Abstract
Study Objectives:
We evaluated factors associated with the presence of sleep disturbance in patients with stroke and whether sleep disturbance predicted change in other patient-reported domains of health over time.
Methods:
Observational cohort study of 2,190 patients with stroke seen in a cerebrovascular clinic February 17, 2015 to July 5, 2017 who completed patient-reported outcome measures (PROMs) at ≥ 1 visit, including the Patient Health Questionnaire-9 depression screen, Quality of Life in Neurological Disorders (NeuroQoL) cognitive function and Patient-Reported Outcomes Information Measurement System (PROMIS) sleep disturbance, fatigue, anxiety, social role satisfaction, physical function, and pain interference. Separate multivariable models were constructed with PROMIS sleep disturbance as the dependent variable. Covariates included clinical and demographic variables, the Patient Health Questionnaire-9 depression screen scored on the PROMIS metric, and 1 of the 6 other PROMs. Among the 476 patients with ≥ 2 visits, linear regression models were constructed to determine the association of baseline sleep disturbance with follow-up PROMs after adjustment for the corresponding baseline PROMIS/NeuroQol scores, depression score, and clinical variables.
Results:
Younger age and all PROM scores were associated with sleep disturbance; depression had the greatest association among PROMs (beta estimate 0.53, 95% confidence interval, 0.49, 0.57), physical function had the least (−0.06, 95% confidence interval, −0.11, −0.01). Baseline PROMIS sleep disturbance score was associated with worse adjusted follow-up scores for depression, fatigue, social role satisfaction, and physical function.
Conclusions:
Younger age and all 8 PROMs were associated with sleep disturbance in patients with stroke. The degree of sleep disturbance predicted future patient-reported outcomes for multiple domains of health. Further study is warranted to determine if interventions shown to improve sleep symptoms will also improve other outcomes.
Citation:
Katzan IL, Thompson NR, Walia HK, Moul DE, Foldvary-Schaefer N. Sleep disturbance predicts future health status after stroke. J Clin Sleep Med. 2020;16(11):1863–1870.
Keywords: patient-reported outcomes, stroke, sleep
BRIEF SUMMARY
Current Knowledge/Study Rationale: Sleep disturbance is frequent after stroke and effective treatments are available. Understanding the factors associated with sleep disturbance and the role of sleep on outcomes after stroke will help frame the importance of identifying and managing treatable sleep-related conditions in survivors of stroke.
Study Impact: The degree of sleep disturbance independently predicted future physical function, satisfaction with social roles, depression, and fatigue. These findings raise the possibility that the interventions that improve sleep disturbance may have an impact on multiple aspects of patient-perceived health.
INTRODUCTION
Clinically relevant sleep symptoms occur in over a quarter of patients after stroke.1 Poststroke sleep disorders includes sleep-disordered breathing, which occurs in over 50% of survivors of stroke2; insomnia and hypersomnia, occurring in 20–40% of patients with stroke3,4; restless legs syndrome,5,6 occurring in 10–15% of stroke survivors; as well as circadian rhythm sleep disturbances and parasomnias. Symptom-based treatments are available,7 yet sleep disturbance after stroke is still underappreciated in clinical practice and commonly ignored.8,9 Given its prevalence and treatability, it is important to understand the factors associated with sleep disturbance, which may help identify the patients who would most benefit from assessment of sleep symptoms and improve our understanding the mechanisms of sleep disturbance after stroke.
Furthermore, role of sleep on outcomes after stroke has become a pressing issue.7,9,10 Most studies have consisted of cross-sectional designs and have not include patient-reported outcomes.11,12 Therefore, the objectives of our study were to (1) evaluate factors associated with the presence of sleep disturbance in stroke patients and (2) determine the role of patient-reported sleep disturbance in future patient-reported domains of health in patients with stroke.
METHODS
We performed a retrospective cohort study of patients with ischemic stroke, transient ischemic attack (TIA), intracerebral hemorrhage (ICH), or subarachnoid hemorrhage (SAH) seen in the ambulatory Cerebrovascular Clinic from February 17, 2015 to July 5, 2017. As previously described,13 patients with cerebrovascular diseases routinely completed patient-reported outcome measures (PROMs) using the Knowledge Program data collection system either on electronic tablets at the time of their ambulatory visit or through the electronic health record patient portal (MyChart, Epic Systems) before their appointment. Clinicians completed the National Institutes of Health Stroke Scale (NIHSS) and modified Rankin Scale (mRS) during each visit and recorded the date of the last cerebrovascular event. The NIHSS consists of 15 items and is a standard scale for measuring for neurologic impairment.14 The mRS is a one-item scale of global disability commonly used in clinical stroke trials.15 Inclusion criteria for this cohort study included age > 18 years old, completion of Patient-Reported Outcomes Information Measurement System (PROMIS) sleep disturbance scale at 1 or more ambulatory visits during the study period, and clinical diagnosis of ischemic stroke, ICH, SAH, or TIA.
Patient-reported outcome measures
The computer adaptive testing versions of the Quality of Life in Neurological Disorders (NeuroQoL) cognitive function v1.0 scale16 and the following 6 PROMIS v1.0 scales17 were completed by patients: sleep disturbance, physical function, satisfaction with social roles, pain interference, fatigue, and anxiety. These scales have been validated for use in wide range of diseases and symptoms.16,17 The PROMIS sleep disturbance scale is comprised of questions regarding perceived sleep quality and difficulty falling asleep and staying asleep. With computer adaptive testing, the most informative questions are selected from an item bank of questions based on the patient’s prior responses. Scores of PROMIS and NeuroQoL tools are standardized to the general United States adult population on the T-scale with mean of 50 and standard deviation of 10. Higher PROMIS score always represents more of the concept being measured. For negatively worded concepts: sleep disturbance, pain interference, fatigue, and anxiety, higher scores indicated worse health status. For positively worded concepts: physical function, cognitive function, and satisfaction with social roles, higher scores indicate better health status.
The Patient Health Questionnaire-9 (PHQ-9), the depression screen used at our institution, was also collected. The PHQ-9 item responses were cross-linked along the PROMIS metric, providing a PROMIS depression score that was equivalent to the PHQ-9 scores.18 This cross-linkage allowed us to assess the severity of depressive symptoms along the same standardized scale as the other PRO measures in this study.
Additional demographic and visit-based information in the data set was obtained from the electronic health record. Approximate household income was estimated using the ZIP code based on 2010 census data.
Statistical analysis
Patient and clinical characteristics at baseline were summarized using descriptive statistics for patients included and excluded from the study.
Association of demographic and clinical factors with PROMIS Sleep Disturbance score (objective 1)
To evaluate the association of demographic and clinical factors with PROMIS sleep disturbance score, correlations were calculated between PROMIS sleep disturbance and other PROM scores using Pearson correlation coefficients. Separate multivariable linear regression models were then created with the PROMIS sleep disturbance score as the dependent variable. Each model included the PHQ-9 depression scale scored on the PROMIS metric and 1 of the 6 other PROMs collected in this study: NeuroQoL cognitive function, PROMIS fatigue, satisfaction with social roles, physical function, and pain interference. Depression was included in each model because of its known correlation with sleep disturbance and the potential impact of depression on patient’s perceptions of their health in other domains. Only depression and 1 other PROM were included in each model to avoid collinearity issues that would have arisen from the inclusion of multiple PROMs together. Additional covariates included: age (years), sex, race (White, Black, other), marital status (married, single, other), disability status (mRS categorized as 0–1, 2–3, 4–5), time from stroke (0–90, 91–365, > 365 days), and estimated median household income based on ZIP code. Median income was derived based on 2010 United States Census data. Because patient perceptions at different time points may differ by level of disability, an interaction term was included between mRS and time from stroke in each model. These models were replicated in each stroke subtype (ischemic stroke, TIA, ICH, SAH).
Determine the role of patient-reported sleep disturbance in future patient-reported health domains (objective 2)
To determine the role of patient-reported sleep disturbance in future patient-reported domains of health, separate multivariable linear regression models were created. The dependent variable was the follow-up score for NeuroQoL cognitive function and each of the following PROMIS domains: physical function, satisfaction with social roles, depression, anxiety, fatigue, and pain interference. The independent variable for each model was the PROMIS sleep disturbance score. To adjust for baseline status, the score of the baseline domain score was included (eg, for PROMIS physical function, the baseline PROMIS physical function score was included as a covariate). The multivariable models were further adjusted for the following covariates: PHQ-9 score on PROMIS metric, age (years), sex, race (White, Black, other), marital status (married, single, other), disability status (mRS 0–1, 2–3, 4–5), time from stroke (0–90, 91–365, > 365 days), estimated median household income based on ZIP code, and interval (days) between PROM scores.
The relationship between baseline sleep disturbance and follow-up PROMIS T-scores based on the multivariable models was displayed graphically for all domains where sleep disturbance was a significant predictor.
Sensitivity analysis to evaluate the effect of removing the sleep item in the PHQ-9 depression screen
The validated PHQ-9 screen includes the question “Trouble falling or staying asleep, or sleeping too much”. Because inclusion of this item in the PHQ-9 score could conceivably affect the relationship between PROMIS sleep disturbance and PROMIS tools in multivariable models that included the PHQ-9, the multivariable models were recomputed after replacing the PHQ-9 score with a “PHQ-8” score that did not contain the question regarding sleep.
All computations were done in R, version 3.4.1. All tests were 2-sided, and P values < 0.05 were considered statistically significant. We adjusted for multiple testing using Holm’s method. Missing data were handled with multiple imputation using the mice package, version 2.30 in R. The study was approved by the Cleveland Clinic Institutional Review Board. Requirement for informed consent was waived.
RESULTS
During the study period, 2,190 patients with ischemic stroke, TIA, ICH, or SAH completed the PROMIS sleep disturbance scale on at least 1 visit and were included in the study cohort. The majority of patients in the study cohort had ischemic stroke and completed their first PROMs during the study period a median of 67 days from stroke. Median mRS of the study cohort was one indicating mild disability (Table 1). Patient data were completed by caregiver proxies in 23.6% of first visits in the cohort, ranging from 8.6% in patients with mRS = 0 (no symptoms) to 82.2% in patients with mRS = 4–5 (severe disability). Compared to patients who did not complete PROMIS sleep disturbance at their visit and were therefore excluded, cohort patients were more likely to be white, married, lived in wealthier zip codes, and had higher diastolic blood pressure, and more time elapse since their stroke. They were also less likely to have one of several comorbid conditions and had better NIHSS and modified Rankin scale scores (Table S1 in the supplemental material).
Table 1.
Characteristics of the study cohort, stratified by stroke type.
| All Patients | Ischemic Stroke | Transient Ischemic Attack | Intracerebral Hemorrhage | Subarachnoid Hemorrhage | P Value | |
|---|---|---|---|---|---|---|
| n | 2,190 | 1,396 | 380 | 210 | 204 | |
| Age, mean (SD) | 60.7 (14.8) | 60.5 (14.9) | 64.6 (13.6) | 57.7 (16.5) | 57.5 (12.4) | < .001 |
| Female | 1,083 (49.5%) | 627 (44.9%) | 208 (54.7%) | 116 (55.2%) | 132 (64.7%) | < .001 |
| Race | ||||||
| White | 1,737 (79.3%) | 1,095 (78.4%) | 320 (84.2%) | 164 (78.1%) | 158 (77.5%) | .440 |
| Black | 336 (15.3%) | 221 (15.8%) | 46 (12.1%) | 32 (15.2%) | 37 (18.1%) | |
| Other | 34 (1.6%) | 19 (1.4%) | 7 (1.8%) | 4 (1.9%) | 4 (2.0%) | |
| Missing | 83 (3.8%) | 61 (4.4%) | 7 (1.8%) | 10 (4.8%) | 5 (2.5%) | |
| Marital Status | ||||||
| Married | 1,346 (61.5%) | 849 (60.8%) | 255 (67.1%) | 122 (58.1%) | 120 (58.8%) | .021 |
| Nonmarried | 764 (34.9%) | 492 (35.3%) | 119 (31.3%) | 76 (36.2%) | 77 (37.8%) | |
| Missing | 80 (3.7%) | 55 (3.9%) | 6 (1.6%) | 12 (5.7%) | 7 (3.4%) | |
| Median income by ZIP code (× $1,000), mean (SD) | 52.7 (17.9) | 52.9 (18.2) | 53.6 (18.2) | 51.5 (15.8) | 50.9 (16.8) | .271 |
| BMI (kg/m2), median (IQR) | 28 (24, 32) | 28 (24, 32) | 28 (25, 33) | 26 (23, 32) | 27 (24, 31) | .042 |
| Cancer | 459 (21.0%) | 270 (19.3%) | 122 (32.1%) | 35 (16.7%) | 32 (15.7%) | < .001 |
| Chronic renal failure | 145 (6.6%) | 96 (6.9%) | 26 (6.8%) | 10 (4.8%) | 13 (6.4%) | .712 |
| Diabetes | 500 (22.8%) | 341 (24.4%) | 102 (26.8%) | 31 (14.8%) | 26 (12.7%) | < .001 |
| Depression | 318 (14.5%) | 192 (13.8%) | 59 (15.5%) | 34 (16.2%) | 33 (16.2%) | .595 |
| Coronary artery disease | 320 (14.6%) | 213 (15.3%) | 72 (18.9%) | 22 (10.5%) | 13 (6.4%) | < .001 |
| Hypertension | 1,030 (47.0%) | 637 (45.6%) | 203 (53.4%) | 101 (48.1%) | 89 (43.6%) | .039 |
| Active antidepressant(s) prescription | 529 (24.2%) | 320 (22.9%) | 105 (27.6%) | 48 (22.9%) | 56 (27.5%) | .167 |
| Days since stroke, median (IQR) | 67 (32, 388.5) | 64 (32, 319) | 56 (21, 278) | 69 (39, 423) | 360 (51, 1060) | < .001 |
| NIHSS score, median (IQR) | 0 (0, 1) | 0 (0, 1) | 0 (0, 0) | 0 (0, 2) | 0 (0, 0) | < .001 |
| Modified Rankin Scale Score | ||||||
| 0 | 617 (28.2%) | 329 (23.6%) | 208 (54.7%) | 32 (15.2%) | 48 (23.5%) | < .001 |
| 1 | 695 (31.7%) | 477 (34.2%) | 94 (24.7%) | 62 (29.5%) | 62 (30.4%) | |
| 2 | 410 (18.7%) | 296 (21.2%) | 29 (7.6%) | 52 (24.8%) | 33 (16.2%) | |
| 3 | 201 (9.2%) | 143 (10.2%) | 9 (2.4%) | 34 (16.2%) | 15 (7.4%) | |
| 4 | 70 (3.2%) | 50 (3.6%) | 1 (0.3%) | 14 (6.7%) | 5 (2.5%) | |
| 5 | 11 (0.5%) | 6 (0.4%) | 0 (0.0%) | 4 (1.9%) | 1 (0.5%) | |
| Missing | 186 (8.5%) | 95 (6.8%) | 39 (10.3%) | 12 (5.7%) | 40 (19.6%) | |
| PROMIS Sleep Disturbance Score, mean (SD) | 49.9 (10.4) | 49.4 (10.5) | 51.0 (10.0) | 49.9 (9.9) | 51.3 (11.3) | .025 |
| PHQ-9 on PROMIS metric, mean (SD) | 49.9 (10.7) | 50.0 (10.9) | 49.0 (10.2) | 51.1 (10.8) | 50.3 (10.7) | .190 |
| PROMIS Physical Function* Score, mean (SD) | 41.5 (10.5) | 41.3 (10.6) | 43.5 (9.3) | 39.2 (11.2) | 41.6 (11.2) | < .001 |
| PROMIS Fatigue Score, mean (SD) | 53.4 (10.5) | 53.5 (10.5) | 52.5 (10.6) | 54.3 (10.0) | 53.5 (11.2) | .266 |
| PROMIS Anxiety Score, mean (SD) | 52.9 (10.1) | 52.6 (10.0) | 52.8 (9.6) | 53.9 (10.4) | 53.8 (10.7) | .264 |
| PROMIS Pain Interference Score, mean (SD) | 52.7 (10.7) | 52.4 (10.8) | 52.9 (10.2) | 52.8 (10.6) | 54.4 (10.7) | .128 |
| PROMIS Social Roles* Score, mean (SD) | 44.9 (11.2) | 44.6 (11.2) | 46.8 (11.0) | 43.0 (10.7) | 45.4 (11.7) | .001 |
| NeuroQoL Cognitive Function* Score, mean (SD) | 46.5 (10.3) | 46.5 (10.2) | 48.3 (9.2) | 44.0 (10.7) | 45.7 (12.1) | .009 |
*Higher scores indicate better functioning. BMI = body mass index, IQR = interquartile range; mRS = modified Rankin Scale; NeuroQoL = Quality of Life in Neurological Disorders; PHQ-9 = Patient Health Questionnaire 9 depression screen; PROMIS = Patient-Reported Outcome Measurement Information System; SD = standard deviation.
There were 476 patients in the study cohort who completed PROMs on 2 or more visits. These patients were more likely to be white, had less time elapse since their stroke, and had worse mRS scores than cohort patients who had a single completion of PROMs during the study period (Table S2).
Association of demographic and clinical factors with PROMIS Sleep Disturbance score (objective 1)
Correlations between PROMIS sleep disturbance was highest for depression (r = .57; 95% CI 0.50, 0.63) and lowest for PROMIS physical function (r = −.23; 95% CI −0.32, −0.15) (Table 2). Table S3 displays the results of the separate multivariate models examining the factors associated with PROMIS Sleep Disturbance score for the full cohort. The interaction between mRS and time since stroke was not statistically significant, so it was excluded from further analyses. In all models, older age and mRS score 4–5 was associated with less sleep disturbance compared to mRS score 0–1. More depression (PHQ-9 on the PROMIS metric) was consistently associated with more sleep disturbance. Finally, for each model, worse scores on the corresponding PROMIS scale were associated with worse sleep disturbance. Depression had the greatest association with sleep disturbance, with beta estimates ranging from 0.37 to 0.53 depending on what other PROM was included as a covariate in the model. PROMIS physical function had the least association with PROMIS sleep disturbance with beta estimate −0.06 (95% CI −0.11 to −0.01) after adjustment for depressive symptoms and other clinical and demographic variables.
Table 2.
Pearson correlations between baseline PROMIS Sleep Disturbance and other baseline PROMIS/NeuroQoL scores.
| PROMIS/NeuroQoL Scores | r (95% CI) |
|---|---|
| PHQ-9 on PROMIS metric | .57 (0.50, 0.63) |
| PROMIS physical function | −.23 (−0.32, −0.15) |
| PROMIS fatigue | .50 (0.43, 0.57) |
| PROMIS anxiety | .51 (0.44, 0.58) |
| PROMIS pain Interference | .51 (0.44, 0.57) |
| PROMIS social role satisfaction | −.37 (−0.44, −0.28) |
| NeuroQoL cognitive function | −.41 (−0.52, −0.29) |
n = 2,190 patients. NeuroQoL = Quality of Life in Neurological Disorders; PHQ-9 = Patient Health Questionnaire 9 depression screen; PROMIS = Patient-Reported Outcome Measurement Information System.
These models were performed separately for ischemic stroke, TIA, ICH, and SAH subgroups (data not shown). Depression, pain interference, and fatigue were associated with sleep disturbance in all stroke types. Cognitive function and anxiety was associated with sleep disturbance in all stroke types except SAH. Satisfaction with social roles was associated with sleep disturbance in all stroke subtypes except ICH. Physical function was associated with sleep disturbance in the TIA subgroup only. Younger age was associated with worse sleep disturbance in ischemic stroke and TIA patients. Among patients with ICH, men had more sleep disturbance than women after adjustment for depressive symptoms and other clinical and demographic variables.
Determine the role of patient-reported sleep disturbance in future patient-reported health domains (objective 2)
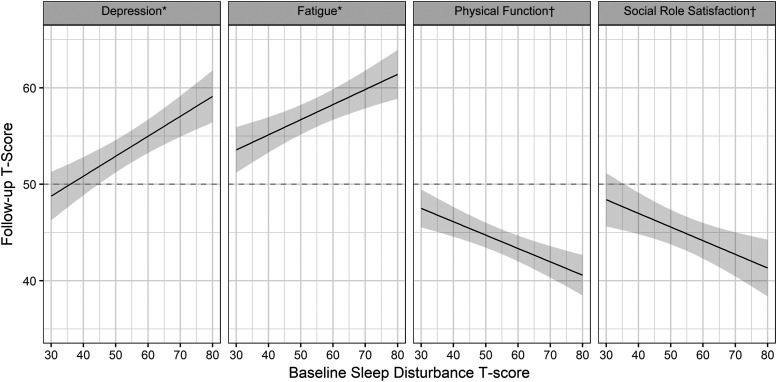
In multivariable models, worse baseline PROMIS sleep disturbance score was associated with worse follow-up scores for depression, fatigue, social role satisfaction, and physical function after adjustment for each scale’s baseline score, the baseline depression score, and additional clinical variables (Table 3, Figure 1).
Table 3.
Effect of baseline PROMIS sleep disturbance score on follow-up PROMIS and NeuroQoL domain scores in multivariable models.
| Dependent Variable | Estimate of PROMIS Sleep Disturbance (95% Confidence Interval) | Holm-Adjusted P Value |
|---|---|---|
| PHQ-9 on PROMIS Metric (n = 428) | 0.21 (0.13, 0.29) | < .001 |
| PROMIS Physical Function (n = 468)* | −0.14 (−0.20, -0.07) | < .001 |
| PROMIS Fatigue (n = 459) | 0.16 (0.08, 0.23) | < .001 |
| PROMIS Anxiety (n = 455) | 0.10 (0.01, 0.18) | .064 |
| PROMIS Pain Interference (n = 438) | 0.06 (−0.02, 0.14) | .275 |
| PROMIS Satisfaction with Social Roles (n = 431)* | −0.14 (−0.23, −0.05) | .010 |
| NeuroQol Cognitive Function (n = 332)* | −0.05 (−0.15, 0.06) | .352 |
In each model, the dependent variable is the follow-up PROMIS/NeuroQol domain score, and the independent variable is the baseline PROMIS sleep disturbance score. Covariate includes corresponding baseline PROMIS/NeuroQoL score and the variables: baseline PHQ-9 on PROMIS Metric, age, sex, race, marital status, median income by ZIP code, baseline modified Rankin Scale score, time since stroke, and interval between PROM measurements. *Higher scores indicate better functioning. NeuroQoL = Quality of Life in Neurological Disorders; PHQ-9 = Patient Health Questionnaire 9 depression screen; PROMIS = Patient-Reported Outcome Measurement Information System. Statistically significant beta coefficients appear in bold font (P < .05).
Figure 1. Relationship between baseline sleep disturbance and follow-up patient-reported outcomes.
Follow-up PROMIS T-score based on the multivariable models using median values for continuous covariates, reference categories for categorical covariates, and values one standard deviation worse than average of the general population for baseline PROMIS scores. *Higher scores indicate worse outcomes; †higher scores indicate better outcomes. PROMIS = Patient-Reported Outcomes Information Measurement System.
Sensitivity analysis to evaluate the effect of removing the sleep item in the PHQ-9 depression screen
The relationships between clinical variables, PROMIS scale score, and PROMIS sleep disturbance as outlined in Table 3 were similar after repeating the analyses removing the sleep item from the PHQ depression screen (data not shown). The estimates for baseline PROMIS sleep disturbance score in the prediction of future PROMIS scores were also quite similar (Table S4). The association between baseline PROMIS sleep disturbance and follow-up PROMIS anxiety score reached significance: the beta estimate of PROMIS sleep disturbance in model that includes PHQ-9 score was 0.10 (95% CI, 0.01–0.18, P = .064), beta estimate in model that includes PHQ-8 (sleep item removed) was 0.11 (95% CI, 0.03–0.19, P = .016).
DISCUSSION
In this large study of sleep disturbance in patients with stroke, all measured patient-reported domains of health—depression, anxiety, fatigue, pain interference, physical function, cognitive function, and satisfaction with social roles—were associated with sleep disturbance symptoms. Importantly, the degree of sleep disturbance independently predicted future physical function, satisfaction with social roles, depression, and fatigue.
Depressive symptoms, which were measured by the PHQ-9 scale cocalibrated to the PROMIS metric, had the strongest association of all patient-reported domains of health assessed in this study. This is not surprising given the known association between depression and sleep disturbance. Indeed, sleep disturbance is a criterion in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, manual for diagnosis of major depression.19 The association between sleep disturbance in stroke and pain interference, fatigue, and anxiety found in our study have also been previously described.3,20–22 The adjustment for depression in multivariable models in our study provides additional supportive evidence for the independent relationship of sleep disturbance to these domains of health. Although data on the relationship between sleep disturbance and self-reported cognitive function in patients with stroke are sparse, there is strong evidence of a relationship between sleep deprivation and cognitive performance on formal testing in the general population.23 In addition, patients with stroke and poor sleep quality have worse performance on objective measures of cognition compared with controls without stroke with poor sleep quality.24 Similarly, data on the association of sleep disturbance and patient-reported physical function in patients with stroke are limited, but there are substantial data on the association between clinician-reported functional status and sleep disturbance in patients with stroke.25 It is notable, therefore, that patients with greater clinician-reported disability in our cohort (defined as mRS 4–5) had less sleep disturbance. A likely explanation for this finding is the higher proportion of proxy completions of patient-reported scales in patients with mRS 3–5; caregiver proxies may not fully appreciate patients’ sleep symptoms.26
Other than mRS score, younger age was the only other clinical or demographic factor independently associated with sleep disturbance after adjustment for patient-reported scales. Other studies have report an association with increased age and insomnia in patients poststroke27,28. The discrepancies may be due lack of adjustment for depression in these other studies or differences in the specific construct measured (sleep disturbance vs insomnia). Prior reports have suggested that sleep disturbance may be more profoundly felt by stroke survivors who are poor or are part of a minority group.10 Our analysis did not confirm this relationship, although this hypothesis may merit more focused study.
An important finding in our study was that the degree of sleep disturbance predicted future physical function, satisfaction with social roles, depression, and fatigue in patients with stroke. Sleep disturbance often co-occurs with other symptoms such as depression13 and pain, and the relationships between sleep disturbance and many of these domains are most likely bidirectional.29 Pain, for instance, can lead to reduced sleep quality, which in turn could exacerbate the perception of pain.30,31 Overall, the findings that sleep disturbance is associated with worse patient-reported scores for multiple domains of health after adjustment for depressive symptoms and other clinical factors suggests that sleep symptoms impact future patient-reported health after stroke. For every 5 points in PROMIS sleep disturbance scale, scores on other domains worsen by 1–2 points. Although these score differences are modest, the uniform association between sleep symptom severity and all future domain scores suggests a meaningful difference exists.
There are limited data on the effect of sleep symptoms on outcomes after stroke. Sleep-disordered breathing in patients with stroke has been associated with worse outcomes,32 although sleep symptoms are often not apparent in patients with stroke who have sleep-disordered breathing,33,34 and PROMIS sleep disturbance does not detect patients with stroke with high probability of sleep apnea.1 A recently completed prospective study of 368 patients with stroke found that patients with insomnia had greater disability and lower likelihood of return to work at 12 months.12 However, insomnia was not associated with anxiety or depression after adjustment for baseline anxiety and depression scores.12 A study of 208 patients with stroke demonstrated that, among patients with moderate to severe stroke, self-reported sleep disturbance was associated with worse performance on Berg Balance Test at 3 months after adjustment for baseline Berg Balance score, depression, and demographic variables.35 Another study of 214 patients with stroke in acute rehabilitation evaluated the relationship between insomnia and the individual items of the Short Form 8 (SF-8) 1 month after stroke after adjustment for NIHSS, stroke subtype, depression, and hypnotics use.28 The authors found significant associations between insomnia and physical and mental health summary scores. The small sample size and study design precluded the ability to adjust for baseline patient-reported health. These authors and others7,9 suggested that further study is needed to examine the effect of sleep disturbance on outcomes after stroke.
Our study findings have potentially important clinical implications. Effective treatments are available to improve sleep symptoms,7 which include medications,36,37 sleep hygiene,38 cognitive behavioral therapy,39 and acupuncture40 depending on the sleep disorder.2 Findings from this study raise the possibility that the treatment of sleep symptoms, in addition to interventions targeted at other symptoms stroke patients may experience such as depression or pain, could provide an incremental benefit for these symptoms in patients with stroke. Proof of concept has been demonstrated in patients with pain syndromes whose perception of pain improved with restorative sleep.41 Improved sleep has also been shown to improve functional status in patients with fibromyalgia,42 and treatment of sleep apnea with positive airway pressure has been associated with improved neurological outcomes after stroke in some studies.43 Further study is warranted to determine if interventions shown to improve sleep symptoms will improve outcomes in other domains of health in patients with stroke.2,7,44 In addition, given the bidirectional relationships between sleep symptoms and emotional domains of health, it is conceivable that early psychological intervention could reduce the likelihood of sustained sleep difficulties in the chronic phase of stroke as suggested by Sterr and colleagues.45 Because our study was confined to patients with stroke, the findings and implications are limited to this population, although it is conceivable that the relationships between sleep symptoms and future self-reported outcomes and the potential for intervention are similar in other populations.
This study has several limitations. Because stroke patients with sleep apnea often do not experience the same degree of sleepiness as nonstroke patients46 and PROMIS sleep disturbance scale has minimal correlation with probability of having sleep-disordered breathing,1 our study did not meaningfully evaluate the effect of this highly prevalent sleep disorder on outcomes. This may have resulted in residual confounding. In addition, the PHQ-9 depression screen includes a question on sleep disturbance, so inclusion of the PHQ-9 in multivariable models could have reduced the effect of sleep disturbance on outcomes. However, multivariable models repeated after removing the sleep item from the PHQ depression screen demonstrated similar estimates of PROMIS sleep disturbance on follow-up PROMIS scales. Our study cohort consisted of patients with mild stroke seen in an ambulatory clinic at a single institution who completed PROMs at least once during the study period. This likely introduced a selection bias. However, as suggested by our study results, proxy completions, more common in patients with severe stroke, may not be an accurate reflection of sleep disturbance in patients with significant disability. Additional evaluation of patients in additional populations should be done to confirm our findings. Finally, we did not assess for the presence of sleep disturbance before the stroke events and so were unable to determine if patients’ sleep disturbance was pre-existing or new onset after stroke.
CONCLUSIONS
Sleep disturbance contributes to reduced future health-related quality of life and emotional health. Identification of patients with sleep disturbance can help identify patients who are at increased risk for worse outcomes after adjustment for baseline health status. Interventions that improve sleep disturbance may have an impact on multiple aspects of patient-perceived health.
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. The authors report no conflicts of interest.
SUPPLEMENTARY MATERIAL
ABBREVIATIONS
- ICH
intracerebral hemorrhage
- mRS
modified Rankin Scale; clinician-reported measure of global disability
- NeuroQoL
Quality of Life in Neurological Disorders; a suite of patient-reported outcome measures
- NIHSS
National Institutes of Health Stroke Scale; a clinician-reported measure of severity of neurological impairment after stroke
- PHQ-8
Patient Health Questionnaire-9 depression screen with sleep item removed
- PHQ-9
Patient Health Questionnaire-9 depression screen
- PROMs
patient-reported outcome measures
- PROMIS
Patient-Reported Outcomes Information Measurement System; a set of patient-reported outcome measures
- SAH
subarachnoid hemorrhage
- TIA
transient ischemic attack
REFERENCES
- 1.Katzan IL, Thompson NR, Walia HK, Moul DE, Foldvary-Schaefer N. Sleep-related symptoms in patients with mild stroke. J Clin Sleep Med. 2020;16(1):55–64. 10.5664/jcsm.8122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hermann DM, Bassetti CL. Role of sleep-disordered breathing and sleep-wake disturbances for stroke and stroke recovery. Neurology. 2016;87(13):1407–1416. 10.1212/WNL.0000000000003037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leppävuori A, Pohjasvaara T, Vataja R, Kaste M, Erkinjuntti T. Insomnia in ischemic stroke patients. Cerebrovasc Dis. 2002;14(2):90–97. 10.1159/000064737 [DOI] [PubMed] [Google Scholar]
- 4.Vock J, Achermann P, Bischof M, et al. Evolution of sleep and sleep EEG after hemispheric stroke. J Sleep Res. 2002;11(4):331–338. 10.1046/j.1365-2869.2002.00316.x [DOI] [PubMed] [Google Scholar]
- 5.Hermann DM, Bassetti CL. Sleep-related breathing and sleep-wake disturbances in ischemic stroke. Neurology. 2009;73(16):1313–1322. 10.1212/WNL.0b013e3181bd137c [DOI] [PubMed] [Google Scholar]
- 6.Schlesinger I, Erikh I, Nassar M, Sprecher E. Restless legs syndrome in stroke patients. Sleep Med. 2015;16(8):1006–1010. 10.1016/j.sleep.2014.12.027 [DOI] [PubMed] [Google Scholar]
- 7.Mims KN, Kirsch D. Sleep and Stroke. Sleep Med Clin. 2016;11(1):39–51. 10.1016/j.jsmc.2015.10.009 [DOI] [PubMed] [Google Scholar]
- 8.Kim KT, Moon HJ, Yang JG, Sohn SI, Hong JH, Cho YW. The prevalence and clinical significance of sleep disorders in acute ischemic stroke patients-a questionnaire study. Sleep Breath. 2017;21(3):759–765. 10.1007/s11325-016-1454-5 [DOI] [PubMed] [Google Scholar]
- 9.Baglioni C, Nissen C, Schweinoch A, et al. Polysomnographic characteristics of sleep in stroke: a systematic review and meta-analysis. PLoS One. 2016;11(3):e0148496. 10.1371/journal.pone.0148496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khot SP, Morgenstern LB. Sleep and Stroke. Stroke. 2019;50(6):1612–1617. 10.1161/STROKEAHA.118.023553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tang WK, Grace Lau C, Mok V, Ungvari GS, Wong KS. Insomnia and health-related quality of life in stroke. Top Stroke Rehabil. 2015;22(3):201–207. 10.1179/1074935714Z.0000000026 [DOI] [PubMed] [Google Scholar]
- 12.Glozier N, Moullaali TJ, Sivertsen B, et al. The course and impact of poststroke insomnia in stroke survivors aged 18 to 65 years: results from the Psychosocial Outcomes In StrokE (POISE) Study. Cerebrovasc. Dis Extra. 2017;7(1):9–20. 10.1159/000455751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katzan IL, Schuster A, Newey C, Uchino K, Lapin B. Patient-reported outcomes across cerebrovascular event types: More similar than different. Neurology. 2018;91(23):e2182–e2191. 10.1212/WNL.0000000000006626 [DOI] [PubMed] [Google Scholar]
- 14.Brott T, Adams HP Jr, Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–870. 10.1161/01.STR.20.7.864 [DOI] [PubMed] [Google Scholar]
- 15.van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19(5):604–607. 10.1161/01.STR.19.5.604 [DOI] [PubMed] [Google Scholar]
- 16.Cella D, Lai JS, Nowinski CJ, et al. Neuro-QOL: brief measures of health-related quality of life for clinical research in neurology. Neurology. 2012;78(23):1860–1867. 10.1212/WNL.0b013e318258f744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.PROMIS Network . PROMIS - Dynamic Tools to Measure Health Outcomes from the Patient Perspective. www.nihpromis.org. Last accessed June 10, 2020.
- 18.Choi SW, Schalet B, Cook KF, Cella D. Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychol Assess. 2014;26(2):513–527. 10.1037/a0035768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association: Washington, DC; 2013. [Google Scholar]
- 20.Wu S, Mead G, Macleod M, Chalder T. Model of understanding fatigue after stroke. Stroke. 2015;46(3):893–898. 10.1161/STROKEAHA.114.006647 [DOI] [PubMed] [Google Scholar]
- 21.Chen YK, Lu JY, Mok VC, Ungvari GS, Chu WC, Wong KS, Tang WK. Clinical and radiologic correlates of insomnia symptoms in ischemic stroke patients. Int J Geriatr Psychiatry. 2011;26(5):451–457. 10.1002/gps.2547 [DOI] [PubMed] [Google Scholar]
- 22.Hénon H. Pain after stroke: a neglected issue. J Neuro. Neurosurg Psychiatry. 2006;77(5):569. 10.1136/jnnp.2005.085761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Killgore WDS, Weber M. Sleep deprivation and cognitive performance. Sleep Deprivation and Disease. M Bianchi, ed. Springer: New York, NY; 2014. 10.1007/978-1-4614-9087-6_16 [DOI] [Google Scholar]
- 24.Falck RS, Best JR, Davis JC, Eng JJ, Middleton LE, Hall PA, Liu-Ambrose T. Sleep and cognitive function in chronic stroke: a comparative cross-sectional study. Sleep. 2019;42(5):zsz040. 10.1093/sleep/zsz040 [DOI] [PubMed] [Google Scholar]
- 25.Kim J, Kim Y, Yang KI, Kim DE, Kim SA. The relationship between sleep disturbance and functional status in mild stroke patients. Ann Rehabil Med. 2015;39(4):545–552. 10.5535/arm.2015.39.4.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oczkowski C, O’Donnell M. Reliability of proxy respondents for patients with stroke: a systematic review. J Stroke Cerebrovasc Dis. 2010;19(5):410–416. 10.1016/j.jstrokecerebrovasdis.2009.08.002 [DOI] [PubMed] [Google Scholar]
- 27.Palomäki H, Berg A, Meririnne E, Kaste M, Lönnqvist R, Lehtihalmes M, Lönnqvist J. Complaints of poststroke insomnia and its treatment with mianserin. Cerebrovasc Dis. 2003;15(1-2):56–62. 10.1159/000067127 [DOI] [PubMed] [Google Scholar]
- 28.Kim WH, Jung HY, Choi HY, et al. The associations between insomnia and health-related quality of life in rehabilitation units at 1month after stroke. J Psychosom Res. 2017;96:10–14. 10.1016/j.jpsychores.2017.02.008 [DOI] [PubMed] [Google Scholar]
- 29.Roberts RE, Shema SJ, Kaplan GA, Strawbridge WJ. Sleep complaints and depression in an aging cohort: A prospective perspective. Am J Psychiatry. 2000;157(1):81–88. 10.1176/ajp.157.1.81 [DOI] [PubMed] [Google Scholar]
- 30.Roehrs T, Hyde M, Blaisdell B, Greenwald M, Roth T. Sleep loss and REM sleep loss are hyperalgesic. Sleep. 2006;29(2):145–151. 10.1093/sleep/29.2.145 [DOI] [PubMed] [Google Scholar]
- 31.Tiede W, Magerl W, Baumgärtner U, Durrer B, Ehlert U, Treede RD. Sleep restriction attenuates amplitudes and attentional modulation of pain-related evoked potentials, but augments pain ratings in healthy volunteers. Pain. 2010;148(1):36–42. 10.1016/j.pain.2009.08.029 [DOI] [PubMed] [Google Scholar]
- 32.Good DC, Henkle JQ, Gelber D, Welsh J, Verhulst S. Sleep-disordered breathing and poor functional outcome after stroke. Stroke. 1996;27(2):252–259. 10.1161/01.STR.27.2.252 [DOI] [PubMed] [Google Scholar]
- 33.Johnson KG, Johnson DC. Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med. 2010;6(2):131–137. 10.5664/jcsm.27760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ryan CM, Bayley M, Green R, Murray BJ, Bradley TD. Influence of continuous positive airway pressure on outcomes of rehabilitation in stroke patients with obstructive sleep apnea. Stroke. 2011;42(4):1062–1067. 10.1161/STROKEAHA.110.597468 [DOI] [PubMed] [Google Scholar]
- 35.Joa KL, Kim WH, Choi HY, et al. The effect of sleep disturbances on the functional recovery of rehabilitation inpatients following mild and moderate stroke. Am J Phys Med Rehabil. 2017;96(10):734–740. 10.1097/PHM.0000000000000744 [DOI] [PubMed] [Google Scholar]
- 36.Morgenthaler TI, Kapur VK, Brown T, et al. Standards of Practice Committee of the American Academy of Sleep Medicine . Practice parameters for the treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30(12):1705–1711. 10.1093/sleep/30.12.1705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Comella CL. Treatment of restless legs syndrome. Neurotherapeutics. 2014;11(1):177–187. 10.1007/s13311-013-0247-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McCurry SM, Logsdon RG, Teri L, Vitiello MV. Evidence-based psychological treatments for insomnia in older adults. Psychol Aging. 2007;22(1):18–27. 10.1037/0882-7974.22.1.18 [DOI] [PubMed] [Google Scholar]
- 39.Nguyen S, Wong D, McKay A, et al. Cognitive behavioural therapy for post-stroke fatigue and sleep disturbance: a pilot randomised controlled trial with blind assessment. Neuropsychol Rehabil. 2019;29(5):723–738. 10.1080/09602011.2017.1326945 [DOI] [PubMed] [Google Scholar]
- 40.Cao H, Pan X, Li H, Liu J. Acupuncture for treatment of insomnia: a systematic review of randomized controlled trials. J. Altern. Complement. Med. 2009;15(11):1171–1186. 10.1089/acm.2009.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davies KA, Macfarlane GJ, Nicholl BI, Dickens C, Morriss R, Ray D, McBeth J. Restorative sleep predicts the resolution of chronic widespread pain: results from the EPIFUND study. Rheumatology (Oxford). 2008;47(12):1809–1813. 10.1093/rheumatology/ken389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Russell IJ, Holman AJ, Swick TJ, Alvarez-Horine S, Wang YG, Guinta D; Sodium Oxybate 06-008 FM Study Group . Sodium oxybate reduces pain, fatigue, and sleep disturbance and improves functionality in fibromyalgia: results from a 14-week, randomized, double-blind, placebo-controlled study. Pain. 2011;152(5):1007–1017. 10.1016/j.pain.2010.12.022 [DOI] [PubMed] [Google Scholar]
- 43.Brill AK, Horvath T, Seiler A, et al. CPAP as treatment of sleep apnea after stroke: A meta-analysis of randomized trials. Neurology. 2018;90(14):e1222–e1230. 10.1212/WNL.0000000000005262 [DOI] [PubMed] [Google Scholar]
- 44.Duss SB, Brill AK, Bargiotas P, Facchin L, Alexiev F, Manconi M, Bassetti CL. Sleep-Wake Disorders in Stroke-Increased Stroke Risk and Deteriorated Recovery? An Evaluation on the Necessity for Prevention and Treatment. Curr Neurol Neurosci Rep. 2018;18(10):72. 10.1007/s11910-018-0879-6 [DOI] [PubMed] [Google Scholar]
- 45.Sterr A, Kuhn M, Nissen C, et al. Post-stroke insomnia in community-dwelling patients with chronic motor stroke: Physiological evidence and implications for stroke care. Sci Rep. 2018;8(1):8409. 10.1038/s41598-018-26630-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arzt M, Young T, Finn L, Skatrud JB, Bradley TD. Association of sleep-disordered breathing and the occurrence of stroke. Am J Respir Crit Care Med. 2005;172(11):1447–1451. 10.1164/rccm.200505-702OC [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.