Abstract
The malignant phenotype of tumour cells is fuelled by changes in the expression of various transcription factors, including some of the well-studied proteins such as p53 and Myc. Despite significant progress made, little is known about several other transcription factors, including ELF4, and how they help shape the oncogenic processes in cancer cells. To this end, we performed a bioinformatics analysis to facilitate a detailed understanding of how the expression variations of ELF4 in human cancers are related to disease outcomes and the cancer cell drug responses. Here, using ELF4 mRNA expression data of 9,350 samples from the Cancer Genome Atlas pan-cancer project, we identify two groups of patient’s tumours: those that expressed high ELF4 transcripts and those that expressed low ELF4 transcripts across 32 different human cancers. We uncover that patients segregated into these two groups are associated with different clinical outcomes. Further, we find that tumours that express high ELF4 mRNA levels tend to be of a higher-grade, afflict a significantly older patient population and have a significantly higher mutation burden. By analysing dose-response profiles to 397 anti-cancer drugs of 612 well-characterised human cancer cell lines, we discover that cell lines that expressed high ELF4 mRNA transcript are significantly less responsive to 129 anti-cancer drugs, and only significantly more response to three drugs: dasatinib, WH-4-023, and Ponatinib, all of which remarkably target the proto-oncogene tyrosine-protein kinase SRC and tyrosine-protein kinase ABL1. Collectively our analyses have shown that, across the 32 different human cancers, the patients afflicted with tumours that overexpress ELF4 tended to have a more aggressive disease that is also is more likely more refractory to most anti-cancer drugs, a finding upon which we could devise novel categorisation of patient tumours, treatment, and prognostic strategies.
Introduction
Genetic alterations in several transcription factors lead to genome-wide transcription changes that drive the malignant phenotypes [1–3]. Although many of these transcription factors, such as ELF4 a member of E74-like factor family (ELF), play essential physiological roles in healthy proliferating cells, a series of genetic aberrations within genes coding for these factors result in oncogenic behaviour of healthy cells [4, 5]. However, we know far less about how the expression of ELF4 affects the aggressiveness of disease across many human cancer types and their response to drug perturbations. Furthermore, despite the keen interest in determining how perturbations of ELF4 relate to specific aspects of malignant cells, compared to other transcription factors such as TP53 (PubMed score of 46333.87) and MYC (13294.24), ELF4 (35.41) remains among the least studied transcription factor in human cancers [6, 7].
Analysis of ELF4 in various human cancers has revealed that it plays essential roles in cellular differentiation, proliferation, and apoptosis in cancers of the prostate and breast [8], and is paradoxically associated with oncogenic activity [3, 8] and tumour suppressor roles [9]. Also, mutations in the coding sequence and mRNA expression variations of ELF4 have been reported in various human cancers [3, 5, 10]. These and other recent studies [4, 7, 11–13] have also generated a new appreciation of how aberrant ELF4 influences cancer development, the anti-cancer drug response of tumours, and the disease treatment outcomes.
Our current understanding of ELF4 and other cancer genes has largely been facilitated by large cancer profiling projects such as The Cancer Genome Atlas (TCGA) [14] and the International Cancer Genome Consortium [15]. Data get by these large cancer profiling projects have guided the identification of frequently altered cancer genes and the cancer type-specific regulators. Additionally, large-scale drug response screening projects, such as the Genomics of Drug Sensitivity in Cancer (GDSC) project [16], have been valuable in providing well-characterised cancer cell lines as models of disease for both drug discovery and the evaluation of drug action dependencies of cancer cells [17–20].
Here, we investigate the mRNA expression variations of ELF4 across pan-cancer TCGA tumours to identify the changes that have meaningful clinical value. By linking this information with the drug response profiles from the GDSC, we also investigate variations in the response of cancer cell types that are associated with ELF4 mRNA levels. Besides enabling the identification and selection of the most suitable anti-cancer drugs to treat a tumour with different ELF4 expression signatures, a multiscale understanding of ELF4 across different cancer types will likely yield better prediction of disease outcome.
Methods
The study protocol was approved by the University of Cape Town; Health Sciences Research Ethics Committee IRB00001938. The analyses in this study utilised publicly available datasets collected by the TCGA, CCLE and GDSC from consenting participants. Here, all analyses were performed following the relevant policies, regulations, and guidelines provided by the TCGA, CCLE and GDSC to analyse their datasets and report the findings.
We accessed and processed a pan-cancer TCGA project dataset derived from 9,350 patients afflicted with 32 distinct human cancers [21]. These datasets include evenly processed mRNA expression data, gene mutation data, and comprehensive deidentified clinical data for all patients.
Then we segregated the patient’s tumours across the pan-cancer studies into two groups: those that expressed a higher level of ELF4 mRNA transcripts and lower level of ELF4 mRNA transcripts. To achieve this, first, we applied z-normalisation to the measured ELF4 mRNA transcript across all the tumours. Then we considered those tumours with ELF4 mRNA z-score > 0 to have high ELF4 levels (3887 tumours) and those tumours with ELF4 mRNA z-score < 0 to have low ELF4 levels (5463).
Survival analysis
We used the clinical information provided by the Cancer Genome Atlas and the corresponding TCGA sample IDs to match the patient’s samples to the appropriate clinical outcomes and sample features. Then we used the Kaplan-Meier approach to estimate the duration of the overall survival and disease-free survival periods between tumours that expressed a high level of ELF4 mRNA transcripts and low levels of ELF4 mRNA transcripts [22]. Furthermore, across each of the 32 cancer types, we used the Kaplan-Meier method to compare the duration of the overall survival periods between patients afflicted with high-ELF4 tumours and those afflicted with low-ELF4 tumours (see S1 File).
Cancer grades across tumours that expressed high and low levels ELF4
We matched the TCGA sample IDs to the TCGA IDs provided in the clinical sample information to match the patients with tumours that either expressed low or high ELF4 levels to the samples’ clinical features. Then we performed a Chi-squared test to compare the distribution of tumours of various grades across each category of tumours that either expressed high ELF4 level and low ELF4 level.
Distribution of tumour expressed high ELF4 and low ELF4 across cancer types
Across each of the 32 TCGA pan-cancer analyses, we counted the absolute number of tumours that expressed high ELF4 transcript levels and those that expressed low ELF4 transcript levels. We also obtained the overall percentage of tumours that expressed higher or lower mRNA transcript levels of ELF4 across each cancer type.
Comparing median patients’ age, the number of mutations and fraction of the genome altered across the tumour groups
Across the two groups of tumours that expressed high ELF4 and low ELF4, we obtained each patient’s age. Furthermore, we calculated the number of gene mutations in each tumour and the fraction of the genome altered in each tumour. Then we used the nonparametric Mann-Whitney U-test for equality of medians for groups to compare the median age, the median number of mutations per tumour and fraction of the genome altered per patient between each group [23].
Dose-response of cancer cell lines that expressed high and low ELF4 levels
We obtained 244,656 dose-response profiles of 612 cancer cell lines to 397 anti-cancer drugs from the Genomics of Drug Sensitivity in Cancer (GDSC) database [16]. The cell lines within the GDSC database represent 31 different human cancers. Also, we obtained the mRNA expression levels of the ELF4 genes in these 612 cancer cell lines from the Cancer Cell Line Encyclopedia (CCLE; [24]). Using the mRNA expression data from the CCLE, we used the approach described above (for the primary TCGA tumours) to segregate the cell lines into two groups: 1) those with high ELF4 transcript levels and 2) those with low ELF4 transcript levels. Then we used the Welch test to compare the mean differences in the z-score transformed IC50 values between the cell lines with high ELF4 levels and those with low ELF4 levels, for each class of the 397 anti-cancer drugs (also see S2 File).
Differential genes expression and pathway analysis
We used the moderated student t-test employing the negative binomial model to identify differentially expressed mRNAs between PAAD, BRCA, SARC, KIRC and LAUD tumours that expressed higher ELF4 and those that expressed lower ELF4 (see S3 File) [25, 26]. Additionally, pathway enrichment analyses were performed using lists of significantly up-regulated genes in PAAD, BRCA, SARC, KIRC and LUAD tumours that expressed high ELF4. These were used to query Enrichr to return Reactome pathways enriched in the high-ELF4 tumour samples (Fig 5, S4 File).
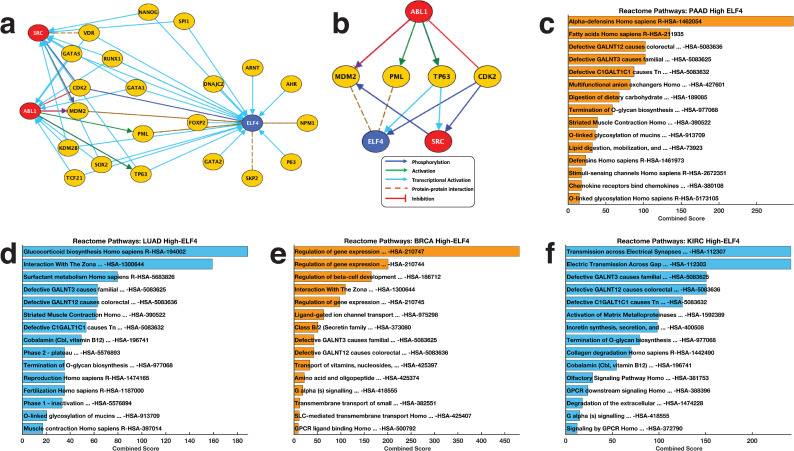
Fig 5.
(a) Complete connectivity network of ELF4 to the drug targets ABL1 and SRC minded from the literature and various protein-protein interaction databases. (b) Pruned network showing only the most highly relevant interaction between ELF4, ABL1 and SRC. Reactome pathways most significantly altered in high-ELF4 tumours belonging to (c) pancreatic adenocarcinomas, (d) lung adenocarcinomas, (e) invasive breast carcinomas, and (f) kidney renal clear cell carcinoma. Refer to S4 File for the complete list of Reactome pathways enriched in these tumours.
Therefore, we used a custom MATLAB script to create the connect network that links ABL1, SRC and ELF4 based on known protein-protein interactions extracted from the Kinase Enrichment Analysis database [27], Chromatin-immunoprecipitation Enrichment Analysis database [28], and UCSC super pathway databases, and Database of Protein, Genetic and Chemical Interactions (BioGrid) [29].
Statistical analyses
All statistical analyses were performed in MATLAB 2020a. Fisher’s exact test was utilised to assess associations between categorical variables. The Welch test for normally distributed data and the Mann-Whitney U-test for non-normally distributed data were used to compare continuous variables. Here, the data distributions were assessed using the Kolmogorov-Smirnov test for goodness of fit [30]. Statistical tests were two-sided and considered significant at p < 0.05 with the Benjamini-Hochberg correction applied where multiple comparisons were involved.
Results
The expression of ELF4 transcript varies across human tumours
We obtained and analysed a TCGA pan-cancer dataset comprising the mRNA expression levels of the ELF4 gene and comprehensively deidentified clinical information. The TCGA collected these datasets from 9,350 patients of 32 distinctive human cancers. We used the z-score normalisation methods to segregate the patient’s tumours into two groups of cancers: those cancers with higher levels of ELF4 (which we named as the "high-ELF4 tumours"; 3,887 samples) and those with a lower level of ELF4 ("low-ELF4 tumours"; 5,463 samples; see Methods sections).
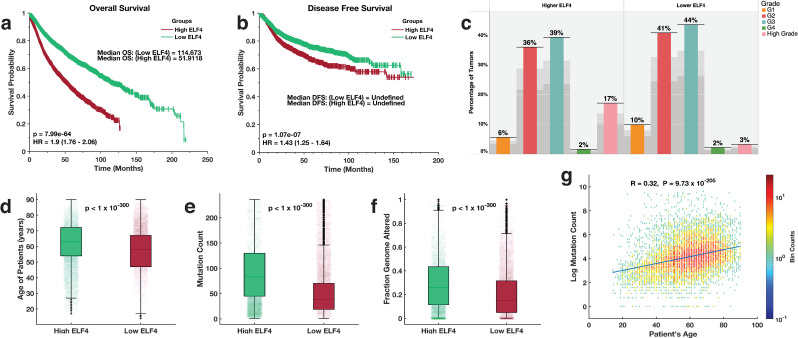
We examined whether the two groups of cancers were associated with different clinical outcomes. Remarkedly, using the Kaplan-Meier method [22], we found that the duration of overall survival (OS) periods for the patients with high-ELF4 tumours (OS = 51.9 months) were significantly shorter (log-rank test; p = 7.99 x 10−64) relative to those of the patients with low-ELF4 tumours (OS = 114.7 months; Fig 1A). Correspondingly, we observed that the disease-free survival (DFS) periods were significantly shorter (log-rank test; p = 1.07 x 10−07) for the patients with high-ELF4 tumours than they were for the patients with low-ELF4 tumours (Fig 1B).
Fig 1.
Kaplan-Meier curve of the overall survival periods (a) and disease-free survival periods (b) of TCGA patients with tumours that expressed high ELF4 and low ELF4 transcript levels. (c) the distribution of various grades tumours derived from 32 human cancer that expressed high ELF4 and low ELF4 transcript levels. Median comparison of the (d) age of the patients (e) number of mutations per patients’ tumours (f) the fraction of the genome altered for each patient tumour between the ELF4-high tumours and ELF4-low tumours. (g) binned scatter plot showing the Pearson’s linear correlation between the age of the patients and the number of mutations in each patient’s tumours. The data points spaced into rectangular bins and each point is coloured based on logarithm bin size with redder colours indicating a higher number of plots. The colour bar shows the colour scale.
Here, these findings expose an association between the expression levels of ELF4 and the clinical outcomes across various cancer types.
Disease factors associated with ELF4 expression
To understand why patients with tumours that express higher levels of ELF4 tended to have worse clinical outcomes (or a more aggressive disease). We assessed the distribution of various tumour grades across the two categories of tumours. Here, we found a significant association between the high-ELF4 tumours (Fisher exact test; odds ratio = 6.1, p = 4.5 x 10−47) with high-grade tumours (Fig 1C).
We found that the median age of the patients with tumours that expressed higher ELF4 was significantly higher (median = 63 years) compared to that of patients with tumours that expressed lower levels of ELF4 (median = 58 years), Wilcoxon rank-sum test (Z = 119.2, p < 1 x 10−300; Fig 1D). We compared the median number of mutations per patient’s tumours across the two groups of disease. Here, we found a higher mutation burden in tumours that expressed higher levels of ELF4 (median = 83 mutations per tumour) than those that expressed lower levels of ELF4 (median = 38 mutations per tumour), Z = 119.2, p < 1 x10-300; Fig 1E. Correspondingly, we found a higher fraction of the genome altered in the high-ELF4 tumours (median = 0.2605 per tumour), than those of the low-ELF4 (median = 0.1499), Z = 200, p < 1 x10-300; Fig 1F.
To further explore the relationship between patients’ age and the mutation load of the tumours afflicting them, we measured the Pearson’s linear correlation coefficients between the patients’ age and the number of mutations found within their tumours. Here, we found that these were significantly positively correlated (Pearson’s correlation = 0.32; p = 9.27 x 10−205; Fig 1D).
Collectively these results show that high-ELF4 tumours, compared to the low-ELF4 tumours, tend to be of a higher-grade, afflict a significantly older patient population and have a significantly higher mutation burden.
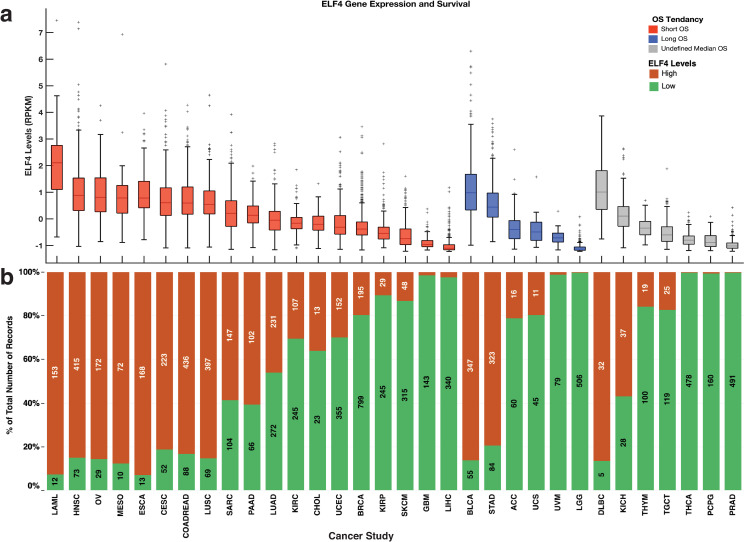
The effect of ELF4 expression varies within cancer-type
Next, we compared the duration of the overall survival periods between patients with tumours that expressed high and low levels of ELF4 across the 32 cancers. Here, for 19 out of 32 cancer types, we found that the overall survival periods were shorter for patients with high-ELF4 tumours than those with low-ELF4 tumours (Fig 2A; S1 File). Among these nineteen cancer types are kidney renal clear cell carcinoma, kidney renal papillary cell carcinoma and liver hepatocellular carcinoma. Surprisingly, for six cancer types, we found that the overall survival periods were longer for patients with high-ELF4 tumours than those afflicted by low-ELF4 tumours. These included, among others, urothelial bladder carcinoma, and adrenocortical carcinoma. For another seven cancer types, including diffuse large B-cell lymphoma and kidney chromophobe, we could not establish the overall influence of the ELF4 expression, as the median OS periods were undefined (i.e., more than 50% of the patients were alive by the reporting time) for both the high-ELF4 cancer patients and the low-ELF4 cancer patients.
Fig 2.
(a) Overall survival comparison within cancer types between patients afflicted with high-ELF4 tumours and those afflicted with low-ELF4 tumours. Compared to the patients with low-ELF4 tumours, the red boxplots indicate median OS durations that are shorter for the patients with high-ELF4 tumours; the blue indicates median OS durations that are longer for the patients with high-ELF4 whereas the grey boxplots indicate median OS periods that are undefined (undefined median DFS period in that > 50% of patients survived beyond the study duration). On each box, the centre mark shows the median, and the left and right edges of the box show the 25th and 75th percentiles, respectively. The whiskers extend to the most extreme data points that are not outliers, and the outliers are shown individually using the ’+’ symbol. (b) shows the percentage of the total number of patients with tumours with each group given the colours of the bars. The number of patients with tumours labels the marks expressed high ELF4 and low ELF4 transcripts. TCGA disease codes and abbreviations: UCEC, uterine corpus endometrial carcinoma; SKCM, skin cutaneous melanoma; BLCA, bladder urothelial carcinoma; UCS, uterine carcinosarcoma; OV, ovarian serous cystadenocarcinoma; LUSC, lung squamous cell carcinoma; STAD, stomach adenocarcinoma; LUAD, lung adenocarcinoma; ESCA, oesophageal adenocarcinoma; DLBC, diffuse large b-cell lymphoma; CESC, cervical squamous cell carcinoma; HNSC, head and neck squamous cell carcinoma; SARC, sarcoma; LIHC, liver hepatocellular carcinoma; BRCA, breast invasive carcinoma; COADREAD, colorectal adenocarcinoma; CHOL, cholangiocarcinoma; ACC, adrenocortical carcinoma; PAAD, pancreatic adenocarcinoma; PRAD, prostate adenocarcinoma; GBM, glioblastoma multiforme; KIRP, kidney renal papillary cell carcinoma; KIRC, kidney renal clear cell carcinoma; MESO, mesothelioma; LGG, brain lower grade glioma; UVM, uveal melanoma; PCPG, pheochromocytoma and paraganglioma; TGCT, testicular germ cell tumours; KICH, kidney chromophobe; THYM, thymoma; LAML, acute myeloid leukaemia; THCA, thyroid carcinoma.
Furthermore, we explored the expression of ELF4 across tumour types across the two pan-cancer groups (high-ELF4 and low-ELF4). We found that ELF4 vary between cancer types, for example, brain lower-grade gliomas (99.9% of the tumours) and prostate adenocarcinomas (99.6%) tended to express lower ELF4 levels, whereas acute myeloid leukaemias (92.7%) and oesophageal adenocarcinomas (92.8%) tended to express higher levels of ELF4 (Fig 2B).
Overall, these findings show that while the expression of ELF4 is associated with increased disease aggressiveness of most cancer types, there are some exceptions.
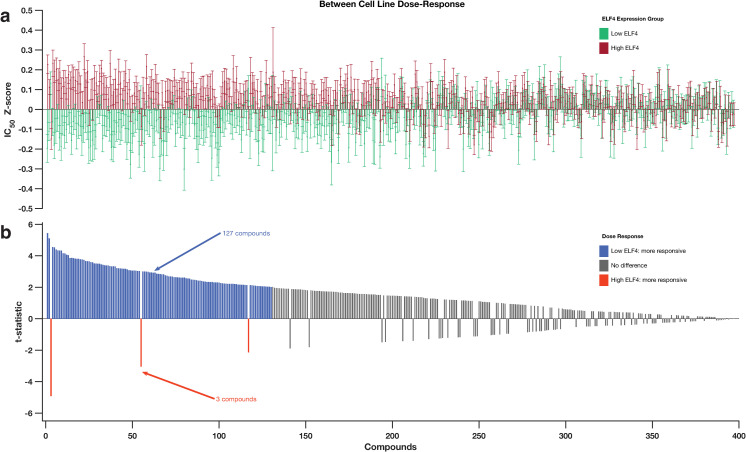
ELF4 expression is associated with significant resistance to most anti-cancer drugs
Since it is virtually impossible to test the primary patients’ tumours that either expressed high or low ELF4 levels to several anti-cancer drugs, we used cancer cell lines to test for any differences in their drug responses. From the GDSC database, we collected the dose-response of 612 cancer cell lines to 397 small molecule inhibitors [16], and their ELF4 mRNA expression levels from the CCLE database [24]. We categorised the cell lines into two groups: 1) those that expressed high ELF4 mRNA transcripts (we refer to these as the "high-ELF4 cell lines") and 2) those that expressed low ELF4 mRNA transcripts (the "low-ELF4 cell lines"; see Methods section). Here, the categories of the cancer cell lines that have ELF4 mRNA levels that correspond to those of cancer cells from the patient groups could be used to examine how ELF4 levels in the patient’s tumour cells are likely to influence the effectiveness of particular anti-cancer drugs.
Therefore, we compared drug z-score normalised half-maximal inhibitory concentration (IC50) values between the two categories of cells for 397 anti-cancer drugs. Remarkedly, we uncovered differences between the high-ELF4 cell lines and low-ELF4 cell lines in their observed dose-response to 130 drugs (Fig 3A).
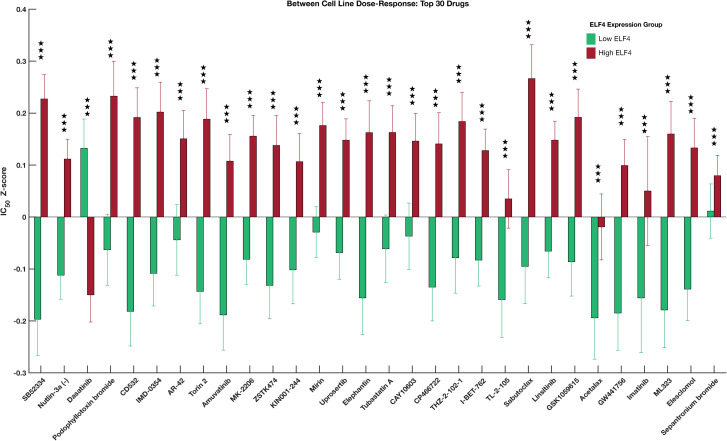
Fig 3.
(a) Comparison of the dose-response profiles between the GDSC cancer cell lines that express higher ELF4 and those that express lower ELF4 transcript. The bar graphs show the logarithm IC50 values of the cancer cell lines that correspond to those that express higher ELF4 (red bars) and express lower ELF4 (green bar). (b) bar graph shows the t-value calculated using the Welch test for each of the 397 anti-cancer drugs used to profile the dose-response of the cell lines by the GDSC. The drugs along the columns are matched to the columns in the top plots. The orange bars indicate the drug to which the high-ELF4 cell lines are significantly more responsive; the blue bars indicate drug to which the low-ELF4 cell lines are significantly more responsive. The grey bars show drugs for which we found a non-statistically significant difference in the responsive between the high-ELF4 cell lines and low-ELF4 cell lines. For details refer to S2 File.
Compared to the high-ELF4 cell lines, the low-ELF4 cell lines were significantly more sensitive to 127 anticancer drugs, including SB52334 (Welch test; p = 9.76 x 10−08), Nutlin-3a (p = 4.13 x 10−07), and CD532 (p = 7.53 x 10−06) (Fig 3B; S2 File). Astoundingly, the high-ELF4 cell lines were only significantly more sensitive than the low-ELF4 cell lines to three anti-cancer drugs: dasatinib (p = 1.16 x 10−06), WH-4-023 (p = 0.0027) and Ponatinib (p = 0.034), all of which target the proto-oncogene tyrosine-protein kinase SRC and tyrosine-protein kinase ABL1 (Fig 3B; S2 File). Furthermore, among the top thirty ranked significant anti-cancer drugs, the high-ELF4 cell lines were only significantly more sensitive (p = 1.16 x 10−06) than low-ELF4 cell lines to dasatinib; one anti-cancer drug (Fig 4).
Fig 4. Top 30 drugs that showed the highest statistically significant dose-response differences between high-ELF4 cell lines and the low-ELF4 cell lines.
The error bars show the standard error of the median logarithm IC50 value for each anti-cancer drug. The three stars show the degrees of statistical significance, i.e., p-values less than 0.001. For details, see S2 File.
Here, our results indicate that the expression of ELF4 does not only detectably impact the clinical outcomes of the patients but might also be a relevant variable to predict the response of tumours to various anti-cancer agents.
To elucidate the mechanism by which dasatinib, WH-4-023, and Ponatinib may regulate ELF4, we constructed a prior-knowledge network that connects ABL1, SRC and ELF4 (Fig 5A). Here, we found that ELF4 acts downstream of ABL1 and SRC, with MDM2, PML, TP63 and CDK2 acting as intermediary signalling proteins (Fig 5B).
Furthermore, we attempted to determine whether any signalling pathways were enriched for among the overexpressed genes of pancreatic adenocarcinomas (PAAD), kidney renal clear cell carcinoma (KIRC), breast invasive carcinoma (BRCA) and lung adenocarcinomas (LUAD) that expressed higher ELF4 compare to those that expressed lower ELF4 (see S3 File). Here, astoundingly, we found that the over-expressed genes in high-ELF4 tumours of PAAD, KIRC, BRCA and LUAD tumours were all enriched for, pathways associated with 1) Defective C1GALT1C1 causes Tn polyagglutination syndrome, 2) Defective GALNT12 causes colorectal cancer 3), Defective GALNT3 causes familial hyperphosphatemic tumoral calcinosis, 4) O-linked glycosylation of mucins Homo sapiens, 5) Termination of O-glycan biosynthesis (Fig 5C–5F, also see S4 File). These results corroborate published observations that link aberrant glycosylation to the increased resistance of cancer cell to drug perturbation [31–33].
Discussion
We examined the relationship between the mRNA expression level ELF4 in thousands of primary tumours and cancer cell lines of 32 different cancer types and both the clinical outcomes and likely anti-cancer drug responses. Others have studied ELF4 in the context of tumorigenesis in cancers of the skin, breast and prostate [3, 10, 12, 13]. To the best of our knowledge, our study is the first to characterise the consequences of ELF4 expression variations across many distinct cancer types based on such many (9,350) primary tumours.
We showed that clinically relevant subtypes of patient tumours, across many cancer types, could be achieved by simply dividing the tumours into two categories based entirely on the expression of ELF4: those tumours which express high ELF4 levels and those that express low ELF4 levels. Just as others have shown that the expression of various genes, including kinases such as the phosphoinositide 3-kinase and transcription factors such as p53, can have clinical implications [34–38], we show here that patients with low-ELF4 tumours tend to have significantly better clinical outcomes than patients with high-ELF4 tumours. Our results suggest that the tumour’s ELF4 expression levels are directly correlated with the aggressiveness of cancer.
Our analyses indicate that high-ELF4 tumours are typical among the elderly, and these also tend to have a higher mutation load (Fig 1D–1F). The frequency of somatic mutations increases with age in both non-cancerous and cancer tissue [39–42]; therefore we suggest that the link between the expression of ELF4 and the mutation burden could be exploited to establish therapeutics that are more effective in treating specific cancers. Whereas ELF4 is virtually undruggable, we could employ a network analysis approach to identify the upstream regulatory proteins that could be targeted to treat tumours that overexpress ELF4 [43, 44]. Furthermore, tumours with higher mutations are more aggressive and respond significantly poorly to most anti-cancer drugs [45]. Accordingly, compared to the low-ELF4 tumours, we discovered higher gene mutation rates in high-ELF4 tumours, which could explain the poorer outcome exhibited by the patients afflicted with high-ELF4 tumours. Put together; we suggest that a combination of factors including the higher-grade tumours, higher mutation burden and the older patient population may in part explain why patients afflicted with high-ELF4 tumours level have worse survival outcomes.
There is a link between the expression of specific genes in cancer cells and the variations in the response of these cells to drug perturbation, and expression levels of these genes can, thus, impact disease treatment outcomes [24, 46–50]. With the advent of personalised medicine, growingly, the aim is to guesstimate the drugs to which a tumour is most likely responsive [51, 52]. Here, to surmount the impractical barrier of testing hundreds of individual drugs on a specific tumour, cell lines that have genetic features resembling that of the tumour are convenient in inferring the drug responses of that tumour [16, 24, 53, 54]. Suitably, by probing the drug response profiles of cancer cell lines, we showed that high-ELF4 tumours and low-ELF4 tumours perhaps respond differently to many anti-cancer drugs. More specifically, compared to the low-ELF4 tumours, the high-ELF4 tumours tended to be significantly responsive to only three (dasatinib, WH-4-023, Ponatinib) drugs out of 397 anti-cancer drugs. Since both, dasatinib and ponatinib also target ABL kinase, and dasatinib, WH-4-023, Ponatinib target the SRC kinase, our finding reveals that the high-ELF4 cancers are likely to signal through SRC and ABL kinases.
Our hypothesis is supported by previous studies that show that the loss of ELF4 causes a profound abrogation in BCR-ABL associated Chronic Myeloid Leukemia [20] and the direct interaction between the Promyelocytic Leukemia (PML) gene and ELF4 [55]. Furthermore, our analysis of the prior knowledge network that connected the SRC and ABL kinases to ELF4 showed that MDM2, PML and TP63 are the likely intermediary proteins that link these kinases to ELF4 [55, 56]. Here, we suggest that many other cellular proteins interact with ELF4, but these interactions remain unknown since ELF4 is not as extensively studied (25 known interactors in the BioGrid database) as other proteins such as p53 (3077 known interactors) and c-MYC (7,325 known interactors) [29]. Therefore, many more experiments and computational analyses are required to elucidate the various pathways and mechanism by which SRC and ABL1 affect the activity of ELF4.
This finding implies that in aside the high-ELF4 tumours being significantly aggressive than low-EFL4 tumours, the high-ELF4 tumour patients may also exhibit worse clinical outcomes merely due to the refractory nature of the high-ELF4 tumours to most anti-cancer drugs. Additionally, since refractory tumours require more aggressive treatment protocols with higher drug doses, it would follow that patients with high-ELF4 tumours are likely to be exposed to such treatments, thus would tend to experience more adverse drug effects that might unfavourably impact their survival [57–60].
Conclusion
Altogether, we have shown that expression of ELF4 varies across tumours of the 32 cancer types investigated and that there is a link between the expression levels of ELF4 in tumours to the age of patients, the mutation burden, and the clinical outcomes. Further, our analyses of the dose-response profiles of well-characterised cell lines have revealed that the expression levels of ELF4 in tumours may be related to the varied responses of the cancer cell to drug perturbation, a finding that could help shape precision medicine.
Supporting information
Within cancer types comparisons of the duration, the overall survival for patients with tumours that express high ELF4 and expressed low ELF4 expression levels.
(XLSX)
(XLSX)
The Sheets with this Microsoft Excel file are names as follows: Cancer-all (e.g., PAAD-all): the differential gene expression results of all the genes between tumours that express high-ELF4 and low ELF4. Cancer-highELF4 Up Genes (e.g., PAAD-highELF4 Up Genes): all the significantly up-regulated genes in the high-ELF4 tumours of that cancer. Cancer-lowELF4 Up Genes ((e.g., PAAD-highELF4 Up Genes) shows the up-regulated genes in the low-ELF4 tumours.
(XLSX)
The Sheets within this Microsoft Excel file are named accordingly.
(XLSX)
Data Availability
The data that support the findings of this study are available from the following repositories: cBioPortal (https://www.cbioportal.org/), Genomics of Drug Sensitivity in Cancer (https://www.cancerrxgene.org/), and the Cancer Cell Line Encyclopaedia (https://portals.broadinstitute.org/ccle/).
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Pavlova NN, Thompson CB. The Emerging Hallmarks of Cancer Metabolism. Cell Metab 2016;23:27–47. 10.1016/j.cmet.2015.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hanahan D, Weinberg RA. Hallmarks of cancer: The next generation. vol. 144. Elsevier; 2011. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 3.Suico MA, Shuto T, Kai H. Roles and regulations of the ETS transcription factor ELF4/MEF. J Mol Cell Biol 2017;9:168–77. 10.1093/jmcb/mjw051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kosti A, Du L, Shivram H, Qiao M, Burns S, Garcia JG, et al. ELF4 is a target of miR-124 and promotes neuroblastoma proliferation and undifferentiated state. Mol Cancer Res 2020;18:68–78. 10.1158/1541-7786.MCR-19-0187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suico MA, Fukuda R, Miyakita R, Koyama K, Taura M, Shuto T, et al. The transcription factor MEF/Elf4 is dually modulated by p53-MDM2 axis and MEF-MDM2 autoregulatory mechanism. J Biol Chem 2014;289:26143–54. 10.1074/jbc.M114.580209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nguyen D-T, Mathias S, Bologa C, Brunak S, Fernandez N, Gaulton A, et al. Pharos: Collating protein information to shed light on the druggable genome. Nucleic Acids Res 2017;45:D995–1002. 10.1093/nar/gkw1072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hsing M, Wang Y, Rennie PS, Cox ME, Cherkasov A. ETS transcription factors as emerging drug targets in cancer. Med Res Rev 2020;40:413–30. 10.1002/med.21575 [DOI] [PubMed] [Google Scholar]
- 8.Sashida G, Bazzoli E, Menendez S, Stephen D. N. The oncogenic role of the ETS transcription factors MEF and ERG. Cell Cycle 2010;9:3457–9. 10.4161/cc.9.17.13000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ando K, Tsushima H, Matsuo E, Horio K, Tominaga-Sato S, Imanishi D, et al. Mutations in the nucleolar phosphoprotein, nucleophosmin, promote the expression of the oncogenic transcription factor MEF/ELF4 in leukemia cells and potentiates transformation. J Biol Chem 2013;288:9457–67. 10.1074/jbc.M112.415703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sashida G, Liu Y, Elf S, Miyata Y, Ohyashiki K, Izumi M, et al. ELF4/MEF Activates MDM2 Expression and Blocks Oncogene-Induced p16 Activation To Promote Transformation. Mol Cell Biol 2009;29:3687–99. 10.1128/MCB.01551-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sze KM, Ho DW, Chiu Y, Tsui Y, Chan L, Lee JM, et al. HBV‐ TERT Promoter Integration Harnesses Host ELF4 Resulting in TERT Gene Transcription in Hepatocellular Carcinoma. Hepatology 2020:hep.31231. 10.1002/hep.31231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aier I, Khan SM. Exploring the Effect of Wild Type and Mutant ELF4 Transcriptional Factor on Oral Cancer Using High-Throughput Sequencing Data. Int. Conf. Bioinforma. Syst. Biol. BSB 2018, Institute of Electrical and Electronics Engineers Inc.; 2018, p. 207–11. 10.1109/BSB.2018.8770545 [DOI] [Google Scholar]
- 13.Budka JA, Ferris MW, Capone MJ, Hollenhorst PC. Common ELF1 deletion in prostate cancer bolsters oncogenic ets function, inhibits senescence and promotes docetaxel resistance. Genes and Cancer 2018;9:198–214. 10.18632/genesandcancer.182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinstein JN, Collisson EA, Mills GB, Mills Shaw KR, Ozenberger BA, Ellrott K, et al. The Cancer Genome Atlas Pan-Cancer analysis project. Nat Publ Gr 2013;45. 10.1038/ng.2764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang J, Baran J, Cros A, Guberman JM, Haider S, Hsu J, et al. International Cancer Genome Consortium Data Portal—a one-stop shop for cancer genomics data. Database (Oxford) 2011;2011:bar026. 10.1093/database/bar026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kafita D, Nkhoma P, Zulu M, Sinkala M. Proteogenomic Analysis of Pancreatic Cancer Subtypes. BioRxiv 2020:2020.04.13.039834. 10.1101/2020.04.13.039834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Y, Xu X, Maglic D, Dill MT, Mojumdar K, Ng PK-S, et al. Comprehensive Molecular Characterization of the Hippo Signaling Pathway in Cancer. Cell Rep 2018;25:1304–1317.e5. 10.1016/j.celrep.2018.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanchez-Vega F, Mina M, Armenia J, Chatila WK, Luna A, La KC, et al. Oncogenic Signaling Pathways in The Cancer Genome Atlas. Cell 2018;173:321–337.e10. 10.1016/j.cell.2018.03.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinkala M, Mulder N, Patrick Martin D. Metabolic gene alterations impact the clinical aggressiveness and drug responses of 32 human cancers. Commun Biol 2019;2. 10.1038/s42003-019-0666-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sinkala M, Zulu M, Nkhoma P, Kafita D, Zulu E, Tembo R, et al. A Systems Approach Identifies Key Regulators of HPV-Positive Cervical Cancer. MedRxiv 2020:2020.05.12.20099424. 10.1101/2020.05.12.20099424 [DOI] [Google Scholar]
- 21.Chang K, Creighton CJ, Davis C, Donehower L, Drummond J, Wheeler D, et al. The Cancer Genome Atlas Pan-Cancer analysis project. Nat Genet 2013;45:1113–20. 10.1038/ng.2764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goel MK, Khanna P, Kishore J. Understanding survival analysis: Kaplan-Meier estimate. Int J Ayurveda Res 2010;1:274–8. 10.4103/0974-7788.76794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hollander M, Wolfe D, Chicken E. Nonparametric statistical methods. 2013. [Google Scholar]
- 24.Barretina J, Caponigro G, Stransky N, Venkatesan K, Margolin AA, Kim S, et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature 2012;483:603–7. 10.1038/nature11003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brooks AN, Yang L, Duff MO, Hansen KD, Park JW, Dudoit S, et al. Conservation of an RNA regulatory map between Drosophila and mammals. Genome Res 2011;21:193–202. 10.1101/gr.108662.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mortazavi A, Williams BA, McCue K, Schaeffer L, Wold B. Mapping and quantifying mammalian transcriptomes by RNA-Seq. Nat Methods 2008;5:621–8. 10.1038/nmeth.1226 [DOI] [PubMed] [Google Scholar]
- 27.Lachmann A, Ma’ayan A. KEA: kinase enrichment analysis. Bioinformatics 2009;25:684–6. 10.1093/bioinformatics/btp026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lachmann A, Xu H, Krishnan J, Berger SI, Mazloom AR, Ma’ayan A. ChEA: transcription factor regulation inferred from integrating genome-wide ChIP-X experiments. Bioinformatics 2010;26:2438–44. 10.1093/bioinformatics/btq466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oughtred R, Stark C, Breitkreutz B-J, Rust J, Boucher L, Chang C, et al. The BioGRID interaction database: 2019 update. Nucleic Acids Res 2019;47:D529–41. 10.1093/nar/gky1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Massey FJ. The Kolmogorov-Smirnov Test for Goodness of Fit. J Am Stat Assoc 1951;46:68–78. 10.1080/01621459.1951.10500769 [DOI] [Google Scholar]
- 31.Hung JS, Huang J, Lin YC, Huang MJ, Lee PH, Lai HS, et al. C1GALT1 overexpression promotes the invasive behavior of colon cancer cells through modifying o-glycosylation of FGFR2. Oncotarget 2014;5:2096–106. 10.18632/oncotarget.1815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bakos É, Hegedüs T, Holló Z, Welker E, Tusnády GE, Zaman GJR, et al. Membrane topology and glycosylation of the human multidrug resistance-associated proteins. J Biol Chem 1996;271:12322–6. 10.1074/jbc.271.21.12322 [DOI] [PubMed] [Google Scholar]
- 33.Very N, Lefebvre T, El Yazidi-Belkoura I. Drug resistance related to aberrant glycosylation in colorectal cancer. Oncotarget 2018;9:1380–402. 10.18632/oncotarget.22377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang J, Nie J, Ma X, Wei Y, Peng Y, Wei X. Targeting PI3K in cancer: Mechanisms and advances in clinical trials. Mol Cancer 2019;18:1–28. 10.1186/s12943-018-0930-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamaguchi S, Takahashi S, Mogushi K, Izumi Y, Nozaki Y, Nomizu T, et al. Molecular and clinical features of the TP53 signature gene expression profile in early-stage breast cancer. Oncotarget 2018;9:14193–206. 10.18632/oncotarget.24447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim JY, Lee E, Park K, Park WY, Jung HH, Ahn JS, et al. Clinical implications of genomic profiles in metastatic breast cancer with a focus on TP53 and PIK3CA, the most frequently mutated genes. Oncotarget 2017;8:27997–8007. 10.18632/oncotarget.15881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang X, Liu L, Yang X, Wang L, Zhang C, Hu Y. Expression of TP53 and IL-1a in unicystic ameloblastoma predicts the efficacy of marsupialization treatment. Med (United States) 2018;97. 10.1097/MD.0000000000009795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sinkala M, Mulder N, Patrick Martin D. Metabolic gene alterations impact the clinical aggressiveness and drug responses of 32 human cancers. Commun Biol 2019;2. 10.1038/s42003-019-0666-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martincorena I, Fowler JC, Wabik A, Lawson ARJ, Abascal F, Hall MWJ, et al. Somatic mutant clones colonize the human esophagus with age. Science (80-) 2018;362:911–7. 10.1126/science.aau3879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kang E, Wang X, Tippner-Hedges R, Ma H, Folmes CDL, Gutierrez NM, et al. Age-related accumulation of somatic mitochondrial DNA mutations in adult-derived human ipscs. Cell Stem Cell 2016;18:625–36. 10.1016/j.stem.2016.02.005 [DOI] [PubMed] [Google Scholar]
- 41.Helgadottir HT. Somatic mutations in healthy cells and age-associated diseases. Inst för biovetenskaper och näringslära / Dept of Biosciences and Nutrition; 2019. [Google Scholar]
- 42.Mason CC, Khorashad JS, Tantravahi SK, Kelley TW, Zabriskie MS, Yan D, et al. Age-related mutations and chronic myelomonocytic leukemia. Leukemia 2016;30:906–13. 10.1038/leu.2015.337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hagenbuchner J, Ausserlechner MJ. Targeting transcription factors by small compounds—Current strategies and future implications. Biochem Pharmacol 2016;107:1–13. 10.1016/j.bcp.2015.12.006 [DOI] [PubMed] [Google Scholar]
- 44.Masamoto Y, Kurokawa M. Targeting chronic myeloid leukemia stem cells: can transcriptional program be a druggable target for cancers? Stem Cell Investig 2018;5. 10.21037/sci.2018.03.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Samstein RM, Lee CH, Shoushtari AN, Hellmann MD, Shen R, Janjigian YY, et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet 2019;51:202–6. 10.1038/s41588-018-0312-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Geeleher P, Cox NJ, Huang R. Clinical drug response can be predicted using baseline gene expression levels and in vitro drug sensitivity in cell lines. Genome Biol 2014;15:R47. 10.1186/gb-2014-15-3-r47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iorio F, Knijnenburg TA, Vis DJ, Bignell GR, Menden MP, Schubert M, et al. A Landscape of Pharmacogenomic Interactions in Cancer. Cell 2016;166:740–54. 10.1016/j.cell.2016.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sinkala M, Mulder N, Martin D. Machine Learning and Network Analyses Reveal Disease Subtypes of Pancreatic Cancer and their Molecular Characteristics. Sci Rep 2020;10:1–14. 10.1038/s41598-020-58290-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ghandi M, Huang FW, Jané-Valbuena J, Kryukov G V., Lo CC, McDonald ER, et al. Next-generation characterization of the Cancer Cell Line Encyclopedia. Nature 2019. 10.1038/s41586-019-1186-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang L, Li X, Zhang L, Gao Q. Improved anticancer drug response prediction in cell lines using matrix factorization with similarity regularization. BMC Cancer 2017;17:513. 10.1186/s12885-017-3500-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bauer DC, Gaff C, Dinger ME, Caramins M, Buske FA, Fenech M, et al. Genomics and personalised whole-of-life healthcare. Trends Mol Med 2014;20:479–86. 10.1016/j.molmed.2014.04.001 [DOI] [PubMed] [Google Scholar]
- 52.Ma’ayan A, Rouillard AD, Clark NR, Wang Z, Duan Q, Kou Y. Lean Big Data integration in systems biology and systems pharmacology. Trends Pharmacol Sci 2014;35:450–60. 10.1016/j.tips.2014.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Diaz-Moralli S, Tarrado-Castellarnau M, Miranda A, Cascante M. Targeting cell cycle regulation in cancer therapy. Pharmacol Ther 2013;138:255–71. 10.1016/j.pharmthera.2013.01.011 [DOI] [PubMed] [Google Scholar]
- 54.Menden MP, Iorio F, Garnett M, McDermott U, Benes CH, Ballester PJ, et al. Machine Learning Prediction of Cancer Cell Sensitivity to Drugs Based on Genomic and Chemical Properties. PLoS One 2013;8:e61318. 10.1371/journal.pone.0061318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Suico MA, Yoshida H, Seki Y, Uchikawa T, Lu Z, Shuto T, et al. Myeloid Elf-1-like Factor, an ETS Transcription Factor, Up-regulates Lysozyme Transcription in Epithelial Cells through Interaction with Promyelocytic Leukemia Protein. J Biol Chem 2004;279:19091–8. 10.1074/jbc.M312439200 [DOI] [PubMed] [Google Scholar]
- 56.Suico MA, Fukuda R, Miyakita R, Koyama K, Taura M, Shuto T, et al. The transcription factor MEF/Elf4 is dually modulated by p53-MDM2 axis and MEF-MDM2 autoregulatory mechanism. J Biol Chem 2014;289:26143–54. 10.1074/jbc.M114.580209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Silver JK, Baima J. Cancer Prehabilitation. Am J Phys Med Rehabil 2013;92:715–27. 10.1097/PHM.0b013e31829b4afe [DOI] [PubMed] [Google Scholar]
- 58.Postow MA, Sidlow R, Hellmann MD. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N Engl J Med 2018;378:158–68. 10.1056/NEJMra1703481 [DOI] [PubMed] [Google Scholar]
- 59.Epstein JB, Thariat J, Bensadoun R-J, Barasch A, Murphy BA, Kolnick L, et al. Oral complications of cancer and cancer therapy. CA Cancer J Clin 2012;62:400–22. 10.3322/caac.21157 [DOI] [PubMed] [Google Scholar]
- 60.Ranpura V, Hapani S, Wu S. Treatment-Related Mortality With Bevacizumab in Cancer Patients. JAMA 2011;305:487. 10.1001/jama.2011.51 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Within cancer types comparisons of the duration, the overall survival for patients with tumours that express high ELF4 and expressed low ELF4 expression levels.
(XLSX)
(XLSX)
The Sheets with this Microsoft Excel file are names as follows: Cancer-all (e.g., PAAD-all): the differential gene expression results of all the genes between tumours that express high-ELF4 and low ELF4. Cancer-highELF4 Up Genes (e.g., PAAD-highELF4 Up Genes): all the significantly up-regulated genes in the high-ELF4 tumours of that cancer. Cancer-lowELF4 Up Genes ((e.g., PAAD-highELF4 Up Genes) shows the up-regulated genes in the low-ELF4 tumours.
(XLSX)
The Sheets within this Microsoft Excel file are named accordingly.
(XLSX)
Data Availability Statement
The data that support the findings of this study are available from the following repositories: cBioPortal (https://www.cbioportal.org/), Genomics of Drug Sensitivity in Cancer (https://www.cancerrxgene.org/), and the Cancer Cell Line Encyclopaedia (https://portals.broadinstitute.org/ccle/).