Abstract
The aim of this study was to investigate impact of central blood pressure (BP) levels and sex on the difference between central and upper arm oscillometric BP values. Oscillometric arterial BP measurements of 675 patients were simultaneously compared with values measured from the ascending aorta. The patients were divided into 3 groups according to systolic BP levels. The upper arm oscillometric device overestimated systolic BP (SBP) at low and medium BP levels but it underestimated SBP at high BP level. As for the effect of sex on differences in central and oscillometric BP, SBP was overestimated to a lesser degree in women than in men at low BP levels, but it was more highly underestimated in women than in men at high BP levels. The difference between oscillometric upper arm BP and aortic BP was directly affected by the patient's central BP level. In addition, the difference between central and oscillometric BP was also affected by sex factor.
The limited accuracy of oscillometric devices has been mentioned in some studies.1, 2 Validation studies to determine the effect of blood pressure (BP) level on oscillometric BP measurement have had major limitations in that BP measurements cannot be taken simultaneously. As a result of extreme fluctuations in pressure at high BP levels, differences in pressure produced using different methods do not reflect true BP differences.3 It is essential to determine the reliability of new oscillometric devices compared with a mercury manometer, which is the gold standard reference method. However, literature related to central aortic BP does not adequately address the relationship between oscillometric BP and central BP measurement.
In recent large randomized controlled trials it has been shown that aortic BP is more important than peripheral BP,4, 5 and new terms such as aortic stiffness, pulse wave velocity, and pulse wave amplification have been defined in this area. Many factors, such as BP, age, sex, heart rate, and diabetes mellitus, can affect pulse wave amplification and aortic stiffness.6, 7 In contrast, a validation study population consists of healthy patients, current users of oscillometric devices, and patients with the aforementioned characteristics. For these reasons, it is reasonable to focus directly on the similarities and differences between oscillometric and central aortic BP measurements.
The aim of this study was to investigate the impact of central BP levels and sex on the difference between central and upper arm oscillometric BP values.
Methods
Patient Selection
A total of 675 patients undergoing routine cardiac catheterization were selected for this study. Patient consent was obtained before any measurements were made, and the project was approved by the local ethics committee. Three centers, located in eastern, western, and central regions of the country, were included in this study. The goal was to create a heterogeneous group that included patients from all 3 centers.
The exclusion criteria were an abnormal atrial or ventricular rhythm, a high degree of atrioventricular block, hemodynamic instability, acute coronary syndrome, cardiogenic shock, severe valvular heart disease, end‐stage renal artery disease, an arm circumference >38 cm or <20 cm, and a body mass index (BMI) >38 kg/m2 or <20 kg/m2.
Arterial BP Measurement
Intra‐arterial BP measurements were performed with a 6‐F pigtail catheter positioned in the ascending aorta and attached to a properly calibrated transducer and monitoring system. The transducer was kept at the same level as the BP cuff to avoid hydrostatic effects. Central BP was measured simultaneously at the upper arm peripheral area starting at deflation of the oscillometric device cuff. Means of 10 to 12 beats recorded from aortic measurements were calculated as the systolic BP (SBP) and diastolic BP (DBP). The paper processing rate of the central BP recording was adjusted to 25 m/s.
Indirect BP Measuring Device
An Omron M3 Intellisense device (HEM‐7051‐E; Omron Healthcare Europe B.V., Hoofddorp, the Netherlands) was used on the upper arm. Each measurement was taken twice and average values were calculated. All values were compared with aortic BP measurements. The cuff of the Omron M3 was positioned across the midportion of the right upper arm, with the bladder directly over the brachial artery and the lower edge 2.5 cm above the antecubital space.
Measurement Protocol
The patients were seated in a warm, quiet room and allowed to rest for at least 5 minutes prior to angiography. Demographic information (ie, age, height, weight, and sex) was recorded for each patient, as well as arm circumference, which was measured at the approximate midpoint of the upper arm. Initial readings were taken with the upper arm device. All BP measurements were made with the patient in a supine position, and each measurement was taken twice at intervals of >30 seconds to minimize venous congestion and at intervals of <2 minutes to limit variability in BP.
Statistical Analysis
Summary values are expressed as mean±standard deviation unless stated otherwise. Discrepancies between our oscillometric and intra‐arterial BP measurements were assessed using Bland‐Altman plots with the MedCalc packet program.8 An intraclass correlation coefficient was used to examine the repeatability of the oscillometric devices with the SPSS 13.0 packet program (SPSS, Inc, Chicago, IL). Differences among the 3 groups were evaluated by analysis of variance for parametric variables and a chi‐square test for categorical variables. Student t test was used to compare parametric data between groups. A two‐tailed P value <.05 was considered statistically significant.
Results
The 675 patients in this study were divided into 3 groups according to their aortic SBP. Those with an SBP <130 mm Hg were categorized as having low BP, those with an SBP between 130 mm Hg and 159.9 mm Hg as having a moderate BP level, and those with an SBP ≥160 mm Hg as having high BP. The patients' characteristics are listed in Table 1. Coronary artery disease (CAD) was apparent in approximately two thirds of the patients. Demographic features such as arm circumference, BMI, and frequency of CAD were similar at each SBP level.
Table 1.
Demographic Characteristics of the Patients According to BP Levels
| Low BP Level (n=291) | Medium BP Level (n=234) | High BP Level (n=150) | P Value | |
|---|---|---|---|---|
| Age, y | 59.1±11.6 | 61.0±11.3 | 64.3±8.8 a | .001 |
| Men/women | 199/92 | 141/93 | 75/75 a | .01 |
| Hypertension, No. (%) | 109 (37.5) | 149 (63.7) | 128 (85.3) a , b | .001 |
| Diabetes mellitus, No. (%) | 70 (24.1) | 58 (24.8) | 56 (37.3) a | .007 |
| Smoking, No. (%) | 109 (37.5) | 61 (26.1) | 30 (20.0) a | .001 |
| Body mass index | 27.8±4.4 | 28.2±4.2 | 28.7±4.5 | .89 |
| Arm circumference, cm | 28.5±3.27 | 28.7±2.8 | 28.6±3.1 | .18 |
| CAD, No. (%) | 191 (65.6) | 163 (69.7) | 92 (61.3) | .24 |
| Total cholesterol, mg/dL | 174.0±47.1 | 188.1±48.8 | 177.7±43.8 | .05 |
| LDL, mg/dL | 109.5±47.1 | 113.6±41.2 | 111.8±38.3 | .61 |
| HDL, mg/dL | 42.2±14.5 | 42.5±15.6 | 44.4±13.7 | .55 |
| Trigliseride, mg/dL | 180.2±47.4 | 133.8±93.1 | 185.7±325.8 | .06 |
| Blood urea, mg/dL | 37.9±16.1 | 36.7±20.0 | 40.1±19.2 | .44 |
| Creatinine, mg/dL | 0.9±0.26 | 1.1±0.8 | 1.2±1.0 a | .01 |
| Mean central SBP | 112.4±12.2 | 143.5±10.8 a | 174.2±13.8 a , b | .001 |
| Mean central DBP | 63.6±9.4 | 73.3±11.0 a | 83.1±13.6 a , b | .001 |
| Heart rate, beats per min | 72.2±10.5 | 75.4±12 | 76.1±13.7 | .26 |
Abbreviations: CAD, coronary artery disease; DBP, diastolic blood pressure; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; SBP, systolic blood pressure. aStatistical importance compared with low blood pressure (BP) level. bStatistical importance compared to medium BP level, P value statistical significance level by analysis of variance.
The upper arm oscillometric device underestimated SBP at high BP levels (Figure 1). The mean bias at this BP level was −3.8 mm Hg. In addition, the device overestimated DBP by about 7 mm Hg at each BP level. Bland‐Altman plots for the SBP and DBP values are shown in Figures 2 and 3, respectively.
Figure 1.
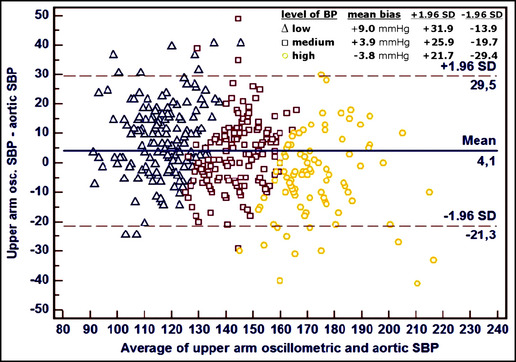
Bland‐Altmann plots of systolic blood pressure (BP) values illustrated according to BP levels obtained from upper arm oscillometric device. SD indicates standard deviation; SBP, systolic blood pressure.
Figure 2.
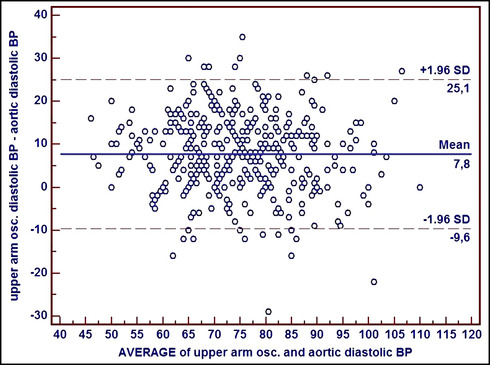
Bland‐Altman plots of diastolic blood pressure (BP) values were shown according to BP levels obtained from upper arm oscillometric device. SD indicates standard deviation.
Figure 3.
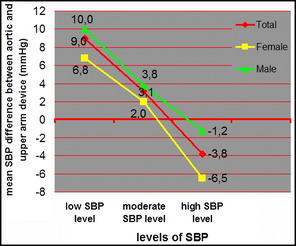
Mean systolic blood pressure (SBP) bias of upper arm device according to BP level and sex.
Some characteristics were different for women and men (Table 2). The effect of sex on differences in central and oscillometric BP according to BP level was also analyzed (Table 2). SBP was overestimated to a lesser degree in women than in men at low BP levels, but it was more highly underestimated in women than in men at high BP levels. There was no difference in SBP between women and men at an intermediate BP level using the upper arm oscillometric device. Differences in DBP between the upper arm and central measurements were also comparable in women and men at each BP level.
Table 2.
A Comparison of BP Measurements and Demographic Features in Men vs Women According to BP Levels
| Low BP Level | Medium BP Level | High BP Level | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Men (n=199) | Women (n=92) | P Value | Men (n=141) | Women (n=93) | P Value | Men (n=75) | Women (n=75) | P Value | |
| Age, y | 58.6±11.6 | 60.1±11.4 | .31 | 61.7±11.1 | 60.0±11.4 | .25 | 65.7±9.6 | 62.8±7.6 | .04 |
| Arm circumference, cm | 28.5±3.2 | 28.6±3.4 | .64 | 28.6±2.9 | 28.8±2.6 | .54 | 27.9±3.3 | 29.1±2.7 | .02 |
| Body mass index | 27.0±3.8 | 29.5±5.0 | .01 | 27.5±4.0 | 29.3±4.2 | .01 | 27.5±4.6 | 29.8±4.0 | .01 |
| Mean central SBP | 110.5±12.3 | 116.6±11.1 | .01 | 143.0±11.3 | 144.2±10.0 | .38 | 175.3±13.6 | 172.0±13.6 | .25 |
| Mean central DBP | 63.5±9.6 | 63.8±9.2 | .74 | 73.4±10.8 | 73.2±11.4 | .91 | 79.9±15.1 | 78.6±12.0 | .54 |
| SBP difference between upper arm and aorta | 10.0±12.2 | 6.8±10.2 | .02 | 3.8±11.6 | 2.0±11.6 | .24 | −1.2±12.3 | −6.4±13.2 | .01 |
| DBP difference between upper arm and aorta | 7.7±9.1 | 6.5±8.4 | .31 | 7.0±8.9 | 9.4±9.0 | .42 | 8.1±8.4 | 8.4±8.7 | .82 |
Abbreviations: BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure. P value statistical significance level by Student t test.
No correlation was found between BMI and SBP differences for the upper arm‐aortic measurements (r=0.03, P=.2). In addition, arm circumference was poorly correlated with SBP differences between the upper arm and aortic BP measurements (r=0.08, P=.03). DBP differences in the upper arm‐aortic BP values were weakly, negatively correlated with BMI (r=−0.10, P=.01) but not with arm circumference (r=0.2, P=.5).
The repeatability of the oscillometric measurements was analyzed according to BP level. The repeatability of the oscillometric measurements for each BP level is shown in Table 3.
Table 3.
Repeatability of Oscillometric Device for Each BP Level
| Low BP Level r (95% CI) | Medium BP Level r (95% CI) | High BP Level r (95% CI) | Total BP Level r (95% CI) | |
|---|---|---|---|---|
| 1 and 2 measurements of SBP with wrist device | 0.92 (0.89–0.93) | 0.90 (0.87–0.92) | 0.95 (0.93–0.96) | 0.97 (0.97–0.98) |
| 1 and 2 measurements of SBP with upper arm device | 0.93 (0.92–0.95) | 0.92 (0.90–0.94) | 0.91 (0.87–0.94) | 0.98 (0.97–0.98) |
| 1 and 2 measurements of DBP with wrist device | 0.94 (0.93–0.96) | 0.87 (0.83–0.90) | 0.96 (0.94–0.97) | 0.95 (0.94–0.96) |
| 1 and 2 measurements of DBP with upper arm device | 0.93 (0.91–0.95) | 0.96 (0.95–0.97) | 0.95 (0.93–0.96) | 0.96 (0.95–0.97) |
Abbreviations: BP, blood pressure; CI, confidence interval; DBP, diastolic blood pressure; SBP, systolic blood pressure; r, intraclass correlation coefficient (Cronbach's α).
Discussion
This is the first study to systematically assess the impact of central BP levels on oscillometric BP measurements. Our results indicate that the SBP measurements produced using an upper arm oscillometric device were closest to the central BP measurement for patients with high BP but overestimated in patients with low or moderate BP. In addition, the difference between central aortic SBP and oscillometric SBP was affected by sex. As for DBP, the upper arm oscillometric device overestimated the DBP at each BP level. Validation of the device was not undertaken in this study because the device was previously validated.9, 10
O'Brien and colleagues11 compared the accuracy of 3 ambulatory devices according to BP level and reported that all 3 oscillometric devices were less accurate in the high‐pressure range. Braam and colleagues2 classified their validation study results according to BP levels of 23 oscillometric BP‐measuring devices. However, they found differences in BP between oscillometric devices and a sphygmomanometer in 9 studies. The authors argued that BP‐measuring devices become less accurate as BP levels increase because of a combination of two factors: the sequential measurements used during validation studies and increasing BP variability at higher BP levels. Mancia and colleagues3 reported that absolute short‐term variability in BP was greater in hypertensive patients than in normotensive individuals. (Short‐term variability increased from 9.5 mm Hg to 12.2 mm Hg for SBP and from 6.1 mm Hg to 9.0 mm Hg for DBP.) In the present study, oscillometric BP measurements were simultaneously obtained together with aortic BP measurements; therefore, an increased difference in BP measurement cannot be attributed to BP variability at high BP level.
In hypertensive patients, it is known that little or no pulse wave amplification occurs and pulse pressure is expected to be similar at the aortic and brachial arterial levels.12 Whether the same holds true for normotensive patients with physiological pulse wave amplification (~15 mm Hg) remains to be established; however, the same is true for elderly patients.13 SBP amplification between the aorta and peripheral arteries decreases with age and heart rate and in accordance with BP level.14 Age did not correlate with differences in SBP between central and oscillometric measurements obtained using either a wrist or upper arm device. A possible explanation for this conflicting result is that the mean age of the study population was relatively low. In addition, the mean age of the patients with high BP was slightly greater than that of the other two groups. This is an expected result since age differences may contribute to the underestimation of BP at high BP levels via decreasing pulse wave amplification.
Weber and colleagues15 found that upper arm devices overestimated SBP by about 4 mm Hg and they found no correlation between mean BP and central‐peripheral measurement differences. Mean SBP values were not mentioned in their paper, but a Bland‐Altman plot revealed that the BP level was moderate. This result is comparable to that produced for patients with a moderate BP in the present study. In this group, mean BP was poorly correlated with differences in central‐peripheral measurement (r=0.2, P=.01). It was reported that oscillometric upper arm BP measurements underestimated SBP (by −7 to −10 mm Hg) in all groups and overestimated DBP.16 However, the mean SBP for each group was >150 mm Hg (150–159 mm Hg). In our study, upper arm devices underestimated the SBP at higher BP levels, but the same devices showed different characteristics at lower and moderate BP levels. Thus, the results of the present study may partially explain the conflicting measurements produced by upper arm oscillometric devices via comparison with central BP levels.
Another issue is the effect of patient characteristics on differences between central and peripheral BP measurements. In brief, it is accepted that BMI and arm circumference are the two main factors that affect the reliability of peripheral BP measurements,17 but the mean of the two parameters was similar for all BP levels in the present study. The difference between central and peripheral BP was poorly correlated with BMI. This poor correlation may be explained by the fact that we excluded patients with both a BMI >38 kg/m2 or <20 kg/m2 and an arm circumference of >38 cm or <20 cm.
Because of the greater number of women than men in this study, the effect of sex on oscillometric measurement was examined in a separate analysis. Sex affected the difference in SBP between the upper arm and aorta at both high and low BP levels. It is possible that the SBP was higher in women than in men (by about 6 mm Hg) at a low BP level. The arm circumference among women was similar to that among men at both low and moderate BP levels, but this situation did not occur at a high BP level. Increasing arm circumference in women may contribute to the underestimation of SBP with an upper arm device only at a high BP level, compared with men. Nevertheless, these factors do not completely explain the effect of sex on SBP differences. It is known that the augmentation index is about 7% higher in women than in men for those older than 55, and the level of estrogen may also affect central arterial pulse wave properties.18, 19 Thus, central wave reflection properties may be important in women for upper arm oscillometric measurements as well as in patients with other demographic characteristics.
Although the mean difference between peripheral and central BP changed significantly according to BP level, the repeatability of the measurements produced using an upper arm oscillometric device was relatively high at all BP levels. Thus, the degree of difference between peripheral and central BP did not affect the repeatability of our oscillometric measurements. For example, if an oscillometric device underestimates the central BP in a single individual, repeated measurement will be underestimated in the same person and vice versa. Because factors affecting the difference between central and oscillometric values were constant during the first and second oscillometric measurements, high repeatability was expected.
Study Limitations
An important limitation of this study is that all BP measurements were taken with the patients in a supine position; however, BP is frequently measured in a sitting position. It has been recommended that BP measurements be performed in both supine and sitting positions, although this matter is under discussion.20, 21 Second, only two types of upper arm oscillometric devices were used as a prototype of their groups in the present study. Thus, our results may not be applicable to all oscillometric devices. Third, our results are not comparable to those of a previous validation study because mercury sphygmomanometers were not used; however, it is important to note that the majority of patients in this study were actual cardiac patients, compared with the frequent use of healthy volunteers in validation studies. Many factors, such as age, CAD, diabetes mellitus, sex, and left ventricular dysfunction, which many oscillometric device users have in the real world, may have complex effects on aortic stiffness and on the difference in peripheral‐central BP. Fourth, an upper arm device with a large standard cuff (22×35 cm) was used in this study because only one type of cuff is commonly used for BP measurement in routine clinical practice. Moreover, some devices are manufactured with only one cuff size; however, we know that the use of an inappropriate cuff size can lead to systematic underestimation or overestimation of pressure when the ratio of bladder width to arm circumference is not 0.40.20 On the other hand, the British Hypertension Society has recommended the use of a single large cuff (12.5×35 cm) for all adults with an arm circumference up to 42 cm to avoid the need for multiple cuff sizes.21 For this reason, patients with a BMI >38 or <20 were excluded from the present study, as were patients with an arm circumference >38 cm. Fifth, pulse wave amplification and aortic stiffness were not measured in this study. The effects of these parameters on oscillometric BP measurements remain unclear.
Conclusions
The results of this study suggest that the difference between oscillometric upper arm BP and aortic BP was directly affected by the patient's central BP level. Another important factor was sex. Based on the results of this study, physicians should consider a patient's BP level and sex when predicting central aortic SBP following upper arm oscillometric measurement. An upper arm oscillometric device reflected the central aortic BP most accurately, especially for men with high BP. For this reason, upper arm oscillometric devices should be considered for self‐measurement by male patients with high BP. Despite technological advances, the values produced by oscillometric BP measurement differed from the central BP values by about ±20 mm Hg for most patients.
Acknowledgment and disclosure
Support of the study: All devices used for the study were taken from Turkey distributors of OMRON Healthcare Co., Ltd. There is no potential conflict of interest among the authors.
J Clin Hypertens (Greenwich). 2013;15:681–686. ©2013 Wiley Periodicals, Inc.24034662
References
- 1. O'Brien E, Atkins N, Mee F, O'Malley K. Comparative accuracy of six ambulatory devices according to blood pressure levels. J Hypertens. 1993;11:673–675. [DOI] [PubMed] [Google Scholar]
- 2. Braam LR, Thien T. Is the accuracy of blood pressure measuring devices underestimated at increasing blood pressure levels? Blood Press Monit. 2005;10:283–289. [DOI] [PubMed] [Google Scholar]
- 3. Mancia G, Ferrari A, Gregorini L, et al. Blood pressure and heart rate variabilities in normotensive and hypertensive human beings. Circ Res. 1983;53:96–104. [DOI] [PubMed] [Google Scholar]
- 4. The CAFE Investigators, for the Anglo‐Scandinavian Cardiac Outcomes Trial (ASCOT) Investigators . Differential impact of blood pressure‐lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) Study. Circulation. 2006;113:1213–1225. [DOI] [PubMed] [Google Scholar]
- 5. Nishijima T, Nakayama Y, Tsumura K, et al. Pulsatility of ascending aortic blood pressure waveform is associated with an increased risk of coronary heart disease. Am J Hypertens. 2001;14:469–473. [DOI] [PubMed] [Google Scholar]
- 6. Bulpitt CJ, Cameron JD, Rajkumar C, et al. The effect of age on vascular compliance in man. Which are the appropriate measures? J Hum Hypertens. 1999;13:753–758. [DOI] [PubMed] [Google Scholar]
- 7. Mitchell GF, Parise H, Benjamin EJ, et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham heart study. Hypertension. 2004;43:1239–1245. [DOI] [PubMed] [Google Scholar]
- 8. Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346:1085–1087. [DOI] [PubMed] [Google Scholar]
- 9. Topouchian J, El Feghali R, El Assaad H, et al. Validation of the Omron HEM‐7051‐E device for blood pressure measurement according to the international validation protocol. J Hypertens. 2006;24:S278. [Google Scholar]
- 10. Altunkan S, Oztaş K, Altunkan E. Validation of the Omron 637‐IT wrist blood pressure measuring device with a position sensor according to the international protocol in adults and obese adults. Blood Press Monit. 2006;11:79–85. [DOI] [PubMed] [Google Scholar]
- 11. O'Brien E, Mee F, Atkins N, Thomas M. Evaluation of three devices for self measurement according to the revised British Hypertension Society Protocol: the Omron HEM‐705CP, Philips HP5332, and Nissei DS‐175. Blood Press Monit. 1996;1:55–61. [PubMed] [Google Scholar]
- 12. Nichols WW, O'Rourke MF. McDonald's Blood Flow in Arteries: Theoretical, Experimental and Clinical Principles, 5th ed. London: Edward Arnold; 2005. [Google Scholar]
- 13. Chemla D, Brahimi M, Nitenberg A. Thumb‐rule for the proper assessment of mean blood pressure at the brachial artery level: what should be changed? J Hypertens. 2007;25:1740–1741. [DOI] [PubMed] [Google Scholar]
- 14. Westerhof BE, Guelen I, Stok WJ, et al. Arterial pressure transfer characteristics: effects of travel time. Am J Physiol Heart Circ Physiol. 2007;292:H800–H807. [DOI] [PubMed] [Google Scholar]
- 15. Weber F, Lindemann M, Erbel R, Philipp T. Indirect and direct simultaneous, comparative blood pressure measurements with the Bosotron 2 device. Kidney Blood Press Res. 1999;22:166–171. [DOI] [PubMed] [Google Scholar]
- 16. Umana E, Ahmed W, Fraley MA, Alpert MA. Comparison of oscillometric and intraarterial systolic and diastolic blood pressures in lean, overweight, and obese patients. Angiology. 2006;57:41–45. [DOI] [PubMed] [Google Scholar]
- 17. Pierin AM, Alavarce DC, Gusmão JL, Halpern A, Mion D Jr. Blood pressure measurement in obese patients: comparison between upper arm and forearm measurements. Blood Press Monit. 2004;9:101–105. [DOI] [PubMed] [Google Scholar]
- 18. McGrath BP, Liang YL, Teede H, et al. Age‐related deterioration in arterial structure and function in postmenopausal women: impact of hormone replacement therapy. Arterioscler Thromb Vasc Biol. 1998;18:1149–1156. [DOI] [PubMed] [Google Scholar]
- 19. Rajkumar C, Kingwell BA, Cameron JD, et al. Hormonal therapy increases arterial compliance in postmenopausal women. J Am Coll Cardiol. 1997;30:350–356. [DOI] [PubMed] [Google Scholar]
- 20. Perloff D, Grim C, Flack J, et al. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–2470. [DOI] [PubMed] [Google Scholar]
- 21. Petrie JC, O'Brien ET, Littler WA, de Swiet M. Recommendations on blood pressure measurement. Br Med J (Clin Res Ed). 1986;293:611–615. [DOI] [PMC free article] [PubMed] [Google Scholar]


