Abstract
The Ambulatory Blood Pressure Control and Home Blood Pressure (Morning and Evening) Lowering By N‐Channel Blocker Cilnidipine (ACHIEVE‐ONE) trial is a large‐scale clinical study on blood pressure (BP) and pulse rate (PR) in the real world with use of cilnidipine, a unique L/N‐type Ca channel blocker, possessing a suppressive action on increased sympathetic activity in patients with essential hypertension. The effects of cilnidipine on morning hypertension were examined. The authors examined 2319 patients treated with cilnidipine for 12 weeks. Clinic systolic BP (SBP) decreased by 19.6 mm Hg from 155.0 mm Hg, whereas morning SBP decreased by 17.0 mm Hg from 152.9 mm Hg after 12‐week cilnidipine treatment. Cilnidipine reduced both morning SBP and PR more markedly in patients with higher baseline morning SBP (−3.2 mm Hg and −1.3 beats per minute in the first quartile of morning SBP, −30.9 mm Hg and −3.2 beats per minute in the fourth quartile), and also reduced both morning PR and SBP more markedly in patients with higher baseline morning PR (0.6 beats per minute and −15.6 mm Hg in <70 beats per minute, and −9.7 beats per minute and −20.2 mm Hg in ≥85 beats per minute). Cilnidipine significantly reduced BP and PR in hypertensive patients at the clinic and at home, especially with higher BP and PR in the morning. J Clin Hypertens (Greenwich). 2012; 00:00–00. ©2012 Wiley Periodicals, Inc.
In recent years, it has been demonstrated that home or 24‐hour blood pressure (BP) monitoring predicts the risk of cardiovascular events. 1 , 2 , 3 Home BP measurements have been rapidly spreading because of its simple approach. Home morning hypertension is associated with a risk for chronic kidney disease and cardiovascular events. 4 , 5 In addition, an elevated pulse rate (PR) is associated with a risk for cardiovascular morbidity and mortality. 6 , 7 Therefore, management of morning hypertension and high PR is important in preventing cardiovascular events. Cilnidipine has two actions 8 , 9 : block L‐type Ca channels in vascular smooth muscle, which exerts an antihypertensive effect similar to L‐type Ca channel blockers (eg, amlodipine), and block N‐type Ca channels at sympathetic nerve endings, which suppresses increased sympathetic activity in animal models 9 , 10 , 11 and humans. 12 , 13 , 14 In this manner, cilnidipine is an effective Ca channel blocker to treat morning hypertension characterized by increased sympathetic activity in the early morning. Amlodipine, an L‐type Ca channel blocker, reduced BP, but its PR‐lowering effect is controversial. 15 , 16 , 17 In contrast, several studies demonstrated that cilnidipine reduced not only BP but also PR. 18 , 19 PR is influenced by both sympathetic and parasympathetic activities. Increased sympathetic activity leads to high PR. We are interested in whether cilnidipine is effective on not only higher BP, but also higher PR in hypertensive patients in the real world. The Ambulatory Blood Pressure Control and Home Blood Pressure (Morning and Evening) Lowering by N‐Channel Blocker Cilnidipine (ACHIEVE‐ONE) trial is a large‐scale clinical study designed to evaluate the clinical effects of cilnidipine on BP and PR measured at the clinic, at home, and by ambulatory BP monitoring (ABPM) in patients with essential hypertension in daily medical practice. Previously, another large‐scale clinical study was reported that cilnidipine reduced BP and PR at the clinic in hypertensive patients. 18 In this study, we examined the effects of cilnidipine on home BP and PR in hypertensive patients in the real world.
Methods
Patients and Study Design
This study was approved by the institutional review board of Jichi Medical University and was registered with the University Medical Information Network Clinical Trials Registry, Japan (UMIN000003695). This study was conducted in conformity with the Japanese Good Post‐Marketing Study Practice, which is a regulation of post‐marketing surveillance activities.
Clinical practitioners were openly recruited from across Japan. Patients had hypertension and accepted cilnidipine medication in daily medical practice during the period from October 2008 to September 2010. Pregnant women and women suspected of being pregnant were excluded from this study, but no restriction was set on age or complications. Each clinical practitioner participating in this study registered hypertensive patients with PostMaNet, an electric data capturing system developed by Fujitsu F.I.P. Corporation (Tokyo, Japan) within 2 weeks of starting cilnidipine treatment and uploaded follow‐up data on each patient into the system. No written informed consent was required, since this was an observational study in daily medical practice, not an interventional study. Cilnidipine is a Ca channel blocker approved in Japan for its use according to the following administration and dosage regimen: (1) for patients with hypertension at a once‐daily oral treatment after breakfast at a dose of 5 to 10 mg, and (2) for patients with severe hypertension at a dose that can be increased up to 20 mg. Regimens for cilnidipine and other concomitant drugs had been decided by practitioners with their patient’s agreement and were not changed until the study was finished, except for patients suffering therapeutic disadvantage. Adverse effects encountered in this study were collected with an electronic data capture system based on report from practitioners. Practitioners trained each patients on how to measure home BP as recommended by the guideline of the Japanese Society of Hypertension. 20 Each patient recorded home BP in a notebook specialized for BP management. During this study, each patient used an electronic cuff oscillometric device that had been approved by the Ministry of Health, Labor, and Welfare, Japan. Individual baseline data of BP and PR at home were determined as a 3‐day average of BP and PR measured once early in the morning (hereinafter called “morning”) and once just before going to bed (hereinafter called “evening”) before starting treatment. Baseline clinic BP and PR were measured once before starting treatment. Home BP and PR in the morning before medication and evening after medication and clinic BP and PR at each visit were measured once at weeks 4, 8, and 12 of treatment.
Statistical Analysis
To estimate sample size for an analysis of relationship between stratified SBP in the morning (MSBP) and PR in the morning (MPR), we assumed that cilnidipine reduced average MPR by 0.5, 1.0, 1.5, 2.5 beats per minute (bpm) in the first, second, third, and fourth quartiles, respectively, of MSBP with 10 bpm standard deviation (SD) of MPR as referenced by another study that cilnidipine reduced PR by 1.2 bpm with SD by 10 bpm. 18 Using these estimated data, sample size in this study was calculated as a total of 2000 patients performed by the one‐way analysis of variance (ANOVA) with two‐sided significance, because 500 patients in each quartile were required to achieve a minimum statistical power of 80%. Data are expressed as mean±SD unless otherwise noted. Evening SBP (ESBP) subtracted from MSBP of the same day was defined as the morning‐evening SBP difference (Di‐ME‐SBP). The average of MSBP and ESBP was defined as the mean morning‐evening SBP (Ave‐ME‐SBP). An unpaired t test was carried out to evaluate differences in baseline values of MSBP and the degree of changes in clinic SBP (CSBP) and MSBP. A Dunnett test was employed to analyze changes in BP and PR after starting treatment. A paired t test or a Wilcoxon signed rank sum test was used for comparison of BP and PR between pretreatment and post‐treatment values. A Fisher exact test was used in the analysis of changes in patient distribution, and a one‐way ANOVA was employed for the analysis of changes in MSBP, MPR, and Di‐ME‐SBP in relation to the value of MSBP, MPR, and Di‐ME‐SBP at baseline. In all tests, P<.05 (two‐tailed) was regarded as significant.
Results
Baseline Characteristics
Patient characteristics are shown in Table I. This report covers data from 2319 patients who had baseline MSBP values in the ACHIEVE‐ONE study. Among them, 171 patients had no MSBP values during cilnidipine treatment. There was no significant difference in baseline MSBP values between the group of 171 patients and the others who measured MSBP at least once during treatment (152.8±18.6 vs 152.9±16.1 mm Hg, respectively, P=.971). Of 171 patients, there were patients who measured CSBP during the treatment. The effects of cilnidipine on CSBP in the two groups showed no significant differences (eg, changes from baseline after 12 weeks were −19.0±22.0 mm Hg [n=65] and −19.3±19.9 mm Hg [n=1876] for 171 patients and the patients who measured MSBP, respectively, P=.911).
Table I.
Characteristics of Patients
| Baseline characteristics of patients, No. | 2319 |
| Age, y | 67.8±12.0 |
| BMI, kg/m2 | 23.9±3.6 |
| Men, No. (%) | 1271 (54.8) |
| Comorbidity, No. (%) | 1704 (73.5) |
| Dyslipidemia, No. (%) | 566 (24.4) |
| Ischemic heart disease, No. (%) | 435 (18.8) |
| Diabetes mellitus, No. (%) | 353 (15.2) |
| Cerebral vascular disorder, No. (%) | 188 (8.1) |
| Chronic kidney disease, No. (%) | 156 (6.7) |
| Cilnidipine monotherapy during the study, No. (%) | 812 (35.0) |
| Combination therapy during the study, No. (%) | 1507 (65.0) |
| Concomitant antihypertensive drug | |
| ARB, No. (%) | 1082 (46.7) |
| Diuretic, No. (%) | 303 (13.1) |
| β‐Blocker, No. (%) | 195 (8.4) |
| αβ‐Blocker, No. (%) | 176 (7.6) |
| CCB, No. (%) | 171 (7.4) |
| ACE inhibitor, No. (%) | 131 (5.6) |
| α‐Blocker, No. (%) | 61 (2.6) |
Abbreviations: ACE, angiotensin‐converting enzyme; ARB, angiotensin receptor blocker; CCB, calcium channel blocker. Age and body mass index (BMI): mean±standard deviation.
Cilnidipine Treatment
In this study, cilnidipine was prescribed once daily in the morning for 1792 (77.3%) patients, once daily in the evening for 267 (11.5%) patients, and twice daily in the morning and evening for 260 (11.2%) patients, with a mean daily dose level being 10.6±3.9 mg.
Changes in BP and PR at the Clinic and at Home
SBP and diastolic BP (DBP) decreased significantly after 4 weeks and thereafter, either at the clinic or at home (Figure 1). Changes from baseline after 12 weeks were −19.6, −17.0, and −13.6 mm Hg, for CSBP, MSBP, and ESBP, respectively. Moreover, PR decreased significantly after 4 weeks both at the clinic and at home (Figure 1).
Figure 1.
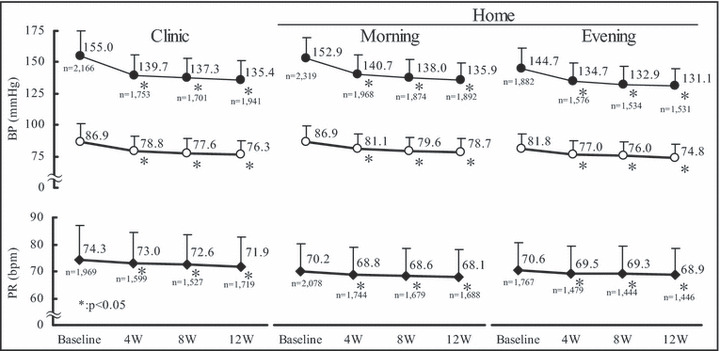
Changes in blood pressure (BP) and pulse rate (PR) at the clinic and at home. W indicates week; bpm, beats per minute; • systolic BP;○ diastolic BP; ♦ PR. *P<.05 vs baseline.
At baseline, 76.0% of patients were in the sustained hypertension group, CSBP ≥140 mm Hg and MSBP ≥135 mm Hg, but this proportion significantly decreased to 25.4% after 12 weeks (Figure 2). The ratio of patients in the well controlled group, CSBP <140 mm Hg and MSBP <135 mm Hg, rose significantly from 5.7% to 35.9% (Figure 2).
Figure 2.
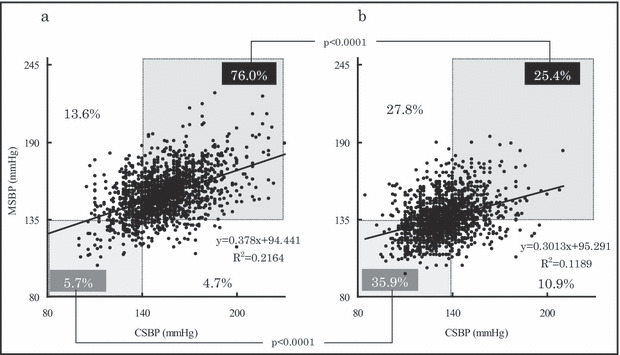
Changes in the percentages of patients categorized by clinic systolic blood pressure (CSBP) and mean systolic blood pressure (MSBP) at baseline (a) and after 12 weeks of treatment (b).
Morning SBP at baseline was divided into quartiles, and changes in MSBP and MPR were compared among the quartiles. Results revealed that the higher the MSBP at baseline, the greater MSBP (P<.0001, Figure 3a and 3b) and MPR (P=.0077, Figure 3c) was reduced. In contrast, the higher baseline ESBP, the more ESBP was reduced (P<.0001), with the exception of evening PR (P=.0868) (data not shown). The same significant reduction pattern was also observed when the relation was analyzed by percentage of reduction. The percentage value of each quartile from MSBP quartile 1 (Q1) to MSBP quartile 4 (Q4), was −2.1, −9.0, −12.5, and −17.7 for MSBP (P<.0001) and −1.1, −1.8, −2.5, and −3.6 for MPR, (P=.0146), respectively. Morning PR at baseline was divided into three categories (<70, ≥70 but <85, and ≥85 bpm) from three studies. A study by Ohasama 21 reported that even in normotensive patients whose MSBPs were <135 mm Hg, the risk for individuals with MPR ≥70 bpm to develop cardiovascular mortality was about double. In addition, the group with higher PR was subdivided into two groups according to the result of a Framingham study 7 that the cardiovascular and all cause mortality risks for individuals with heart rate ≥85 bpm was higher than <85 bpm. The Norway prospective study 22 demonstrated that an increase in PR was associated with increased risk of death from ischemic heart disease and for all‐cause mortality, when PR was divided into three categories, <70, ≥70 but <85, and ≥85 bpm. It was revealed that the higher the baseline MPR, the greater MPR was reduced (Figure 3d and 3e). Furthermore, the higher the baseline MPR, the greater MSBP was reduced (Figure 3f). The same significant reduction pattern was also observed when the relation was analyzed by percentage reduction. The percent value of each category, from MPR <70 bpm to MPR ≥85 bpm, was 1.3, −4.7, and −10.6 for MPR, (P<.0001) and −9.7, −10.6, and −12.4 for MSBP (P<.0106), respectively.
Figure 3.
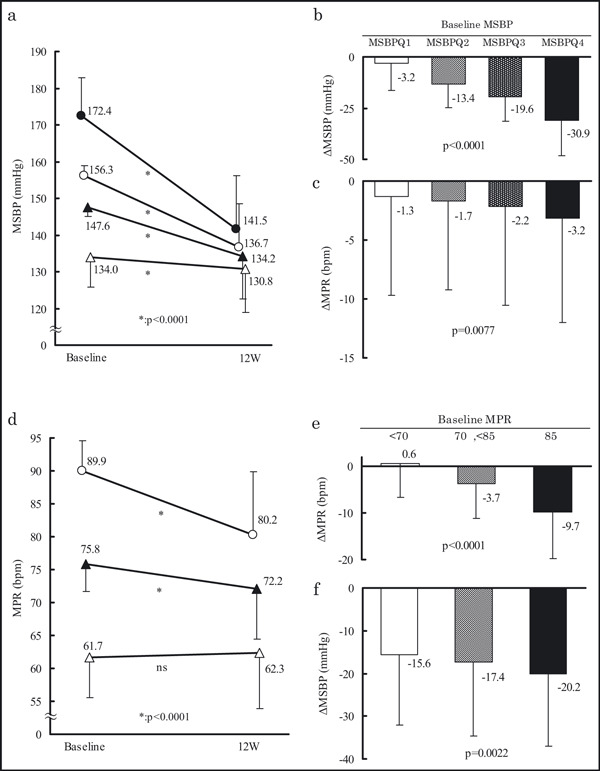
Changes in mean systolic blood pressure (MSBP) and mean pulse rate (MPR) in relation to baseline mean systolic blood pressure (MSBP) quartiles and changes in MPR and MSBP in relation to baseline MPR. MSBP quartile 1 (Q1): MSBP <142.7 mm Hg, MSBP quartile 2 (Q2): MSBP ≥142.7 but <151.7 mm Hg, MSBP quartile 3 (Q3): MSBP ≥151.7 but <161.3 mm Hg, MSBP quartile 4 (Q4): MSBP ≥161.3 mm Hg. Comparison of MSBP between baseline and after 12 weeks of treatment (12W) (a). MSBP quartiles: MSBPQ1 (Δ); MSBPQ2 (▲); MSBPQ3 (○); MSBPQ4 (•). (b) Changes in MSBP from baseline to after 12 weeks of treatment (b). Changes in MPR from baseline to after 12 weeks of treatment (c). Comparison of MPR between baseline and after 12 weeks of treatment (d). MPR: <70 beats per minute (bpm) (Δ); ≥70 but <85 bpm (▲); ≥85 bpm (○). Changes in MPR from baseline to after 12 weeks of treatment (e). Changes in MSBP from baseline to after 12 weeks of treatment (f).
To exclude the possibility that BP‐ and PR‐lowering effects of cilnidipine accounted only for consequence of phenomenon of regression to the mean, we examined the changes in BP and PR in patients treated with cilnidipine in relation to stratified BP and PR at baseline. When each of the four groups divided by MSBP quartiles (MSBPQ1‐Q4) was subdivided into two groups by a cutoff MPR level of 70 bpm, changes in MSBP after treatment were significantly greater in patients with MPR ≥70 bpm than in patients with MPR <70 bpm in the MSBPQ4 group, while in the other lower MSBP groups (MSBPQ1–Q3) there were no significant differences in changes in MSBP between the MPR subgroups (Figure 4). It is also noted that MSBP and MPR at home had little correlation with each other at baseline (r=0.095), after 12‐week treatment (r=−0.012), or in amount of changes (r=0.101) by Spearman’s correlation coefficient analysis.
Figure 4.
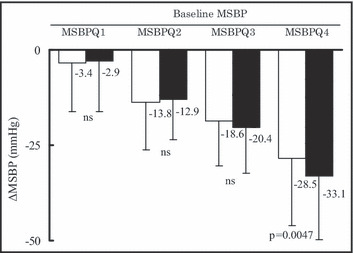
Changes in mean systolic blood pressure (MSBP) in relation to MSBP quartile and mean pulse rate (MPR) categories at baseline. MSBP quartile 1 (Q1): MSBP <142.7 mm Hg; MSBP quartile 2 (Q2): MSBP ≥142.7 but <151.7 mm Hg; MSBP quartile 3 (Q3): MSBP ≥151.7 but <161.3 mm Hg; MSBP quartile 4 (Q4): MSBP ≥161.3 mm Hg. MPR: <70 bpm (□); ≥70 beats per minute (bpm) (▪). ns indicates not significant.
Among patients with morning hypertension (MSBP ≥135 mm Hg), the percentage of patients with high MPR (≥70 bpm) decreased significantly from 46.5% at baseline to 24.4% after 12 weeks (P<.0001, not shown).
Significant decreases in MSBP and MPR were also seen when β‐blockers were concomitantly used (Table II). While MSBP and MPR decreased significantly by 17.3 mm Hg from 153.3±15.7 mm Hg and by 2.1 bpm from 70.7±10.3 bpm without β‐blockers, they also decreased significantly by 13.7 mm Hg from 149.3±16.2 mm Hg and by 1.8 bpm from 67.0±10.8 bpm, respectively, with β‐blockers after 12 weeks. Similar results were also observed in patients without concomitant antihypertensive drug use as well as in patients with or without angiotensin receptor blockers (ARBs), and angiotensin‐converting enzyme (ACE).
Changes in Ave‐ME‐SBP and Di‐ME‐SBP
We previously reported that the percentages of elderly people, drinkers, and β‐blocker users were higher in the group with Di‐ME‐SBP ≥15 mm Hg than that with <15 mm Hg in medicated hypertensive patients. 23 Therefore, it was desirable to manage the Di‐ME‐SBP below 15 mm Hg even in hypertensive patients whose CSBP were well controlled. 23 In the present study, the percentage of patients with Ave‐ME‐SBP ≥135 mm Hg decreased significantly from 85.1% at baseline to 43.1% after 12 weeks, and that of patients with Ave‐ME‐SBP ≥135 mm Hg and Di‐ME‐SBP ≥15 mm Hg decreased significantly from 20.9% to 7.1%. Moreover, normotensives with Ave‐ME‐SBP <135 mm Hg and Di‐ME‐SBP <15 mm Hg rose significantly from 10.6% to 45.8% (Figure 5).
Figure 5.
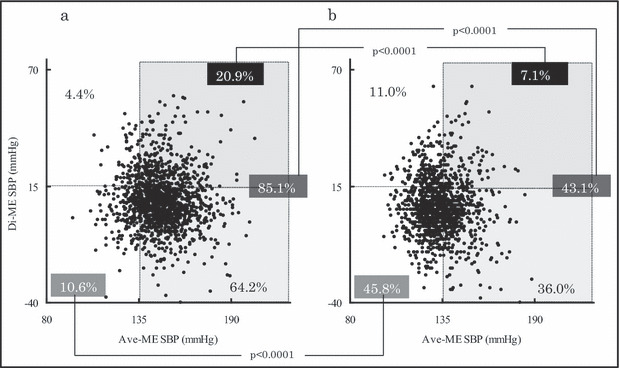
Changes in the percentage of patients distributed into four groups categorized by mean morning‐evening systolic blood pressure (Ave‐ME‐SBP) and morning‐evening systolic blood pressure difference (Di‐ME‐SBP) at baseline (a) and after 12 weeks of treatment (12W) (b).
When Di‐ME‐SBP at baseline was divided into quartiles, it was revealed that the higher the baseline Di‐ME‐SBP, the more Di‐ME‐SBP decreased. In contrast, in the case that baseline Di‐ME‐SBP was <0.7 mm Hg, in which patients whose ESBP was higher than MSBP were included, Di‐ME‐SBP increased (Figure 6).
Figure 6.
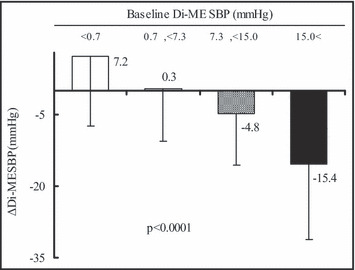
Changes in morning‐evening systolic blood pressure difference (Di‐ME‐SBP) in relation to Di‐ME‐SBP quartiles at baseline.
Adverse Reactions Related to Cilnidipine
A total of 63 episodes of adverse reactions occurred in 59 patients (2.54%). Major adverse reactions were dizziness (8 episodes, 0.34%), hypotension (5 episodes, 0.22%), flushing (4 episodes, 0.17%), hot flushes (4 episodes, 0.17%), and palpitations (4 episodes, 0.17%).
Discussion
ACHIEVE‐ONE is a large‐scale clinical study on hypertensive patients. The study demonstrated that a unique L/N‐type Ca channel blocker, cilnidipine, reduced both MSBP and MPR more markedly in patients with higher MSBP at baseline, and those with both MPR and MSBP more markedly in patients with higher MPR at baseline. These effects of cilnidipine are new features not known in conventional L‐type Ca channel blockers. We speculated that cilnidipine suppressed increased sympathetic activity in the morning by independent BP‐ and PR‐lowering effects through neuronal N‐type Ca channel blocking in addition to L‐type Ca channel blocking. 8 , 9
The percentage of patients with baseline MSBP >135 mm Hg was 90% in the present study and 94% in an add‐on study of amlodipine 5 to 10 mg daily. 24 MSBP decreased by 17 mm Hg from 152.9 mm Hg in the present study and by 16 mm Hg from 151.5 mm Hg in the add‐on study of amlodipine. In addition, similar to conventional L‐type Ca channel blockers, cilnidipine reduced MSBP more markedly in patients with higher MSBP at baseline. The BP‐lowering effect through L‐type Ca channel blocking of cilnidipine was comparable to that of amlodipine. This result may involve a consequence of the regression to the mean. However, cilnidipine reduced MSBP more markedly in patients with higher MPR at baseline and also reduced MPR more markedly in patients with higher MSBP at baseline. Furthermore, as shown in Figure 4, reductions in MSBP were significantly greater in the high MPR (≥70 bpm) group than the low (<70 bpm) MPR group, only at the top quartile of MSBP at baseline. Given that regression to the mean was the only factor that led to BP lowering, there was no difference between the PR groups (Figure 4). Therefore, the BP‐lowering effect of cilnidipine in the morning hypertension group (MSBPQ4) with high MPR (≥70 bpm) was one of the effects of cilnidipine itself.
Generally, morning hypertension involves increased sympathetic activity 25 , 26 and the renin‐angiotensin system (RAS). 28 Cilnidipine reduced MSBP and MPR even in patients who had already been administrated β‐blockers or RAS inhibitors (including ARBs and ACE inhibitors). These additive BP‐ and PR‐lowering effects of cilnidipine may be a reflection of dual L‐and N‐type Ca channel–blocking actions differing from β‐adrenergic receptor blocking and RAS‐inhibiting actions (Table II). Cilnidipine would be an optimal Ca channel blocker for patients with “high rate morning hypertension” characterized by high MSBP and MPR.
Table II.
Changes in MSBP and MPR in Relation to Concomitantly Used Hypertensive Drugs
| MSBP | MPR | |||||||
|---|---|---|---|---|---|---|---|---|
| Week 0 | Week 12 | No. | P Value | Week 0 | Week 12 | No. | P Value | |
| Cilnidipine monotherapy | 154.6±14.4 | 135.1±12.1 | 666 | <.0001 | 71.0±10.6 | 68.8±10.1 | 609 | <.0001 |
| Combination therapy | 151.6±16.4 | 136.4±14.2 | 1226 | <.0001 | 69.6±10.2 | 67.6±10.2 | 1079 | <.0001 |
| RAS inhibitor (−) | 153.0±15.5 | 135.6±12.6 | 914 | <.0001 | 70.7±10.6 | 68.5±10.0 | 823 | <.0001 |
| ARB (+) | 152.6±16.0 | 136.4±14.4 | 895 | <.0001 | 69.5±10.3 | 67.4±10.1 | 794 | <.0001 |
| ACE inhibitor (+) | 149.6±16.5 | 136.0±12.7 | 110 | <.0001 | 71.2±10.9 | 69.4±11.2 | 96 | =.0326 |
| β‐Blocker (−) | 153.3±15.7 | 136.0±13.4 | 1582 | <.0001 | 70.7±10.3 | 68.6±10.1 | 1423 | <.0001 |
| β‐Blocker (+) | 149.3±16.2 | 135.6±14.3 | 310 | <.0001 | 67.0±10.8 | 65.2±10.1 | 265 | =.0005 |
Abbreviations: ACE, angiotensin‐converting enzyme; ARB, angiotensin receptor blocker; MPR, morning pulse rate; MSBP, morning systolic blood pressure; RAS, renin‐angiotensin system.
It has been reported that elevated PR is a risk for cardiovascular events. 29 , 30 Recently, a large population cohort of apparently healthy men and women showed that an increase in resting PR from <70 bpm to >85 bpm during a 10‐year period was associated with a 1.9‐fold higher risk of death from ischemic heart disease. 22 In addition, ivabradine, a selective PR‐lowering drug, has been reported to reduce cardiovascular mortality or hospitalization of patients with heart failure. 31 The PR‐lowering effect of cilnidipine has been confirmed by several reports, 18 , 19 , 32 although that of amlodipine is controversial, 15 , 16 , 17 significant PR reduction was not observed in the open‐label repeated studies in patients treated with L‐type Ca channel blockers, amlodipine, 33 lercanidipine, and nifedipine GITS. 34 Cilnidipine lowered MPR only in the high MPR group. In hypertensive patients with PR <70 bpm, even if they had increased sympathetic activity, cilnidipine significantly reduced MSBP but not MPR, suggesting that the L‐type channel–blocking action may be predominantly effective compared with the N‐type–blocking action in these patients. Therefore, cilnidipine may be still beneficial for future cardiovascular risk for hypertensive patients with low PR as well as those with high PR. It was reported that renal sympathetic denervation significantly lowered BP, but did not reduce PR or plasma noradrenaline levels, and even progressed glomerular hyperfiltration. 35 In addition, the Cilnidipine vs Amlodipine Randomised Trial for Evaluation in Renal Disease (CARTER) study demonstrated that cilnidipine prevented the prognosis of renal disease beyond its BP‐lowering effects. 36 Therefore, the combination of cilnidipine and renal sympathetic denervation may achieve better PR control and cardiorenal protection as well as BP control.
In the present study, cilnidipine reduced Di‐ME‐SBP in patients with baseline Di‐ME‐SBP >15 mm Hg by MSBP‐lowering effects. We demonstrated in our previous report that the percentages of medicated hypertensive patients with older age, regular alcohol drinking, and β‐blocker use were higher in the group with Di‐ME‐SBP >15 mm Hg than in the group with Di‐ME‐SBP <15 mm Hg. 23 Therefore, it was recommended to keep Di‐ME‐SBP <15 mm Hg even in patients whose CSBP were well controlled. 23 We also demonstrated that the risk for stroke was 2.1‐fold higher in the presence of sustained hypertension (Av‐ME‐SBP ≥135 mm Hg and Di‐ME‐SBP <20 mm Hg) and 6.6‐fold higher in the presence of morning hypertension (Av‐ME‐SBP ≥135 mm Hg and Di‐ME‐SBP ≥20 mm Hg). We speculated that cilnidipine prevents cerebrovascular events in morning hypertensive patients.
Study Limitations
A limitation of this study is that it did not incorporate a control group. Therefore, relative evaluation of the efficacy of cilnidipine was not possible despite the large number of patients enrolled into the study. Each BP measurement device may not be validated. BP data self‐measured at home were transcribed to a notebook and reported by patients to practitioners. Therefore, data may potentially include transcription errors and reporting bias.
Conclusions
This study clarified the characteristics of cilnidipine including greater MSBP reductions in a high MPR (≥70 bpm) group than a low (<70 bpm) MPR group at the top quartile of MSBP at baseline. An L/N‐type Ca channel blocker, cilnidipine, significantly reduced BP and PR at the clinic and at home in Japanese hypertensive patients, especially with high BP and high PR in the morning, in a real‐world setting.
Acknowledgments and disclosures: Kazuomi Kario, the principal investigator of ACHIEVE‐ONE, supervised its conduct and data analysis and had primary responsibility for the writing of this paper. The other authors have read and approved the manuscript of this study. None of the authors received remuneration for performing the study. We are indebted to all those who cooperated with ACHIEVE‐ONE and provided valuable data for this study. Details of the members of ACHIEVE‐ONE are listed in the Appendix.
Funding: This study was financially supported by Ajinomoto Pharmaceuticals Co., LTD, Tokyo Japan, and Mochida Pharmaceutical Co., LTD, Tokyo, Japan.
Hokkaido: Tetsuo Betsuyaku, Haruhiko Yoshimura, Hideki Nakamura, Harutatsu Muto, Manabu Hayashi, Atsushi Tamada, Katsuhisa Ishii, Noriyuki Nomura, Takanori Ogawa, Masaaki Umetsu, Akihiko Suzuki, Kazusuke Ito, Masatoshi Sato, Masahiko Kato, Tomoaki Matsumoto, Keiji Yoneya, Nobuichi Hikita, Kimio Nishizato, Yukinaga Nozawa, Yoshiaki Aizawa, Takayuki Mori, Tomonari Akatsu, Yoshiyuki Suzuki.
Tohoku: Tetsuo Yagi, Hiroki Hosaka, Takashi Saito, Eiichi Tanaka, Joji Sato, Masatoshi Akimoto, Osamu Kawashima, Satoru Chiba, Mutsuo Harada, Etsuo Otomo, Eiichiro Ikeno, Masayasu Nakagawa, Junya Chiba, Tetsu Watanabe, Ryohei Sakamoto, Tetsuro Shishido, Minoru Inoue, Kunihiko Kameda, Tomonori Igarashi, Takuya Miyamoto, Noriyuki Sato, Masami Murasawa, Makoto Sato, Yoshikazu Tamura, Makoto Ito, Yuichi Tsunoda, Takehiko Miyashita.
Kanto: Kazuo Eguchi, Manabu Moriya, Hiromi Mitsubayashi, Akio Amano, Eiji Tamiya, Makoto Noda, Katsuhiko Asanuma, Takahiro Oki, Hiroyuki Yamaguchi, Kazuhiro Shimizu, Yuji Kasamaki, Kunihiko Teraoka, Eitaro Kodani, Takayuki Morishima, Koichiro Yoshioka, Riichiro Nakayama, Junichi Nakagawa, Yawara Niijima, Shuji Kamikawa, Masahiro Tamano, Kumiko Nakayama, Zenpei Ono, Toru Yatsuhashi, Akio Oshima, Eiji Uchida, Tetsuo Sakai, Kazutoshi Mitsuo, Takahiro Uchida, Tamotsu Tejima, Nobuyuki Makishima, Natsue Kato, Masaya Kishi, Kenichi Sakakura, Yoko Pierce, Hiroshi Shibayama, Nobuo Hatori, Shigeru Kuroki, Kiyoshi Nakazawa, Hiroyuki Fujii, Takeharu Hayashi, Shinji Okubo, Morihisa Sekido, Yasumasa Fujiwara, Shuichi Taguchi, Toshihiko Nishioka, Masayuki Inagaki, Hisako Omori, Takeshi Endo, Hideshi Takenobu, Kazuki Fukui, Koh Tenei, Kenichi Ota, Jo Aikawa, Taku Iwaki, Yuichi Shinmaru, Kenichi Amitani, Tadashi Morimura, Hideki Nagaoka, Osamu Sasaki, Mikio Yuhara, Hideo Fujinuma, Junan Hou, Goki Watanabe, Toshihiro Makise, Yasuhiro Takagi, Yuriko Sato, Konomi Sakata, Hirotoshi Omura, Nobuhisa Hagiwara, Naoyuki Serikawa, Miki Ishiyama, Hideaki Kanazawa, Kazuhei Hibiya, Mitsuyuki Shimizu, Masahiko Shimizu, Kayoko Sato, Junichi Yamaguchi, Tsuyoshi Shiga, Takahiro Shibata, Masao Moroi, Ichiro Mizuguchi, Yoshiro Chiba, Koji Ohira, Yoshikatsu Sugito, Shinichi Suga, Nakabumi Kuroda, Junji Kanda, Masaaki Nagashima, Hisao Hara, Hiroshi Noda, Shunsaku Iwasaki, Masamichi Niizuma, Yasuo Okusu, Hiromaro Ito, Masaki Ota, Osahiro Takahashi, Mariko Endo, Daigo Kamei, Atsushi Takagi, Hiroshi Ogawa, Hidetaka Seguchi, Kagari Murasaki, Seiji Fukushima, Kei Suzuki, Zenko Nagashima, Masashi Otsuka, Sosuke Takahashi, Rihito Yamada, Toyoyuki Okubo, Toshiyuki Takahashi, Satoshi Hoshide, Hironobu Kawai, Toshiyuki Ando, Ami Issiki, Masatsugu Uchida, Nobuaki Shikama, Hiroshi Takahashi, Takahiro Sato, Masataka Sumiyoshi, Naoko Ishizuka, Takamasa Iwasawa, Tomohiro Seino, Tetsuya Tomariguchi.
Koshinetu: Osamu Kinoshita, Tsutomu Araki, Yoshio Ikeda, Chieko Itamoto, Toru Ida, Masanao Tani, Hokuriku Minoru Tagawa, Teruaki Kimura, Takane Owaki, Hiroaki Shintaku, Akira Nakano, Tomoyasu Momose, Yoshiteru Sekiguchi, Senshu Hifumi, Yasuhiko Mitsuke, Hitoshi Kitazawa, Toru Geshi, Minoru Takahashi, Taku Matsubara, Hiroyasu Uzui, Norito Homma, Noburu Konno, Masayuki Ogiwara, Hideo Miura, Akihiro Obata, Shinsuke Saito, Taro Kusuyama, Nobuo Koshiji, Ryuichi Sakai, Shunsuke Imai, Noriyuki Sekimura, Shoji Hotta.
Tokai: Koichi Yokoya, Norimoto Houda, Takashi Tanigawa, Issei Uchida, Masayoshi Sarai, Hiroshi Sato, Hajime Terada, Yasushi Wakabayashi, Takuo Ogawa, Tomohiko Shigemasa, Yasuaki Dohi, Kei Kawakami, Atsushi Taguchi, Tomonori Sugiura, Kengo Maeda, Kenji Miyagishima, Shigeo Sugino, Ryoji Ishiki, Hisashi Umeda, Sachiko Fukuta, Yasushi Wakida, Kazuhiro Matsuo, Fukashi Kasuya, Daisuke Kamoi, Motoyuki Fukuda, Takashi Shimojo, Shozo Ogawa, Kazunori Hayashi, Toshihiko Goto, Tomomitsu Tani, Rika Hasegawa, Yasushi Suzuki.
Kinki: Hidenori Kido, Shin Takiuchi, Toshiki Shimizu, Takashi Sakamoto, Jin Nariyama, Takahisa Yamada, Shinji Yoshida, Tomohiro Shinozuka, Yasumasa Yamamoto, Kenshi Fujii, Morihiko Kondo, Koji Hasegawa, Hiroyuki Miyamoto, Daisuke Shishikura, Kazuho Miyakoshi, Mitsumasa Oyanagi, Hiromichi Wada, Hideki Otsuki, Arata Iwasaki, Yasuyo Nakajima, Takeshi Kimura, Tetsuya Nomura, Yasuji Doi, Munenori Yoshizumi, Tadashi Miyamoto, Shinichi Yamamoto, Tomohiro Katsuya, Mitsunori Kawato, Hiroshi Kuwaki, Hideyuki Takaoka, Koshi Matsuo, Nobuaki Inoshiro, Masayasu Izuhara, Satoshi Morimoto, Yutaka Umayahara, Megumi Fukuyama, Shoichi Miyamoto, Masahiro Yamazaki, Tetsuro Kusaba, Takatomo Shima, Yoshitaka Iwanaga, Yukinori Shinoda, Mitsuo Matsuda, Naoki Murai, Tsuyoshi Sakoda, Mitsuhiko Ota, Haruki Endo, Koichi Seta, Kazuo Takeda, Kazuhiko Iguchi, Keisuke Shioji, Eiji Takai, Takayoshi Nemoto, Yoshihide Sakaguchi, Takashi Morita, Mitsugu Taniguchi, Masatoshi Nakao, Masahito Hiura, Kazunori Kashiwase, Akio Kimura, Soshiro Hanyu, Satoshi Iwaoka, Kim Su Sik, Issei Sano, Yuji Saito, Daisuke Kambayashi, Kunitake Fukai, Yoshio Kohno, Susumu Nishikawa, Hiromi Yamamoto, Shinobu Miyake, Shinichiro Oyama, Yoshihiro Himura, Natsuya Keira, Hirosumi Sakai, Dainari Nakashima, Osamu Nakajima, Yoshihumi Kojima, Yasushi Sasaki, Kazuya Ueda, Yasunori Nishida, Yota Urakabe, Hakuo Takahashi, Ryunosuke Tazaki, Masatake Fukunami, Hideki Goto, Katsuhiro Kobayashi, Naohiro Yoshida, Yasushi Okumoto, Taku Kato, Kan Zen, Hirofumi Takashima, Masayo Izawa, Kazuhisa Kijima, Hirokazu Mitsuoka, Mayu Nishio, Takahito Tokuoka, Hiroyuki Hashimoto, Katsuyuki Hasegawa, Keiichi Sakurai, Yukiko Kuga, Mitsuru Tsujimoto.
Chugoku: Yoji Neishi, Kazuyoshi Okada, Satoru Sakuragi, Issei Komatsubara, Minako Ohara, Yuko Toyama, Satoshi Miyazaki, Mai Fujiwara, Masaki Hashimoto, Tetsuya Sato, Mitsunori Okamoto, Fumiharu Miura, Nobuyuki Yamada, Fumiyo Tsunoda, Nobuyuki Morishima, Yukihiro Fukuda, Jun Iwasaki, Kenji Kawamoto, Machiko Tanakaya, Hiromoto Kosaka, Nobuo Shiode, Yasuko Kato, Asao Mimura, Soichiro Fuke, Atsuyuki Watanabe, Kunihisa Kohno.
Shikoku: Hitoshi Miyajima, Kiyoshi Nishino, Hiroyuki Fujinaga, Koji Sakai, Sakuma Takahashi, Shinobu Hosokawa, Yasumi Shintani, Junichiro Koga, Takafumi Okura, Shuntaro Ikeda, Kiyotaka Oshima, Kazuhiro Kawano, Akiyoshi Kakutani, Shunsuke Orino, Kenichi Miyoshi, Masanori Kuwabara, Miho Abe, Masaru Takahashi, Hiroshi Matsuoka, Jun Irita, Atsuhiko Iuchi, Norihito Kageyama, Koichi Kishi, Junichi Mikawa, Riyo Ogura, Hideo Kawakami, Akira Oshita.
Kyushu: Shinichi Ando, Ryo Shiraishi, Hideki Oka, Sumito Narita, Tatsuya Nunohiro, Tokushi Koga, Hiroshi Ono, Shigeru Kaseda, Yoshihiro Takeshi, Noboru Tamaki, Yasuhisa Iriki, Yoshihiro Fukuoka, Yoshihiko Otsubo, Shinichiro Fujishima, Ichiro Kajiwara, Masahiro Sonoda, Hidenori Tanaka, Manabu Setoguchi, Yoshito Nakamura, Masayoshi Yoshida, Kimiaki Nagase, Atsushi Iwata, Yasukazu Sato, Masahiko Nagata, Hirohide Kubo, Masachika Kuwabara, Noriaki Matsumoto, Sakuji Shigematsu, Chihiro Nakanishi, Hiroaki Nishikawa, Toshiaki Kadokami, Masanori Okabe, Yoshiaki Shintani, Yoshihisa Kizaki, Tadashi Yamamoto, Yuzo Uchida, Koichi Kaikita, Yoichi Tatsukawa, Tomoaki Makino, Naoki Ishikawa.
A part of this study was presented at the 34th Annual Scientific Meeting of the Japanese Society of Hypertension, Utsunomiya, Japan, October 20–22, 2011.
References
- 1. Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population‐based observation in Ohasama, Japan. J Hypertens. 1998;16:971–975. [DOI] [PubMed] [Google Scholar]
- 2. Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow‐up results from the pressioni arteriose monitorate e loro associazioni (pamela) study. Circulation. 2005;111:1777–1783. [DOI] [PubMed] [Google Scholar]
- 3. Kario K, Pickering TG, Matsuo T, et al. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–857. [DOI] [PubMed] [Google Scholar]
- 4. Ohkubo T, Asayama K, Kikuya M, et al. Prediction of ischaemic and haemorrhagic stroke by self‐measured blood pressure at home: the Ohasama study. Blood Press Monit. 2004;9:315–320. [DOI] [PubMed] [Google Scholar]
- 5. Agarwal R, Andersen MJ. Prognostic importance of clinic and home blood pressure recordings in patients with chronic kidney disease. Kidney Int. 2006;69:406–411. [DOI] [PubMed] [Google Scholar]
- 6. Palatini P, Benetos A, Grassi G, et al. Identification and management of the hypertensive patient with elevated heart rate: statement of a European Society of Hypertension consensus meeting. J Hypertens. 2006;24:603–610. [DOI] [PubMed] [Google Scholar]
- 7. Gillman MW, Kannel WB, Belanger A, et al. Influence of heart rate on mortality among persons with hypertension: the Framingham study. Am Heart J. 1993;125:1148–1154. [DOI] [PubMed] [Google Scholar]
- 8. Ogihara T, Kano T, Kakinuma C. Evaluation of the inhibitory effect of dihydropyridines on n‐type calcium channel by virtual three‐dimensional pharmacophore modeling. Arzneimittelforschung. 2009;59:283–288. [DOI] [PubMed] [Google Scholar]
- 9. Takahara A. Cilnidipine: a new generation Ca channel blocker with inhibitory action on sympathetic neurotransmitter release. Cardiovasc Ther. 2009;27:124–139. [DOI] [PubMed] [Google Scholar]
- 10. Takahara A, Koganei H, Takeda T, et al. Antisympathetic and hemodynamic property of a dual l/n‐type Ca(2+) channel blocker cilnidipine in rats. Eur J Pharmacol. 2002;434:43–47. [DOI] [PubMed] [Google Scholar]
- 11. Takahara A, Iwasaki H, Nakamura Y, et al. Cardiac effects of l/n‐type Ca2+ channel blocker cilnidipine in anesthetized dogs. Eur J Pharmacol. 2007;565:166–170. [DOI] [PubMed] [Google Scholar]
- 12. Sakata K, Shirotani M, Yoshida H, et al. Effects of amlodipine and cilnidipine on cardiac sympathetic nervous system and neurohormonal status in essential hypertension. Hypertension. 1999;33:1447–1452. [DOI] [PubMed] [Google Scholar]
- 13. Kosaka T, Nakagawa M, Ishida M, et al. Cardioprotective effect of an l/n‐type calcium channel blocker in patients with hypertensive heart disease. J Cardiol. 2009;54:262–272. [DOI] [PubMed] [Google Scholar]
- 14. Tomiyama H, Kimura Y, Kuwabara Y, et al. Cilnidipine more highly attenuates cold pressor stress‐induced platelet activation in hypertension than does amlodipine. Hypertens Res. 2001;24:679–684. [DOI] [PubMed] [Google Scholar]
- 15. Eguchi K, Kario K, Shimada K. Differential effects of a long‐acting angiotensin converting enzyme inhibitor (temocapril) and a long‐acting calcium antagonist (amlodipine) on ventricular ectopic beats in older hypertensive patients. Hypertens Res. 2002;25:329–333. [DOI] [PubMed] [Google Scholar]
- 16. Eguchi K, Kario K, Hoshide Y, et al. Comparison of valsartan and amlodipine on ambulatory and morning blood pressure in hypertensive patients. Am J Hypertens. 2004;17:112–117. [DOI] [PubMed] [Google Scholar]
- 17. Ishimitsu T, Minami J, Yoshii M, et al. Comparison of the effects of amlodipine and losartan on 24‐hour ambulatory blood pressure in hypertensive patients. Clin Exp Hypertens. 2002;24:41–50. [DOI] [PubMed] [Google Scholar]
- 18. Nagahama S, Norimatsu T, Maki T, et al. The effect of combination therapy with an l/n‐type Ca(2+) channel blocker, cilnidipine, and an angiotensin II receptor blocker on the blood pressure and heart rate in Japanese hypertensive patients: an observational study conducted in Japan. Hypertens Res. 2007;30:815–822. [DOI] [PubMed] [Google Scholar]
- 19. Yamagishi T. Beneficial effect of cilnidipine on morning hypertension and white‐coat effect in patients with essential hypertension. Hypertens Res. 2006;29:339–344. [DOI] [PubMed] [Google Scholar]
- 20. Imai Y, Otsuka K, Kawano Y, et al. Japanese Society of Hypertension (JSH) guidelines for self‐monitoring of blood pressure at home. Hypertens Res. 2003;26:771–782. [DOI] [PubMed] [Google Scholar]
- 21. Hozawa A, Ohkubo T, Kikuya M, et al. Prognostic value of home heart rate for cardiovascular mortality in the general population: the Ohasama study. Am J Hypertens. 2004;17:1005–1010. [DOI] [PubMed] [Google Scholar]
- 22. Nauman J, Janszky I, Vatten LJ, et al. Temporal changes in resting heart rate and deaths from ischemic heart disease. JAMA. 2011;306:2579–2587. [DOI] [PubMed] [Google Scholar]
- 23. Ishikawa J, Kario K, Hoshide S, et al. Determinants of exaggerated difference in morning and evening blood pressure measured by self‐measured blood pressure monitoring in medicated hypertensive patients: Jichi morning hypertension research (J‐MORE) study. Am J Hypertens. 2005;18:958–965. [DOI] [PubMed] [Google Scholar]
- 24. Kario K, Odawara M, Kimura K, et al. Nearly half of uncontrolled hypertensive patients could be controlled by high‐dose titration of amlodipine in the clinical setting: the Achieve study. Curr Hypertens Rev. 2011;7:102–110. [Google Scholar]
- 25. Schofl C, Becker C, Prank K, et al. Twenty‐four‐hour rhythms of plasma catecholamines and their relation to cardiovascular parameters in healthy young men. Eur J Endocrinol. 1997;137:675–683. [DOI] [PubMed] [Google Scholar]
- 26. Marfella R, Gualdiero P, Siniscalchi M, et al. Morning blood pressure peak, qt intervals, and sympathetic activity in hypertensive patients. Hypertension. 2003;41:237–243. [DOI] [PubMed] [Google Scholar]
- 27. Kario K. Morning surge in blood pressure and cardiovascular risk: evidence and perspectives. Hypertension. 2000;56:765–773. [DOI] [PubMed] [Google Scholar]
- 28. White WB. Importance of blood pressure control over a 24‐hour period. J Manag Care Pharm. 2007;13:34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Palatini P. Role of elevated heart rate in the development of cardiovascular disease in hypertension. Hypertension. 2000;58:745–750. [DOI] [PubMed] [Google Scholar]
- 30. Fox K, Borer JS, Camm AJ, et al. Resting heart rate in cardiovascular disease. J Am Coll Cardiol. 2007;50:823–830. [DOI] [PubMed] [Google Scholar]
- 31. Swedberg K, Komajda M, Bohm M, et al. Ivabradine and outcomes in chronic heart failure (shift): a randomised placebo‐controlled study. Lancet. 2000;376:875–885. [DOI] [PubMed] [Google Scholar]
- 32. Tanaka M. The l/n‐type calcium channel blocker, cilnidipine, reduces heart rate and albuminuria in patients with type 2 diabetes. J Int Med Res. 2000;38:602–610. [DOI] [PubMed] [Google Scholar]
- 33. Habeler G, Lenzhofer R, Pall H, et al. [Effectiveness and tolerance of amlodipine in treatment of patients with mild to moderate hypertension. Results of a long‐term study with a new calcium antagonist]. Wien Klin Wochenschr. 1992;104:16–20. [PubMed] [Google Scholar]
- 34. Fogari R, Mugellini A, Zoppi A, et al. Differential effects of lercanidipine and nifedipine GITS on plasma norepinephrine in chronic treatment of hypertension. Am J Hypertens. 2003;16:596–599. [DOI] [PubMed] [Google Scholar]
- 35. Lohmeier TE, Iliescu R, Liu B, et al. Systemic and renal‐specific sympathoinhibition in obesity hypertension. Hypertension. 2000;59:331–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fujita T, Ando K, Nishimura H, et al. Antiproteinuric effect of the calcium channel blocker cilnidipine added to renin‐angiotensin inhibition in hypertensive patients with chronic renal disease. Kidney Int. 2007;72:1543–1549. [DOI] [PubMed] [Google Scholar]


