Abstract
Objective:
The purpose of this study was to examine the relationships between medical mistrust and trust and to determine if these measures differentially predict antiretroviral therapy (ART) medication adherence for African American adults living with HIV.
Design:
A total of 458 HIV positive African Americans completed a cross-sectional survey.
Main Outcome Measures:
Self-reported ART adherence was collected using the visual-analog scale. The Beliefs About Medicines Questionnaire was used to assess medication necessity and concern beliefs.
Results:
All measures of medical mistrust and trust were significantly negatively correlated, ranging from r = − 0.339 to −0.504. Race-based medical mistrust significantly predicted medication necessity and concern beliefs, whereas general medical mistrust only significantly predicted medication concerns. Both measures of trust significantly predicted medication necessity beliefs and medication concerns. Higher levels of race-based medical mistrust predicted lower medication adherence, whereas, neither trust in own physician nor trust in healthcare provider significantly predicted medication adherence. However, trust in own physician significantly predicted medication necessity beliefs which predicted medication adherence.
Conclusion:
Trust and mistrust are not simply opposites of one another. These findings provide evidence for the complexity of understanding the relationship between health care trust, mistrust, and patient-related health beliefs and behaviors.
Keywords: trust in physician, medication adherence, African Americans, HIV
Medical mistrust is common, particularly among racial minorities. Often this mistrust is attributed to historical instances of maltreatment by medical and research institutions, such as the Tuskegee Syphilis Study among Africa Americans (Ball, Lawson, & Alim, 2013). In addition to historical instances of mistreatment, individual experiences of perceived racism and discrimination of minority patients within patient-provider interactions also impact an individual’s mistrust of their own provider as well as the institution (LaVeist, Nickerson, & Bowie, 2000; López-Cevallos, Harvey, & Warren, 2014). Medical mistrust among African Americans negatively influences many health behaviors, including engagement in preventive health services and disease management (Eaton et al., 2015; Hammond, Matthews, Mohottige, Agyemang, & Corbie-Smith, 2010; Sheppard, Mays, LaVeist, & Tercyak, 2013). Among a sample of Black women, for example, high levels of mistrust were associated with lower engagement in genetic counseling and testing for breast cancer (Sheppard, Mays, LaVeist, & Tercyak, 2013). High levels of medical mistrust are also associated with longer delays in routine check-ups (Hammond et al., 2010). Eaton et al. (2015) also found similar results among Black men who have sex with men: global medical mistrust predicted longer gaps in time since participants’ last medical exam. Additionally, medical mistrust mediated the relationship between the participant’s reported racial and sexual orientation stigma and their engagement in care (Eaton et al., 2015).
Medical mistrust is also a concern among people living with HIV. Dale, Bogart, Wagner, Galvan, and Klein (2016) found that general medical mistrust longitudinally predicted lower antiretroviral therapy (ART) adherence. Conversely, they found that racism-related mistrust, or the belief that providers treat African Americans poorly due to race, did not predict ART adherence. This finding suggests that there may be a difference in the way race driven mistrust of the healthcare system impacts health behaviors as opposed to the more general mistrust of the institution. Finally, treatment-related conspiracy beliefs may exemplify medical mistrust. Endorsement of statements such as “people who take antiretroviral treatments are human guinea pigs for the government” is associated with poorer ART adherence (Bogart, Wagner, Galvan, & Banks, 2010).
Beliefs about medications may play a mediating role in the impact that trusting or mistrusting one’s own physician has on medication adherence (Thrasher, Earp, Golin, & Zimmer, 2008). Kalichman, Eaton, and Cherry (2010) found that one in five people living with HIV endorsed the statement “HIV treatments do more harm than good” and that those who endorsed these beliefs were significantly less likely to use ART. In a subsequent study Kalichman, Eaton, Kalichman and Cherry (in press) conducted a multiple meditational analysis to test Horne’s Necessity-Concerns Framework, a model used to investigate the extent to which an individual believes their medications are necessary and the extent to which they have concerns about the effects of their medications (Horne, Cooper, Gellaitry, Date, & Fisher, 2007; Horne et al., 2013) as mediators of the relationship between race-based medical suspicion and ART adherence. The authors found that concerns about medications mediated the relationship but believing that medications are necessary did not. This analysis, however, does not take into account the potential influence of trust in one’s own physician. Although general medical mistrust is assumed to negatively correlate with trust in one’s own physician, this is not a one-to-one correlation (Earl et al., 2013). Thus, individual differences in trust in one’s own physician versus general medical mistrust may exhibit different relationships with beliefs and subsequent adherence behaviors.
This relationship between trust in one’s own physician and medication adherence may be particularly important in historically disenfranchised or oppressed groups, like African Americans and HIV positive individuals. Both of these groups, as well as the intersection of African Americans who have HIV, have a history of being treated poorly by health care workers as well as the healthcare system as an institution (Halbert, Armstrong, Gandy, et al., 2006; Jacobs, Rolle, Ferrans, et al., 2006) and this may explain why trust in physicians is often diminished in these groups (Boulware, Cooper, Ratner, LaVeist, & Powe, 2003; Saha, Jacobs, Moore, & Beach, 2010). However, having trust in one’s physician is vital to a variety of health outcomes, including adherence to medications (Piette, Heisler, Krein, & Kerr, 2005). Trust in a patient’s physician is a strong predictor of treatment adherence among people living with HIV (Altice, Mostashari & Friedland, 2001; Blackstock, Addison, Brennan & Alao, 2012), with greater trust being linked to greater adherence.
Trust and mistrust are not simply opposites of one another; an individual can both trust their own physician and be generally mistrustful of healthcare providers. The purpose of this study was to explore the relationships between trust and mistrust and to determine if measures of trust and mistrust differentially predict ART medication adherence for African American adults living with HIV. Finally, using structural equation modeling, we tested the relationships between trust, mistrust, medication beliefs and medication adherence to extend previous research.
Methods
Procedure
A cross-sectional survey was designed to assess participants’ perceptions about medical institutions as well as their own physician. The survey also assessed beliefs about antiretroviral medications and self-reported adherence. Assessments were completed anonymously using audio-computer assisted self-interview (ACASI) on password protected tablets. Participants were men and women living with HIV who were attending a holiday grocery store gift card giveaway at a community-based research site in Atlanta, GA. In order to participate in the cross-sectional survey, participants had to be 18 or older, English speaking, and had to present proof of HIV positive status (i.e. presenting a photo-identification along with a name matching ART prescription, medication bottle, HIV clinic card or other verification of HIV status). Participants were not excluded based on reading level or sight/hearing impairment as the assessment was collected via ACASI and staff members were available if participants needed assistance or had questions.
Measures
Participants completed basic demographic information including gender identity, sexual orientation, education, employment, and age. Participants also self-reported whether their most recent HIV viral load test was detectable or undetectable and what the value of their most recent CD4 T cell count was with the option of ‘I don’t know’.
General medical mistrust.
Three items from the Medical Mistrust Index (MMI; LaVeist, 2000) were adapted to address general mistrust of health care providers. Example items are “Patients have sometimes been deceived or misled by healthcare providers” and “When healthcare providers make mistakes they usually cover it up.” Items were responded to on a 5-point Likert scale, 1 = Strongly Agree, 5 = Strongly Disagree, and were coded such that higher scores indicated higher levels of mistrust of healthcare providers (α = 0.89).
Race-based medical mistrust.
Participants completed the discrimination and suspicion subscales of the Group-Based Medical Mistrust Scale (GBMMS; Shelton et al., 2010). Items were modified to indicate self-identified race because participants in the study may identify as Black or African American. A sample item is “People of my race cannot trust doctors and health care workers.” Items were responded to on a 5-point Likert scale, 1 = Strongly Agree, 5 = Strongly Disagree, and were coded such that higher scores indicated higher levels of medical mistrust (α = 0.89). When analyzed as subscales, the suspicion and discrimination scales both demonstrated acceptable reliability (α = 0.89, α = 0.79, respectively).
Trust in own physician.
Six items of the Trust in Physician Scale (Freburger, Callahan, Currey & Anderson, 2003) were used to assess participants’ feelings about their own physician. Example items are “My doctor is usually considerate of my needs and puts them first” and “I trust my doctor’s judgments about my medical care.” Items were responded to on a 5-point Likert scale, 1 = Strongly Agree, 5 = Strongly Disagree, and were coded such that higher scores indicated higher levels of trust in own physician (α = 0.82).
Trust in health care providers.
Three items were created to assess trust in health care providers more broadly. These items were “I trust that my healthcare providers are giving me the best treatment available,” “I trust that my healthcare providers have my best interest in mind when treating me,” and “I trust that my healthcare providers will tell me if a mistake is made about my medical treatment.” Items were responded to on a 5-point Likert scale, 1 = Strongly Agree, 5 = Strongly Disagree, and were coded such that higher scores indicated higher levels of trust in healthcare providers (Cronbach’s α = 0.92).
Medication necessity and concern beliefs.
We utilized the Beliefs About Medicines Questionnaire (Horne, Weinman, & Hankins, 1999) to assess participants’ concerns about their HIV medications as well as their beliefs about the necessity to take them in order to stay healthy. In Horne’s Necessity-Concerns Framework (Horne, Cooper, Gellaitry, Date, & Fisher, 2007; Horne et al., 2013) these scales are defined as two independent constructs. The medication necessity scale is comprised of 5 items focused on the benefits of ART medications. An example item is “Without my HIV medicines, I would be very ill.” The medication concerns scale is comprised of 5 items reflecting apprehension and the potential negative effects of taking these medications. An example item is “I sometimes worry about long-term effects of my HIV medicines.” All necessity and concern beliefs were responded to on a 5-point Likert scale, 1 = Strongly Agree, 5 = Strongly Disagree. Responses were coded such that higher scores on each scale indicated greater necessity beliefs and greater concerns (necessity beliefs Cronbach’s α = 0.77, concern beliefs Cronbach’s α = 0.80).
ART adherence.
The visual analog scale (VAS) was used to assess adherence. The VAS is a horizontal number line ranging from 0 to 100. Participants were instructed to click on the number line to indicate what percent of HIV medications they thought they took during the past month. This simple measure has been found to correlate strongly with more in-depth measures of self-report and reasonably well with more objective measures of ART adherence (i.e. pill count; viral load; Finitsis, Pellowski, Huedo-Medina, Fox, & Kalichman, 2016; Kalichman et al., 2009).
Statistical Analyses
For these analyses, only people who identified as Black or African American were included. To characterize the sample, means and rates were calculated. Bivariate correlations were calculated to determine the relationships between the measures of mistrust and trust; Pearson’s r’s are reported. For participants who reported being on antiretroviral therapy, bivariate regressions were conducted to determine the impact of differing measures of mistrust and trust on medication necessity and concern beliefs and on antiretroviral adherence; standardized betas are reported.
Trust in one’s physician, race-based medical mistrust, medication necessity and concern beliefs were modeled using latent variables. Measurement models of these latent variables were conducted first. Error variances that had modification indices >20 were correlated. A structural equation model (SEM) was tested investigating the simultaneous relationships between trust in one’s physician, race-based medical mistrust, medication necessity and concern beliefs and how well these constructs predict medication adherence. The SEM controlled for gender, education, and time since testing HIV positive. Model fit was determined using the Tucker-Lewis Index (TLI>0.90 good fit) and the Root Mean Square Error of Approximation (RMSEA > 0.05 good fit; > 0.08 acceptable fit; MacCallum, Browne, & Sugawara, 1996). IBM SPSS Amos 24 was used for the measurement and structural models (Arbuckle, 2006). Missing data was handled through full information maximum likelihood in AMOS (Allison, 2003).
Results
This study consisted of 458 men and women living with HIV who identify as Black or African American (Table 1). The majority of participants were male (68.3%), middle-aged (M=47.9, SD = 9.3) and on disability (55.5%) or unemployment (22.9%). This sample was fairly well educated with 366 participants having completed high school or more (79.9%). Additionally, they were fairly healthy; the majority of participants had an undetectable HIV RNA viral load (84.5%) and a CD4 T-cell count greater than 200 (79.0%) and had been living with HIV for a substantial amount of time (M=15.4 years, SD=8.7). A total of 385 participants reported being on antiretroviral therapy (ART) with an average adherence of 89.6% on the visual analog scale (VAS). Because of the negative skew in this measure, it was transformed using the formula log10(x+1) for regression analyses.
Table 1:
Demographic characteristics of 458 Africa American adults living with HIV
| Characteristic | N | % |
|---|---|---|
| Gender Identity^ | ||
| Male | 313 | 68.3 |
| Female | 140 | 30.9 |
| Sexual Orientation | ||
| Gay/Homosexual | 199 | 43.4 |
| Bisexual | 63 | 13.8 |
| Straight/Heterosexual | 195 | 42.6 |
| Education | ||
| Less than H.S. | 92 | 20.1 |
| H.S. Diploma/GED | 160 | 34.9 |
| More than H.S. | 206 | 45 |
| Employment/Income | ||
| Working Full Time | 42 | 9.2 |
| Working Part Time | 43 | 9.4 |
| On disability | 254 | 55.5 |
| Unemployed | 105 | 22.9 |
| Student | 5 | 1.1 |
| Other | 9 | 2 |
| On ART | ||
| Yes | 385 | 84.1 |
| No | 72 | 15.7 |
| CD4 T-Cell Count | ||
| Less than or equal to 200 | 39 | 8.5 |
| Great than 200 | 362 | 79 |
| Unknown | 57 | 12.4 |
| HIV viral load | ||
| Detectable | 58 | 12.7 |
| Undetectable | 387 | 84.5 |
| Unknown | 13 | 2.8 |
| M | SD | |
| Age | 47.9 | 9.3 |
| Years since diagnosis | 15.4 | 8.7 |
| VAS | 89.6 | 19.4 |
5 participants did not identify a gender
Correlations Between Measures of Mistrust and Trust
Table 2 shows a correlation matrix of the two measures of mistrust (including subscales) and the two measures of trust. All measures of mistrust were significantly positively correlated with one another; general medical mistrust and race-based medical mistrust were positively correlated (r = 0.684, p<0.001). Trust in own physician and trust in healthcare providers were also positively correlated (r = 0.781, p<0.001). As predicted, all measures of trust were significantly negatively correlated with the measures of mistrust.
Table 2:
Correlation matrix examining the relationships between all measures of mistrust and trust, N=458
| General Medical Mistrust | Race-Based Medical Mistrust | Suspicion Subscale | Discrimination Subscale | Trust in own Physician | Trust in Healthcare Providers | |
|---|---|---|---|---|---|---|
| General Medical Mistrust | 1.000 | 0.684*** | 0.640*** | 0.611*** | −0.406*** | −0.339*** |
| Race-Based Medical Mistrust | 1.000 | 0.899*** | 0.924*** | −0.504*** | −0.441*** | |
| Suspicion Subscale | 1.000 | 0.662*** | −0.428*** | −0.379*** | ||
| Discrimination Subscale | 1.000 | −0.488*** | −0.422*** | |||
| Trust in own Physician | 1.000 | 0.781*** | ||||
| Trust in Healthcare Providers | 1.000 |
p<0.001
Bivariate Regressions Predicting Medication Necessity and Concern Beliefs and ART Adherence
Both measures of trust positively predicted medication necessity beliefs, indicating that individual with higher levels of trust in both their physician and healthcare providers had greater beliefs that their medications were necessary to their health (Table 3). The predictive value of the medical mistrust measures on medication necessity beliefs was mixed. Race-based medical mistrust significantly negatively predicted medication necessity beliefs (β = −0.144, p<0.01), such that individuals with higher levels of mistrust were less likely to believe that their medications were necessary, and this was largely driven by the discrimination subscale of the measure (β = −0.183, p<0.001). General medical mistrust and the suspicion subscale of the race-based medical mistrust did not significantly predict medication necessity beliefs.
Table 3:
Bivariate regressions predicting medication necessity and concern beliefs and bivariate regression predicting antiretroviral adherence, N=385
| Predicting Medication Necessity Beliefs | Predicting Medication Concern Beliefs | Predicting Adherence | |||
|---|---|---|---|---|---|
| General Medical Mistrust | −0.056 | 0.364*** | −0.060 | ||
| Race-Based Medical Mistrust | −0.144** | 0.483*** | −0.115* | ||
| Suspicion Subscale | 0.072 | 0.472*** | −0.142** | ||
| Discrimination Subscale | −0.183*** | 0.416*** | −0.073 | ||
| Trust in own Physician | 0.287*** | −0.307*** | 0.023 | ||
| Trust in Healthcare Providers | 0.239*** | −0.286*** | 0.027 | ||
| Medication Necessity Beliefs | - | - | 0.097^ | ||
| Medication Concern Beliefs | - | - | −0.124* |
p<0.10,
p<0.05,
p<0.01
All measures of medical mistrust significantly and negatively predicted medication concern beliefs, indicating that individuals with higher levels of medical mistrust endorsed more concerns about their medications. Both measures of trust also significantly predicted medication concerns but in the opposite direction, such that those with higher levels of trust in their own physician and in healthcare providers in general were less concerned about their medications.
The two measures of medical mistrust differed in how well they predicted medication adherence: general medical mistrust did not predict ART adherence, however, race-based medical mistrust did significantly predict medication adherence (β = −0.115, p<0.05); individuals with higher levels of race-based medical mistrust had lower adherence. This seems to be driven by the suspicion subscale of this measure (β = −0.142, p<0.01). Trust in healthcare providers did not significantly predict medication adherence nor did trust in own physician. Greater medication concern beliefs were significantly associated with poorer medication adherence (β = −0.124, p<0.05). Greater medication necessity beliefs were associated with better self-reported medication adherence; however, this was not significant at conventional levels (β = 0.097, p=0.057).
Structural Equation Model Predicting ART Adherence
A structural equation model was conducted to determine the relationships between the constructs simultaneously and how they predict medication adherence as measured by the VAS (Figure 1). The model had good fit (X2 = 702.60, df = 364, p<0.001; TLI =0 .915; RMSEA = 0.059). Trust in own doctor and race-based medical mistrust were highly, negatively correlated (r = −0.508, p<0.001). Trust in own physician significantly positively predicted medication necessity beliefs (β =−0.433, p<0.001) but did not predict medication concern beliefs when controlling for race-based medical mistrust (β = 0.019, p = 0.75). Additionally, race-based medical mistrust significantly predicted medication concern beliefs (β =0.607, p<0.001) and positively predicted medication necessity beliefs, although not significantly when controlling for trust in own physician (β =0.117, p = 0.091). Medication necessity beliefs significantly predicted medication adherence (β = 0.132, p<0.05), such that higher necessity beliefs predicted higher medication adherence. Medication concern beliefs did not significantly predict ART adherence (β =−0.087, p=0.241). Finally, neither trust in own physician nor race-based medical mistrust significantly predicted medication adherence directly at conventional significance levels (β = −0.115, p =0.102; β = −0.139, p=0.089, respectively).
Figure 1:
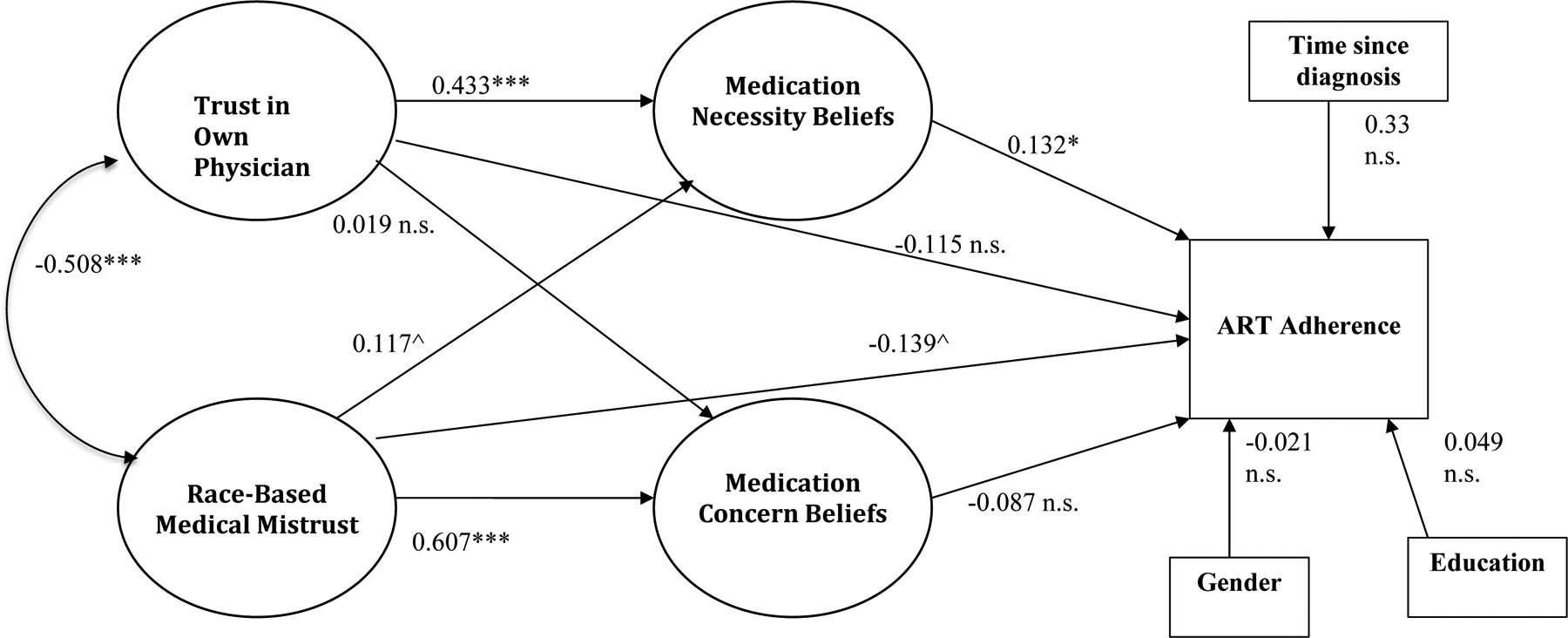
Structural equation model of the relationships between trust in own doctor, race-based medical mistrust, medication beliefs, and ART adherence, N=385
Note: all data presented in figure is new
n.s. = not significant, ^p<0.10, *p<0.05, ***p<0.001
Fit indices:
X2 = 702.60, df = 364, p<0.001
TLI = 0.915
RMSEA = 0.049
Discussion
This study provides greater insight into the roles that medical mistrust and trust in one’s own physician have on medication beliefs and the subsequent impact these constructs have on ART adherence. Medical mistrust and trust are highly, but not perfectly, correlated and, subsequently, have differing impacts on medication beliefs and medication adherence. In general, both medical mistrust and trust predicted medication concerns in their expected directions; higher levels of medical mistrust was associated with greater medication concerns, whereas greater trust in physicians and health care providers was associated with less concerns about medications. Conversely, greater trust in physicians and healthcare providers was significantly associated with higher levels of believing that medications are necessary for maintaining health. However, measures of medical mistrust were not consistently associated with medication necessity beliefs. These findings illustrate that there are some specific differences in how measures of medical mistrust and trust operate with regard to impacting medication beliefs, and measures of medical mistrust and trust are not simply opposites of one another.
Additionally, the current study indicates that although general medical mistrust and race-based medical mistrust were highly correlated, only race-based mistrust significantly predicted medication adherence, bivariately. This is the opposite of what Dale et al. (2016) found in their longitudinal study of African American men living with HIV in Los Angeles. These differences may be due to geographical differences in the HIV epidemic and possibly differences in experiences of discrimination dependent on area of the country and racial climates. This underscores the importance of using multiple measures of medical mistrust in order to better understand these relations and to tailor interventions to specific contexts. Additionally, these differences may exist due to study design (i.e. cross-sectional versus longitudinal). It is plausible that race-based medical mistrust predicts current ART non-adherence but does not predict it over time.
The amount of trust a patient has towards their physician did not directly impact their medication adherence, however, it was significantly related to medication necessity beliefs. This finding adds insight into the literature that focuses solely on the impact of the patient-provider relationship to adherence. The lack of a direct link between trust in own physician and medication adherence, both bivariately and in the structural equation model, in comparison to the direct relationship between race-based medical mistrust, bivariately and trending on significance in the SEM, highlights that individuals affected by HIV may not be as impacted by individual experiences in the healthcare system as much as perceived institutional discrimination directed at the racial group that they are a part of (Beach, Keruly, & Moore, 2006; Sankar, Neufeld, Berry, & Luborsky, 2011; Whetten et al., 2006). Further investigation, particularly in the form of qualitative research, is needed to disentangle individuals’ experiences and perceptions of their own doctors’ biases, interpersonal interactions, and treatment decisions, in contrast to healthcare providers in general, in order to better understand the findings from the current study.
There are several limitations to the current study. First, the VAS was used as a measure of medication adherence for this study. As a measure of self-report, it is known to be positively biased, such that individuals tend to report being more adherent compared to more objective measures such as unannounced pill count and pharmacy refill data, however, it is well correlated with these measures and other self-reported measures of non-adherence (Finitsis et al., 2016). Given that there is no gold standard for medication adherence measurement, this study should be replicated with additional measures of adherence, both objective and subjective. Secondly, the study design was cross-sectional and thus, the findings cannot be claimed as causal. As time progresses, medical trust and mistrust may change based on individual experiences. Additionally, medication beliefs can change over time and in turn influence medication adherence (Aikens & Klinkman, 2012; Schuz et al., 2011). Investigating changes over time in trust, mistrust, and medication beliefs would be a valuable next step in this line of research. Third, although our sample size was large, it was fairly healthy with the majority of participants having undetectable viral loads and CD4 T cell counts greater than 200. Thus, these findings may not extend to less healthy samples. Fourth, we did not collect information about the race of the participant’s healthcare providers or main HIV care physician. Previous research has shown mixed results in regards to the benefits of patient-provider race concordance for minority patients (Jerant, Bertakis, Fenton, Tancredi, & Franks, 2011; Meghani et al., 2009; Sweeney, Zinner, Rust, & Fryer, 2016). However, race of provider may still influence how much a patient trusts them or a patient’s general trust in the healthcare system (Sohler, Fitzpatrick, Lindsay, Anastos, & Cunningham, 2007). Unfortunately, we cannot explore this influence with the current data. Lastly, our sample was older and living with HIV for a substantial amount of time. This may have implications for the measures of trust and mistrust. History-based theories of trust suggest that trust is a product of many cumulative experiences and interactions over years (Hammond, 2010; Kramer 1999). Because our sample has been living with HIV for some time, these cumulative healthcare experiences may push the amount of trust and mistrust individuals have to the extreme. It is possible that people living with HIV for a shorter amount of time may not have had as many interactions with the healthcare system and their doctors, which may impact how well trust and mistrust relate to medication beliefs and adherence.
There is still more to learn about the relationships between trust and mistrust of the healthcare system, its workers, and its effects on medication adherence. Nevertheless, our findings offer how important considerations for future interventions that focus on HIV medication adherence, particularly in African American communities. A systematic review on African American’s beliefs about their HIV care on treatment adherence found similar themes of race-based medical mistrust impacting ART adherence (Gaston, & Alleyne-Green, 2013). Recommendations for interventions include that providers to openly evaluate their personal beliefs that could adversely affect their treatment decisions, listen to patient narratives, and share treatment decisions in order to create a transparent clinical environment. Additional research should also focus on the causes of race-based medical mistrust other than patient-provider interactions, such as media portrayals of African American patients and their (often White) providers, to identify other potential avenues of intervention. Addressing the multiple sources of patient experiences and beliefs should be a priority in advancing HIV care for minority populations.
Funding:
This study was funded by the National Institute on Drug Abuse under grant R01DA033067 and the National Institute of Mental Health under grants T32MH074387 and T32MH078788.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Aikens JE & Klinkman MS (2012). Changes in patients’ beliefs about their antidepressant during the acute phase of depression treatment. General Hospital Psychiatry, 34, 3, 221–226. [DOI] [PubMed] [Google Scholar]
- Allison PD (2003). Missing data techniques for structural equation modeling. Journal of Abnormal Psychology, 112, 4, 545–557. [DOI] [PubMed] [Google Scholar]
- Altice FL, Mostashari F, & Friedland GH (2001). Trust and the acceptance of and adherence to antiretroviral therapy. Journal of Acquired Immuno Deficiency Syndromes, 28, 1, 47–58. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL (2006). Amos (Version 7.0) [Computer Program]. Chicago: SPSS. [Google Scholar]
- Ball K, Lawson W, & Alim T (2013). Medical mistrust, conspiracy beliefs & HIV-related behavior among African Americans. Journal of Psychology and Behavioral Science, 1, 1–7. [Google Scholar]
- Beach MC, Keruly J, & Moore RD (2006). Is the quality of the patient-provider relationship associated with better adherence and health outcomes for patients with HIV? Journal of General Internal Medicine, 21, 661–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackstock OJ, Addison DN, Brennan JS, & Alao OA (2012). Trust in primary care providers and antiretroviral adherence in an urban HIV clinic. Journal of Health Care for the Poor and Underserved, 23, 1, 88–98. [DOI] [PubMed] [Google Scholar]
- Bogart LM, Wagner G, Galvan FH, & Banks D (2010). Conspiracy beliefs about HIV are related to antiretroviral treatment nonadherence among African-American men with HIV. Journal of Acquired Immuno Deficiency Syndromes, 53, 5, 648–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulware LE, Cooper LA, Ratner LE, LaVeist TA, & Powe NR (2003). Race and trust in the health care system. Public Health Reports, 118, 4, 358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale SK, Bogart LM, Wagner GJ, Galvan FH, & Klein DJ (2016). Medical mistrust is related to lower longitudinal medication adherence among African-American males with HIV. Journal of Health Psychology, 21, 7, 1311–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earl TR, Beach MC, Lombe M, Korthuis PT, Sharp VL, Cohn JA, … Saha S (2013). Race, relationships and trust in providers among Black patients with HIV/AIDS. Social Work Research, 37, 3, 219–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton L, Driffin DD, Kegler C, Smith H, Conway-Washington C, White D, & Cherry C (2015). The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. American Journal of Public Health, 105, 2, e75–e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finitsis DJ, Pellowski JA, Huedo-Medina TB, Fox MC, & Kalichman SC (2016). Visual analog scale (VAS) measurement of antiretroviral adherence in people living with HIV: A meta-analysis. Journal of Behavioral Medicine, 39, 6, 1043–1055. [DOI] [PubMed] [Google Scholar]
- Freburger JK, Callahan LF, Currey SS & Anderson LA (2003). Use of the trust in physician scale in patients with rheumatic disease: psychometric properties and correlates of trust in the rheumatologist. Arthritis & Rheumatism (Arthritis Care & Research), 49, 1, 51–58. [DOI] [PubMed] [Google Scholar]
- Gaston GB, & Alleyne-Green B (2013). The impact of African Americans’ beliefs about HIV medical care on treatment adherence: a systematic review and recommendations for interventions. AIDS and Behavior, 17, 1, 31–40. [DOI] [PubMed] [Google Scholar]
- Halbert CH, Armstrong K, Gandy OH, & Shaker L (2006). Racial differences in trust in health care providers. Archives of Internal Medicine, 166, 8, 896–901. [DOI] [PubMed] [Google Scholar]
- Hammond WP (2010). Psychosocial correlates of medical mistrust among African Americanmen. American Journal of Community Psychology, 45, 87–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond WP, Matthews D, Mohottige D, Agyemang A, & Corbie-Smith G (2010). Masculinity, medical mistrust, and preventive health services delays among community-dwelling African-American men. Journal of General Internal Medicine, 25, 12, 1300–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R, Chapman SCE, Parham R, Freemantle N Forbes A, & Cooper V (2013). Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PLOS One, 8, 12, e80633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R, Cooper V, Gellaitry G, Date HL, & Fisher M (2007). Patients’ perceptions of highly active antiretroviral therapy in relation to treatment uptake and adherence. Journal of Acquired Immuno Deficiency Syndromes, 45, 3, 334–341. [DOI] [PubMed] [Google Scholar]
- Horne R, Weinman J, & Hankins M (1999). The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychology & Health, 14, 1–24 [Google Scholar]
- Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, & Warnecke RB (2006). Understanding African Americans’ views of the trustworthiness of physicians. Journal of General Internal Medicine, 21, 6, 642–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerant A, Bertakis KD, Fenton JJ, Tancredi DJ, & Franks P (2011). Patient-provider sex and race/ethnicity concordance: a national study of healthcare and outcomes. Medical Care, 49, 11, 1012–1020. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Amaral CM, Swetzes C, Jones M, Macy R, Kalichman MO, & Cherry C (2009). A simple single-item rating scale to measure medication adherence: further evidence for convergent validity. Journal of the International Association of Physicians in AIDS Care, 8, 6 367–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Eaton L, & Cherry C (2010). There is no proof that HIV causes AIDS: AIDS denialism beliefs among people living with HIV/AIDS. Journal of Behavioral Medicine, 33, 6, 432–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Eaton L, Kalichman MO, & Cherry C (in press). Medication beliefs mediate the association between medical mistrust and antiretroviral adherence among African Americans living with HIV/AIDS. Journal of Health Psychology, [DOI] [PubMed] [Google Scholar]
- Kramer R Trust and distrust in organizations: Emerging perspectives, enduring questions. Annual Review of Psychology, 50, 569–598. [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Nickerson KJ, & Bowie JV (2000). Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Medical Care Research and Review, 57, 146–161. [DOI] [PubMed] [Google Scholar]
- López-Cevallos DF, Harvey SM, & Warren JT (2014). Medical mistrust, perceived discrimination, and satisfaction with health care among young-adult rural Latinos. Journal of Rural Health, 30, 344–351. [DOI] [PubMed] [Google Scholar]
- Meghani SH, Brooks JM, Gipson-Jones T, Waite R, Whitfield-Harris L, & Deatrick JA (2009). Patient-provider race-concordance: does it matter in improving minority patients’ health outcomes. Ethnicity & Health, 14, 1, 107–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette JD, Heisler M, Krein S, & Kerr EA (2005). The role of patient-physician trust in moderating medication nonadherence due to cost pressures. Archives of Internal Medicine, 165(15): 1749–1755. [DOI] [PubMed] [Google Scholar]
- Saha S, Jacobs EA, Moore RD, & Beach MC (2010). Trust in physicians and racial disparities in HIV care. AIDS Patient Care and STDS, 24, 7, 415–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar S, Neufelf S, Berry R, & Luborsky M (2011). Cultural rationales guiding medication adherence among African American with HIV/AIDS. AIDS Patient Care and STDS, 25, 9, 547–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuz B, Wurm S, Ziegelmann JP, Warner LM, Tesch-Romer C, & Schwarzer R (2011). Changes in functional health, changes in medication beliefs, and medication adherence. Health Psychology, 30, 1, 31–39. [DOI] [PubMed] [Google Scholar]
- Shelton RC, Winkel G, Davis SN, Roberts N, Heiddis V, Hall SJ, & Thompson HS (2010). Validation of the group-based medical provider mistrust scale among urban Black men. Journal of General Internal Medicine, 25 (6): 549–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppard VB, Mays D, LaVeist T, & Tercyak KP (2013). Medical mistrust influences black women’s level of engagement in BRCA 1/2 genetic counseling and testing. Journal of the National Medical Association, 105, 1, 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohler NL, Fitzpatrick LK, Lindsay RG, Anastos K, & Cunningham CO (2007). Does patient-provider racial/ethnic concordance influence ratings of trust in people with HIV infection? AIDS and Behavior, 11, 6, 884–896. [DOI] [PubMed] [Google Scholar]
- Sweeney CF, Zinner D, Rust G, & Fryer GE (2016). Race/ethnicity and health care communication: does patient-provider concordance matter? Medical Care, 54, 11, 1005–1009 [DOI] [PubMed] [Google Scholar]
- Thrasher AD, Earp JA, Golin CE, & Zimmer CR (2008). Discrimination, distrust, and racial/ethnic disparities in antiretroviral therapy adherence among a national sample of HIV-infected patients. Journal of Acquired Immuno Deficiency Syndromes, 49, 1, 84–93. [DOI] [PubMed] [Google Scholar]
- Whetten K, Leserman J, Whetten R, Ostermann J, Thielman N, Swartz M, & Stangl D (2006). Exploring lack of trust in care providers and the government as a barrier to health services use. American Journal of Public Health, 96, 4, 716–721. [DOI] [PMC free article] [PubMed] [Google Scholar]


