Abstract
A large body of research links wealth and health, but most previous work focuses on net worth. However, the assets and debts that comprise wealth likely relate to health in different and meaningful ways. Further, racial differences in wealth portfolios may contribute to racial health gaps. Using longitudinal data from the Panel Study of Income Dynamics (PSID) and mixed effects growth curve models, we examine the associations between various wealth components and multiple health outcomes. We also investigate whether Black-White differences in wealth portfolios contribute to racial health inequality. We find that savings, stock ownership, and homeownership consistently improve health, but debt is associated with worse health, even after adjusting for total net worth. We find little evidence that home equity is associated with health. Findings also reveal differential health returns to assets by race. These findings provide new insights into the complex relationship among race, wealth, and health.
Keywords: wealth, racial health disparities, life course and aging, debt, assets
INTRODUCTION
An extensive body of research documents stark and persistent racial disparities in health, with Black Americans being more likely than White Americans to experience disease, death, and disability from a range of conditions, including various types of cancer, strokes and other cardiovascular events, and complications from diabetes (Williams et al. 2010). This research provides clear evidence that Black-White health disparities reflect racial differences in the accumulation of psychological, social, and environmental exposures across the life course, including socioeconomic exposures. Because socioeconomic status (SES) is a fundamental determinant of health (Link and Phelan 1995) and strongly patterned by race (Kochhar et al. 2011), the racial patterning of socioeconomic resources is a key pathway linking racism and population health (Phelan and Link 2015). Consistent with this notion, studies show that Black-White health gaps are, in large part, generated from race differences in SES (Boen 2016; Brown 2018; Hayward et al. 2000).
In particular, a growing body of literature links wealth and health (Boen and Yang 2016). Wealth cushions households from economic hardship brought on by unemployment or illness; allows households to continue paying rents or mortgages, car payments, and other bills even when wages are temporarily suspended; and can support the health needs of individuals who have exited the paid labor force (Boen and Yang 2016; Spilerman 2000). Wealth accumulation is also a status attainment process in which individuals accumulate wealth over their lives and pass resources (and usually class status) to their descendants (Oliver and Shapiro 2006). Importantly, racial wealth inequality is extreme; Black Americans own approximately 5 cents for every dollar of White wealth (Kochhar et al. 2011), a disparity that reflects the accumulation of historical and contemporary racial discrimination and exclusion across political and institutional spheres (Darity et al. 2018; Oliver and Shapiro 2006). Building on evidence that racial wealth inequality persists across both historical time (Pfeffer, Danziger, and Schoeni 2013) and the life course (Brown 2016), research documents that the Black-White wealth gap is an essential determinant of Black-White health disparities, net of race differences in other socioeconomic indicators (Boen 2016; Bond Huie et al. 2003; Kim and Miech 2009).
Despite important advances in research on race, wealth, and health, three critical gaps remain in the literature. First, previous research focuses on the association between total wealth—operationalized as net worth, or the sum of total assets net of debts—and health, yet the components of wealth likely relate to health in different ways. Importantly, asset ownership is likely to be associated differently with health than having debt, and understanding these different relationships could help clarify the mechanisms underlying the wealth-health association. Similarly, different types of assets are likely to be associated with health in different ways. An important distinction in how assets may differentially affect health is liquidity. The more liquid an asset, the more easily it can be converted to cash and used to support healthy behaviors and lifestyles and pay for medical treatment. In their review on the state of wealth inequality research, Killewald, Pfeffer, and Schachner (2017) emphasize this gap in our understanding of the links between wealth and well-being and call for new research on the varying consequences of different wealth components on outcomes such as health. To date, however, few studies assess the association between various wealth components and health. Second, the wealth portfolios of Black Americans and White Americans vary greatly (Keister 2000a; Killewald, Pfeffer, and Schachner 2017), but it is unclear whether racial differences in wealth components contribute to Black-White health gaps. Finally, there is evidence that Black and White individuals receive different health returns to socioeconomic resources—including wealth (Finnigan 2014)—but it is unclear whether racial differences in the health returns to different wealth components factor into Black-White health gaps.
We fill these gaps by integrating insights from the vast literatures on racial and socioeconomic health inequality, wealth accumulation, and the life course perspective to study how various dimensions of wealth are associated with individual health and racial health gaps across six outcomes, including self-rated health, chronic conditions, work limitations, disability risk, psychological distress, and body mass index. We have three objectives. First, we examine how wealth components, including homeownership, home equity, savings, stock investments, and debt, are differently associated with each health outcome. Second, we assess whether racial differences in wealth portfolios contribute to Black-White disparities in the outcomes. Finally, we examine whether Black and White individuals receive similar health returns to different wealth components, thereby providing a more nuanced understanding of the racialized nature of the socioeconomic gradient in health. Whereas most previous research on wealth and health uses cross-sectional data or data on older adult samples, we use longitudinal data and mixed effects growth curve models to reduce concerns about reverse causality.
We find that the components of net worth are, indeed, associated with health in different ways and that the associations vary by the health outcome in question. For example, homeownership, savings, stock ownership are consistently protective of health, but debt is associated with worse health. We find little evidence that home equity is associated with health once other factors are controlled, despite home equity being a key dimension of net worth for most American households. Adjusting for racial differences in total wealth substantially reduces Black-White health gaps across outcomes, and racial differences in wealth portfolios play a particularly salient role in shaping racial disparities in self-rated health, chronic conditions, and disability. We also find that the associations between assets and health sometimes vary by race, with important implications for research and policy. Together, these findings provide a more nuanced understanding of the links between race and racism, wealth accumulation, and racial health disparities and offer new insights into how wealth-generating policies could also most effectively reduce health inequality.
BACKGROUND
Wealth and Health
There is a clear socioeconomic gradient in health, with declines in SES being associated with increased morbidity and mortality from a host of causes (Link and Phelan 1995). SES shapes exposure to risks and toxins, access to goods and resources, and opportunities in ways that promote or harm health (Marmot 2004). Wealth is a particularly strong correlate of individual health and population health inequality, net of other SES indicators such as income and education (Boen 2016; Boen and Yang 2016; Hajat et al. 2010; Sweet et al. 2013). The association between wealth and health persists across health outcomes including self-rated health, BMI, systolic blood pressure, and C-reactive protein (Boen 2016; Boen and Yang 2016). The tendency for wealth inequality to increase over the life course (Brown 2016) is a particularly important factor explaining racial health gaps that increase with age, a pattern that is not attenuated by educational attainment or income (Boen 2016; Shuey and Willson 2008). Quasi-natural experiments linking external wealth shocks from the Great Recession (Boen and Yang 2016) and lottery winnings (Cesarini et al. 2016) to health outcomes suggest that the wealth-health link may, indeed, be causal.
Scholars theorize that three mechanisms link wealth and health (Boen and Yang 2016), though these mechanisms are rarely tested empirically. First, wealth affects household consumption in ways that affect health (Sousa 2009). Households with more liquid assets can afford better medical care, higher quality health insurance, leisure and physical activity, and other opportunities, resources, and goods that can promote physical and mental health and reduce disease burden. Conversely, when household budgets tighten in response to financial insecurity, consumption on health-related goods and services declines in ways that negatively affect long-term well-being (Charron-Chénier, Fink, and Keister 2016; Lusardi, Schneider, and Tufano 2010; Wall, Vujicic, and Nasseh 2012). There is evidence, for example, that when budgets tighten in response to economic challenges, households reduce spending on medical care (Lusardi, Schneider, and Tufano 2010), groceries (Rose 1999), and other health-related goods and resources linked to a variety of physical and mental health outcomes. Second, time use may mediate the association between wealth and health (Burgard, Ailshire, and Kalousova 2013; Catalano et al. 2011; Mani et al. 2013). Households with more wealth may not need to spend as much time as lower wealth households in paid work and can outsource household labor, leaving them more time for health-promoting activities (e.g., socializing, physical activity). By contrast, households with fewer assets or high debt may need to allocate more time and energy to the paid labor market and to unpaid household labor and care work in ways that could affect health. Finally, wealth-related stress can affect health (Yilmazer, Babiarz, and Liu 2015). Low assets or high debt can increase anxiety, frustration, and hopelessness (Drentea and Reynolds 2014). High levels of financial strain increase physiological dysregulation and that Black-White differences in financial stress mediate racial disparities in disease risk (Boen 2019). Low levels of wealth may also contribute to health deterioration because of stress related to feelings of subordination and lack of control over important life decisions (Cutler, Lleras-Muney, and Vogl 2008). In addition to the stress of low wealth ownership or high debt, there may also be health gradients among the relatively wealthy due to stress, whereby households with riskier portfolios experience more stress than households that own more stable assets. Together, exposure to the variety of wealth-related stressors can chronically upregulate physiological and psychological functioning over time in ways that increase health and disease risk from a host of causes (McEwen 1998).
The Racial Wealth Gap and Population Health Inequality
Racial disparities in wealth are an important contributor to Black-White health gaps (Boen 2016; Bond Huie et al. 2003; Kim and Miech 2009). Racial wealth gaps in the United States are striking: the median net worth of White households is roughly 20 times that of Black households (Kochhar et al. 2011). Contemporary racial disparities in wealth reflect the persistent effects of racially exclusionary policies and institutional practices as well as present day racial discrimination and oppression. The exclusion of agricultural and domestic workers—many of whom were Black—from receiving Social Security benefits; redlining practices by the Home Owners’ Loan Corporation; and racially restrictive lending policies of the Federal Housing Authority in the years following World War II are just a few examples of historical policies and practices that prevented Blacks in the U.S. from accumulating wealth in the same ways as Whites (Oliver and Shapiro 2006). Contemporary racial discrimination in the housing, lending, and labor markets further exacerbates racial wealth inequality (Gaddis 2015; Grodsky and Pager 2001; Rugh forthcoming) and contributes to racial health disparities. For example, homes in highly segregated Black neighborhoods appreciate more slowly than homes in predominately White neighborhoods, which negatively impacts Black wealth holdings (Flippen 2004). In addition, lenders disproportionately target Black families with subprime mortgages, a pattern which contributed to the tremendous loss of Black household wealth during the Great Recession (Farber 2013). In these ways, racial wealth inequality is a key pathway linking structural and institutional racism to population health inequality.
Importantly, wealth accumulation is a life course and intergenerational status attainment process. Individuals accumulate wealth as they age and can pass their assets—net of debts—to descendants. Families draw on their wealth to create opportunities for offspring, secure a desired standard of living, and pass along class status to future generations (Oliver and Shapiro 2006). As a result, racial wealth inequality reflects a form of cumulative disadvantage (Brown 2016): Black-White wealth inequality emerges early in the life course due to racial differences in familial wealth; widens across the life span as Whites experience more rapid rates of wealth accumulation than Blacks; and persists across generations and historical time as families unequally pass along wealth to their descendants. In these ways, the racial wealth gap plays an essential role in the persistence of racial stratification across the life course and historical time in ways that shape population health patterns (Sewell 2016).
STUDY EXPECTATIONS
Wealth Components and Health
Despite increased scholarly attention to the links among wealth, race, and health, important questions about the role of wealth in population health remain unanswered. Two broad patterns motivate our expectations. First, the assets and debts that comprise net worth likely relate to health in ways that differ from each other and from total net worth. For a typical household, net worth is a vague, abstract term that has little bearing on their day-to-day experiences, but the assets and debts that are included in net worth can be meaningful and consequential. Homeownership is an important example. Owning a home provides a degree of financial and psychological security (Finnigan 2014; Yilmazer, Babiarz, and Liu 2015) that leads it to be the asset most people want to own before others, particularly for low-income households (Keister 2008). Historically, homeownership has been an important indicator of class status and achievement (Rossi and Weber 1996), suggesting that homeownership may be associated with health outcomes by improving both objective and subjective social standing and reducing stress. Home equity—home value less mortgage debt on the home—is also important to a household’s financial security, but it is unlikely that home equity has a clear, direct association with health. For most households, home equity is a vague notion. Even if a homeowner has a sense of the current market value of their home, the real market value may differ dramatically from that estimate. Most importantly, home equity is not liquid. Home equity loans give homeowners access to the equity, and home equity has long-term benefits as it can be used to fund expenses after home is sold (e.g., retirement); however, in the short-run, there is likely to be very little effect of home equity on health.
Financial assets and debts are also likely to be associated with health, but for different reasons. The association between financial assets—including cash savings and other investments—and health is likely to be strong and positive. Because financial assets are liquid, they are likely to be positively associated with health through each of the three mechanisms that link wealth and health. Financial assets can support consumption of the goods and services that improve health; they can pay for medical care and health insurance, create a financial buffer against income interruptions, and create a safe and pleasant living environment (Spilerman 2000). Owning financial assets may offer households more time to allocate to health-promoting activities and reduce the stress that accompanies asset poverty. By contrast, the association between debt and health is likely to be strong and negative (Drentea and Reynolds 2014). Debt could be used to fund health-promoting forms of consumption; households can acquire debt for asset investment purposes (e.g., purchasing a home) or to fund human capital investments (e.g., paying for college) in ways that support health. Still, research suggests that debt generates stress that is likely to overshadow any benefits that its use creates (Turunen and Hiilamo 2014). In particular, studies link unsecured consumer debt to poor health (Berger and Houle 2019). Interest rates on these types of debt are often especially high, making it difficult for debtors to pay off principle (Hodson, Dwyer, and Neilson 2014), which may make these types of unsecured debts particularly stressful and harmful for health.
Racial Wealth Inequality and Black-White Health Disparities
The second broad pattern that motivates our expectations is that the wealth portfolio of the average Black household differs markedly from the portfolio of the average White household at all levels of income, education, and family background. Given potentially differing associations between wealth components and health, Black-White differences in wealth portfolios may contribute to racial disparities in health, though this is largely unknown. Black-White differences in homeownership and home equity are well-documented: Black households are less likely to own homes than White households, have lower home equity when they own homes, and accumulate value in their homes more slowly than White households (Killewald and Bryan 2018; Krivo and Kaufman 2004). Ownership of financial assets also differs between Black and White households. Black households are less likely than White households to have non-zero cash savings and to invest in stocks and other financial assets; when Black households hold these financial assets, their holdings tend to be less valuable than those of White households (Gittleman and Wolff 2004; Keister 2000, 2004, 2014). These differences hold when income, education, family background, and other correlates of asset ownership and value are controlled. Debts are also important: when income, education, family background, and other correlates of debt are controlled, Black households tend to have more debt than White households—including mortgages, consumer debt, student loans, and other forms of debt—at least partly because their saved assets are lower (Killewald and Bryan 2018). In the case of student debt—an increasingly heavy burden for many households—Black students take on greater debt than their White counterparts largely because their parents are less able to cover the financial costs associated with college (Houle 2014). These race differences in wealth composition do not reflect individual preferences but rather stem from the broader structure of racial stratification in the US that has patterned access to financial opportunities and resources by race (Darity et al. 2018).
It is also possible that Black and White individuals receive different health returns to various wealth components. There is evidence that Blacks receive fewer protective health benefits from socioeconomic resources than Whites (Boen 2016; Finnigan 2014; Shuey and Willson 2008). Differences in labor market experiences and workplace exposures; disparities in early life socioeconomic exposures and related differential exposure to the stressors associated with upward mobility; contextual disadvantages associated with poverty and residential segregation; and differences in exposure to racial discrimination—including particularly high levels of racial discrimination among higher SES Black Americans—are some of the proposed mechanisms preventing Black individuals from converting asset gains into health improvements in the same way as Whites (Assari 2018; Gaydosh et al. 2018; Pearson 2008). There is widespread evidence of differential returns to income and education by race [see Assari (2018) for a review]. Still, less is known about whether Blacks and Whites experience the same health returns to wealth components. Indeed, Black homeowners do not receive the same health benefits associated with homeownership as Whites and differences in neighborhood characteristics, loan terms, and ownership insecurity may contribute to these patterns (Finnigan 2014). Still, more research in this area is needed, as failing to account for racial heterogeneity in the associations between different dimensions of wealth and health may result in misestimating the role of wealth in racial health disparities (Pearson 2008).
Expectations
Using nationally representative, longitudinal data, we examine how different components of net worth—including particular assets and debt—are associated with diverse indicators of health. We also assess how Black-White differences in wealth portfolios contribute to racial health gaps as individuals age. We have five broad expectations:
H1: Liquid assets are more strongly associated with the health outcomes than illiquid assets.
H2: Debt is negatively associated with health.
H3: Race differences in wealth composition mediate Black-White health gaps.
H4: Black respondents experience fewer health returns to assets than White respondents.
H5: Black respondents experience more health harm from debt than White respondents.
DATA AND METHODS
Data
Data for this study come from the Panel Study of Income Dynamics (PSID), the longest running nationally representative, longitudinal study of individuals and families in the United States. The PSID began in 1968 and included two independent samples: a nationally-representative sample of families identified by the Survey Research Center at the University of Michigan (“SRC sample”) and an oversample of low income families drawn from the Survey of Economic Opportunity ( “SEO sample”) conducted by the U.S. Census Bureau. Together, these samples constituted a nationally-representative probability sample of U.S. families. Respondents and their family members have been interviewed continuously since 1968, including biennial interviews since 1997. The PSID sample grows as children and grandchildren from PSID families form their own households and join the PSID as respondents. The PSID sample grew from roughly 5,000 families in 1968 and now includes more than 24,000 individuals in over 10,000 families. The PSID is ideal for our purposes because it includes excellent longitudinal, nationally representative data on both health and wealth.
A major challenge to scholarship on the links between wealth and health is endogeneity. As we describe, we include our wealth measures as lagged variables to reduce concerns about reverse causality. Still, in order to improve our ability to make inferences about the relationship between wealth and health, we leverage the 2007–09 Great Recession’s exogenous shock to household wealth. We limit our analyses to four survey waves: the years leading up to (2005), during (2007 and 2009), and after (2011) the Great Recession. Because many households lost wealth during the Great Recession through market mechanisms—rather than as a consequence of changes to individual health—any association between wealth and health during this period is less likely to be subject to concerns about reverse causality and endogeneity. Limiting our analyses to these survey waves improves causal interpretation of our models. Supplementary analyses using data from the 1984–2015 waves of the PSID provided substantively similar results.
Analytic Samples
Our analytic samples include Black and White PSID respondents who were the household head or spouse of the household head aged 25 years or older and were interviewed in at least two waves between 2005–2011. These sample restrictions produced an eligible sample of 40,106 person-years. Given low levels of missing data, further restricting the sample to cases with complete data for the independent variables used in the analyses resulted in final eligible sample of 39,831 person-years and 11,039 unique individuals. In general, compared to the analytic sample, excluded respondents had fewer socioeconomic resources. Our final samples vary by outcome: self-rated health (n=38,450 person-years; 11,036 unique individuals), number of chronic conditions (n=38,364 person-years; 11,031 unique individuals), work limitations (n=38,510 person-years; 11,039 unique individuals), disability (n=38,523 person-years; 11,039 unique individuals), psychological distress (n=37,672 person-years; 10,905 unique individuals), and body mass index (n=37,574 person-years; 10,953 unique individuals).
Outcomes
We use six indicators of health as our outcome variables: self-rated health (where 1=excellent and 5=poor); number of chronic conditions, a count of number of diagnosed conditions (asthma, cancer, diabetes, hypertension, myocardial infarction, and stroke; range = 0–6); work limitations, defined by whether a respondent reported s/he had a physical or nervous condition that limited the amount of work s/he could do (0=not at all, 1=just a little, 2=somewhat, and 3=a lot); disability, defined by whether respondents’ described their employment status as “disabled” (1=disabled); psychological distress, a continuous measurement of non-specific psychological distress measured via the Kessler Psychological Distress Scale (K-6) (range = 0–24) (Kessler et al. 2002); and body mass index (BMI), a continuous measure (kg/m2). We selected this set of health outcomes because, in unique and complementary ways, they reflect ongoing changes in well-being over the life course and include a diverse array of subjective, objective, status, and diagnosis-related markers of physical and mental health. Given that this study is among the first to examine how various wealth components shape trajectories of health, we include a relatively diverse, nonspecific array of outcomes to insights into how the associations might vary across measures of self-rated/diagnosed and physical/mental health, which can serve as a building block for future research on the topic.
Wealth
We use multiple measures of household wealth. Our composite measure of wealth is household net worth (total assets less total debts) in 2015 dollars and inverse hyperbolic sine (IHS) transformed, which both reduces extreme right-skew and allows us to retain negative wealth values. Supplemental analyses including raw wealth values, spline functions, and stratified analyses by negative/positive net worth produced substantively identical results to those reported here. To assess how various wealth components are associated with our outcomes, we include measures of home equity, cash savings, stocks, and debt, which are all included as IHS-transformed continuous measures, which again reduces skew and allows us to retain negative values. Supplemental analyses with alternative operations of these variables—including no transformations, dummy transformations, cubed-root transformations, cubed-root proportion transformations, wealth-wealth component interactions, and wealth components as proportions of total assets—all yielded substantively similar results to those reported in this paper. In addition, we include an indicator for homeownership (1=owns home). All wealth measures are lagged, so that health at time t is a function of wealth at time t-1. To test for differential health returns to total wealth and the wealth components by race, we also include interaction terms for all wealth measures (e.g., Black*wealth, Black*savings, etc.).
Other Measures
To examine racial disparities in wealth and health, we include a dummy measure for race (1=Black). To assess age patterns of health and racial health disparities, we include continuous measures of age and age2, as well as Black*age and Black*age2. To isolate the unique associations between our measures of wealth and our health outcomes, we include a continuous, lagged measure of household income, inflated to 2015 dollars and log-transformed (base 10). We also control education (1=less than high school, 2=high school, 3=some college, 4=bachelors, and 5=advanced degree). To test for differential returns to education and income by race and ensure that our results are not confounded by differential returns to education and income by race, we include Black*education and Black*income interactions. To account for selective attrition, we include a death measures of (1=died during survey period). Finally, all models adjust for gender (1=female) and region of residence (1=South).
Analytic Methods
First, we use descriptive statistics to examine racial differences in the variables included in the analysis, paying particular attention to racial disparities in wealth and health. Next, we use mixed effects growth curve models to estimate the longitudinal associations between our wealth measures and the outcomes and assess the extent to which racial disparities in wealth components contribute to the age patterning of racial health inequality. In these models, observations at level 1 are nested within individuals at level 2. Our models include random intercepts at both the individual and household levels. The link function of these mixed effects models differs across dependent variables. For self-rated health and work limitations (ordinal outcomes), we use cumulative link mixed models, which are functionally equivalent to ordinal logistic regression but that allow for random effects. We use mixed effects Poisson models for the number of conditions and psychological distress outcomes. We model our binary outcome of disability with mixed effects logit models. Finally, we use a linear mixed effects model for the continuous BMI outcome.
For all outcomes, Model 1 is a base model of Black-White health disparities that includes demographic controls but does not adjust for SES. Models 2a and 2b build on Model 1 by adjusting for income and education (Model 2a) and Black*income and Black*education (Model 2b). The inclusion of total wealth and Black*wealth in Models 3a and 3b, respectively, allow us to assess how wealth relates to the outcomes net of the other indicators of SES, whether the wealth contributes to the racial health gaps, and whether Blacks and Whites receive similar health returns to wealth. Finally, Model 4a builds on Model 3b by including the wealth components, and Model 4b is the fully adjusted model that also includes the Black*wealth component interactions. Model 4a allows us to examine how the wealth components relate to the outcomes and contribute to Black-White health gaps. Model 4b also assesses whether Blacks and Whites receive similar health returns to the wealth component measures.
To assess mean-level racial health gaps and examine the age patterning of Black-White health disparities, we consider the magnitudes, directions, and statistical significance of the parameter estimates for race, Black*age, and Black*age2 across the models and outcomes. We assess the extent to which inclusion of the various wealth measures into the models reduces the magnitude, direction, and/or significance of Black-White disparities in the intercepts or growth rate of health with age. We hypothesize that racial differences in net worth and wealth composition mediate black-white health disparities, but there are currently no available methods for estimating multiple mediators in a multilevel framework with non-linear outcomes that fully accounts for the covariance structure of mixed effects models. As such, we estimate how inclusion of wealth components improves model fit via Akaike information criterion (AIC), which measures the maximum likelihood of each model while penalizing for each additional estimated parameter, such that models which are overfit will have worse AIC than models with fewer parameters. The Black*wealth and Black*wealth component interaction terms indicate whether Blacks and Whites receive differential health returns to the various wealth measures. Given space constraints, we present the model results for self-rated health in Table 2 and summarize the results for all outcomes in Figures 2 and 3. Full models for chronic conditions, work limitations, disability, psychological distress, and BMI are in the Appendix.
Table 2.
Mixed Effects Models for Self-Rated Health
| Model 1 | Model 2a | Model 2b | Model 3a | Model 3b | Model 4a | Model 4b | |
|---|---|---|---|---|---|---|---|
| Black | 0.148 | −0.143 | −2.853*** | −2.607*** | −2.447*** | −2.076*** | −1.950*** |
| Age | 0.012*** | 0.023*** | 0.029*** | 0.037*** | 0.038*** | 0.041*** | 0.040*** |
| Age2 | 0.000*** | 0.000 | −0.000 | −0.000 | −0.000 | −0.000 | −0.000 |
| Gender (1=female) | 0.237*** | 0.227*** | 0.230*** | 0.222*** | 0.224*** | 0.216*** | 0.218*** |
| Black * Age | 0.037*** | 0.035*** | 0.026*** | 0.027*** | 0.024*** | 0.022*** | 0.023*** |
| Black * Age2 | −0.001*** | −0.001*** | −0.000** | −0.000** | −0.000* | −0.000* | −0.000** |
| Region (1=South) | 0.155*** | 0.131** | 0.121** | 0.141** | 0.138** | 0.133** | 0.132** |
| Year | 0.008* | 0.012** | 0.012** | 0.003 | 0.003 | −0.002 | −0.001 |
| Died | 1.463*** | 1.318*** | 1.313*** | 1.292*** | 1.294*** | 1.260*** | 1.254*** |
| Income | −0.220*** | −0.347*** | −0.285*** | −0.277*** | −0.214*** | −0.204*** | |
| Black * Income | 0.225*** | 0.197*** | 0.181*** | 0.145*** | 0.126*** | ||
| Education | |||||||
| High school | −0.608*** | −0.689*** | −0.673*** | −0.670*** | −0.604*** | −0.588*** | |
| Some college | −0.806*** | −0.908*** | −0.891*** | −0.889*** | −0.800*** | −0.780*** | |
| Bachelors | −1.176*** | −1.266*** | −1.243*** | −1.240*** | −1.090*** | −1.068*** | |
| Advanced | −1.427*** | −1.511*** | −1.507*** | −1.507*** | −1.335*** | −1.311*** | |
| Black * Education | |||||||
| Black * High school | 0.116 | 0.149 | 0.135 | 0.122 | 0.086 | ||
| Black * Some college | 0.176 | 0.217 | 0.203 | 0.208 | 0.150 | ||
| Black * Bachelors | 0.320* | 0.320* | 0.311* | 0.320* | 0.252 | ||
| Black * Advanced | 0.349* | 0.343* | 0.341* | 0.349* | 0.278 | ||
| Wealth (total net worth) | −0.029*** | −0.033*** | −0.018*** | −0.017*** | |||
| Black * Wealth | 0.010** | 0.008* | 0.006 | ||||
| Wealth Components | |||||||
| Own home (1=yes) | −0.070 | −0.059 | |||||
| Home equity | −0.006 | −0.005 | |||||
| Savings | −0.040*** | −0.052*** | |||||
| Stocks | −0.024*** | −0.022*** | |||||
| Debt | 0.017*** | 0.016*** | |||||
| Black * Wealth Components | |||||||
| Black * Own home | −0.023 | ||||||
| Black * Home equity | −0.001 | ||||||
| Black * Savings | 0.027*** | ||||||
| Black * Stocks | −0.011 | ||||||
| Black * Debt | −0.001 | ||||||
| Intercepts | |||||||
| Threshold=1 | −0.786*** | −4.257*** | −5.816*** | −5.248*** | −5.167*** | −4.544*** | −4.490*** |
| Threshold=2 | 0.972*** | −2.422*** | −3.971*** | −3.388*** | −3.307*** | −2.671*** | −2.616*** |
| Threshold=3 | 2.593*** | −0.714*** | −2.259*** | −1.663*** | −1.582*** | −0.932*** | −0.877*** |
| Threshold=4 | 4.066*** | 0.816*** | −0.730*** | −0.125 | −0.045 | 0.612** | 0.668** |
| AIC | 97,736 | 96,128 | 96,043 | 95,779 | 95,769 | 95,488 | 95,486 |
Note: Results of cumulative link mixed models. Includes random intercepts for individuals and households. Years of analysis = 2005–2011. n=38,450 person-years; 11,036 unique individuals. Race reference category = White. Degree reference category = Less than high school. All wealth variables transformed via an inverse hyperbolic sine (IHS) and inflated to 2015 U.S. dollars via the Consumer Price Index.
Figure 2. Parameter Estimates of Associations between Wealth Components and Health Outcomes.
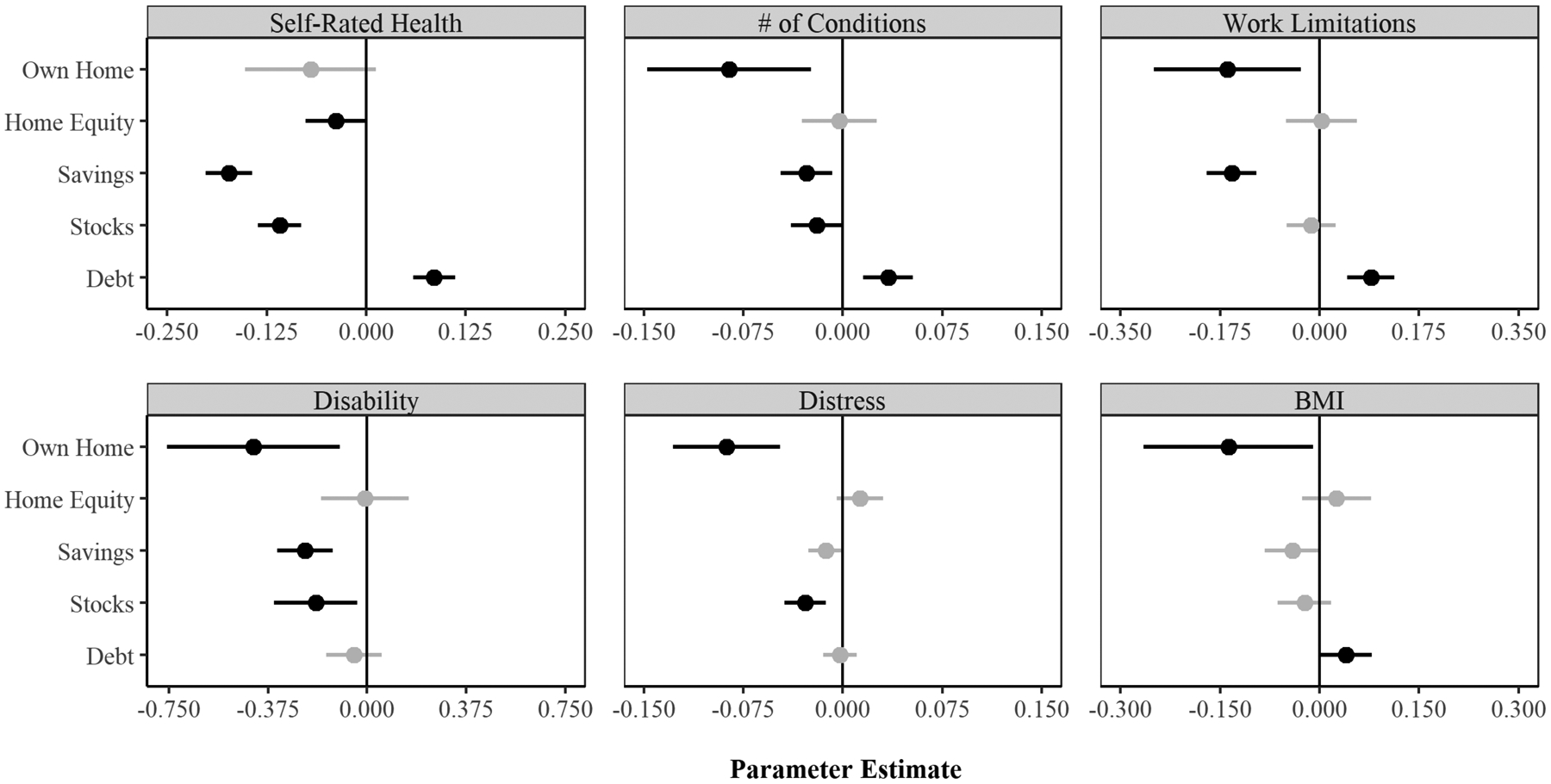
Note: Parameter estimates based on Model 4a (in Table 2 and Appendix A), shaded based on statistical significance (Black = p<.05) and standardized to reflect the association between a one standard deviation change in each independent variable with a one unit change in each dependent variable.
Figure 3. Racial Disparity in Self-Rated Health.
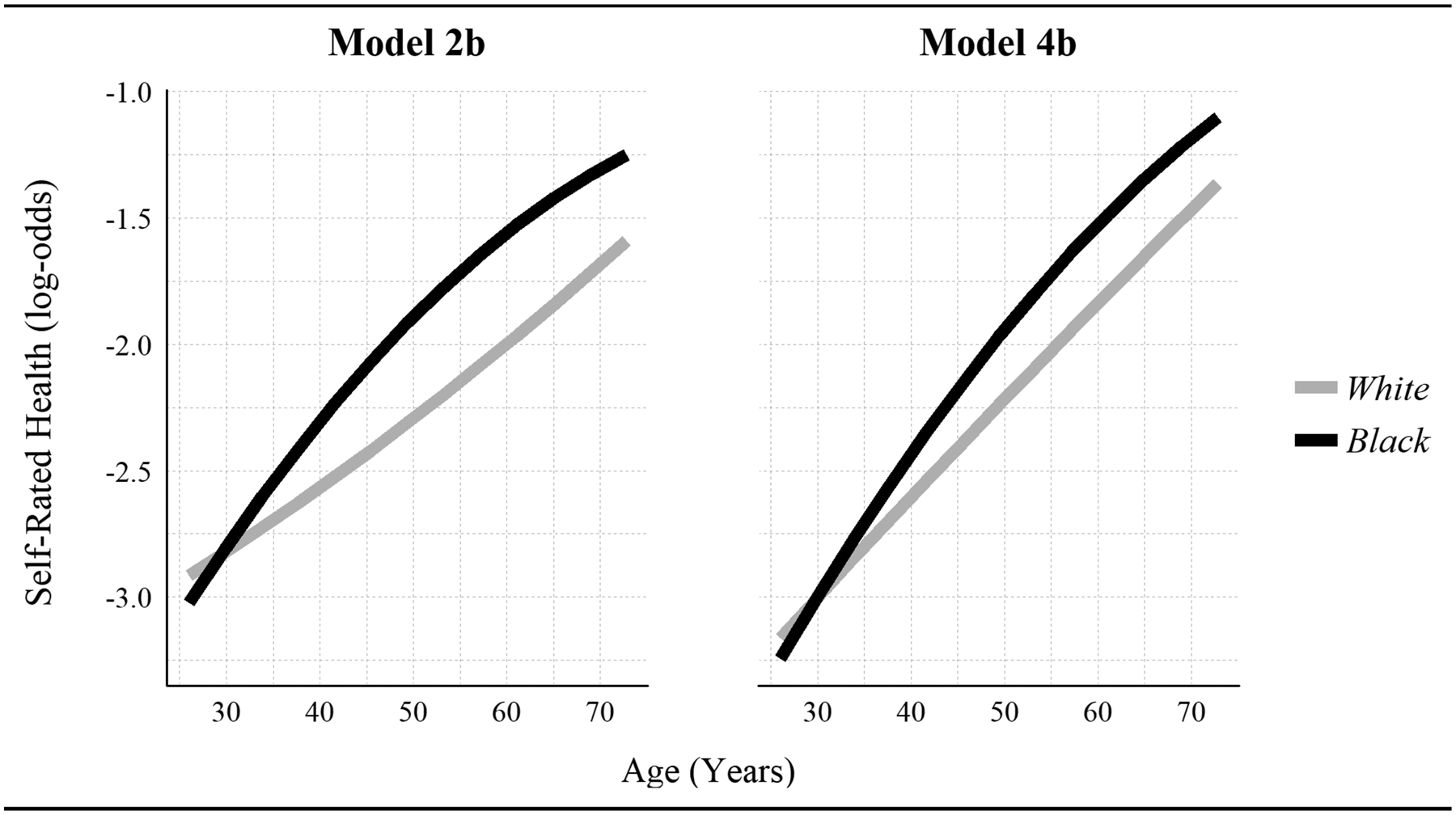
Note: Predicted Black-White disparity in self-rated health with no adjustment for wealth (based on Model 2a of Table 2) and with adjustment for total net worth and the wealth components (Model 4a of Table 2).
RESULTS
Descriptive Statistics
Table 1 displays descriptive statistics for the sample by race and reveals striking Black-White disparities in the measures of health and SES. With the exception of work limitations, Blacks have worse health than Whites across the measures of health (p<0.001). Whites in the sample have net worth that is nearly 7 times that of Blacks (p<0.001). Compared to Blacks, Whites have more home equity, savings, and stocks, carry more debt, and are nearly twice as likely to own a home (p<0.001). Figure 1 visually illustrates the Black-White wealth gap and shows a striking overdispersion of Blacks with near-zero net worth compared to Whites, who show greater representation in right tail of the wealth distribution.
Table 1.
Descriptive Statistics by Race
| Whites | Blacks | p-value | |
|---|---|---|---|
| Mean/Prop | Mean/Prop | ||
| Health | |||
| Self-Rated Health (1=excellent; 5=poor) | 2.54 | 2.84 | <0.001 |
| Number of Conditions (range=0–6) | 0.75 | 0.92 | <0.001 |
| Work Limitations (range=0–3) | 0.40 | 0.40 | 0.889 |
| Disability (1=yes) | 0.04 | 0.09 | <0.001 |
| 30-Day Distress (K6) (range=0–24) | 1.88 | 2.76 | <0.001 |
| Body mass index (kg/m2) | 27.47 | 30.19 | <0.001 |
| Wealth Components (thousands) | |||
| Net Worth | 442.42 | 64.49 | <0.001 |
| Home Equity | 113.47 | 30.17 | <0.001 |
| Savings | 35.82 | 6.60 | <0.001 |
| Stocks | 61.26 | 3.20 | <0.001 |
| Debt | 13.27 | 11.09 | <0.001 |
| Own Home (1=yes) | 0.77 | 0.48 | <0.001 |
| Income (thousands) | 95.89 | 53.52 | <0.001 |
| Demographics | |||
| Age | 50.46 | 47.33 | <0.001 |
| Female (1=yes) | 0.51 | 0.60 | <0.001 |
| Southern Residence (1=yes) | 0.32 | 0.69 | <0.001 |
| Degree | |||
| Less than High School | 0.07 | 0.16 | <0.001 |
| High School | 0.49 | 0.61 | <0.001 |
| Some College | 0.09 | 0.08 | 0.150 |
| Bachelors | 0.22 | 0.09 | <0.001 |
| Advanced | 0.13 | 0.05 | <0.001 |
| Died | 0.07 | 0.07 | 0.334 |
Note: Finances in U.S. dollars, inflated to Consumer Price Index 2015. Statistics based on last observation of each individual. n=11,039 individuals, 7,490 Whites, 3,549 Blacks. p-values of difference in means/proportions between Whites and Blacks.
Figure 1. Racial Disparities in Net Worth.
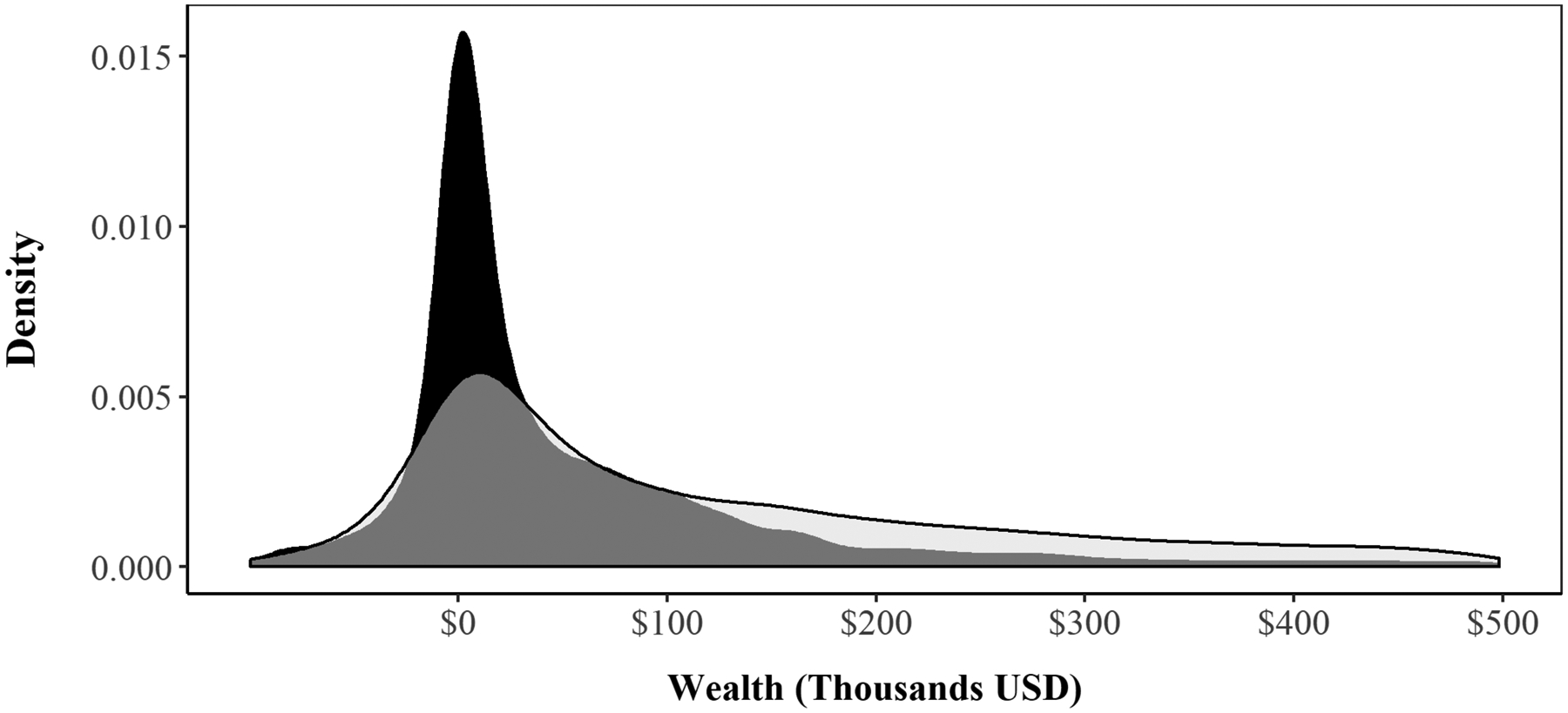
Notes: Estimates based on last observation of each individual in PSID subsample (Years=2005–2011; n=11,039 individuals) and inflated to Consumer Price Index 2015.
Growth Curve Models
Net Worth, Wealth Components, and Health
Results from the multilevel growth curve models for self-rated health are in Table 2. We include full model results for the other outcomes in Appendix A. Table 2, Model 1 includes sociodemographic variables, and Model 2a adjusts for income and education, both of which are protective against poor health. Model 3a includes net worth, and results show that net worth is protective against poor health (β=–.029, p<0.001), net of income and education. Model 4a includes each of the wealth components simultaneously and reveals that home equity, savings, and stocks are all protective against poor health, net of one another and net of income, education, and total net worth. Debt is associated with worse self-rated health (β=.017, p<0.001). There is no association between homeownership and self-rated health.
Detailed model results for other outcomes are included in Appendix A. Although the various wealth components relate to health in different ways, there is some consistency across outcomes. Results from Model 4a indicate that homeownership is associated with better health for all outcomes in Appendix A. Across most outcomes, we find that homeownership, savings, and stocks are associated with better health. We also find evidence that debt is associated with worse health, including more chronic conditions, more work limitations, and higher BMI. Results provide little evidence of an association between home equity and health. Figure 2 summarizes our findings regarding the associations between the wealth components and health by displaying standardized parameter estimates of the associations between the wealth components and each of the outcomes based on Model 4a for each outcome. Importantly, across the majority of outcomes, the inclusion of wealth components in Model 4a significantly and substantially improves model fit over Models 3a and 3b.
Net Worth, Wealth Components, and Racial Health Disparities
Comparing the coefficient estimate for the dummy indicator for race—which signifies the Black-White disparity in the outcomes—across analytic models reveals how the socioeconomic measures contribute to Black-White health inequality. In the models for self-rated health presented in Table 2, results from Model 1 show that Blacks and Whites have similar levels of health at younger ages, but the race gap in self-rated health diverges with age (Black*age: β=.037, p<0.001). In Models 2a, 3a, and 4a—which adjust for income and education, net worth, the wealth components in a stepwise fashion—a race gap in the intercept emerges to show in Models 3a and 4a that younger Blacks have better self-rated health than Whites. Still, a race gap in the growth rate persists, whereby Blacks experience faster age-related health decline than Whites. The race gap in the growth rate of the disparity is smallest in Models 4a and 4b, which adjust for net worth, the wealth components, and the other socioeconomic factors. Figure 3 plots the age patterning of the racial wealth gap in self-rated health based on Models 2a (which adjusts for income and education but not net worth or the wealth components) and Model 4a (which adjusts for income, education, net worth, and the wealth components). This Figure highlights a narrowing of the racial gap with age.
Results for the other outcomes presented in Appendix A reveal a similar pattern regarding the contribution of the socioeconomic factors to Black-White health disparities. In general, after adjusting for income and education in Model 2a, adjusting for wealth and the wealth components in subsequent models slightly reduces the race gap in the intercept and generally results in an attenuation of the race gap in the growth rate. These findings suggest that the racial patterning of net worth and the wealth components contribute to the age patterning of the Black-White gap in health, net of racial disparities in income and education.
Differential Returns to SES by Race
Models with the subscript “b” include interaction terms that indicate the extent to which Blacks and Whites receive differential health returns to the various socioeconomic factors. In Model 2b of Table 2, results from the self-rated health outcome show that, while education and income are protective against poor health, Blacks receive fewer health protections from increases in income (Black*income: β=.225, p<0.001) than Whites. At higher levels of education, Blacks also experience worse self-rated health than Whites. Results from the other outcomes, presented in the Appendix, reveal similar results with regard to race differences in returns to income, with Blacks generally receiving fewer health protections than Whites. Results in the Appendix show mixed evidence of race differences in returns to education. Compared to Whites with similar levels of education, Blacks have higher BMIs but similar levels of chronic conditions, work limitations, disability, and psychological distress outcomes. By contrast, Black Americans have lower levels of psychological distress compared to Whites with similar levels of education.
Results from Model 3b in Table 2 indicate that, in terms of self-rated health, Blacks receive fewer health protections from increases in net worth than Whites. By contrast, results from the other outcomes provide little convincing evidence of differential returns to net worth by race. Results from Model 4b include the race*wealth component interaction terms and show that, compared to Whites, Blacks receive fewer health protections from savings than Whites. Across the other outcomes, our findings indicate little evidence for differential returns to the wealth components. Estimates for psychological distress are the only other outlier, with additional savings appearing to yield distinct advantages for Blacks compared to Whites (Black*savings: β=–.012, p<0.001). We graphically illustrate this finding regarding the differential returns to savings by race for the self-rated health and psychological distress outcomes in Figure 4, which follows the approach suggested by Long and Mustillo (2018) to plot the racial disparity in predicted probabilities of self-rated health and predicted level of psychological distress by level of savings using marginal effects. As seen in Figure 4, Blacks are more likely to report poor health and less likely to report excellent health than Whites with similar levels of savings. By contrast, the racial disparity in psychological distress narrows as savings increase.
Figure 4. Racial disparities in health by savings.
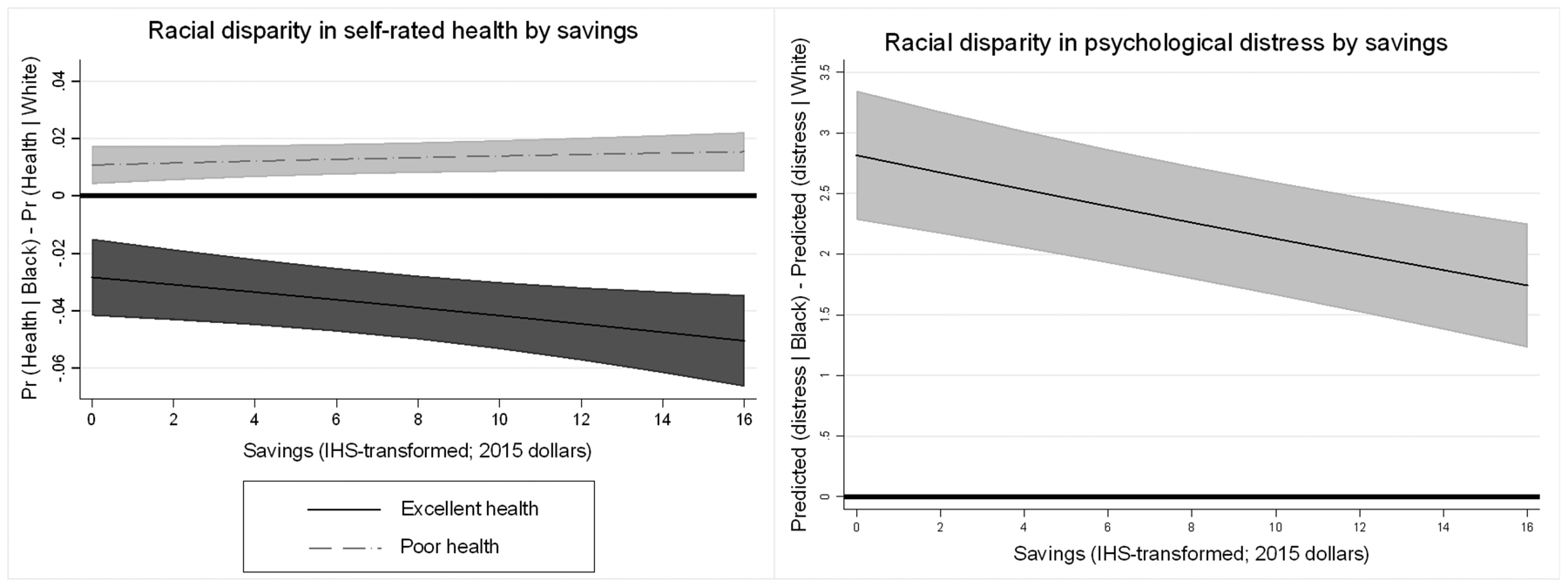
Note: Racial disparities in predicted health by level of savings. Zero (indicating no racial difference) is reference line. In creating plots, we use parameter estimates from Model 4b and follow the approach proposed by Long and Mustillo (2018) for calculating differences in predicted probabilities (self-rated health)/predicted outcomes (psychological distress) and marginal effects.
DISCUSSION
A body of research links wealth to both individual health (Boen and Yang 2016; Hajat et al. 2010; Sweet et al. 2013) and racial disparities in health (Boen 2016; Bond Huie et al. 2003; Kim and Miech 2009). Still, because previous research typically operationalizes wealth as total net worth, it is unclear how different wealth components—including various types of assets and debt—uniquely relate to health. Similarly, despite evidence of racial differences in wealth portfolios (Gittleman and Wolff 2004; Keister 2000, 2004, 2014; Killewald and Bryan 2018), few studies assess how racial variation in wealth composition patterns racial health inequality or test whether there are race variations in the health returns to different types of assets and debt. Using rich, longitudinal data from the PSID, this study is among the first to comprehensively assess how various wealth components differentially shape individual health and provides new insights into how Black-White differences in wealth portfolios contribute to Black-White disparities in health. By leveraging the exogenous shock to household wealth that occurred immediately preceding and during the Great Recession, our study provides evidence of the links among net worth, wealth composition, and individual and population health.
Our study makes three key contributions. First, we find that the components of total wealth are associated with health in different ways. Notably, we find that savings, stocks, homeownership, debts, and health are associated even when adjusting for total wealth and when including all of the wealth components simultaneously in analytic models. While we also find that net worth is associated with the outcomes, our findings indicate that the association between wealth and health is more nuanced than previously documented. Across the outcomes, we find a relatively high degree of consistency in the associations between the wealth components and health, which underscores the robustness of our results and the wealth-health relationship. Across most outcomes, we find that savings and stocks are associated with better health, with those owning more in savings and stocks having better self-rated health, fewer health conditions, less risk of work limitations, less disability, and lower levels of distress. Although we hypothesized that households with riskier portfolios—as indicated by owning substantial stocks and investments—might experience increased health risk, our findings did not support this expectation. Having a higher-risk wealth portfolio may be stressful, but this type of stress would likely be categorized as what McEwen (2017) deems a “good” or “tolerable” stressor. That is, the decision to place significant assets in equities may be stressful, but potential future gains may counteract this stress. Unlike toxic stressors—over which the individual has little control and few resources to cope—more tolerable stressors have fewer adverse effects on physical or mental health. Consistent with previous research (Finnegan 2014; Yilmazer, Babiarz, and Liu 2015), we also found evidence that homeownership is associated with health across several outcomes, including chronic conditions, work limitations, disability, psychological distress, and BMI. Previous research suggests that owning a home confers psychosocial benefits to homeowners despite being illiquid. Homeowners may also experience better housing quality on average as well as greater levels of financial stability (Rossi and Weber 1996). Still, we found that after adjusting for total wealth and the other wealth components, there is no link between home equity and health. Including the wealth component measures in Model 4a generally improves fit over Models 3a and 3b, which adjust for education, income, and total net worth, indicating that the wealth components are important dimensions of well-being, net of other indicators of SES.
The absence of a relationship between home equity and health suggests that liquid and illiquid assets may be associated differently with health in meaningful ways that warrant future attention from health scholars. We consistently find that liquid assets—such as savings and investments—are strongly associated with health. Our evidence of the links between illiquid assets—such as homes and home equity—is a bit more mixed. It is therefore possible that these dimensions of health shape health through varying mechanisms. Assets with more immediate cash values such as savings and stocks facilitate paying for basic needs such as food, housing, and transportation, which each have health benefits. Being able to access the cash value of an asset also makes it possible to spend that asset on preventative and routine medical care and to pay for medical emergencies. Households with limited liquid assets may be less able to pay for health-supporting resources and may be more likely to forego both preventative and emergency medical treatments. For these reasons, liquid assets may support health by serving as sources of financial insurance and safety nets. By contrast, home ownership may confer high levels of control, stability, and neighborhood integration to residents (Rossi and Weber 1996). Though we hypothesized that liquid assets would be more strongly associated with the outcomes than illiquid assets (Hypothesis 1), our results provide mixed support by showing consistent associations between liquid assets and health but also strong associations between home ownership and health. We are unable to test the mechanisms linking savings, investments, and home ownership to health, but our findings are robust, suggesting that future work in this area should continue to assess the links between these assets and health.
Consistent with previous research (Drentea and Reynolds 2014; Hodson, Dwyer, and Neilson 2014), we find that debt is associated with worse health, net of assets, providing support for Hypothesis 2. In particular, we found that individuals carrying more debt had worse self-rated health, more chronic conditions, more work limitations, more disability, and higher BMIs. Previous research indicates that debt can increase feelings of hopelessness and frustration (Drentea and Reynolds 2014) in ways that shape both physical and mental health risk. The uncertainty and worry associated with debt may serve as salient stressors in the lives of individuals in ways that promote high levels of risk across physiological systems. Studies find that the health risk is particularly grave for unsecured debts, which are notoriously difficult to pay down (Berger and Houle 2019).
Second, our findings indicate that the racial differences in wealth portfolios play a critical role in patterning Black-White health inequality, providing evidence in support of Hypothesis 3. Descriptive statistics shown both in Table 1 and Figure 1 document striking levels of Black-White wealth inequality. Consistent with previous research (Boen 2016; Bond Huie et al. 2003; Kim and Miech 2009), we find Black-White gaps in total wealth play an essential role in shaping racial disparities in age patterns of health and disease risk. As shown in Table 1, findings also provide evidence of racial differences in wealth portfolios, including Black-White differences in home ownership and equity, savings, stocks, and debt. Results from the growth curve models provided some evidence that race differences in wealth portfolios contributed to the age patterning of Black-White health gaps, particularly in the self-rated health, chronic conditions, and disability models. In these models, adjusting for net worth and the wealth components often attenuated the race gap in the growth rates of the disparities with age, in particular. As mediation techniques for multilevel models advance, future research should continue to assess whether and how race differences in wealth composition mediate racial health gaps. A large body of research documents the persistence and growth of the racial wealth gap across both historical time (Pfeffer, Danziger, and Schoeni 2013) and the life course (Brown 2016). Our findings are consistent with the notion that the unequal patterning of socioeconomic resources, including wealth, is a primary pathway through which racism harms health (Phelan and Link 2015).
Third, whereas few studies account for the racialized nature of the socioeconomic gradient in health, we examine whether Blacks and Whites experience similar health returns to increases in SES. We find mixed evidence regarding the association between the various assets and health and respondent race (Hypothesis 4). For example, we find that Black respondents received fewer returns to self-rated health but greater psychological protections with increases in savings, as illustrated in Figure 4. We do not find evidence of differential vulnerability to debt by race (Hypothesis 5). In these ways, results from the self-rated health models provide evidence of the diminishing returns hypothesis (Boen 2016; Shuey and Willson 2008). Stress resulting from discrimination, differential experiences in the labor market, and exposure to early-life, household, and neighborhood poverty may prevent Blacks Americans from converting socioeconomic gains into health improvements in the same ways as Whites. By contrast, our results from the psychological distress models showed higher levels of returns to savings for Black Americans compared to Whites. Recent research suggests that Black Americans may be simultaneously “psychologically resilient” and “physically vulnerable” (Erving, Satcher, and Chen 2020). One the one hand, Black Americans may derive more psychological benefits from increases in resources like savings while at the same time not receiving the same returns as Whites when it comes to other domains of well-being. We were unable to test these mechanisms, but future research should continue to explore racial differences in returns to SES. Across outcomes, education, income, and wealth are generally protective against poor health. Still, across most outcomes, Black Americans receive fewer health protections from increases in income than Whites. Blacks also experience worse self-rated health than Whites with similar levels of education and wealth, though results show little evidence of race differences in returns to education or total net worth for the other outcomes. Understanding the mechanisms producing differential returns to socioeconomic resources by race is particularly important because failing to do so may result in misestimating both the effects of SES on health and the potential health risks of income allocation for Black Americans, in particular (Boen 2016; Pearson 2008).
Our study is not without limitations that should be considered in future research. First, although we examine the associations between the wealth components and health outcomes, we were unable to study many factors—such as neighborhood characteristics and intergenerational transfers—that shape wealth accumulation and health. Future studies should integrate these measures to add further nuance to understanding of the wealth-health connection. Second, our study uses a summary measure indicating total debt, but research should consider how different types of debt (e.g., student loan debt, credit card debt, etc.) may relate to health differently. Third, our study provides evidence of links between wealth components and a variety of outcomes. Future research can build on the findings presented here to interrogate the social, biological, and psychological mechanisms undergirding these links.
A final limitation of this work relates to our treatment of financial assets. In particular, we are unable to disaggregate the types of financial assets in which households hold their assets. The difference between liquid and illiquid assets is central to our arguments, but there are potential costs associated with using some financial assets. Most important, fees make some assets more accessible and useful than other assets for in terms of paying for health related expenses. In particular, there can be fees associated with accessing funds that are in Individual Retirement Accounts (IRAs), employer-sponsored defined contribution plans (e.g., 401k, 403b accounts), deferred compensation accounts (i.e., 457 plans), and similar accounts. The most common fees are those paid for using the funds before a specified age. The age restriction and fees vary by the type of account, but the fees can be substantial. Ideally, we would have data on the type of accounts in which respondents have their financial assets, but the PSID does not include this level of detail. Even other data sets that include detailed information about financial asset accounts (e.g., the Survey of Consumer Finances) do not include information about the specific restrictions on the respondents’ particular account. Importantly, however, even if we had this detailed information about respondent financial assets, our results would probably not change substantively. Although the proportion of financial assets held in retirement and other accounts with fees associated with early use has grown over time, most households (the bottom 90%, or those below the top 10% of the wealth distribution) hold relatively few of their financial assets in pooled investment accounts of any sort, including retirement accounts (Keister 2014). In fact, households in the bottom 90% of the wealth distribution held only 1.5% of their assets in pooled investment accounts; the bulk of the financial assets held by the majority of households is in transaction accounts—such as savings and checking accounts—that have no fees associated with use of the funds held in them (Keister 2014). Future research could usefully explore the role that fees associated with liquid assets have on 1) if people access those assets for healthcare and other health-related expenses, and 2) whether the types of financial assets that households own are differentially associated with health outcomes.
Together, these findings provide a more nuanced understanding of the socioeconomic determinants of individual health and Black-White health gaps and offer new insights into how wealth-generating interventions can also most effectively reduce population health inequality. Our findings add to the large and growing body of research showing strong, prospective associations between wealth and health, which together suggest that wealth policy in the US is, inherently, health policy. Still, results from this study also indicate that, when it comes to health, not all assets are created equal; in particular, our findings suggest that efforts to build the liquid assets of American households—including savings and investments—and promote homeownership may yield the greatest population health returns. Because the fundamental drivers of wealth inequality are structural—located in historical and contemporary policies and institutional practices—reducing levels of wealth inequality, including particularly stark and persistent Black-White wealth gaps, requires widespread systemic change aimed at building and/or redistributing wealth (Darity et al. 2018). Intervening to close the racial wealth gap will not only promote economic equity, but it is critical for racial health equity.
Supplementary Material
AUTHOR BIOGRAPHIES
Courtney E. Boen is an assistant professor in the Department of Sociology and research associate in the Population Studies Center and Population Aging Research Center at the University of Pennsylvania. Dr. Boen’s research focuses on the social determinants of population health inequality, with a particular focus on the role of racism in shaping health disparities across the life course.
Lisa A. Keister is professor in the Department of Sociology and the Sanford School of Public Policy; she is also a research associate in the Duke Network Analysis Center and Duke University Population Research Institute. Her research explores wealth ownership and inequality including identifying the factors that affect household decisions about saving.
Brian Aronson is a postdoctoral fellow in the Department of Sociology at Indiana University, Bloomington of Pennsylvania. Dr. Aronson’s research focuses on social network analysis, institutions, public health, and inequality.
Footnotes
SUPPLEMENTAL MATERIAL
Additional supporting information may be found in the online version of this article.
References
- Assari Shervin. 2018. “Health disparities due to diminished return among black Americans: Public policy solutions.” Social Issues and Policy Review 12(1): 112–145. [Google Scholar]
- Berger Lawrence M., and Houle Jason N.. 2019. “Rising Household Debt and Children’s Socioemotional Well-being Trajectories.” Demography 56(4): 1273–1301. [DOI] [PubMed] [Google Scholar]
- Boen Courtney. 2016. “The Role of Socioeconomic Factors in Black-White Health Inequities Across the Life Course: Point-in-Time Measures, Long-Term Exposures, and Differential Health Returns.” Social Science & Medicine 170:63–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen Courtney and Yang YC. 2016. “The Physiological Impacts of Wealth Shocks in Late Life: Evidence from the Great Recession.” Social Science & Medicine 150:221–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond Huie, Stephanie A, Krueger Patrick M., Rogers Richard G. and Hummer Robert A.. 2003. “Wealth, Race, and Mortality.” Social Science Quarterly 84(3):667–684. [Google Scholar]
- Brown Tyson H. 2016. “Diverging Fortunes: Racial/Ethnic Inequality in Wealth Trajectories in Middle and Late Life.” Race and Social Problems 8(1):29–41. [Google Scholar]
- Brown Tyson H. 2018. “Racial stratification, immigration, and health inequality: A life course-intersectional approach.” Social Forces 96(4): 1507–1540. [Google Scholar]
- Burgard Sarah A., Ailshire Jennifer A. and Kalousova Lucie. 2013. “The Great Recession and Health People, Populations, and Disparities.” The Annals of the American Academy of Political and Social Science 650(1):194–213. [Google Scholar]
- Catalano R, Goldman-Mellor S, Saxton K, Margerison-Zilko C, Subbaraman M, LeWinn K and Anderson E. 2011. “The Health Effects of Economic Decline.” Annual Review of Public Health 32:431–450. doi: 10.1146/annurev-publhealth-031210-101146 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesarini David, Lindqvist Erik, Östling Robert, and Wallace Björn. 2016. “Wealth, health, and child development: Evidence from administrative data on Swedish lottery players.” The Quarterly Journal of Economics 131(2): 687–738. [Google Scholar]
- Charron-Chénier Raphaël, Fink Joshua J., and Keister Lisa A.. 2017. “Race and consumption: Black and White disparities in household spending.” Sociology of Race and Ethnicity 3(1): 50–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler David M., Adriana Lleras-Muney, and Tom Vogl. 2008. Socioeconomic status and health: dimensions and mechanisms (No. w14333). National Bureau of Economic Research. [Google Scholar]
- Darity W Jr, Hamilton D, Paul M, Aja A, Price A, Moore A, & Chiopris C 2018. “What we get wrong about closing the racial wealth gap.” Samuel DuBois Cook Center on Social Equity and Insight Center for Community Economic Development. [Google Scholar]
- Drentea Patricia and Reynolds John R.. 2014. “Where does Debt Fit in the Stress Process Model?” Society and Mental Health 5(1):16–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faber Jacob. W. 2013. “Racial dynamics of subprime mortgage lending at the peak.” Housing Policy Debate 23(2): 328–349. [Google Scholar]
- Finnigan R 2014. “Racial and ethnic stratification in the relationship between homeownership and self-rated health.” Social Science & Medicine 115: 72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flippen Chenoa. 2004. “Unequal returns to housing investments? A study of real housing appreciation among black, white, and Hispanic households.” Social Forces 82(4): 1523–1551. [Google Scholar]
- Gaddis SM 2014. “Discrimination in the Credential Society: An Audit Study of Race and College Selectivity in the Labor Market.” Social Forces 93(4):1451–1479. [Google Scholar]
- Gaydosh L, Schorpp KM, Chen E, Miller GE, & Harris KM (2018). College completion predicts lower depression but higher metabolic syndrome among disadvantaged minorities in young adulthood. Proceedings of the National Academy of Sciences 115(1): 109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittleman Maury and Wolff Edward N.. 2004. “Racial Differences in Patterns of Wealth Accumulation.” Journal of Human Resources 39(1):193–227. [Google Scholar]
- Grodsky Eric and Pager Devah. 2001. “The Structure of Disadvantage: Individual and Occupational Determinants of the Black-White Wage Gap.” American Sociological Review:542–567. [Google Scholar]
- Hajat A, JS Kaufman KM Siddiqi Rose, A. and Thomas JC. 2010. “Do the Wealthy have a Health Advantage? Cardiovascular Disease Risk Factors and Wealth.” Social Science & Medicine 71(11):1935–1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward Mark D., Miles Toni P., Crimmins Eileen M. and Yang Yu. 2000. “The Significance of Socioeconomic Status in Explaining the Racial Gap in Chronic Health Conditions.” American Sociological Review:910–930. [Google Scholar]
- Hodson Randy, Dwyer Rachel E., and Neilson Lisa A.. 2014. “Credit card blues: the middle class and the hidden costs of easy credit.” The Sociological Quarterly 55(2): 315–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houle JN 2014. “Disparities in debt: Parents’ socioeconomic resources and young adult student loan debt.” Sociology of Education, 87(1), 53–69. [Google Scholar]
- Keister Lisa A. 2014. “The one percent.” Annual Review of Sociology 40: 347–367. [Google Scholar]
- Keister Lisa A. 2000a. “Race and Wealth Inequality: The Impact of Racial Differences in Asset Ownership on the Distribution of Household Wealth.” Social Science Research 29(4):477–502. [Google Scholar]
- Keister Lisa A. 2000b. Wealth in America: Trends in Wealth Inequality. Cambridge University Press. [Google Scholar]
- Keister Lisa A. and Moller Stephanie. 2000. “Wealth Inequality in the United States.” Annual Review of Sociology 26:63–81 (http://www.jstor.org/stable/223437). [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Walters EE & Zaslavsky AM 2002. “Short screening scales to monitor population prevalences and trends in nonspecific psychological distress.” Psychological Medicine 32: 959–976. [DOI] [PubMed] [Google Scholar]
- Killewald A, & Bryan B 2018. “Falling Behind: The Role of Inter-and Intragenerational Processes in Widening Racial and Ethnic Wealth Gaps through Early and Middle Adulthood.” Social Forces: 97(2): 705–740. [Google Scholar]
- Killewald Alexandra, Pfeffer Fabian T. and Schachner Jared N.. 2017. “Wealth Inequality and Accumulation.” Annual Review of Sociology 43: 379–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Jinyoung and Miech Richard. 2009. “The Black–White Difference in Age Trajectories of Functional Health Over the Life Course.” Social Science & Medicine 68(4):717–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochhar R, Taylor P, & Fry R 2011. Wealth gaps rise to record highs between Whites, Blacks and Hispanics (Vol. 26). Washington, DC: Pew Research Center. [Google Scholar]
- Krivo Lauren J. and Kaufman Robert L.. 2004. “Housing and Wealth Inequality: Racial-Ethnic Differences in Home Equity in the United States.” Demography 41(3):585–605. [DOI] [PubMed] [Google Scholar]
- Link Bruce G. and Phelan Jo. 1995. “Social Conditions as Fundamental Causes of Disease.” Journal of Health and Social Behavior: 80–94. [PubMed] [Google Scholar]
- Long J.Scott, and Mustillo Sarah A.. 2018. “Using predictions and marginal effects to compare groups in regression models for binary outcomes.” Sociological Methods & Research 1–37. [Google Scholar]
- Lusardi Annamaria, Schneider Daniel J. and Tufano Peter. 2010. The Economic Crisis and Medical Care Usage NBER Working Paper No. 15843. [Google Scholar]
- Mani A, Mullainathan S, Shafir E and Zhao J. 2013. “Poverty Impedes Cognitive Function.” Science (New York, N.Y.) 341(6149):976–980. doi: 10.1126/science.1238041 [doi]. [DOI] [PubMed] [Google Scholar]
- Marmot Michael. 2004. “Status syndrome.” Significance 1(4): 150–154. [Google Scholar]
- McEwen Bruce S. 1998. “Stress, Adaptation, and Disease: Allostasis and Allostatic Load.” Annals of the New York Academy of Sciences 840(1):33–44. [DOI] [PubMed] [Google Scholar]
- McEwen Bruce S. 2017. “Neurobiological and systemic effects of chronic stress.” Chronic Stress 1: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver Melvin L. and Shapiro Thomas M.. 2006. “Black Wealth/White Wealth.” New York: Routledge. [Google Scholar]
- Pearson Jay A. 2008. “Can’t buy me whiteness: New lessons from the Titanic on race, ethnicity, and health.” Du Bois Review: Social Science Research on Race 5(1): 27–47. [Google Scholar]
- Pfeffer Fabian T., Danziger Sheldon and Schoeni Robert F.. 2013. “Wealth Disparities before and After the Great Recession.” The Annals of the American Academy of Political and Social Science 650(1):98–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan Jo C. and Link Bruce G.. 2015. “Is Racism a Fundamental Cause of Inequalities in Health?” Annual Review of Sociology 41:311–330. [Google Scholar]
- Rose D 1999. “Economic determinants and dietary consequences of food insecurity in the United States.” The Journal of Nutrition 129(2): 517S–520S. [DOI] [PubMed] [Google Scholar]
- Rossi Peter H., and Weber Eleanor. 1996. “The social benefits of homeownership: Empirical evidence from national surveys.” Housing Policy Debate 7(1): 1–35. [Google Scholar]
- Rugh Jacob S. Forthcoming. “Why Black and Latino Home Ownership Matter to the Color Line and Multiracial Democracy.” Race and Social Problems: 1–20. [Google Scholar]
- Sewell AA 2016. “The racism-race reification process: a mesolevel political economic framework for understanding racial health disparities.” Sociology of Race and Ethnicity 2(4): 402–432. [Google Scholar]
- Shuey Kim M. and Willson Andrea E.. 2008. “Cumulative Disadvantage and Black-White Disparities in Life-Course Health Trajectories.” Research on Aging 30(2):200–225. [Google Scholar]
- Sousa Ricardo M. 2009. “Wealth Effects on Consumption-Evidence from the Euro Area.”. [Google Scholar]
- Spilerman Seymour. 2000. “Wealth and Stratification Processes.” Annual Review of Sociology 26:497–524. [Google Scholar]
- Sweet Elizabeth, Nandi Arijit, Adam Emma K. and McDade Thomas W.. 2013. “The High Price of Debt: Household Financial Debt and its Impact on Mental and Physical Health.” Social Science & Medicine 91:94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turunen Elina, and Hiilamo Heikki. 2014. “Health effects of indebtedness: a systematic review.” BMC Public Health 14(1): 489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall TP, Vujicic M and Nasseh K. 2012. “Recent Trends in the Utilization of Dental Care in the United States.” Journal of Dental Education 76(8):1020–1027. doi: 76/8/1020 [pii]. [PubMed] [Google Scholar]
- Williams David R., Mohammed Selina A., Leavell Jacinta and Collins Chiquita. 2010. “Race, Socioeconomic Status, and Health: Complexities, Ongoing Challenges, and Research Opportunities.” Annals of the New York Academy of Sciences 1186(1):69–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willson Andrea E., Shuey Kim M. and Elder Glen H. Jr. 2007. “Cumulative Advantage Processes as Mechanisms of Inequality in Life Course Health1.” American Journal of Sociology 112(6):1886–1924. [Google Scholar]
- Wolff Edward N. 2016. “Household Wealth Trends in the United States, 1962 to 2013: What Happened Over the Great Recession?” Russel Sage Foundation Report. [Google Scholar]
- Yilmazer Tansel, Babiarz Patryk and Liu Fen. 2015. “The Impact of Diminished Housing Wealth on Health in the United States: Evidence from the Great Recession.” Social Science & Medicine 130:234–241. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


