings for group O (oscillometric measurements first) and group A (aneroid measurements first). Children in group O first underwent two oscillometric and then two aneroid measurements and children in group A had their blood pressure measured by the two techniques in reverse order. The boxes show the interquartile range, the line across the box denotes the median blood pressure value, and the whiskers indicate the range of values, excluding outliers. The shaded boxes represent the oscillometric measurements and the white boxes the aneroid measurements.
Discussion
In this study, we compared BP measurements obtained using aneroid and oscillometric monitors in 9‐ to 10‐year‐old Icelandic children. We found no difference between the two techniques for average systolic BP, while diastolic BP was significantly lower with the oscillometric method. Further analysis showed a minor difference in systolic BP between the two methods when the order of measurements was accounted for. Although the mean difference between the two methods was trivial, a marked variability in the BP difference was observed. A significant downward trend in BP was observed with each repeated measurement and agreement between the BP monitors was limited.
The current study is the first one to compare an aneroid sphygmomanometer with an oscillometric BP monitor in a population‐based sample. However, Flynn and colleagues16 compared an aneroid sphygmomanometer and an oscillometric ambulatory BP monitor in a population of 235 children with CKD, with a median age of 12 years, many of whom were taking antihypertensive medications (72%). The mean of three aneroid measurements was compared with the mean of two oscillometric measurements as the authors omitted the first oscillometric reading from the calculation. The oscillometric monitor overestimated both systolic and diastolic BP by 9 mm Hg and 6 mm Hg, respectively. Unfortunately, the measurements obtained with the two BP devices were not performed at the same time, which means that the BP difference observed could have been caused by a true variability in BP rather than a real difference between the BP monitors. Several previous studies have compared mercury sphygmomanometer and automated oscillometric BP measurements in children. The largest one is the San Antonio Triethnic Children BP Study,19 which included 7208 children, aged 5 to 17 years, who underwent three BP measurements with a Dinamap 8100 oscillometric BP monitor (Critikon, Inc, Tampa, FL) and three measurements with a mercury sphygmomanometer. Approximately half of the study subjects had their first three BP measurements obtained by the Dinamap monitor while the other half had their BP first measured using the mercury sphygmomanometer. In contrast to our findings, the oscillometric BP readings were on average approximately 11 mm Hg higher than those obtained using the mercury sphygmomanometer. Furthermore, in a study of prepubertal diabetic children carried out by Australian investigators, the Dinamap 8100 overestimated the systolic BP by 5 mm Hg and underestimated the diastolic BP reading by 2 mm Hg when compared with a conventional mercury sphygmomanometer.20 A number of other studies have found BP obtained using oscillometric monitors to be either higher10 or lower9 than with mercury sphygmomanometers. These inconsistencies are most likely explained by the different BP devices used in each study. The fact that diastolic BP seems to be lower with the oscillometric method may either suggest difficulties in the determination of the fifth Korotkoff sound with the auscultatory technique or the fact that the oscillometric monitor detects vibrations in the arterial wall rather than the actual BP.
Two recent US studies14, 15 have investigated the difference between BP measurements obtained with aneroid and mercury sphygmomanometers. The first study14 compared the two measurement techniques in 727 individuals participating in the National Health and Nutrition Examination Survey (NHANES) and found systolic BP to be minimally higher with the aneroid sphygmomanometer in children aged 8 to 17 years. In the other study,15 Shah and colleagues conducted a comparison of aneroid and mercury BP monitors among 193 participants in the SEARCH for Diabetes in Youth Study and found no difference between the two methods in the mean systolic BP, while the diastolic BP was slightly lower with the aneroid monitor.
In the present study, a significant downward trend was observed with each consecutive measurement of both systolic and diastolic BP. Limited data have been published on the effect of repeated measurements on BP readings. However, a recent study in the United Kingdom clearly demonstrated that the first BP reading is significantly higher than the subsequent readings irrespective of whether oscillometric or manual auscultatory measurement methods were used.11 Although the first 3 measurements in the aforementioned Australian study demonstrated a downward trend, the difference between the readings was not significant.20 The effect of repeated measurements appears to be independent of the method used. The reason for this phenomenon is not fully understood but it seems likely that the additional rest and stress reduction associated with increasing number of measurements may play a significant role. The effect of repeated measurements, however, makes the comparison of different BP measurement techniques difficult. After assigning the children to two groups, O and A, we used two strategies to control for the known reduction in BP values that occurs with increasing number of measurements. First, when each child served as its own control and the first and second BP readings were compared with the third and fourth readings, approximately half of the children had their BP first measured using the automated oscillatory method and the other half with the aneroid sphygmomanometer, which should cancel out the effect of measurement order on the difference in BP obtained by the two techniques. Secondly, we compared each of the two oscillometric readings in one group with the corresponding two aneroid measurements in the other group, thereby eliminating the effect of measurement order on the BP difference. If the BP measurements in all the children had first been carried out using the same device, it would have been impossible to differentiate the effect of measurement order from a true difference between the measurement techniques.
Using either strategy, the first systolic BP reading was slightly higher with the oscillometric monitor. However, the fourth systolic BP reading was higher with the aneroid technique when the two groups were compared. This inconsistency is probably of little clinical significance, considering the small magnitude of the average BP difference between the measurement techniques. The observed reduction in diastolic BP with repeated measurements was more consistent with the oscillometric technique, which yielded lower readings on all but the first measurement. Auscultatory difficulties may have resulted in overestimation of the diastolic BP with the aneroid device. In addition, some of the discordance between the oscillometric and aneroid diastolic BP measurements could be attributable to digital preference for the aneroid measurements. Moreover, the possibility that the software of the oscillometric device could not reliably determine K5 cannot be excluded.
While the average systolic BP readings with the oscillometric and aneroid monitors were similar in our study, there was considerable variation in the BP readings between the two monitors for each individual child. This variability resulted in limited agreement between the two techniques in diagnosing elevated BP (systolic BP ≥95th percentile), as approximately 50% of those found to have elevated BP by one method were normotensive with the other. The agreement improved to approximately 70% when children with BP in the prehypertensive range were included in this analysis. Flynn and colleagues16 reported similar findings when they compared BP measurements in children with CKD obtained using aneroid and oscillometric methods. In their study, the agreement between the methods in classification of the BP was limited (approximately 60%, κ statistic 0.27). Limited agreement between auscultatory and automated oscillometric measurement techniques has also been described in a number of other studies.9, 10, 12, 19, 20, 21, 22, 23 Notably, in the normative BP dataset published by the National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents, there is only a 4 mm Hg difference between BP in the prehypertensive (BP in the 90th percentile) and hypertensive (95th percentile) range. Therefore, multiple BP measurements are recommended before the diagnosis of elevated BP or hypertension is made using either method.
In the current study, the mean difference in systolic BP obtained with the two monitors correlated positively with BMI. While we do not have a plausible explanation for this finding, one can speculate that auscultatory difficulties in overweight children may have contributed to the observed BP difference. No published studies are available for comparison.
Study Strengths
The population‐based sample and the large number of participating children are the main strengths of this study, yielding 80% power to detect a mean difference of 0.7 mm Hg between the two methods. We also believe that the narrow age range of our study sample may reduce measurement errors as anthropometric measures are likely to be more homogenous than in a group of children with a wider age range. Furthermore, the aneroid BP measurements were all performed by the same physician, which should have decreased measurement variability.
Study Limitations
A relatively small number of BP measurements performed with each method may be viewed as a potential limitation of our study. Because of the significant decline in BP readings observed with increasing number of measurements, more than two recordings may have been needed with each BP monitor to accurately assess the agreement between them. Another limitation is the lack of validation of the two BP devices in children. Finally, the precision of the BP readings may have been affected by a slight difference in the width of the BP cuffs used in the study, which were specifically designed for each BP monitor.
Conclusions
The first systolic BP was higher with the oscillometric technique, whereas no significant differences between the mean values of all systolic BP readings obtained with the aneroid sphygmomanometer and the oscillometric BP monitors were observed. The oscillometric diastolic BP was similar to or lower than the corresponding aneroid BP. Although the mean difference between the two BP measurement techniques was trivial, a significant intraindividual variability in BP readings was observed that explains the limited agreement between the two techniques in the diagnosis of elevated BP. Elevated BP readings with either technique should be interpreted with caution and multiple measurements are encouraged to facilitate an accurate diagnosis of hypertension.
Funding
The study was supported by Landspitali – The National University Hospital of Iceland Research Fund.
Disclosures and acknowledgements
Sigridur Birna Eliasdottir and Sandra Dis Steinthorsdottir contributed equally to this work. Preliminary results of this study appeared in an abstract form at the Biennial Meeting of the Nordic Society of Nephrology in Helsinki, Finland, August 2009, and the Annual Meeting of the European Society of Pediatric Nephrology in Birmingham, UK, in September of 2009.
We would like to thank the participants and all the principals, teachers, and secretaries at the participating schools for their support. We would also like to thank all the school nurses who measured the height and weight of the participating children.
We are grateful to Vistor Inc (Horgatun 2, 210 Gardabaer, Iceland) for kindly providing the oscillometric Philips blood pressure monitor. None of the authors have any affiliations with Vistor. Finally, we thank Loftur I. Bjarnason, Computer Scientist, for data management and programming.
Statement of Financial Disclosure
The authors have no financial relationship relevant to this article or conflict of interest to disclose.
J Clin Hypertens (Greenwich). 2013;15:776–783. ©2013 Wiley Periodicals, Inc.24112661
References
- 1. Sorof JM, Lai D, Turner J, et al. Overweight, ethnicity, and the prevalence of hypertension in school‐aged children. Pediatrics. 2004;113:475–482. [DOI] [PubMed] [Google Scholar]
- 2. Genovesi S, Giussani M, Pieruzzi F, et al. Results of blood pressure screening in a population of school‐aged children in the province of Milan: role of overweight. J Hypertens. 2005;23:493–497. [DOI] [PubMed] [Google Scholar]
- 3. McNiece KL, Poffenbarger TS, Turner JL, et al. Prevalence of hypertension and pre‐hypertension among adolescents. J Pediatr. 2007;150:640–644. [DOI] [PubMed] [Google Scholar]
- 4. Steinthorsdottir SD, Eliasdottir SB, Indridason OS, et al. Prevalence of hypertension in 9‐ to 10‐year‐old Icelandic school children. J Clin Hypertens. 2011;10:774–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Erlingsdottir A, Indridason OS, Thorvaldsson O, Edvardsson VO. Blood pressure in children and target‐organ damage later in life. Pediatr Nephrol. 2010;25:323–328. [DOI] [PubMed] [Google Scholar]
- 6. Raitakari OT, Juonala M, Kahonen M, et al. Cardiovascular risk factors in childhood and carotid artery intima‐media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–2283. [DOI] [PubMed] [Google Scholar]
- 7. Berenson GS, Srinivasan SR, Bao W, et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults: the Bogalusa Heart Study. N Engl J Med. 1998;338:1650–1656. [DOI] [PubMed] [Google Scholar]
- 8. Nelson MR, Quinn S, Bowers‐Ingram L, et al. Cluster‐randomized controlled trial of oscillometric vs. manual sphygmomanometer for blood pressure management in primary care (CRAB). Am J Hypertens. 2009;22:598–603. [DOI] [PubMed] [Google Scholar]
- 9. Wong SN, Tz Sung RY, Leung LC. Validation of three oscillometric blood pressure devices against auscultatory mercury sphygmomanometer in children. Blood Press Monit. 2006;11:281–291. [DOI] [PubMed] [Google Scholar]
- 10. Park MK, Menard SW, Yuan C. Comparison of auscultatory and oscillometric blood pressures. Arch Pediatr Adolesc Med. 2001;155:50–53. [DOI] [PubMed] [Google Scholar]
- 11. Miranda JJ, Stanojevic S, Bernabe‐Ortiz A, et al. Performance of oscillometric blood pressure devices in children in resource‐poor settings. Eur J Cardiovasc Prev Rehabil. 2008;15:362–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mattu GS, Heran BS, Wright JM. Comparison of the automated non‐invasive oscillometric blood pressure monitor (BpTRU) with the auscultatory mercury sphygmomanometer in a paediatric population. Blood Press Monit. 2004;9:39–45. [DOI] [PubMed] [Google Scholar]
- 13. Barker ME, Shiell AW, Law CM. Evaluation of the Dinamap 8100 and Omron M1 blood pressure monitors for use in children. Paediatr Perinat Epidemiol. 2000;14:179–186. [DOI] [PubMed] [Google Scholar]
- 14. Ostchega Y, Prineas RJ, Nwankwo T, Zipf G. Assessing blood pressure accuracy of an aneroid sphygmomanometer in a national survey environment. Am J Hypertens. 2011;24:322–327. [DOI] [PubMed] [Google Scholar]
- 15. Shah AS, Dolan LM, D'Agostino RB Jr, et al. Comparison of mercury and aneroid blood pressure measurements in youth. Pediatrics. 2012;129:e1205–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Flynn JT, Pierce CB, Miller ER 3rd, et al. Reliability of resting blood pressure measurement and classification using an oscillometric device in children with chronic kidney disease. J Pediatr. 2012;160:434–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Graves JW, Tibor M, Murtagh B, et al. The Accoson Greenlight 300, the first non‐automated mercury‐free blood pressure measurement device to pass the International Protocol for blood pressure measuring devices in adults. Blood Press Monit. 2004;9:13–17. [DOI] [PubMed] [Google Scholar]
- 18. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents . The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(Suppl 2 4th Report):555–576. [PubMed] [Google Scholar]
- 19. Menard SW, Park MK, Yuan CH. The San Antonio Biethnic Children's Blood Pressure Study: auscultatory findings. J Pediatr Health Care. 1999;13:237–244. [DOI] [PubMed] [Google Scholar]
- 20. Jin RZ, Donaghue KC, Fairchild J, et al. Comparison of Dinamap 8100 with sphygmomanometer blood pressure measurement in a prepubertal diabetes cohort. J Paediatr Child Health. 2001;37:545–549. [DOI] [PubMed] [Google Scholar]
- 21. Midgley PC, Wardhaugh B, Macfarlane C, et al. Blood pressure in children aged 4–8 years: comparison of Omron HEM 711 and sphygmomanometer blood pressure measurements. Arch Dis Child. 2009;94:955–958. [DOI] [PubMed] [Google Scholar]
- 22. Narogan MV, Narogan MI, Syutkina EV. Validation of A&D UA‐778 blood pressure monitor in children. Blood Press Monit. 2009;14:228–231. [DOI] [PubMed] [Google Scholar]
- 23. Stergiou GS, Yiannes NG, Rarra VC. Validation of the Omron 705 IT oscillometric device for home blood pressure measurement in children and adolescents: the Arsakion School Study. Blood Press Monit. 2006;11:229–234. [DOI] [PubMed] [Google Scholar]



 Comparison of Aneroid and Oscillometric Blood Pressure Measurements in Children
Comparison of Aneroid and Oscillometric Blood Pressure Measurements in Children