Abstract
Background
Post-stroke spasm is currently a complex clinical problem that remains to be resolved. Due to its excellent efficacy and few side effects, clinicians have used fire acupuncture to treat post-stroke spasticity in China.
Objectives
The purpose of this study was to evaluate the clinical efficacy of fire acupuncture compared with conventional acupuncture to treat post-stroke spasms and provide a detailed summary of the commonly used acupoints.
Methods
Eight databases (MEDLINE/PubMed, Web of Science, the Cochrane database, EMBASE, CBM, CNKI, WanFang, and VIP) were searched for randomized controlled trials (RCTs) published from database inception through August 30, 2020. RCTs that compared fire acupuncture with conventional acupuncture as a treatment intervention for patients with spasticity after stroke were included. Revman 5.3 software was used to calculate risk ratios (RR) and standard mean differences (SMD) with 95% confidence intervals (CI). Methodological evaluation or critical appraisal of the included articles was assessed using RoB-2.
Results
Sixteen studies with a total of 1,118 patients were included. Although according to the standards of the Rob 2.0 tool, most studies are considered to have some problems. Comprehensive analysis of the results revealed a consistent trend indicating several advantages of using fire needles compared to conventional acupuncture in treating post-stroke spasms, including the effective rate, recovery rate, and improvement of multiple scales represented by MAS. Concerning secondary outcomes, using the scales of FMA, BI, or NDS in this random model meta-analysis, fire acupuncture exhibited better performance compared to acupuncture [SMD = 2.27, 95%CI [1.40,3.13 (random-effects model) ], [SMD = 1.46,95% CI [1.03,1.90 (random-effects model)], and [SMD = 0.90, 95%CI [0.44,1.35 (random-effects model)], respectively, with moderately high heterogeneity. When the effective rate was used as an outcome in the subgroup analysis, fire needles performed better than conventional acupuncture with respect to damage to the upper or lower limbs, and the thickness and depth of acupuncture. When the modified Ashworth scale (MAS) was used as the outcome, and the damage occurred in the lower extremity, the acupuncture depth exceeded 15mm, or the duration of stroke was longer than six months, the fire needles did not perform better than conventional acupuncture, [SMD = 0.01, 95%CI [-0.47,0.48 (fix-effects model)], [SMD = 0.21 [-0.51,0.93(random-effects model)], and [SMD = 0.76, 95%CI [-0.08,1.60 (random-effects model)], respectively. The acupoints identified with the highest frequencies in this study were Yang-meridian, including LI11-Quchi (nine times), LI4-Hegu (seven times), and ST36-Zusanli (five times). Moreover, no serious adverse effects were reported in any of the studies included in this analysis.
Conclusions
Despite several limitations, this was the first meta-analysis to focus on the treatment of post-stroke spasticity using fire needle acupuncture compared with conventional acupuncture. Our results confirmed that fire needles could provide a better clinical effect than conventional acupuncture, which will help standardize fire needle treatment strategies for post-stroke spasms.
Introduction
Stroke is a major public health problem and ranked as the most common cause of disability [1]. Although recent medical advances have reduced stroke to the fourth cause of death worldwide [2], it still represents a condition that results in devastating physical disability, particularly due to the presence of spasticity [3]. Stroke is the primary cause of death in China [4, 5], and the most common post-stroke complication is spasticity [6]. The prevalence of post-stroke spasticity ranges from 30% to 80% in stroke survivors [7], with a 90% probability of occurrence approximately three weeks after a stroke event [8, 9].
Spasticity is a motor disorder associated with lesions of the central nervous system (CNS) that provoke different clinical syndromes, including spasms, clonus, or hypertonia. It is noteworthy that spasticity is associated with reduced functional independence and a fourfold increase in direct care costs during the first year after stroke [10]. Several therapeutic approaches have been proposed to manage spasticity, including central muscle relaxants (baclofen and baclosan) and peripheral muscle relaxants (xeomi) [11–14]. Although medications can relieve the spasms, the relief is not long-lasting, and severe side effects are associated with long-term use of these drugs, including cardiac arrhythmia, hyperkalemia, and amyostasia. These adverse side-effects must be taken into consideration, particularly with elderly patients. Therefore, current studies are focused on identifying alternative treatment strategies, including conventional acupuncture and fire acupuncture. These alternative treatment strategies are prevalent in China and have been incorporated into clinical practice.
Some evidence suggests that acupuncture (including electroacupuncture) could reduce spasticity associated with other CNS diseases [15]. The fire needle is an important component of acupuncture. Due to their excellent curative effect and reduced side effects, fire needles have been used recently by clinicians in China to treat post-stroke spasticity. The efficacy of acupuncture is widely recognized. It has been used to resolve functional recovery problems after CNS injury for many years in Asian countries and is increasingly popular in western countries [15]. However, the general knowledge of fire needles around the world is still insufficient. Additionally, the results of studies on the comparative effectiveness of fire needles and conventional acupuncture in treating spasticity in stroke survivors have been variable. Therefore, it was necessary to conduct a systematic review and meta-analysis of the existing literature to objectively evaluate the clinical efficacy and safety of fire acupuncture for spasms after stroke.
Methods
This systematic review and meta-analysis was registered in the PROSPERO database at http://www.crd.york.ac.uk/PROSPERO(CRD42020188959) and followed the guidelines provided by the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement [16].
The elaboration of the scientific question was based on the PICO strategy [17] considering:
P- Participants/population: Patients diagnosed with limb cramps after stroke will be focused on. No restrictions on gender, age, and ethnicity.
I- intervention(s):Intervention groups are treated with fire needle alone.
C- Comparator(s)/control: The control group used acupuncture instead of fire needle on the basis of any type of acupuncture type
O- Outcome(s): The main outcome indicators included the effective rate (ER), recovery rate (RR), and the modified Ashworth scale (MAS). Secondary outcomes: The secondary outcome indicators included one of the following, Fugl-Meyer (FMA), Barthel Index (BI), and Neurological Function Deficit Scale (NDS).
Data sources and search strategies
Eight databases (MEDLINE/PubMed, Web of Science, the Cochrane database, EMBASE, CBM, CNKI, WanFang, and VIP) were searched for RCTs published from the database inception through August 2020. Various combinations of Medical Subject Headings (MeSH) and non-MeSH terms were used, including “fire needle,” “red-hot needle,” “heated needle,” “needle,” “acupuncture,” “acupotomy,” “stroke,” "cerebrovascular accident,” “spasm,” “paraparesis,” “spastic,” and "spasticity after stroke,” which were searched individually or in combination. Language, study population, or country restrictions were not applied. Moreover, we examined other relevant medical journals and magazines to identify literature not included in the electronic databases. The specific search strategy is provided in the S1 Appendix.
Criteria for inclusion and exclusion
Criteria for inclusion
Studies that met the following conditions were enrolled in the analysis. The studies covered patients diagnosed with stroke and did not take muscle relaxants or have increased muscle tone. The experimental group only used fire acupuncture as the intervention, while the control group was treated with conventional acupuncture or electroacupuncture. The type, thickness, and procedure used for fire acupuncture were not limited. The main outcome indicators included the effective rate, recovery rate, and scales used to assess the degree of spasticity of the extremities. The scales used to assess daily living activities and neurological deficits were used as the secondary outcome indicators. There was no restriction on age, gender, course of the disease, and treatment location. The language of the published research was not limited.
Criteria for exclusion
Studies were excluded based on the following conditions. Fire acupuncture was combined with other treatment methods, including traditional Chinese medicine, blood puncture, rehabilitation, Chinese herbal (patent) medicine, or other treatments in the intervention group. The control group, which was acupuncture or electroacupuncture, was combined with other complex therapies. The patients exhibited increased muscle tone caused by other diseases. Others exclusion criteria that were used included whether the study was retrospective, a review, or a case report, the patient baseline data were inconsistent the study used inappropriate random sequence generation methods, conference papers, or data were missing from the report with no reply from the corresponding author(s).
Data collection, extraction, and management
A piloted data extraction form that has been discussed and developed by all the reviewers was assessed and extracted independently by two authors (QX and ZSM). A standardized form was used to extract data, including general information, study characteristic, participant characteristic, interventions characteristics, outcomes and so on. Any disagreement in data extraction was resolved by discussion or negotiation with a third arbitrator (ZWF). The data included in the study were extracted according to a pre-designed standardized table, including the first author, publication date, and treatment location. The patient information included age, course of the disease, gender, and sample size. The intervention information included selection and depth of acupuncture points, materials used for acupuncture, treatment frequency, adverse events, and whether follow-up examinations occurred. If the data are incomplete or other problems are encountered during data extraction, we contacted the author by phone or e-mail for additional information. Each eligible trial was assigned to a study ID in the following formats: the name of the first author + space + year of publication (e.g, Wang T 2019).
Risk of bias assessment
The Cochrane Handbook for Systematic Reviews(RoB-2) was used to evaluate all studies in this analysis to determine the bias associated with each study. RoB 2 [18] -a revised Cochrane tool assessing risk of bias arising from five domains in randomised trials:(1) the randomisation process, (2)deviations from the intended interventions,(3) missing outcome data, (4) measurement of the outcome, (5) and selection of the reported result. Each domain a risk of bias (low risk, some concerns, or high risk) based on the domain algorithm, and made an overall judgment (low risk, some concerns or high risk) using the described criteria. According to RoB 2, risk-of-bias judgments for each domain have the following categories: low risk of bias, some concerns, or high risk of bias. Judgments are based on and summarise the answers to signalling questions. interior agreement will be assessed for each domain of bias and for the overall RoB judgement by juding Fleiss’s Kappa scores [19, 20]. 44 45 We will group agreement as poor (0.00), slight (0.01–0.20), fair (0.21–0.40), moderate (0.41–0.60), substantial (0.61–0.80) or almost perfect (0.81–1.00) [21].
The STRICTA checklist was used to evaluate the quality of the research. The funnel chart was used to analyze potential publication bias.
Data synthesis
All analyses were conducted with Review Manager V.5.3 software and Stata. If a meta-analysis is not possible, we provided a narrative summary of the results from individual studies. The relative risk (RR) was used to analyze dichotomous outcomes. The mean difference (MD) was used to analyze continuous outcomes with the same unit. Otherwise, the standardized mean difference (SMD) was used. The uncertainty was expressed with 95% confidence intervals (95%CI). We measured heterogeneity using the I2 statistic. Fixed-effects model was used if heterogeneity is found. Random effect model was used where significant statistical heterogeneity exists. Heterogeneity was further explored using meta-regression with backward elimination to analyze the associations between treatment effect and the participant characteristics. Funnel plot was used to examine the potential for publication bias. We judged heterogeneity based on the p-value. When the I2 was less than or equal to 50%, we determined that the heterogeneity was within an acceptable range, and adopted a fixed-effect model for the meta-analysis. We concluded that the heterogeneity was high if the I2 is greater than 50% and used a random-effect model for data analysis. If the number of studies included in the analysis is sufficient, subgroup analysis was used to determine heterogeneity. If the number of included articles exceeds 10, we thought that meta regression can be used to find the source of the heterogeneity.
Outcome measures
Primary outcomes
The main outcome indicators included the effective rate (ER), recovery rate (RR), and the modified Ashworth scale (MAS). The ER and RR reflected the improvement before and after treatment. The MAS is considered to be an important tool to assess spasticity after stroke. The scale is divided into 0, 1, 1+, 2, 3, and 4, to achieve a total of six levels. A higher score indicated increased muscle spasticity (0 = none, 4 = most severe).
Secondary outcomes
The secondary outcome indicators included one of the following, Fugl-Meyer (FMA), Barthel Index (BI), and Neurological Function Deficit Scale (NDS). The FMA covers complex content, including tendon reflexes, muscle coordination, finger grip, joint mobility, and others. The lower the score, the worse the condition (0 = none and 100 = most severe). The BI scale primarily reflected the activities of daily life (0 = not affected and 100 = most severe). The NDS mainly evaluated speech, consciousness, facial paralysis, limb function, and others (0 = none and 45 = most severe). The primary outcome indicators included the effective rate (ER), recovery rate (RR), and the modified Ashworth scale (MAS). The ER and RR reflected the improvement before and after treatment. The MAS scale is divided into 0, 1, 1+, 2, 3, and 4. The higher the score, the worse the degree of muscle spasticity (0 = none, 4 = most severe).
Results
Study selection
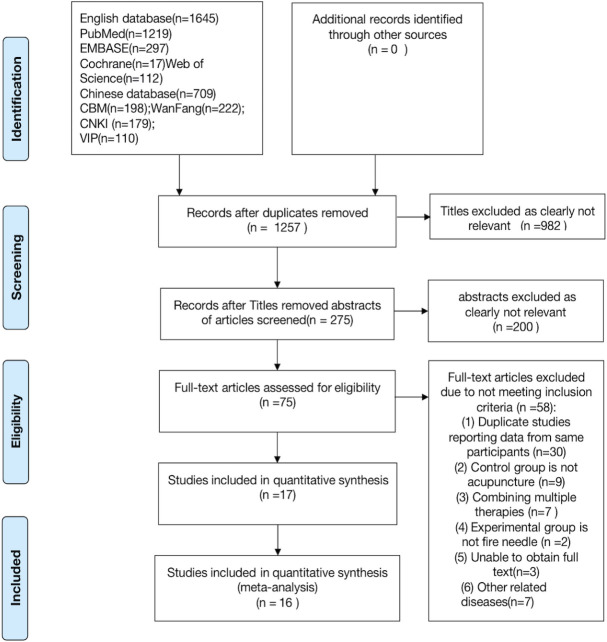
A total of 2,354 articles related to the topic were retrieved through a comprehensive database search, of which, 1,097 articles were duplicates. Based on the premise of excluding all irrelevant data, a total of 17 RCTs were included in the analysis. One of the 17 articles was eliminated from the final set of studies because the data were incomplete, and the missing data could not be obtained from the study’s corresponding author. Eventually, 16 articles, with a total of 1,118 patients, were included in the analysis [22–37]. The detailed screening process is shown in (Fig 1).
Fig 1. Modified PRISMA flow diagram of included/excluded studies.
Study characteristics
Basic characteristics of the included studies
All trials were conducted in China and published in Chinese, and all studies were carried out based on traditional acupuncture theory. Among the included studies, four were master theses [25, 33, 34, 37]. All the control groups included in the studies received acupuncture treatment. Fifteen of the studies compared fire needles with conventional acupuncture [21, 22, 25–27], and one study compared fire needle acupuncture with electroacupuncture [37]. The sixteen studies were published between 2005 and 2018. The ages of the patients ranged from 34 to 80 years. The course of the disease ranged from two months to one year. However, two studies did not report relevant information [23, 30]. Nine articles provided comprehensive information [21–24, 27, 31, 33, 34, 36, 37] regarding the type of stroke (intracerebral hemorrhage or cerebral infarction) exhibited by the patients. On the other hand, no specific information concerning the type of stroke was mentioned in four studies [25–27, 29, 30]. Three studies described the type of stroke that the patients experienced, but the report lacked detailed figures [28, 32, 35]. Eleven studies emphasized the state of the stroke, of which seven studies recorded that the patients were in the recovery period or sequelae after stroke [23, 25, 28, 31–33]. Three studies included patients who were in the recovery period, one study included participants that were in the sequelae period [36] and four studies did not report the related information [23, 25, 28, 31–34]. In seven studies, patients received basic medical treatment, including control of blood pressure, regulation of blood glucose, stabilization of blood lipids, and nutritional support [21–23, 25, 28, 31–32, 34].
In addition to receiving acupuncture, participants in four studies also participated in basic rehabilitation training [22, 24, 28, 30]. All studies described the specific sites of treatment. Five studies assessed the upper limbs [24, 25, 29, 31, 37], one study evaluated the fingers [22], and nine studies assessed the upper and lower limbs [19, 23–25, 27–29, 33]. Except for three studies that distinguished the severity of stroke [28, 36, 37], none of the other studies provided such a description. Fifteen trials [22–35, 37] used ER, and nine studies [24, 25, 27, 28, 30, 32–35] used the MAS scale to assess the degree of improvement in spasticity after treatment. The FMA scale also was used in ten studies [23–28, 30, 32, 34, 35]. Six studies utilized the BI scale to assess the daily abilities of patients [23, 26, 28, 34, 35, 37]. No studies conducted follow-up assessments. None of the studies reported any fatal adverse events that resulted from acupuncture. The detailed characteristics of each study are shown in (Table 1).
Table 1. Detail of studies include.
| First author (year) | Age range TG/CG (M±SD) | Genger(M:F) TG/CG (M±SD) | Sample size (TG/CG) | Duraton after Stroke (TG/CG) | Control intervention | Outcome measures | Intergroup differences | Follow -up |
|---|---|---|---|---|---|---|---|---|
| Peng A [22], 2017 | T:57.1±7.8 C:56.7±8.2 | T:15/11 C:14/12 | 26/26 | NR | AT:30 min,everyday,rest for 1 day after 6 consecutive treatment,30d | ER | P < 0.05 In favor of FA | NR |
| Yang [23], 2017 | T:60.5±5.8 C:61.8 ±6.4 | T:11/7 C:12/6 | 18/18 | 18.5±3.9/20.5± 4.3(w) | AT:10 min,every other day,1 session (1 session = 3 wk, one day rest between each weeks | ER;(2)FMA; (3) BI | (1)(2)(3)P < 0.05 In favor of FA | NR |
| Sang [24], 2017 | T:62.57±5.75 C:63.20±7.07 | T:19/11 C:17/13 | 30/30 | 168.70±56.99/166.17±87.02(d) | EA:30 min,everyday,14d | (1)ER;(2);FMA(3)MAS | (1)(2)(3)P < 0.05 In favor of FA | NR |
| Liu [25], 2018 | NR | T:19/12 C:18/13 | 31/31 | 15-338/17-342(d) | AT:30 min,every other day (1 session = 28d,a total of 14 treatment | (1)ER(2)FMA(3)MAS(wrist.elbow) | (1)(2)(3)P < 0.05 In favor of FA | NR |
| Chai [26], 2017 | T:61.90±3.18 C:58.93 ±11.93 | T:17/13 C:16/14 | 30/30 | 110.57±36.641/112.70±36.69(d) | AT:30 min,everyday,4 weeks (6 times a week) | ER (2)FMA (3) BI | (1)(2)(3)P < 0.05 In favor of FA | NR |
| Wang [27], 2018 | T:64.87±8.18 C:65.67±7.52 | T:19/11 C17/13 | 30/30 | 99.83±32.31/99.83±32.31(d) | AT:30 min,everyday,14d | (1)ER; (2)FMA; (3)MAS (wrist,elbow,keen,ankle); (4)NDS(median,ulnar nerve) | (1)(2)(3)(4)P < 0.05 In favor of FA | NR |
| Deng [28], 2017 | T:61. 4±6. 2 C:63. 2±7. 7 | T:25/19 C:22/20 | 44/42 | 5.9±2.3/6. 1± 2.6(m) | AT:30 min,every other day 2 session (1 session = 7 times) | (1)ER; (2)FMA; (3)BI;; (4)MAS; (5)NDS(median, ulnar nerve) | (1)(2)(3)(4)P < 0.05 In favor of FA | NR |
| Peng B [29], 2017 | T:66.5±1.2 C:67.6±2.3 | NC | 50/50 | NR | AT:30 min | ER | P < 0.05. In favor of FA | NR |
| Sheng [30], 2017 | T:55. 62 ± 4.19 C:56.21± 3.98 | T:16/15 C:17/14 | 31/31 | 185.62±63.19/185.48±64.22 (d) | AT:30min,everyday,(1session = 6 times,1 day rest between every session),30d | (1)ER;(2)FMA;(3)MAS(wrist, elbow, keen, ankle) | (1)(2)(3)P < 0.05 In favor of FA | NR |
| Xu [31], 2015 | T:58.3±7.8 C:57.4±8.1 | T:29/11 C:27/13 | 40/40 | 20.2±4.6/19.6±4.3(w) | AT:30 min,every other day 2 session (1 session = 2 weeks) | ER | P < 0.05. In favor of FA | NR |
| Wang [32], 2015 | T:52.3±21.4 C: 5 4.5±20.7 | T:22/18 C:20/20 | 40/40 | 175.6±94.6/18.72±88.6(d) | AT:30 min,every other day(Rest for 1 day after 6 consecutive treatment) | (1)ER; (2)FMA; (3)MAS | (1)(2)(3)P < 0.05 In favor of FA | 1 mo |
| Yuan [33], 2015 | T:64.31±5.62 C:66.25±4.12 | T:18/12 C:16/14 | 30/30 | 8.22±3.53 /7.71±4.20(m) | EA:20min,everyday,2 session(Rest 2 days after 5 consecutive treatment) | ER; (2) BI;(3)MAS; (4)NDS | (1)(2)(3)(4)P < 0.05.In favor of FA | NR |
| Liu [34], 2014 | T:63.97±9.66 C:67.47±9.32 | T:16/14 C:13/17 | 30/30 | 167.35±34.26/179.33+42.32 (d) | AT:30min,everyday,8 times(Rest for 1 day after 6 consecutive treatment) | ER; (2)BI; (3)FMA; (4)MA S | (1)(2)(3)(4)P 0.05 In favor of FA | NR |
| Zhao [35], 2013 | T:61.20±7.35 C:60.70±6.79 | T:23/17 C:21/19 | 40/40 | 2.76±1.05/3.02±1.41(m) | AT:30min,everyday,2 session (1 session = 9 times) | (1)ER; (2)FMA; (3)MAS;(4) NDS | (1)(2)(3)(4)P < 0.05 In favor of FA | NR |
| Chen [36], 2005 | NR | T:18/12 C:16/14 | 30/30 | 7.8/8(m) | AT:30 min,every other day 2m | BI | P < 0.05. In favor of FA | NR |
| Gao [37], 2004 | T:56±0.71 C:54.8±5.13 | T:23/7 C:20/10 | 30/30 | 250.13/245.6 (d) |
AT: everyday | (1)ER; (2)NDS | (1)(2)P < 0.05 In favor of FA | NR |
NC = not record; EA = electroacupuncture; AT = acupuncture treatment; ER = effective rate; RR = Recovery rate; FMA = Fugl-Meyer; MAS = The modified Ashworth scale; CSI = Clinic Spastcity Index; BI = Barthel Index; NDS = neurological function deficit scale; TG = treatment group; CG = control group; M = mean; SD = standard deviation.
Details of the intervention groups in the included studies
There were eleven studies [21–31] that provided the insertion depth of the fire needles, which ranged from 3mm to 30mm in ten studies. However, one study utilized shallow skin penetration to a depth of only 1mm to 3mm [26]. Concerning the types of fire needles used, they were approximately 0.35mm in diameter with lengths that ranged from 20 to 40 mm. The course of treatment ran between two weeks and one month. It was emphasized that a rest period was to be taken in the middle of the treatment. Additional details are shown in (Table 2). The acupuncture points used with high frequency in the sixteen studies were as follows (Table 3), LI11-Quchi (nine times), LI10-Shousanli (nine times), Extrapoint-baxie (seven times), SJ5-Waiguan (seven times), LI4-Hegu (seven times), SI3-Houxi (six times), ST-Zusanli (five times), LR3-Taichong (four times), SJ4-Yangchi (four times), and SP6-Sanyinjiao (four times). Among all the meridians, the large intestine meridian of the hand-yangming, the small intestine meridian of the taiyang, and the triple energizer meridian of the hand-shaoyang were the three most frequently used. These meridians are usually referred to as the three yang channels of the hand.
Table 2. Details of experimental interventions.
| First author (year) | points | Needle type | Depth of Insertion (TG/CG) | Treatment Frequency | Sessions (TG/CG) |
|---|---|---|---|---|---|
| Peng A [22], 2017 | SP10(Xuehai), SI3 (Houxi), GB44 (Zuqiaoyin), Extra-point (Baxie), LI10 (Shousanli), LI11 (Quchi), LI14 (Bilao), SJ5 (Waiguan), KI3 (Taixi), SJ4 (Yangchi) | NR | NR | Every two days | 30 days (Rest for 2 day after 5 comsec utive treatment) |
| Yang [23], 2017 | Wrist:SJ3 (Zhongzhu), SJ4 (Yangchi), LI4 (Hegu);Upper limb:LI10 (Shousanli), LI11 (Quchi), SJ5(Waiguan);Lower limb:BL40 (Weizhong), BL39 (Weiyang), BL40(Heyang), BL57 (Chengshan), BL37(Yinmen), SP6(Sanyinjiao) | 0.35mm*(30~40)mm | NR | every other day | 1 session (1 session = 3 wk) |
| Sang [24], 2017 | LI10 (Shousanli), SJ10(Tianjing) | NR | 0.5–1 cm (5-10mm) | Every day | 14 d |
| Liu [25], 2018 | Extra-point (Jiaji)(C3-7、T1-3) | 0.35mm*(20~40)mm | 0.5–1.5cun (17-33mm) | every ther day | 1 session 1 session = 28d,a total of 14 treatments) |
| Chai [26], 2017 | LI15(Jianyu), LI11 (Quchi), SJ5(Waiguan), SI3(Yanglao), GB34(Yanglinquan), SP6(Sanyinjiao), ST6(Zusanli),Ashi point | 0.5mm*(25~30)mm | 1-3mm | every day | 4 weeks (3 times a week) |
| Wang [27], 2018 | Upper limb:SJ5(Waiguan), LI10 (Shousanli), LI15(Jianyu);Lower limb:ST6 (Zusanli), GB34(Yanglinquan),BL40 (Weizhong), LR3 (Taichong) |
0.4mm*40mm | 1.5cun (50mm) | every day | 14 d |
| Deng [28], 2017 | Upper limb:LI15(Jianyu), LI11 (Quchi), LI10 (Shousanli), SJ5(Waiguan), LI4 (Hegu),HT1(Jiquan),LU5(Chize);Lower limb:GB30(Huantiao),ST6(Zusanli), GB34(Yanglinquan),LR3(Taichong),SP6(Sanyinjiao), KI6(Taixi),GB40(Qiuxu)L | 0.35mm*40mm | 15mm | every other day | 2 session (1 session = 7 times) |
| Peng B [29], 2017 | LI4 (Hegu),LI11 (Quchi),LI15(Jianyu) | NR | 3-15mm | NR | NR |
| Sheng [30], 2017 |
LI4 (Hegu),LI11 (Quchi),LI15(Jianyu),LI10 (Shousanli),GB34(Yanglinquan), BL40 (Weizhong), LR3(Taichong),GB30 (Huantiao),HT1(Jiquan) | 0.45mm*40mm | 3-15mm | every two days | 30 d (Rest for 2 days after 5 consecut-ive treatment) |
| Xu [31], 2015 | DU20(Baihui),Extra-poin (Taiyang),GB20 (Fengchi), DU16 (Fengfu) HT1(Jiquan),LU5(Chize),PC3(Quze),PC6(Neiguan),PC7(Daling),LI4(Hegu), SI3(Houxi),SP6(Sanyinjiao),SP9(Yinlingquan),(LR3(Taichong),LR2(Jimai),KI10(Yingu),SP5(Shangqiu),GB40(Qiuxu) | NR | 10-20mm | every other day | 2 session (1 session = 2 weeks) |
| Wang [32], 2015 | LI15(Jianyu), LI14 (Bilao), LI11 (Quchi),LI10 (Shousanli), SJ5(Waiguan), SJ(Yangchi),SI3(Houxi),LI4(Hegu),Extra-point (Baxie),SP9(Yinlingquan), SP6(Sanyinjiao),KI10(Yingu),LR3(Taichong),GB44(Zuqiaoyin) | 0.40mm*45mm | 3-15mm | every two days | 30 d (Rest for 2 days after 5 consecut- tive treatment) |
| Yuan [33], 2015 | A:Upper limb:LI15(Jianyu), LI4(Hegu),HT3(Shaohai),LI3(Sanjian), Lower limb:ST31(Biguan),ST36(Zusanli), LR3(Taichong) B:Upperlimb:SI9(Jianzhen),LU5(Chize),LI10(Shousanli),SI3(Houxi), Lower limb:GB30 (Huantiao),GB31 (Fengshi),BL57(Chengshan),BL60(Kunlun) Group A and Group B alternate | 0.30–0.35mm*20-75mm | 20-25mm for upper limb; 20-30mm for Lower limb | every day | 2session(1session = 2 weeks) (Rest for 2 days after 5 consecutive treatm ent) |
| Liu [34], 2014 | A:PC6(Neiguan), LU5(Chize), PC3(Quze), HT3(Shaohai), SI3(Houxi), LI10(Shousanli),LI11 (Quchi) B:PC2(Tianquan),HT2(Qingling),LU3(Tianfu),LI15(Jianyu),LI14(Bilao), SJ13(Naohui) Group A and Group B alternate | 0.65mm*50mm | 0.3cun (10mm) | every two days | 8 times |
| Zhao [35], 2013 | Extra-point (Baxie), Extra-point (Shangbaxie), ST36(Zusanli),ST40(Jiexi), ST34(Liangqiui),ST32(Futu),Extra-point (Bafeng) | NR | NR | every three days | 2 session (1 session = 3 times) |
| Chen [36], 2005 | Upper limb:LI15(Jianyu),LI10(Shousanli),LI11 (Quchi),LI4 (Hegu),Extra-point (Bafeng);Lower limbs:ST36(Zusanli),ST34(Liangqiui),ST32(Futu),ST40(Jiexi), Extra-point (Baxie) | NR | NR | every other day | 2 m |
| Gao [37], 2004 | Jiaji(C4-7),LI15(Jianyu),SJ14(Jianliao), SI13(Quyuan),SI12(Bingfeng), SI11(Tianzong),SJ10(Tianjing),LI5(Yangxi),SJ4(Yangchi),SI3(Houxi), SJ9(Sidu), LI11 (Quchi),LI12(Zhouliao),Extra-point (Waibaxie), | NR | NR | every other day | NR |
Table 3. Frequency of main acupoints.
| Upper limbs | Frequency | Lower limbs | Frequency |
|---|---|---|---|
| Quchi (LI11) | 9 | Zusanli (ST36) | 5 |
| Shousanli (LI10) | 9 | Taichong (LR3) | 4 |
| Baxie (Extra-point) | 7 | Sanyinjiao (SP6) | 4 |
| Waiguan (SJ5) | 7 | Weizhong (BL40) | 3 |
| Hegu (LI4) | 7 | Taixi (KI3) | 3 |
| Houxi (SI3) | 6 | Yinlinquan (SP9) | 3 |
| Yangchi (SJ4) | 4 | Yanglinquan (GB34) | 3 |
| Chize (LU5) | 4 | Zhaohai(KI6) | 2 |
| Bilao (LI14) | 3 | Qiuxu(GB40) | 2 |
STRICTA checklist for the included studies
The STRICTA checklist is taken from the Standards for Reporting Interventions in Controlled Trials of Acupuncture [38]. Additional details are shown in Table 4. All studies [22–37] fully described the style of acupuncture that was used, the rationale for treatment, and the literature sources used to justify the rationale for acupuncture use. Concerning needling details, ten studies [25–34] recorded unilateral or bilateral usage of acupuncture points. Only one study [35] did not specify the number of acupuncture points. Five studies [22, 23, 35–37] did not describe the depth of acupuncture needle insertion. All eleven studies [25–27, 28–34, 37] discussed possible reactions that were caused by the use of acupuncture. Due to the particular forms of fire needles that were used, all studies explained the stimulation form of acupuncture. Only one study [22] did not record the needle retention time. Six studies did not introduce the type of acupuncture [22, 23, 29, 30, 35–36] two studies [29–37] did not describe the number of treatment sessions, and one trial [29] did not mention the treatment frequency. All eleven studies did not combine acupuncture with other therapies. Nine of the studies thoroughly described the setting and context for treatment, and two studies [29, 30] did not. None of the studies described the duration of relevant training for the acupuncture therapists. Also, only three studies [22, 29, 35] mentioned the training time and professional level for acupuncture therapists. All studies provided sources that justified the choice of control subjects.
Table 4. STRICTA, Standards for Reporting Interventions in Controlled Trials of Acupuncture.
| Study | Acupuncture rationale | Needling details | Treatment regime | Cointerventions | Practitioner background | Control intervention | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First author(year) | 1a | 1b | 1c | 2a | 2b | 2c | 2d | 2e | 2f | 2g | 3a | 3b | 4a | 4b | 5a | 5b | 5c | 6a | 6b | 6c |
| Peng A [22], 2017 | YES | YES | YES | NO | YES | NO | NO | YES | NO | NO | YES | YES | NO | YES | NO | YES | YES | YES | NO | YES |
| Yang [23], 2017 | YES | YES | YES | NO | YES | NO | NO | YES | YES | YES | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Sang [24], 2017 | YES | YES | YES | NO | YES | YES | NO | YES | YES | NO | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Liu [25], 2018 | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Chai [26], 2017 | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Wang [27], 2018 | YES | YES | YES | YES | YES | YES | NO | YES | YES | YES | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Deng [28], 2017 | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Peng B [29], 2017 | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | NO | NO | NO | NO | NO | YES | YES | NO | NO | YES |
| Sheng [30], 2017 | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | NO | NO | NO | YES | NO | YES | YES |
| Xu [31], 2015 | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Wang [32], 2015 | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | YES | NO | YES | YES | NO | YES | YES |
| Yuan [33], 2015 | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Liu [34], 2014 | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | YES | NO | NO | YES | NO | YES | YES |
| Zhao [35], 2013 | YES | YES | YES | NO | NO | NO | NO | YES | YES | NO | YES | YES | NO | YES | NO | NO | YES | NO | NO | YES |
| Chen [36], 2005 | YES | YES | YES | NO | YES | NO | YES | NO | YES | NO | YES | YES | NO | YES | NO | NO | YES | NO | NO | YES |
| Gao [37], 2004 | YES | YES | YES | NO | YES | NO | NO | YES | YES | YES | NO | YES | NO | YES | NO | NO | YES | NO | NO | YES |
STRICTA, Standards for Reporting Interventions in Controlled Trials of Acupuncture;1a, style of acupuncture; 1b, rationale for treatment (eg, syndrome patterns, segmental levels, trigger points) and individualisation if used; 1c, literature sources to justify rationale; 2a, points used (unilateral/bilateral); 2b, numbers of needles inserted; 2c, depths of insertion (eg, cun or tissue level); 2d, responses elicited (eg, de qi or twitch response); 2e, needle stimulation (eg, manual or electrical); 2f, needle retention time; 2g, needle type (gauge, length, and manufacturer or material); 3a, number of treatment sessions; 3b, frequency of treatment; 4a, other interventions (eg, moxibustion, cupping, herbs, exercises, lifestyle advice); 4b, setting and context of treatment, including instructions to practitioners, and information and explanations to patients; 5a, duration of relevant training; 5b, length of clinical experience; 5c, expertise in specific condition; 6a, intended effect of control intervention and its appropriateness to research question and, if appropriate, blinding of participants (eg, active comparison, minimally active penetrating or non-penetrating sham, inert); 6b, explanations given to patients of treatment and control interventions, details of control intervention (precise description, as for item 2 above, and other items if different); 6c, sources that justify choice of control; No, no details report; Yes, details reported.
Study quality
According to the criteria of the RoB 2.0 Tool, most of the studies are considered to have some concerns. The items that affect the quality of most studies are the blind implementation and missing outcome data, Only three presented low risk of bias in all the assessed domains [23, 29, 30], other studies have suggested some concerns to a certain degree in each items (Table 5), Fleiss’s Kappa scores in our research Hinted substantia (Fleiss’s Kappa scores = 0.75).
Table 5. Assessment of risk of bias for all included studies using the revised of bias tool (Rob 2.0).
| Studies | Randomization | Intervention | Missing | Outcome | Reported | Overall |
|---|---|---|---|---|---|---|
| Data | measurement | results | Risk | |||
| Peng A [22], 2017 | High | Some concerns | Some concerns | Some concerns | Low | High |
| Yang [23], 2017 | Low | Low | Low | Low | Low | Some concerns |
| Sang [24], 2017 | High | Low | Some concerns | Some concerns | Low | High |
| Liu [25], 2018 | Some concerns | Low | Low | Low | Low | Some concerns |
| Chai [26], 2017 | Low | Low | Low | Low | Low | Low |
| Wang [27], 2018 | Low | Low | Low | Low | Low | Low |
| Deng [28], 2017 | Some concerns | Low | Low | Low | Low | Some concerns |
| Peng B [29], 2017 | Some concerns | Some concerns | Low | Some concerns | Low | High |
| Sheng [30], 2017 | Low | Low | Some concerns | Low | Low | Some concerns |
| Xu [31], 2015 | Some concerns | Some concerns | Some concerns | Low | Low | Some concerns |
| Wang [32], 2015 | Low | Low | Some concerns | Low | Low | Low |
| Yuan [33], 2015 | Low | Low | Low | Low | Low | Low |
| Liu [34], 2014 | Low | Low | Low | Low | Low | Some concerns |
| Zhao [35], 2013 | Some concerns | Low | Some concerns | Low | Low | Some concerns |
| Chen [36], 2005 | Some concerns | Low | Some concerns | Low | Low | Some concerns |
| Gao [37], 2004 | Some concerns | Low | Some concerns | Low | Low | Some concerns |
Low: Low risk of bias
High: High risk of bias
Some concerns: Some concerns of risk of bias
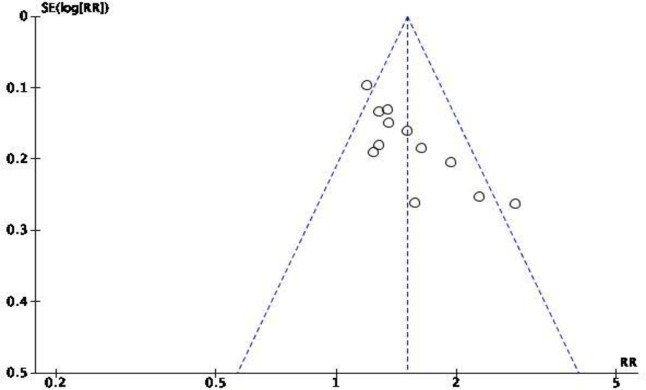
Funnel plot of publication bias. Using a funnel plot, the research team analysed publication bias in all included studies (Fig 2). The outcome suggested that there was little publication bias.
Fig 2. Funnel plot of studies comparing fire acupuncture after stroke in ER.
Results of the meta-analysis
Main outcomes for ER, RR, and MAS
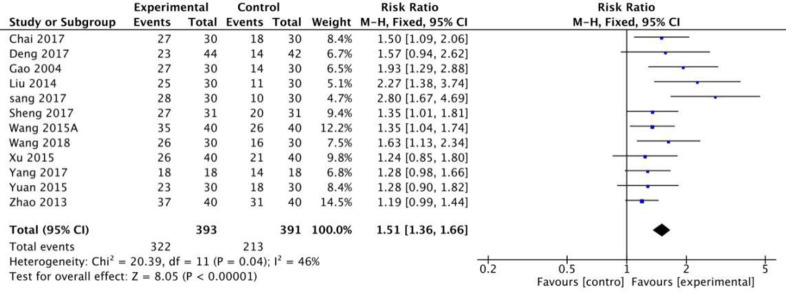
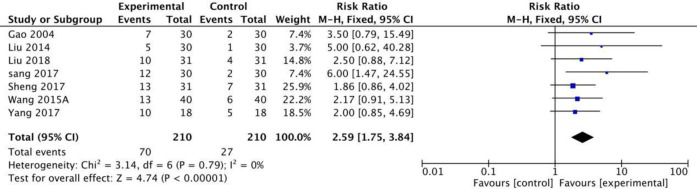
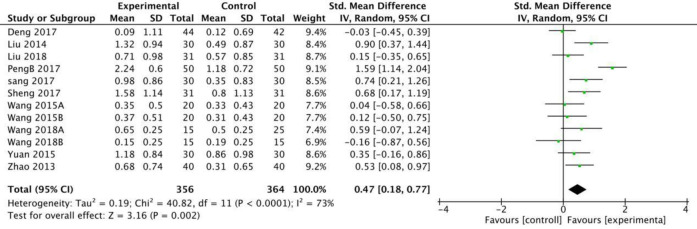
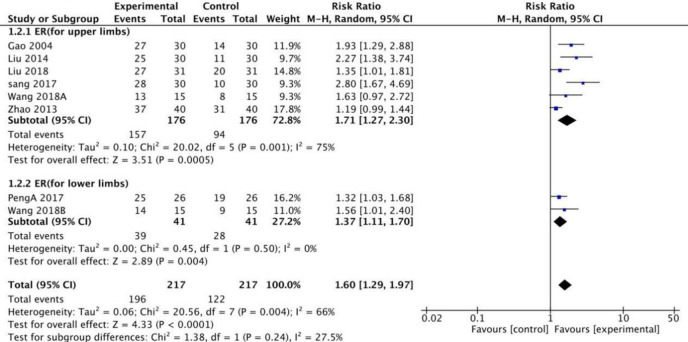
Twelve RCTs in this study used the MAS scale to calculate the effective rates. The meta-analysis revealed that when a fixed model was used, the fire needle group could significantly improve the post-stroke spasticity compared with the acupuncture group [RR = 1.51[1.36,1.66], P<0.001, Fig 3]. Seven studies with a total of 420 patients used the MAS scale to evaluate the recovery rate. The results of the fixed model showed that the therapeutic effect of fire needles was superior [RR = 2.59 [1.75, 3.84], P <0.001, Fig 4]. A total of 12 studies that included 720 patients used the MAS scale to assess changes before and after treatment for patients with spasticity after stroke. The random model results demonstrated that, compared with the acupuncture group, the fire needle group had a stronger correlation with the improved score [MD = 0.47, 95%CI [0.18, 0.77], P = 0.002, Fig 5]. All results are provided in (Table 6).
Fig 3. Meta-analysis of fire acupuncture versus acupuncture for spasticity after stroke in ER.
Fig 4. Meta-analysis of fire acupunture versus acupuncture for spasticity after stroke in RR.
Fig 5. Meta-analysis of fire acupuncture versus acupunture for spasticity after in MAS.
Table 6. Meta-analysis of the effects of fire acupuncture vs. electroacupuncture or acupuncture.
| Outcomes or Subgroup 1.1ER | Studies 12 | Participants 784 | Statistical Method Risk Ratio (M-H, Fixed, 95% CI) | Effect Estimate 1.51 [1.36,1.66] | P | Heterogeneity |
|---|---|---|---|---|---|---|
| P<0.00001 | P = 0.04;I2 = 46% | |||||
| 1.2ER(for limbs) | 8 | 434 | Risk Ratio (M-H, Random, 95% CI) | 1.60 [1.29,1.97] | P<0.00001 | P = 0.004;I2 = 66% |
| 1.2.1ER(for upper limbs) | 6 | 352 | Risk Ratio (M-H, Random, 95% CI) | 1.71 [1.27,2.30] | P = 0.0005 | P = 0.001;I2 = 75% |
| 1.2.2ER(for lower limbs) | 2 | 82 | Risk Ratio (M-H, Random, 95% CI) | 1.37 [1.11,1.70] | P = 0.004 | P = 0.50;I2 = 0% |
| 1.3ER(for the thickness of FA) | 10 | 566 | Risk Ratio (M-H, Fixed, 95% CI) | 1.46 [1.30, 1.64] | P<0.00001 | P = 0.75;I2 = 0% |
| 1.3.1ER(≤0.35mm*(20~40)mm) | 4 | 244 | Risk Ratio (M-H, Fixed, 95% CI) | 1.42 [1.19, 1.70] | P<0.0001 | P = 0.79;I2 = 0% |
| 1.3.1ER(>0.35mm*(20~40)mm) | 6 | 322 | Risk Ratio (M-H, Fixed, 95% CI) | 1.49 [1.28, 1.73] | P<0.00001 | P = 0.46;I2 = 0% |
| 1.4ER (for the depth of FA) | 11 | 662 | Risk Ratio (M-H, Fixed, 95% CI) | 1.53 [1.37, 1.71] | P<0.00001 | P = 0.23;I2 = 22% |
| 1.4.1ER(<3mm) | 1 | 60 | Risk Ratio (M-H, Fixed, 95% CI) | 1.50 [1.09, 2.06] | P = 0.01 | Not applicable |
| 1.4.2ER(3-15mm) | 7 | 462 | Risk Ratio (M-H, Fixed, 95% CI) | 1.57 [1.38, 1.80] | P<0.00001 | P = 0.05;I2 = 52% |
| 1.4.3ER(>15mm) | 3 | 140 | Risk Ratio (M-H, Fixed, 95% CI) | 1.39 [1.09, 1,79] | P = 0.009 | P = 0.61;I2 = 0% |
| 1.5RR(for the whole body) | 7 | 420 | Risk Ratio (M-H, Fixed, 95% CI) | 2.59 [1.75, 3.84] | P<0.00001 | P = 0.79;I2 = 0% |
| 1.6MAS(for the whole body) | 12 | 720 | Std.Mean Difference (IV, Random, 95% CI) | 0.47 [0.18, 0.77] | P = 0.002 | P<0.0001;I2 = 73% |
| 1.7MAS | 8 | 401 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.41 [0.21, 0.61] | P<0.0001 | P = 0.15;I2 = 35% |
| 1.7.1MAS(for upper limbs) | 6 | 332 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.50 [0.28, 0.72] | P<0.00001 | P = 0.22;I2 = 29% |
| 1.7.2MAS(for lower limbs) | 2 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.01 [-0.47, 0.48] | P = 0.98 | P = 0.57;I2 = 0% |
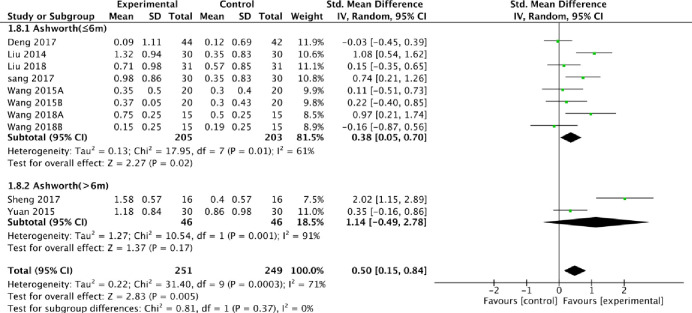
| 1.8MAS(the course of disease) | 10 | 500 | Std.Mean Difference (IV, Random, 95% CI) | 0.50 [0.15, 0.84] | P = 0.004 | P = 0.0003;I2 = 71% |
| 1.8.1MAS(≤6m) | 8 | 408 | Std.Mean Difference (IV, Random, 95% CI) | 0.38 [0.05, 0.70] | P = 0.02 | P = 0.01;I2 = 61% |
| 1.8.2MAS(>6m) | 2 | 92 | Std.Mean Difference (IV, Random, 95% CI) | 1.14 [-0.49, 2.78] | P = 0.17 | P = 0.001;I2 = 71% |
| 1.9MAS(the depth of FA) | 10 | 570 | Std.Mean Difference (IV, Random, 95% CI) | 0.48 [0.11, 0.85 | P = 0.01 | P<0.00001;I2 = 78% |
| 1.9.1MAS(3-15mm) | 8 | 510 | Std.Mean Difference (IV, Random, 95% CI) | 0.54 [0.12, 0.95] | P = 0.01 | P<0.00001;I2 = 81% |
| 1.9.2MAS(>15mm) | 2 | 60 | Std.Mean Difference (IV, Random, 95% CI) | 0.21 [-0.51, 0.93] | P = 0.57 | P = 0.16;I2 = 50% |
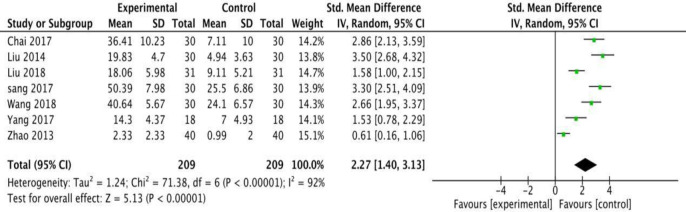
| 1.10FMA | 7 | 418 | Std.Mean Difference (IV, Random, 95% CI) | 2.27 [1.40, 3.13] | P<0.00001 | P<0.00001;I2 = 92% |
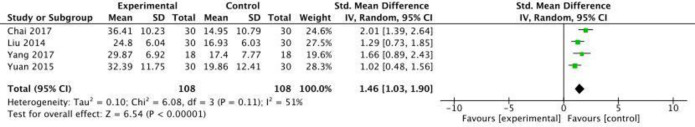
| 1.11BI | 4 | 216 | Std.Mean Difference (IV, Random, 95% CI) | 1.46 [1.03, 1.90] | P<0.00001 | P = 0.11;I2 = 51% |
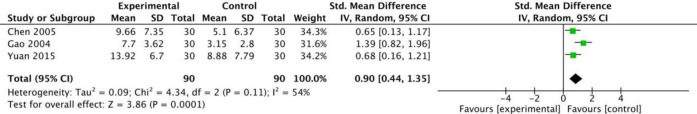
| 1.12NDS | 3 | 180 | Std.Mean Difference (IV, Random, 95% CI) | 0.90 [0.44, 1.35] | P = 0.0001 | P = 0.11;I2 = 54% |
ER = effective rate; RR = Recovery rate; FMA = Fugl-Meyer; MAS = The modified Ashworth scale; CSI = Clinic Spastcity Index;
BI = Barthel Index; NDS = neurological function deficit scale.
Subgroup analysis
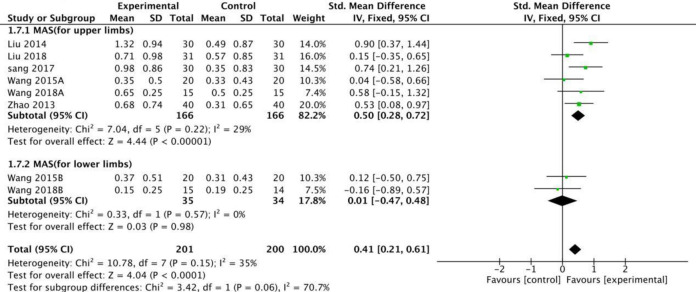
Based on the subgroup analysis of stroke-injured limbs on the ER side, the random model results showed that fire needle therapy for the upper and lower limbs produced significant improvements, [RR = 1.71 [1.27, 2.30] and RR = 1.37 [1.11, 1.70], Fig 6], respectively. When using MAS to evaluate the degree of spasm in limbs injured by stroke, the fixed model results revealed that fire needles produced better results than conventional acupuncture in reducing the MAS score for the upper limbs [SMD = 0.50, 95%CI [0.28, 0.72], Fig 7]. However, the lower limbs did not show significant improvement [SMD = 0.01, 95% CI [-0.47, 0.48], Fig 7].
Fig 6. Meta-analysis of fire acupuncture versus acupuncture for spasticity after stoke.
Fig 7. Meta-analysis of fire acupuncture versus acupuncture for spasticity after stoke according to region.
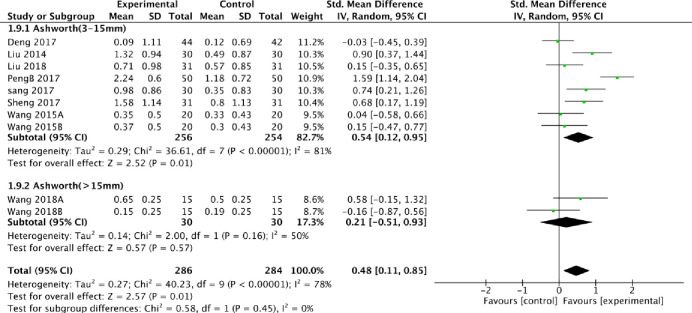
We also conducted a subgroup analysis based on the thickness of the fire needles and acupuncture depth. From the perspective of efficiency, fire needles were better than acupuncture to some extent with low heterogeneity, regardless of the depth or thickness changes in the subgroup analysis. When MAS was used to evaluate the improvement based on acupuncture depth, the random model results demonstrated that the fire needles were significantly deeper compared to conventional acupuncture, where the acupuncture depth was 3 to 15mm [SMD = 0.54, 95% CI [0.12, 0.95], Fig 8]. It is worth noting that when the acupuncture depth exceeded 15mm, the fire needles were not superior to acupuncture [SMD = 0.21, 95% CI [-0.51, 0.93], Fig 8].
Fig 8. Meta-analysis of fire acupuncture versus acupuncture for spasticity after stoke according to depth of acupuncture in MAS.
We also extracted additional information from the studies included in the meta-analysis. When combined with the stroke duration and the extent of improvement as assessed using MAS, the subgroup analysis established that the extent of improvement for the fire needle scale was superior to acupuncture [SMD = 0.38, 95% CI [0.05, 0.70], Fig 9] when the stroke duration was less than six months. As expected, there was no difference between fire needles and conventional acupuncture when the duration of stroke was longer than six months [SMD = 1.14, 95% CI [-0.49, 2.78], Fig 9]. All results are presented in (Table 6).
Fig 9. Meta-analysis of fire acupuncture versus acupuncture for spasticity after stoke according to the course of disease.
Secondary outcomes for FMA, BI, and NDS
A random model meta-analysis was used to assess the secondary outcomes. Using any of the scales, FMA, BI, or NDS, revealed that fire acupuncture exhibited better performances compared to conventional acupuncture [SMD = 2.27, 95% CI [1.40, 3.13], Fig 10], [SMD = 1.46, 95% CI [1.03, 1.90], Fig 11], and [SMD = 0.90, 95% CI [0.44, 1.35], Fig 12], respectively, with moderately high heterogeneity. All results are presented in (Table 6).
Fig 10. Meta-analysis of fire acupuncture versus acupuncture for spasticity after stroke in FMA.
Fig 11. Meta-analysis of fire acupuncture versus acupunture for spasticity after stroke in B1.
Fig 12. Meta-analysis of fire acupuncture versus acupuncture for spasticity after stroke in NDS.
Results of meta-regression
We initially judged that the source of heterogeneity may come from two major aspects. One is the difference related to stroke information, such as the type of stroke (intracerebral hemorrhage or cerebral infarction or both), and the influence of the location of spasm after stroke (Whole body, upper extremity or lower extremity), The second is the difference from the specific implementation process of fire acupuncture, such as the number of acupuncture points, the depth of acupuncture, and the frequency of treatment. All of the above differences may be the source of heterogeneity. Therefore, we performed meta-regression on the following factors. The results suggested that none of the above factors are the cause of heterogeneity (P>0.05), the results showed in (Table 7).
Table 7. Result of meta-regression.
| Factor | P-value | 95% Confidence interval |
|---|---|---|
| gauge of needle | 0.168 | [-0.859424,0.1974747] |
| Depth of insertion | 0.716 | [-2.718377,0.3675489] |
| Treatment Frequency | 0.594 | [-0.6249931,0.3985297] |
| Number of needle | 0.417 | [-0.5323939,1.091061] |
| Type of stroke | 0.206 | [-1.0366451,0.2878423] |
| Location of spasticity | 0.784 | [-0.5455986,0.6842484] |
| Pooled -result | 0.224 | [-1.280113, 4.283351] |
Discussion
Joint convulsion, deformities, and muscle atrophy caused by stroke always result in clinical symptoms that include motor dysfunction, joint swelling, pain, and numbness. These symptoms reduce a patient’s quality of life and produce severe physical, psychological, and economic burdens on patients, leading to depression, low self-esteem, despair, and suicidal thoughts [39, 40]. More importantly, stroke survivors may have reduced motivation to pursue rehabilitation training due to spasticity, which, in turn, has negative effects on their recovery outcomes [41, 42]. Multiple studies have recognized the efficacy of acupuncture for stroke sequelae, including relief of anxiety, and improved quality of life, especially for stroke patients [43]. Several meta-analyses focused on clinical practice have demonstrated that acupuncture exerts a beneficial effect in neurological and motor function recovery, including increased balance and muscle strength, and decreased spasticity [44, 45]. Clinical experience has indicated that fire-needle treatment takes less time, requires fewer visits, has more rapid results, and fewer side effects compared to chemical medicinal alternatives [46] At the same time, related clinical research has reported that fire-needle therapy was effective for sequelae of apoplexy [47, 48]. Most of the literature that was included in this study was published after 2015. Thus, the clinical and scientific focus on the use of fire needles has increased in China recently, confirming that fire needles are a reliable and reproducible treatment for post-stroke spasms. Therefore, we conducted this systematic review and meta-analysis of RCTs to summarize the safety and efficacy of fire-needle therapy versus conventional acupuncture used to treat post-stroke spasticity with respect to recovery outcomes.
Comprehensive analysis of our results presented a consistent trend that the use of fire needles was advantageous compared to conventional acupuncture in treating post-stroke spasms. The benefits included improvements in the effective rate, recovery rate, and improvements based on multiple scales represented by MAS. Moreover, there were no reports of serious adverse effects in any of the included studies, such as fainting, dizziness, or unstable blood pressure. This was similar to many clinical studies that have demonstrated the efficacy of conventional acupuncture on multiple sequelae of stroke [43]. In fact, guidelines for adult stroke rehabilitation and recovery recommend acupuncture for the treatment of stroke spastic paralysis. Therefore, we used conventional acupuncture as a control to comprehensively compare the advantages and disadvantages of fire acupuncture and provide valuable clinical evidence to show that fire acupuncture has unique advantages in relieving stroke spasms. Our results confirmed that fire needle treatment for post-stroke spasticity exerted better clinical effects compared to conventional acupuncture, which was consistent with previous clinical experiences and many current research conclusions [46] Also, the degree of improvement in the scores from FMA, BI, and NDS reflected that fire acupuncture decreased spasticity, and improved balance, accuracy, range of motion, and maintained stability in patients who had experienced a stroke.
One important finding was the high degree of heterogeneity among the different types of fire needles that were examined. There was no significant difference in the clinical efficacy of fire needles compared with conventional acupuncture with respect to the thickness of the fire needle diameter. Subgroup analysis revealed that when the fire needle depth exceeded 15mm, the fire needle was more efficient compared to conventional acupuncture [RR = 1.39, 95%CI ([1.09, 1,79), P = 0.009]. However, the improvement in the MAS score is not significant. [SMD = 0.21, 95% CI (-0.51, 0.93), P = 0.57].
The high heterogeneity of some results in the article cannot be ignored. Therefore, we conducted a meta-regression to find the source of heterogeneity. Based on clinical experience, we analyzed the following factors that may cause high heterogeneity, such as the type of stroke, and the location of spasm after stroke, the number of acupuncture points, the depth of acupuncture, and the frequency of treatment. However, the results of meta-regression suggest that none of the above factors is the cause of heterogeneity, but we can not rule out the influence of other uncontrollable factors, such as the period of stroke and the severity of stroke. Unfortunately, due to the fact that there are many missing values for these two factors in the included article, meta-regression cannot be performed, Therefore, we cannot analyze the impact of these two factors on heterogeneity. Future research should be as complete as possible to standardize the clinical application of fire needles and provide evidence for its further promotion.
Stroke is an acute cerebrovascular event, but the sequelae are chronic and persistent. Therefore, we conducted a subgroup analysis of studies that provided data on the course of stroke using MAS as a measurement indicator. Not surprisingly, fire needles exhibited excellent effects when the stroke duration was less than six months. However, when the stroke duration was longer than six months, results from fire needles were not different from conventional acupuncture. This result was consistent with the traditional understanding that a long duration of stroke did not present the best chances for recovery. However, only two studies were included in the subgroup analysis for which the stroke duration that was longer than six months and acupuncture depths that were more than 15mm. Thus, while the clinical implications should not be ignored, the subgroup analysis results should be treated with caution.
Based on traditional Chinese medicine theory, both conventional acupuncture and fire acupuncture act through adjusting the balance of human qi and blood, which, as a whole, produces therapeutic effects that alleviate and cure the diseases. Research has indicated that fire needle stimulation at lesions or acupoints can improve local blood circulation, enhance local tissue metabolism, and even eliminate the pathological changes in local tissues, including edema, hyperemia, exudation, adhesion, calcification, contracture, and ischemia. The results of fMRI studies have indicated that acupuncture therapy in patients with chronic hemiparetic stroke may exhibit modest improvements in upper limb function (specifically, spasticity and range of motion) by increasing ipsilesional motor cortex activity [49, 50]. Previous studies showed that fire needle acupuncture significantly increased BDNF expression, promoted endogenous NSC proliferation and differentiation into neurons, inhibited neuronal apoptosis, reduced inflammation by autophagy, and promoted recovery of motor neuron function [51, 52].
According to the current experimental research results and review, the mechanisms by which fire acupuncture produces antispasmodic effects after stroke are believed to be related to spasm-related neurotransmitters and receptors, and spasticity is relieved by increasing the expression of inhibitory transmitters or decreasing the expression of excitatory neurotransmitters [53]. Acupuncture also has been shown to protect central neurons in multiple ways to achieve functional restructuring of the CNS, which is crucial for strengthening central control of lower motor neurons that regulate muscle tension and to relieve muscle spasticity [54, 55].
Precise descriptions of the protocols used in acupuncture therapy are essential to enable replication and improve the transferability of the results. Generally, an acupuncture treatment plan for spasticity management should include a series of personalized and goal-oriented therapies that are tailored to the specific needs of each patient. As much as possible, we summarized the details of the acupuncture points and intervention details included in each study to provide clinicians with more options for acupuncture. The acupoints that appeared in our investigation with high frequency included the Yang-meridian, such as LI11-Quchi (nine times), LI4-Hegu (seven times), ST36-Zusanli (five times), and others. These results further verified the importance of regulating the Yang-meridian in the treatment of this disease. The result was consistent with the results of a relevant review published in 2017 [45]. Studies have shown that acupuncture in LI4 and LI11 affected local skin temperature and blood flow, while stimulation of LI11 and ST 36 were more likely to activate areas of the brain (frontal lobe, parietal lobe, sub-lobar lobe, cerebellum, and midbrain regions), causing ReHo value changes, which might promote recovery after stroke [56–58]. We also compared the key items reported in the included studies with those recommended by the Standards for Reporting Intervention in Clinical Trials of Acupuncture (STRICTA) guideline [38]. It should help clinicians and researchers to examine the standardized and more clearly described details of the studies included in this meta-analysis (Table 3). Interestingly, according to current research, acupuncture is a universally recognized non-drug treatment that can have a beneficial role in diseases that often accompany stroke, including depression, fatigue, and cognitive decline [59–61]. These observations also suggest that the efficacy of fire needles in the treatment of post-stroke spasticity may be underestimated.
This is the first meta-analysis to focus on the treatment of post-stroke spasms using fire needle acupuncture compared with conventional acupuncture. Although needle penetration depth and needle thickness are still controversial, our study should help to standardize fire needle treatment strategies for post-stroke spasms. We also expect our results to be adopted by policymakers and promote fire needle acupuncture as an alternative therapy to further reduce the burden of stroke on public health.
Limitation
Several limitations of our study should be noted. First, because of the specifics of the fire needle procedure, it was not possible to carry out blind studies. Thus, the quality of the included trials was not very high. Second, the sample size was not large enough, and the number of events was small (several subgroup analyses included only two studies), which may have influenced the reliability of the conclusions and their interpretation. Third, many factors led to the moderate heterogeneity of particular outcomes in the meta-analysis process, including individual differences, varied treatment protocols (including timing, type, duration, acupoints that were used, and intensity), the stroke type, lesion location, stroke duration, and the spasticity severity. Finally, as shown by the publication dates for the literature included in this study, fire needles, which were primarily used in China, had been widely used only for the past five years in clinical practice to treat post-stroke spasticity. There are very few scholars outside of China who have focused on fire needle treatment for post-stroke spasms, resulting in the majority of participants being Chinese. This result might limit the extrapolation of our conclusions to different populations to some extent. Moreover, dissemination of the results in English would be beneficial in moving this field forward because it would help increase the interests of clinicians and researchers in using and examining the effectiveness of fire acupuncture therapies for spasticity after stroke.
Conclusions
Although the sample size and some methodological qualities of the 16 RCTs included in the present study were not entirely satisfactory, we were able to demonstrate, to a limited extent, the efficacy of fire needle therapy for post-stroke spasticity. Acupuncture has been recommended by the World Health Organization (WHO) as an alternative and complementary strategy for stroke treatment and for improving stroke care. It is anticipated that future higher-quality RCTs will help determine the efficacy and provide reliable support for increased use of fire needles in the treatment of post-stroke spasms.
Supporting information
(DOCX)
(DOCX)
Acknowledgments
We thank Anrong Wang and sijia Cheng for helping to review the full-text articles for eligibility.
The authors would like to express their gratitude to EditSprings (https://www.editsprings.com/) for the expert linguistic services provided.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
(1) Zhuweifeng full name:Zhuweifeng Guangdong Provincial Famous Chinese Medicine Studio Construction Project Grant numbers:Guangdong Chinese Medicine Office 2018(5) (2) Zhaoxu Zhang full name:2020 Major Project of Science and Technology Project of Guangdong Province Traditional Chinese Medicine Bureau Grant numbers:(20203015) the funder play an role in the preparation of the manuscript (3) Zhaoxu Zhang full name:Science and technology development plan of Shandong Province Grant numbers:(2017G006021) the funder play an role in the preparation of the manuscript.
References
- 1.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis or the Global Burden of Disease Study 2010.Lancet. 2012;380(9859):2095–2128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sommerfeld DK, Eek EU, Svensson AK, et al. Spasticity after stroke: its occurrence and association with motor impairments and activity limitations. Stroke. 2004;35(1):134–139. 10.1161/01.STR.0000105386.05173.5E [DOI] [PubMed] [Google Scholar]
- 3.Rajsic S, Gothe H, Borba HH, et al. Economic burden of stroke: a systematic review on post-stroke care. Eur J Health Econ. 2019;20(1):107–134. 10.1007/s10198-018-0984-0 [DOI] [PubMed] [Google Scholar]
- 4.Wu S, Wu B, Liu M, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394–405. 10.1016/S1474-4422(18)30500-3 [DOI] [PubMed] [Google Scholar]
- 5.Wu P, Mills E, Moher D, Seely D. Acupuncture in poststroke rehabilitation: a systematic review and meta-analysis of randomized trials. Stroke. 2010;41(4):e171–e179. 10.1161/STROKEAHA.109.573576 [DOI] [PubMed] [Google Scholar]
- 6.Harrison RA, Field TS. Post stroke pain: identification, assessment, and therapy. Cerebrovasc Dis. 2015;39(3–4):190–201. 10.1159/000375397 [DOI] [PubMed] [Google Scholar]
- 7.Tang EY, Amiesimaka O, Harrison SL, et al. Longitudinal Effect of Stroke on Cognition: A Systematic Review. J Am Heart Assoc. 2018;7(2):e006443. Published 2018 Jan 15. 10.1161/JAHA.117.006443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lozano R, Naghavi M, Foreman K, et al. Treatment of Patients with Acute Stroke in Stroke Units (with or without Early Supported Discharge). Oslo, Norway: Knowled Centre for the Health Services at The Norwegian Institute of Public Health (NIPH); June 2010. [PubMed] [Google Scholar]
- 9.Burke JF, Lisabeth LD, Brown DL, Reeves MJ, Morgenstern LB. Determining stroke’s rank as a cause of death using multicause mortality data. Stroke. 2012;43(8):2207–2211. 10.1161/STROKEAHA.112.656967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lundström E, Smits A, Borg J, et al. Four-fold increase in direct costs of stroke survivors with spasticity compared with stroke survivors without spasticity: the first year after the event. Stroke. 2010;41(2):319–324. 10.1161/STROKEAHA.109.558619 [DOI] [PubMed] [Google Scholar]
- 11.Hara T, Abo M, Hara H, et al. The Effect of Repeated Botulinum Toxin A Therapy Combined with Intensive Rehabilitation on Lower Limb Spasticity in Post-Stroke Patients. Toxins (Basel). 2018;10(9):349. 10.3390/toxins10090349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dong Y, Wu T, Hu X, Wang T. Efficacy and safety of botulinum toxin type A for upper limb spasticity after stroke or traumatic brain injury: a systematic review with meta-analysis and trial sequential analysis. Eur J Phys Rehabil Med. 2017;53(2):256–267. 10.23736/S1973-9087.16.04329-X [DOI] [PubMed] [Google Scholar]
- 13.Do KH, Chun MH, Paik NJ, et al. Safety and efficacy of letibotulinumtoxinA(BOTULAX®) in treatment of post stroke upper limb spasticity: a randomized, double blind, multi-center, phase III clinical trial. Clin Rehabil. 2017;31(9):1179–1188. 10.1177/0269215516689331 [DOI] [PubMed] [Google Scholar]
- 14.Iskra DA, Kovalenko AP, Koshkarev MA, et al. Combination of central and peripheral muscle relaxants in the treatment of post-stroke spasticity. Zhurnal nevrologii i psikhiatrii imeni S.S. Korsakova. 2019;119(12.Vyp.2):51–57. 10.17116/jnevro201911912251 [DOI] [PubMed] [Google Scholar]
- 15.Zhu Y, Yang Y, Li J. Does acupuncture help patients with spasticity? A narrative review. Ann Phys Rehabil Med. 2019;62(4):297–301. 10.1016/j.rehab.2018.09.010 [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown D. A Review of the PubMed PICO Tool: Using Evidence-Based Practice in Health Education. Health Promot Pract. 2020;21(4):496–498. 10.1177/1524839919893361 [DOI] [PubMed] [Google Scholar]
- 18.Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. Published 2019 Aug 28. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 19.Hallgren KA. Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutor Quant Methods Psychol. 2012;8(1):23–34. 10.20982/tqmp.08.1.p023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nelson KP, Edwards D. A measure of association for ordered categorical data in population-based studies. Stat Methods Med Res. 2018;27(3):812–831. 10.1177/0962280216643347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Page MJ, McKenzie JE, Higgins JPT. Tools for assessing risk of reporting biases in studies and syntheses of studies: a systematic review. BMJ Open. 2018;8(3):e019703. Published 2018 Mar 14. 10.1136/bmjopen-2017-019703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng FY, Jia ZK, Jiang N. Study on Fire Needle Treatment of Lower Limb Spasm after Stroke Based on the Theory of Leading Yang from Yin[Chinese].Chinese Journal of Integrated Traditional Western Medicine On Cardiovascular. 2017;5(30):160–161. 10.16282/j.cnki.cn11-9336/r.2017.30.130 [DOI] [Google Scholar]
- 23.Yang ZQ, Yuan HN, Hang WF. Clinical Observation on Fire Needle Treatment of Spastic Hemiplegia after Stroke[Chinese]. Shenzhen Journal of Integrated Traditional Chinese and Western Medicine. 2017;27(20):60–61. 10.16458/j.cnki.1007-0893.2017.20.027 [DOI] [Google Scholar]
- 24.Sang P, Wang YH. Observation on the Therapeutic Effect of Fire Needling in the Treatment of Upper Limb Spasticity After Cerebral Infarction[Chinese].China Continuing Medical Education.2017;9(32):108–111. [Google Scholar]
- 25.Liu Q, Zhou HF, Zhang W, et al. Clinical Observation on Filiform-fire Needing at Jiaji Points in Treating Post-stroke Upper-limb Spastic Paralysis [Chinese]. Journal of Guangzhou University of Traditional Chinese Medicine. 2018,35(03):430–435. 10.13359/j.cnki.gzxbtccm.2018.03.011 [DOI] [Google Scholar]
- 26.Chai FC. Observation of Clinical Curative Effect of Fire Needle Treating Spasticity of Stroke[Chinese]. Shanxi Journal of Traditional Chinese Medicine.2017 [Google Scholar]
- 27.Wang YH. Clinical Study on the Treatment of Spasticity after Cerebral Infarction by intermuscular Fire needling[Chinese]. Heilongjiang Journal of Traditional Chinese Medicine.2018. 32185998 [Google Scholar]
- 28.Deng Y, Liu Y. Clinical Observation of Applying Milli Fire Neddle Therapy Based on the Rules of Treatment of Regulating Qi and Blood, Warming Yang and Ventilating Qi in the Treatment of Spastic Hemiplegia[Chinese].Journal of Sichuan Traditional Chinese Medicine. 2019;35(01):186–189 [Google Scholar]
- 29.Peng FY, Jia ZK, Jiang N. Comparative analysis of the effect of vast, Guan-needling and conventional acupuncture on upper limb spasticity after stroke[Chinese]. Chinese Journal of Integrated Traditional Western Medicine On Cardiovascular.2017;5(12):84–85. 10.16282/j.cnki.cn11-9336/r.2017.12.065 [DOI] [Google Scholar]
- 30.Sheng GY, Zhao QL. Application of fire needle in the treatment of spastic hemiplegia after stroke[Chinese]. Nei Mongol Journal of Traditional Chinese Medicined. 2017;36(14):doi:115.10.16040/j.cnki.cn15-1101.2017.14.115 [Google Scholar]
- 31.Xu YY, Liao MX. Clinical observation of filiform fire needling in treating 40 cases of spastic hemiplegia after stroke[Chinese].Jiangsu Journal of Traditional Chinese Medicine. 2015;47(02):63–64. [Google Scholar]
- 32.Wang N, Li ZF, Wu HH. Clinical Observation on therapeutic Effect of Red-hot Needle Therapy for Spastic Hemiplegia in Stroke Patients[Chinese].Acupuncture Research. 2015;40(04):304–308. 10.13702/j.1000-0607.2015.04.009 [DOI] [PubMed] [Google Scholar]
- 33.Yuan BG. Clinical Efficacy on Milli-fire needle treatment of stroke spastic paralysis[Chinese]. Journal of Guangzhou University of Traditional Chinese Medicine.2015 [Google Scholar]
- 34.Liu Y. Clinical curative effect of reinforcing Yang and reducing yin by fire needle on post-stoke upper-limb muscular hypertonia[Chinese]. Journal of Fujian University of Traditional Chinese Medicine.2014. [Google Scholar]
- 35.Zhao MH, Qian H, Zhuang LX. Observation on the clinical curative effect of fire-acupuncture on Baxie and Shangbaxie points in treating finger contracture after stroke[Chinese]. Journal of Guangzhou University of Traditional Chinese Medicine.013;30(02):175–178. 10.13359/j.cnnki.gzxbtcm.2013.02.010 [DOI] [Google Scholar]
- 36.Chen JZ. Clinical Observation on Fire Needle Treatment of Sequelae of Stroke[Chinese]. Journal of Guangzhou University of Traditional Chinese Medicine.2005. [Google Scholar]
- 37.Gao TY, Mei FH, Duan WQ, et al. Evaluation of the effect of fire needle on upper limb spasm after stroke[Chinese]. Nei Mongol Journal of Traditional Chinese Medicine.2004;05:7–8. 10.13359/j.cnki.gzxbtcm.2013.02.010 [DOI] [Google Scholar]
- 38.MacPherson H, Altman DG, Hammerschlag R, et al. Revised Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. Journal of evidence-based medicine 2010;3(3):140–155. 10.1111/j.1756-5391.2010.01086.x [DOI] [PubMed] [Google Scholar]
- 39.Kamalakannan S, Gudlavalleti ASV, Gudlavalleti VSM, et al. Incidence & prevalence of stroke in India: a systematic review. Indian Journal Of Medical Research 2017;146(2):175–185. 10.4103/ijmr.IJMR_516_15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marcheschi E, Von Koch L, Pessah-Rasmussen H, et al. Home setting after stroke, facilitators and barriers: a systematic literature review. Health and Social Care in the Community 2018;26(4):e451–e459. 10.1111/hsc.12518 [DOI] [PubMed] [Google Scholar]
- 41.Li Z, Alexander SA. Current evidence in the management of poststroke hemiplegic shoulder pain: a review. Journal Of Neuroscience Nursing 2015;47(1):10–19. 10.1097/JNN.0000000000000109 [DOI] [PubMed] [Google Scholar]
- 42.Chau JPC, Lo SHS, Yu X, et al. Effects of Acupuncture on the Recovery Outcomes of Stroke Survivors with Shoulder Pain: A Systematic Review. Frontiers in Neurology.2018;9:30. 10.3389/fneur.2018.00030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhu W, Ye Y, Liu Y, et al. Mechanisms of acupuncture therapy for cerebral ischemia: an evidence-based review of clinical and animal studies on cerebral ischemia. Journal of neuroimmune pharmacology 2017;12(4):575–592. 10.1007/s11481-017-9747-4 [DOI] [PubMed] [Google Scholar]
- 44.Wang J, Zhai Y, Wu J, et al. Acupuncture for Chronic Urinary Retention due to Spinal Cord Injury: A Systematic Review. Evidence-based complementary and alternative medicine 2016; 9245186. 10.1155/2016/9245186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chavez LM, Huang SS, MacDonald I, et al. Mechanisms of Acupuncture Therapy in Ischemic Stroke Rehabilitation: A Literature Review of Basic Studies. International journal of molecular sciences 2017;18(11):2270. 10.3390/ijms18112270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yue XY, Feng ZQ, Yu XY, et al. Fire-needle acupuncture for upper limb spastic paralysis after stroke: Study protocol for a randomized controlled trial. Journal of integrative medicine 2019;17(3):167–172. 10.1016/j.joim.2019.03.002 [DOI] [PubMed] [Google Scholar]
- 47.Wang N, Li Z. Life quality improvement of spastic hemiplegia of stroke treated with fire-needle: a randomized controlled trial[Chinese]. Zhongguo Zhen Jiu. 2015;35(11):1105–1109. [PubMed] [Google Scholar]
- 48.Yuan Y, Qian XL, Yan WM, Zhou S. Fire needling on dysphagia due to pseudobulbar palsy after stroke: a randomized controlled trial[Chinese]. Zhongguo Zhen Jiu.2020; 40(4):347–51. 10.13703/j.0255-2930.20190502-0003 . [DOI] [PubMed] [Google Scholar]
- 49.Schaechter JD, Connell BD, Stason WB. Correlated change in upper limb function and motor cortex activation after verum and sham acupuncture in patients with chronic stroke. The journal of alternative and complementary medicine.2007;13(5):527–532. 10.1089/acm.2007.6316 [DOI] [PubMed] [Google Scholar]
- 50.Wu Z, Hu J, Du F, et al. Long-term changes of diffusion tensor imaging and behavioural status after acupuncture treatment in rats with transient focal cerebral ischaemia. Acupuncture in Medicine 2012;30(4):331–338. 10.1136/acupmed-2012-010172 [DOI] [PubMed] [Google Scholar]
- 51.Xu J, Cheng S, Jiao Z. Fire Needle Acupuncture Regulates Wnt/ERK Multiple Pathways to Promote Neural Stem Cells to Differentiate into Neurons in Rats with Spinal Cord Injury. CNS & Neurologica isorders-Drug Targets 2019;18(3):245–255. 10.2174/1871527318666190204111701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu J, Wu Y. Electro-acupuncture-modulated miR-214 prevents neuronal apoptosis by targeting Bax and inhibits sodium channel Nav1.3 expression in rats after spinal cord injury. Biomed Pharmacother. 2017;89:1125–1135. 10.1016/j.biopha.2017.02.077 [DOI] [PubMed] [Google Scholar]
- 53.Liu C, Li R, Song X. Effect of catgut implantation at acupoints on GABA(B) and mGluR1 expressions in brain stem of rats with spasticity after stroke. Journal of Traditional Chinese Medicine 2014;34(5):566–571. 10.1016/s0254-6272(15)30064-9 [DOI] [PubMed] [Google Scholar]
- 54.Shi LH, Guo LX, Zhang HL, et al. Acupuncture for poststroke spasticity: A protocol of a systematic review and meta-analysis. Medicine (Baltimore). 2019;98(39): e17124. 10.1097/MD.0000000000017124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li J, He J, Du Y, et al. Electroacupuncture improves cerebral blood flow and attenuates moderate ischemic injury via Angiotensin II its receptors-mediated mechanism in rats. BMC Complementary and Alternative Medicine 2014;14:441. 10.1186/1472-6882-14-441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li W, Ahn A. Effect of Acupuncture Manipulations at LI4 or LI11 on Blood Flow and Skin Temperature. Journal of acupuncture and meridian studies. 2016;9(3):128–133. 10.1016/j.jams.2015.08.005 [DOI] [PubMed] [Google Scholar]
- 57.Xie G, Yang S, Chen A, et al. Electroacupuncture at Quchi and Zusanli treats cerebral ischemia-reperfusion injury through activation of ERK signaling. Exp Ther Med. 2013;5(6):1593–1597. 10.3892/etm.2013.1030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen SQ, Cai DC, Chen JX, et al. Altered Brain Regional Homogeneity Following Contralateral Acupuncture at Quchi (LI 11) and Zusanli (ST 36) in Ischemic Stroke Patients with Left Hemiplegia: An fMRI Study. Chinese Journal of Integrative Medicine.2020;26(1):20–25. 10.1007/s11655-019-3079-6 [DOI] [PubMed] [Google Scholar]
- 59.Wang S, Yang H, Zhang J. Efficacy and safety assessment of acupuncture and nimodipine to treat mild cognitive impairment after cerebral infarction: a randomized controlled trial. BMC Complementary and Alternative Medicine 2016;16(1):361. 10.1186/s12906-016-1337-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen LY, Yen HR, Sun MF, Lin CL, Chiang JH, Lee YC. Acupuncture treatment is associated with a decreased risk of developing stroke in patients with depression: A propensity-score matched cohort study. J Affect Disord. 2019;250:298–306. 10.1016/j.jad.2019.03.020 [DOI] [PubMed] [Google Scholar]
- 61.Chen L, Fang J, Ma R. Additional effects of acupuncture on early comprehensive rehabilitation in patients with mild to moderate acute ischemic stroke: a multicenter randomized controlled trial. BMC Complementary and Alternative Medicine 2016;16(1):226. 10.1186/s12906-016-1193-y [DOI] [PMC free article] [PubMed] [Google Scholar]