Abstract
There are currently few recommendations on how to assess inter‐arm blood pressure (BP) differences. The authors compared simultaneous with sequential measurement on mean BP, inter‐arm BP differences, and within‐visit reproducibility in 240 patients stratified according to age (<50 or ≥60 years) and BP (<140/90 mm Hg or ≥140/90 mm Hg). Three simultaneous and three sequential BP measurements were taken in each patient. Starting measurement type and starting arm for sequential measurements were randomized. Mean BP and inter‐arm BP differences of the first pair and reproducibility of inter‐arm BP differences of the first and second pair were compared between both methods. Mean systolic BP was 1.3±7.5 mm Hg lower during sequential compared with simultaneous measurement (P<.01). However, the first sequential measurement was on average higher than the second, suggesting an order effect. Absolute systolic inter‐arm BP differences were smaller on simultaneous (6.2±6.7/3.3±3.5 mm Hg) compared with sequential BP measurement (7.8±7.3/4.6±5.6 mm Hg, P<.01 for both). Within‐visit reproducibility was identical (both r=0.60). Simultaneous measurement of BP at both arms reduces order effects and results in smaller inter‐arm BP differences, thereby potentially reducing unnecessary referral and diagnostic procedures.
Inter‐arm blood pressure (BP) differences have been established since the early 20s of the last century.1 The importance of assessing inter‐arm BP differences is to prevent underestimation and undertreatment of hypertension because the arm with the highest BP should be taken as a reference. Therefore, guidelines on BP measurement recommend bilateral BP measurement at a patient's first visit.2, 3 In addition, large inter‐arm BP differences in systolic BP (SBP) may indicate the presence of atherosclerotic plaques and other vascular occlusive diseases and are associated with increased cardiovascular risk.4, 5 A recent meta‐analysis of studies assessing the inter‐arm BP differences showed that a SBP difference ≥15 mm Hg was associated with an increased risk of cardiovascular mortality.6 This is in line with another recent prospective study in hypertensive primary care patients, which showed that a BP difference of ≥10 mm Hg was an independent predictor of cardiovascular events and all‐cause mortality after 10 years of follow‐up.7
Despite the clinical relevance of inter‐arm BP differences, there are few recommendations on how they should be assessed. The recently released guidelines on arterial hypertension of the European Society of Cardiology (ESC) and European Society of Hypertension (ESH) recommend simultaneous measurement, although this recommendation is not supported by evidence. Sequential measurement of inter‐arm BP differences is potentially influenced by order effects as the first BP is on average higher than subsequent readings.8 Indeed, more patients with a large inter‐arm BP difference were found in studies that used sequential assessment of inter‐arm BP differences compared with studies that assessed BP simultaneously.9 Simultaneous measurements, on the other hand, may directly influence BP. Previous studies have shown that unilateral cuff inflation may increase SBP from 4 mm Hg to 9 mm Hg.10, 11, 12 Explanatory mechanisms include muscle compression,13 pain and discomfort during the measurement,14 and increased arousal as a result of the knowledge that BP is being measured.15 This reactive rise in BP might be stronger during simultaneous bilateral BP measurement compared with unilateral sequential measurements.
Our primary objective was therefore to assess BP differences between sequential and simultaneous measurements. Our second aim was to compare absolute inter‐arm BP differences and within‐visit reproducibility of inter‐arm BP differences between these methods in normotensive and hypertensive patients at low and high risk for cardiovascular disease.
Patients
We performed a randomized cross‐over study between April 2010 and May 2012 to compare BP, inter‐arm BP differences, and within‐visit reproducibility between simultaneous and sequential BP measurement. Prior to the study, we defined 4 groups according to BP status (BP <140/90 mm Hg or ≥140/90 mm Hg) and age (<50 or ≥60 years) to ensure that patients at low and high cardiovascular risk were included. An equal number of patients were included in each group. Patients were hospital employees, students, or patients recruited from the hypertension clinic of a large teaching hospital in Amsterdam, the Netherlands. Patients were included if they were aged 18 years or older and able to provide written informed consent. Reasons for exclusion were pregnancy, smoking or coffee consumption <1 hour before the study visit, inability to acquire valid measurements (eg, when the arm was too large to fit an appropriate cuff or because of cardiac arrhythmias), and established unilateral or bilateral abnormalities influencing blood flow or causing obstruction of the lymphatic system to the left or right arm.
All eligible participants provided informed consent. The study was approved by the institutional review board.
Methods
Cardiovascular risk was assessed by a standardized questionnaire that included age, medication use, current smoking status, alcohol drinking behavior, ethnicity (self‐defined black, white, or other), and history of diabetes, hypertension, and cardiovascular events. Self‐reported dyslipidemia, diabetes, and hypertension or use of statin therapy, glucose‐lowering therapy, or BP‐lowering medication was used to define the presence of dyslipidemia, diabetes, and hypertension, respectively. For alcohol intake, the number of patients with a daily alcohol consumption of ≥2 units (women) or ≥3 units (men) was documented. Height and weight were registered to calculate body mass index (BMI). BP was taken after at least 5 minutes of rest while seated, with appropriately sized cuffs positioned at heart level and both arms supported. Sequential and simultaneous BP measurements were taken with the same validated BP device (Watch BP office ABI, Microlife, Widnau, Switzerland).16, 17 This device is equipped with two linked cuffs allowing both simultaneous and sequential measurement with the same device.
The first BP measurement was taken on the nondominant arm and used to classify patients into BP categories. Subsequently, the order of measurement type (sequential vs simultaneous) and sequence (starting arm for sequential measurements) were randomized using a computer‐generated randomization scheme. For sequential measurement, 3 measurements alternating between arms (ie, left‐right‐left or vice versa) were taken. To avoid time‐order effects, an equal number of readings were taken for simultaneous measurements, meaning that 3 simultaneous pairs were recorded in every patient. For sequential measurements, we defined the first BP pair as the first and second measurement, and the second pair as the second and third measurement. During all measurements both cuffs remained attached to both arms.
Mean BP of the first simultaneous and sequential pair was compared to calculate BP differences between both methods. To correct for a potential order effect, we also compared the mean BP of every individual sequential measurement with the mean BP of the corresponding arm assessed by simultaneous measurement.
Inter‐arm BP differences were expressed as absolute values (without sign). To assess differences in inter‐arm BP differences between sequential and simultaneous measurements, we compared the first pair of both methods. We classified inter‐arm BP differences into 3 commonly used categories (≥10, ≥15, and ≥20 mm Hg) to assess the number of patients with large inter‐arm BP differences. We compared the categorized inter‐arm BP differences between the first and second pair of each method and between the first pairs of both methods. Cardiovascular events were defined as a history of ischemic stroke, transient ischemic attack (TIA), myocardial infarction, or peripheral vascular disease. Cardiovascular risk factors were defined as a history of hypertension, diabetes, or dyslipidemia, male sex, age 60 years or older, current smoker, alcohol use of ≥2 units per day for women and ≥3 units per day for men, and a BMI >25 kg/m2.
Sample Size Calculation and Statistical Analysis
To assess whether simultaneous BP measurement influences absolute BP levels, we assumed that an SBP difference of ≥2 mm Hg with sequential measurement would be clinically relevant. A 2 mm Hg increase in SBP is associated with a 10% increase in stroke risk and a 7% increase in risk of ischemic heart disease.18 Assuming a standard deviation (SD) difference of 11 mm Hg, we calculated that 239 persons would be needed to demonstrate a 2 mm Hg difference with 80% power and α=0.05.19 We aimed to include 240 patients with 60 patients in each stratum.
Baseline variables were expressed as mean and SD for variables with a parametric distribution. Categorical variables were expressed as actual numbers and percentages. Differences in parametric variables between patients were compared with an independent t test and within patients with a paired t test. Differences in parametric variables among subgroups were compared with analysis of variance with post‐hoc analysis where appropriate. Categorical variables were compared with Pearson's χ2 between patients and with the McNemar test for within‐patient comparison. Correlations of parametric variables were assessed with Pearson's correlation coefficient. Bland‐Altman analysis was used to express within‐visit reproducibility of inter‐arm BP differences by simultaneous and sequential BP measurement.
Results
A flow‐chart of study participants is shown in the supplemental data. After exclusion, 60 patients were included in each group, totaling 240 patients aged 52±21 years, of which 107 were men (45%). Baseline characteristics stratified for age and BP are presented in Table 1. Older patients reported most cardiovascular events, including 28 (23%) patients with ischemic stroke or TIA, 12 (10%) with coronary artery disease, and 12 (10%) with peripheral artery disease. Younger patients reported 3 (3%) ischemic strokes or TIAs, 2 (2%) coronary artery diseases, and 1 (1%) peripheral artery disease.
Table 1.
Baseline Characteristics (N=240)
| Young and BP | Old and BP | Young and BP | Old and BP | |
|---|---|---|---|---|
| <140 and <90 mm Hg | <140 and <90 mm Hg | ≥140 and/or ≥90 mm Hg | ≥140 and/or ≥90 mm Hg | |
| (n=60) | (n=60) | (n=60) | (n=60) | |
| Age, y | 26.6 (6.7) | 72.9 (8.8) | 39.7 (6.8) | 69.7 (8.6) |
| Men | 20 (33) | 26 (43) | 27 (45) | 34 (57) |
| BMI | 23.9 (4.1) | 26.8 (6.8) | 27.9 (6.3) | 26.5 (4.0) |
| White | 46 (77) | 50 (83) | 28 (47) | 53 (88) |
| SBP | 120 (10.9) | 126 (14.2) | 154.2 (17.5) | 160.1 (19.0) |
| DBP | 72.8 (7.7) | 73.6 (9.6) | 98.7 (12.1) | 88.5 (10.6) |
| CVE | 0 | 22 (37) | 3 (5) | 16 (27) |
| Smoking | 18 (30) | 9 (15) | 15 (25) | 9 (15) |
| DM | 4 (7) | 16 (27) | 9 (15) | 13 (22) |
| Hypertension | 6 (10) | 38 (63) | 44 (73) | 44 (73) |
| Dyslipidemia | 3 (5) | 19 (32) | 6 (10) | 16 (27) |
| Alcohol | 12 (20) | 10 (17) | 6 (10) | 9 (15) |
| CV risk factors | 1.3 (1.0) | 2.9 (1.3) | 2.7 (1.2) | 4.0 (1.2) |
Abbreviations: BP, blood pressure; BMI, body mass index; CV, cardiovascular; CVE, cardiovascular events defined as a documented ischemic stroke, transient ischemic attack, myocardial infarction, or documented peripheral vascular disease; DBP, diastolic blood pressure; DM, diabetes mellitus; old, 60 years and older; SBP, systolic blood pressure; young, younger than 50 years.
Continuous variables are expressed as mean (standard deviation [SD]) and frequencies as numbers (percentages).
Mean BP
The mean SBP of the first pair was lower with sequential measurement (134.3±20.2 mm Hg) than by simultaneous measurement (135.7±21.1 mm Hg, Δ 1.3±7.5 mm Hg; P<.01), while diastolic BP (DBP) values did not differ (81.0±14.9 mm Hg vs 81.4±15.1 mm Hg, Δ 0.4±5.3 mm Hg; P=.21). The difference in SBP disappeared when comparing the mean SBP of the first pair of sequential measurement with the mean SBP of the first two simultaneous measurements taken at the corresponding arms of sequential measurements (Δ 0.5±6.8 mm Hg; P=.24).
Mean SBP was higher on the arm that was measured first (135.1±20.9 mm Hg) compared with the arm that was measured second (133.5±21.0, P=.03) with sequential measurement. When comparing these BPs with the mean BP of the corresponding arm of the simultaneous measurements, the first measurement was also higher (135.8±23.8 mm Hg) compared with the second measurement (133.8±21.7 mm Hg, P<.01). For hypertensive patients, the difference in SBP between the first and second measurement was 2.3±11.7 mm Hg on sequential (P=.03) and 2.6±10.2 mm Hg on simultaneous measurement (P<.01), while this difference was 0.7±9.4 mm Hg (P=.40) on sequential and 1.4±9.0 mm Hg (P=.10) on simultaneous measurement for normotensive patients.
Inter‐Arm BP Differences
Inter‐arm BP differences of the first pair of sequential measurements were larger (7.8±7.3/4.6±5.6 mm Hg) compared with the first pair of simultaneous measurements (6.2±6.7/3.3±3.5 mm Hg, P<.01 for both SBP and DBP values). Inter‐arm BP differences of the second pair of sequential measurement (7.6±7.6/4.2±3.8 mm Hg) were also larger compared with the first pair of simultaneous measurements (P<.01 both for systolic and diastolic values). Mean systolic inter‐arm BP difference on sequential measurement varied between 6.8±5.4 mm Hg for young normotensive and 9.2±8.8 mm Hg for old hypertensive patients, and for simultaneous measurements between 5.8±4.3 mm Hg for young normotensive and 6.9±7.4 mm Hg for young hypertensive patients.
Large systolic inter‐arm BP differences (≥10 mm Hg) were less often observed by simultaneous (18%) compared with sequential (26%) measurements (P<.01). Inter‐arm BP differences of ≥15 mm Hg and ≥20 mm Hg were found in 20 (8%) and 10 (4%) patients on simultaneous and 30 (13%) and 17 (7%) patients on sequential measurement (Table 2).
Table 2.
Reproducibility and Comparison of Systolic Inter‐Arm BP Differences According to Commonly Used Cutoff Values for Inter‐Arm BP Differences
| Inter‐Arm BP Difference | ≥10 mm Hg | ≥15 mm Hg | ≥20 mm Hg |
|---|---|---|---|
| First pair of simultaneous measurements | 44 | 20 | 10 |
| Identified by second pair of simultaneous measurements | 15 (34%) | 6 (30%) | 4 (40%) |
| Identified by first pair of sequential measurements | 21 (48%) | 12 (60%) | 5 (50%) |
| First pair of sequential measurements | 63 | 30 | 17 |
| Identified by second pair of sequential measurements | 33 (52%) | 16 (53%) | 7 (41%) |
| Identified by first simultaneous measurement | 21 (33%) | 13 (43%) | 5 (29%) |
Number of patients with a large inter‐arm BP difference found on first simultaneous measurement and first pair of sequential measurement and the number of identical patients with a large inter‐arm BP difference that was identified by either the first pair measurement of the other method or by the second pair of measurement of the same method.
Systolic inter‐arm BP differences assessed by sequential measurement correlated significantly with the number of cardiovascular risk factors (r=0.22, P<.01) and cardiovascular events (r=0.16, P=.01), but not with age and mean BP. Simultaneously assessed inter‐arm BP differences did not significantly correlate with the number of cardiovascular risk factors, cardiovascular events, age, or mean BP.
Within‐Visit Reproducibility
The Bland‐Altman plot in the Figure shows the absolute inter‐arm SBP differences of the first and second measurement pair for both methods. For sequential measurements, the mean difference between the first and second measurement was 0.2 mm Hg, with an SD of 8.1 mm Hg. For simultaneous measurements, the mean difference was 1.0 mm Hg, with an SD of 6.8 mm Hg.
Figure .
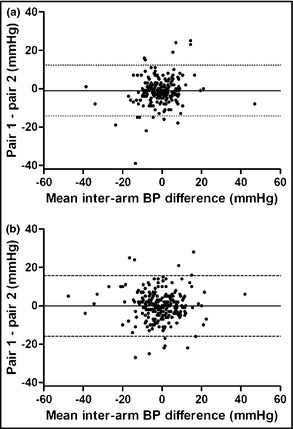
Bland‐Altman plot for inter‐arm blood pressure (BP) differences of simultaneous (a) and sequential (b) BP assessment.
The correlation coefficients of the systolic inter‐arm BP difference between the first and second pairs for sequential and simultaneous measurements were identical (r=0.60, P<.01 for both). The reproducibility of commonly used cut‐off values for inter‐arm BP differences and the number of patients who could be identified by the alternative method is shown in Table 2. The total number of patients who fell into another inter‐arm BP category when comparing the first with the second inter‐arm BP difference was larger for sequential (75 [31%] for systolic and 88 [37%] for diastolic) compared with simultaneous measurements (3 [22%] for systolic, P=.03, and 68 [28%] for diastolic, P=.06).
Discussion
Simultaneous BP measurement results in a slightly but significantly higher BP compared with sequential BP measurement. This difference disappeared when taking two separate BP measurements from the first two simultaneous measurements, pointing towards an order effect. Simultaneous measurement of inter‐arm BP differences led to smaller inter‐arm differences compared with sequential measurement and markedly reduced the number of patients with clinically relevant inter‐arm BP differences with similar reproducibility.
The marginally higher SBP values during simultaneous compared with sequential measurement may suggest that the reactive rise in BP is more outspoken during bilateral compared with unilateral BP measurement. However, this difference was principally attributable to an order effect: when comparing BP of the first and second sequential measurement with the BP at the first and the second simultaneous measurement at the corresponding arm, there were no differences in BP. This suggests that for reliable identification of the arm with the highest BP simultaneous measurement is preferred over sequential measurement.
When looking at inter‐arm BP differences, we found fewer patients with a large inter‐arm BP difference on simultaneous measurement. This finding is in line with a recent meta‐analysis which showed that simultaneous measurement leads to fewer patients with large inter‐arm BP differences compared with sequential measurements.9 This conclusion was drawn by pooling the average inter‐arm BP difference of studies in which the inter‐arm BP difference was assessed simultaneously and comparing them with the pooled average of studies that measured inter‐arm BP differences sequentially. Only two studies included in the meta‐analysis directly compared simultaneous with sequential inter‐arm BP differences in the same patients.20, 21 These studies reported smaller inter‐arm BP differences on simultaneous measurements compared with sequential measurement. However, in both studies, auscultatory BP was used as a comparison, which has been shown to be less accurate in assessing inter‐arm BP differences.9 Another study comparing both methods that was not included in the meta‐analysis reported fewer patients with a large inter‐arm BP difference on simultaneous compared with sequential measurements.22 However, in this study, no true sequential measurements were performed as they were derived from randomly taking one arm of each simultaneous measurement. To avoid these shortcomings, we compared simultaneous with sequential measurements in the same population with the same device and randomized between measurement types as well as starting arm of the sequential measurements. In line with these previous studies, we demonstrated that fewer patients had a large inter‐arm BP difference on simultaneous measurement and also found significantly smaller inter‐arm BP differences on simultaneous compared with sequential measurements.
It has been proposed that inter‐arm BP differences should initially be assessed sequentially and subsequently confirmed by repeated simultaneous measurement when a large inter‐arm BP difference is found.23 When we apply that to the current study population, 2 of 3 patients with an initial large systolic inter‐arm BP difference (≥10 mm Hg) on initial sequential measurement would have a normal inter‐arm BP difference (<10 mm Hg) on a single simultaneous measurement. Adding a second simultaneous measurement further reduced this number, preventing unnecessary diagnostic procedures. Given the high prevalence of large inter‐arm BP differences, simultaneous measurement should therefore be preferred over sequential measurement in assessing inter‐arm BP differences at a patient's first visit.
The clinical significance of inter‐arm BP differences has recently been subject of debate following the publications of Clark and coworkers on the relationship between inter‐arm BP differences and cardiovascular morbidity and mortality. In a meta‐analysis, they demonstrated that inter‐arm SBP differences ≥15 mm Hg with pre‐existent cerebrovascular disease increased cardiovascular mortality and all‐cause mortality.6 This was confirmed in two prospective studies which showed that inter‐arm differences ≥10 mm Hg were an independent predictor for all‐cause mortality.7, 24 These data suggest that systolic inter‐arm differences of ≥10 mm Hg could be considered as an independent risk factor for cardiovascular disease on a population level. However, because the within‐visit reproducibility is poor, it might be a less suitable marker for individual cardiovascular risk prediction.
Study Limitations
Our study has some limitations. First, we did not determine associations between inter‐arm BP differences and vascular pathology in our patients. Second, we do not know whether the simultaneous measurements were truly taken simultaneously because of small differences in the latency of cuff deflation. It is likely that, especially in patients with large inter‐arm BP differences, some differences in measurement time still existed. Nonetheless, simultaneous measurements taken according to the study protocol still showed a clear benefit in reducing the number of patients with large inter‐arm BP differences compared with sequential measurement.
Conclusions
For a reliable estimation of the inter‐arm BP difference, simultaneous measurement should be preferred over sequential BP assessment at a patient's initial visit as it is less influenced by order effects compared with sequential BP measurement and results in smaller inter‐arm BP differences. Within‐visit reproducibility of inter‐arm BP differences assessed by both methods was poor, thereby limiting their use for individual cardiovascular risk prediction.
Supporting information
Figure S1. Flowchart of study participants.
Acknowledgments and Disclosures
The WatchBP office device used for this study was kindly provided by Microlife (Stirling, United Kingdom) without any further involvement in the study. No conflict of interest to disclose.
J Clin Hypertens (Greenwich). 2013;15:839–844. ©2013 Wiley Periodicals, Inc.
References
- 1. Cyriax E. Unilateral alterations in blood pressure: the differential blood‐pressure sign (second communication). Q J Med. 1921;14:309–313. [Google Scholar]
- 2. National Institute for Health and Clinical Excellence . Hypertension: the clinical management of primary hypertension in adults, CG127. NICE, 2011. 2011.
- 3. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–2219. [DOI] [PubMed] [Google Scholar]
- 4. Aboyans V, Criqui MH, McDermott MM, et al. The vital prognosis of subclavian stenosis. J Am Coll Cardiol. 2007;49:1540–1545. [DOI] [PubMed] [Google Scholar]
- 5. Aboyans V, Kamineni A, Allison MA, et al. The epidemiology of subclavian stenosis and its association with markers of subclinical atherosclerosis: the Multi‐Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2010;211:266–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Clark CE, Taylor RS, Shore AC, et al. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta‐analysis. Lancet. 2012;379:905–914. [DOI] [PubMed] [Google Scholar]
- 7. Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood pressure readings between arms and survival: primary care cohort study. BMJ. 2012;344:e1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gould BA, Hornung RS, Kieso HA, et al. Is the blood pressure the same in both arms? Clin Cardiol. 1985;8:423–426. [DOI] [PubMed] [Google Scholar]
- 9. Verberk WJ, Kessels AG, Thien T. Blood pressure measurement method and inter‐arm differences: a meta‐analysis. Am J Hypertens. 2011;24:1201–1208. [DOI] [PubMed] [Google Scholar]
- 10. Charmoy A, Wurzner G, Ruffieux C, et al. Reactive rise in blood pressure upon cuff inflation: cuff inflation at the arm causes a greater rise in pressure than at the wrist in hypertensive patients. Blood Press Monit. 2007;12:275–280. [DOI] [PubMed] [Google Scholar]
- 11. Musso NR, Giacche M, Galbariggi G, Vergassola C. Blood pressure evaluation by noninvasive and traditional methods. Consistencies and discrepancies among photoplethysmomanometry, office sphygmomanometry, and ambulatory monitoring. Effects of blood pressure measurement. Am J Hypertens. 1996;9:293–299. [DOI] [PubMed] [Google Scholar]
- 12. Veerman DP, van Montfrans GA, Wieling W. Effects of cuff inflation on self‐recorded blood pressure. Lancet. 1990;335:451–453. [DOI] [PubMed] [Google Scholar]
- 13. Julius S, Li Y, Brant D, et al. Neurogenic pressor episodes fail to cause hypertension, but do induce cardiac hypertrophy. Hypertension. 1989;13:422–429. [DOI] [PubMed] [Google Scholar]
- 14. Shapiro AP, outsos SE, rifcher E. Patterns of pressor response to noxious stimuli in normal, hypertensive, and diabetic subjects. J Clin Invest. 1963;42:1890–1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Redman S, Dutch J. Cardiovascular responses during cuff inflation in subjects who have been sensitised to the measurement of their blood pressure. N Z Med J. 1984;97:180–182. [PubMed] [Google Scholar]
- 16. Saladini F, Benetti E, Masiero S, Palatini P. Accuracy of Microlife WatchBP Office ABI monitor assessed according to the 2002 European Society of Hypertension protocol and the British Hypertension Society protocol. Blood Press Monit. 2011;16:258–261. [DOI] [PubMed] [Google Scholar]
- 17. Stergiou GS, Tzamouranis D, Protogerou A, et al. Validation of the Microlife Watch BP Office professional device for office blood pressure measurement according to the International protocol. Blood Press Monit. 2008;13:299–303. [DOI] [PubMed] [Google Scholar]
- 18. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 19. Stergiou GS, Baibas NM, Gantzarou AP, et al. Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens. 2002;15:101–104. [DOI] [PubMed] [Google Scholar]
- 20. Eguchi K, Yacoub M, Jhalani J, et al. Consistency of blood pressure differences between the left and right arms. Arch Intern Med. 2007;167:388–393. [DOI] [PubMed] [Google Scholar]
- 21. Lohmann FW, Eckert S, Verberk WJ. Interarm differences in blood pressure should be determined by measuring both arms simultaneously with an automatic oscillometric device. Blood Press Monit. 2011;16:37–42. [DOI] [PubMed] [Google Scholar]
- 22. Kleefstra N, Houweling ST, Meyboom‐de JB, Bilo HJ. [Measuring the blood pressure in both arms is of little use; longitudinal study into blood pressure differences between both arms and its reproducibility in patients with diabetes mellitus type 2]. Ned Tijdschr Geneeskd. 2007;151:1509–1514. [PubMed] [Google Scholar]
- 23. Clark CE. Inter‐arm blood pressure measurement needs to be practical and accurate. Am J Hypertens. 2011;24:1189–1190. [DOI] [PubMed] [Google Scholar]
- 24. Sheng CS, Liu M, Zeng WF, et al. Four‐limb blood pressure as predictors of mortality in elderly chinese. Hypertension. 2013;61:1155–1160. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Flowchart of study participants.


