Abstract
The abnormal thickening of the gallbladder (GB) wall can be caused by a malignant condition like gallbladder carcinoma or by benign lesions such as chronic cholecystitis or xanthogranulomatous cholecystitis (XGC). Mural thickening is a common finding between them as fluorodeoxyglucose (FDG) can be taken up by inflammatory cells also. Here, we present a patient with irregular thickening of the GB wall which was suspected to of GB carcinoma since FDG positron emission tomography/computed tomography scan showed increased tracer uptake in the lesion. However, after surgery the histopathological report was suggestive of XGC.
Keywords: Gallbladder cancer, positron emission tomography/computed tomography scan, xanthogranulomatous cholecystitis
INTRODUCTION
Based on imaging, it can be difficult to differentiate between xanthogranulomatous cholecystitis (XGC) and gall bladder carcinoma by ultrasonography (USG), computed tomography scan, or fluorodeoxyglucose (FDG) positron emission tomography-computed tomography (PET-CT) scan. The common feature of mural thickening on conventional imaging and nonspecific FDG uptake on PET/CT scan makes it very difficult to differentiate between these benign and malignant conditions. Histopathology remains the gold standard for these conditions. Our case highlights the common imaging characteristics of mural thickening and few distinct criteria developed on CT to differentiate between them and pitfall of FDG due to nonspecific uptake in inflammatory cells also apart from malignant tissue.
CASE REPORT
A 71-year-old female presented with pain abdomen and fever since 3 months. USG was suggestive of thickened gallbladder wall. Thus, in view of suspicion of malignancy, the patient was referred for PET-CT scan. Whole-body 18F-FDG PET/CT scan was suggestive of cholelithiasis with intensely FDG avid [Figure 1a–g] circumferential nodular mural thickening in gall bladder, more in the fundus region, showing loss of fat planes with the adjacent liver with small hypodense areas within (arrows). Thus, in view of suspicion of malignancy, cholecystectomy was planned. The histopathology [Figure 2] showed gallbladder mucosa was completely ulcerated with only few foci of flattened mucosa. There was very dense chronic and xanthogranulomatous inflammation in wall suggestive of acute on chronic cholecystitis with xanthogranulomatous inflammation.
Figure 1.
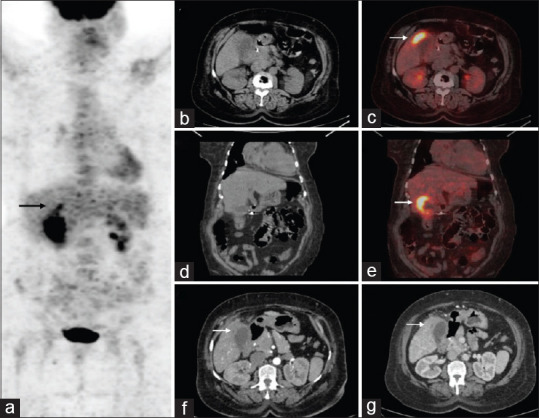
Maximum intensity projection (a) of whole body fluorodeoxyglucose positron emission tomography/computed tomography scan. Axial and coronal computed tomography and fused positron emission tomography/computed tomography (b-e) Images showing fluorodeoxyglucose avid nodular mural thickening, more in the neck and fundus of gallbladder abutting the adjacent hepatic parenchyma. Axial computed tomography arterial and portovenous phases (f-g) showing asymmetric thickening of gallbladder wall in fundus region, with hypodense areas within, abutting adjacent liver
Figure 2.
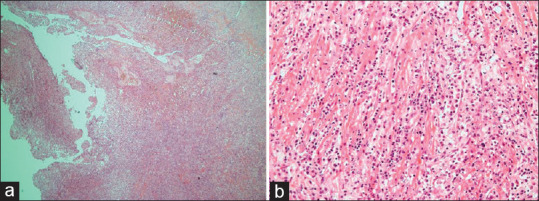
Gallbladder with ulcerated surface epithelium. Wall shows dense mixed inflammatory infiltrate rich in histiocytes (a, H and E × 101). Gallbladder wall shows dense mixed inflammatory infiltrate rich in histiocytes, diffusely infiltrating into the muscle (b, H and E × 200)
DISCUSSION
XGC is a rare chronic gallbladder (GB) disease which is characterized by the proliferation of xanthoma within the GB wall.[1] Macroscopically, it appears like yellowish tumor like mass in the wall of the gall bladder. It is an infrequent chronic granulomatous inflammation of the gall bladder, first described by Christensen and Ishak in 1970 as “Fibroxanthogranulomatous inflammation.”[2] The term XGC was coined by McCoy et al. in 1976.[3] Although it is a benign disease, it is often mistaken as GB carcinoma due to the thickened GB wall. Histologically, the rupture of the Rokitansky-Aschoff sinuses, causes an inflammatory reaction, which can infiltrate adjacent organs, forming dense adhesions. It is a variant of cholecystitis. Extravasation of bile into the GB wall is supposedly the initiating event in the pathogenesis of XGC, which later triggers an inflammatory process that might be acute or chronic. The imaging characteristics reported for XGC are a continuous mucosal line in a thickened GB wall, an intramural GB wall nodule, and the presence of gallstones on a background of chronic GB disease.[4] Because of the similarity to gall bladder cancer in clinical manifestations and radiological findings, makes it difficult to distinguish between them.
Few articles have been published describing the similarities and differences between XGC from gallbladder cancer[5,6] and few reports about false-positive results on FDG-PET/CT scan.[7] Several studies have shown the strong association between gallstones and XGC,[8] as seen in our case. Ultrasound and CT scan may show nonspecific GB wall thickening. The presence of diffuse GB wall thickening, continuous mucosal line, intramural hypoattenuated nodules, absence of macroscopic hepatic invasion, and lack of intrahepatic biliary dilation on CT scan could help differentiate XGC from GB cancer with sensitivity and specificity of 83% and 100%, respectively, when three of these five findings are observed.[9] FDG-PET/CT scan is helpful in differentiating between benign and malignant lesions with sensitivity and specificity ranging from 75% to 78% and 82% to 100%, respectively, for the detection of GB cancer.[10] However, numerous cases of false-positive results have been seen because inflammatory cells in XGC also have high rates of glucose metabolism similar to malignant cells.[11] Thus, XGC is a rare, benign, chronic inflammation of the GB that has clinical, radiological, and intraoperative features similar to that of GB cancer and only histopathology can definitively differentiate the two conditions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patient understands that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zhuang PY, Zhu MJ, Wang JD, Zhou XP, Quan ZW, Shen J. Xanthogranulomatous cholecystitis: A clinicopathological study of its association with gallbladder carcinoma. J Dig Dis. 2013;14:45–50. doi: 10.1111/j.1751-2980.2012.00645.x. [DOI] [PubMed] [Google Scholar]
- 2.Christensen AH, Ishak KG. Benign tumors and pseudotumors of the gallbladder. Report of 180 cases. Arch Pathol. 1970;90:423–32. [PubMed] [Google Scholar]
- 3.McCoy JJ, Jr, Vila R, Petrossian G, McCall RA, Reddy KS. Xanthogranulomatous cholecystitis. Report of two cases. J S C Med Assoc. 1976;72:78–9. [PubMed] [Google Scholar]
- 4.Zhao F, Lu PX, Yan SX, Wang GF, Yuan J, Zhang SZ, et al. CT and MR features of xanthogranulomatous cholecystitis: An analysis of consecutive 49 cases. Eur J Radiol. 2013;82:1391–7. doi: 10.1016/j.ejrad.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 5.Bo X, Chen E, Wang J, Nan L, Xin Y, Wang C, et al. Diagnostic accuracy of imaging modalities in differentiating xanthogranulomatous cholecystitis from gallbladder cancer. Ann Transl Med. 2019;7:627. doi: 10.21037/atm.2019.11.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ewelukwa O, Ali O, Akram S. Xanthogranulomatous cholecystitis mimicking gallbladder cancer. BMJ Case Rep. 2014;2014:bcr2013200530. doi: 10.1136/bcr-2013-200530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Makino I, Yamaguchi T, Sato N, Yasui T, Kita I. Xanthogranulomatous cholecystitis mimicking gallbladder carcinoma with a false-positive result on fluorodeoxyglucose PET. World J Gastroenterol. 2009;15:3691–3. doi: 10.3748/wjg.15.3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han SH, Chen YL. Diagnosis and treatment of xanthogranulomatous cholecystitis: A report of 39 cases. Cell Biochem Biophys. 2012;64:131–5. doi: 10.1007/s12013-012-9381-y. [DOI] [PubMed] [Google Scholar]
- 9.Goshima S, Chang S, Wang JH, Kanematsu M, Bae KT, Federle MP. Xanthogranulomatous cholecystitis: Diagnostic performance of CT to differentiate from gallbladder cancer. Eur J Radiol. 2010;74:e79–83. doi: 10.1016/j.ejrad.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 10.Anderson CD, Rice MH, Pinson CW, Chapman WC, Chari RS, Delbeke D. Fluorodeoxyglucose PET imaging in the evaluation of gallbladder carcinoma and cholangiocarcinoma. J Gastrointest Surg. 2004;8:90–7. doi: 10.1016/j.gassur.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Sawada S, Shimada Y, Sekine S, Shibuya K, Yoshioka I, Matsui K, et al. Expression of GLUT-1 and GLUT-3 in xanthogranulomatous cholecystitis induced a positive result on (18)F-FDG PET: Report of a case. Int Surg. 2013;98:372–8. doi: 10.9738/INTSURG-D-13-00092.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


