1. INTRODUCTION
Myringostapediopexy has been defined as a retraction of the tympanic membrane limited to the posterosuperior region, in which there is erosion of the long process of the incus and fixation of the affected tympanic segment to the stapes head. While it has been suggested that natural myringostapediopexy alone does not result in clinically relevant conductive hearing loss, discontinuity of the incudostapedial joint can cause significant conductive hearing loss requiring ossiculopasty.1, 2 A systematic review has shown the use of hydroxyapatite biocement is effective in closing air-bone gap for these patients; however, this is generally an elective surgical procedure performed in the operating room.2
A 24-year-old patient presented to the otology clinic at the UC Irvine Medical Center, Orange, CA with conductive hearing loss. On exam she had myringostapediopexy and had a previously-placed tympanostomy tube which had not helped her hearing. She was pregnant and losing her insurance within a few weeks and could not purchase a hearing aid. After discussion of the options, she elected to have an office-based ossicular chain reconstruction using hydroxyapatite bone cement using a transtympanic approach.
2. TECHNICAL DESCRIPTION
A cotton ball was impregnated with benzocaine spray and applied to the ear canal for 15 minutes. The ear was prepped with betadine and draped in a sterile fashion. Under guidance of the microscope, the stapes was visualized through the tympanic membrane. An approximately 3 mm × 1mm segment of the tympanic membrane was anesthetized with a 90% liquified phenol applicator (Apdyne, Denver, CO, USA). A myringotomy was performed in the posterosuperior quadrant approximately 1.5 mm posterior to the observed adhesion. Using a sickle knife, the tympanic membrane was separated from the incus and the superior aspect of the stapes capitulum. Due to significant adhesion, the tympanic membrane was not entirely freed from the inferior aspect of the stapes capitulum. There was a thin fibrous band between the incus long process remnant and stapes capitulum. Hydroxyapatite bone cement (OtoMimix, Olympus, PA, USA) was used to bridge the incus and stapes for reconstruction of the ossicular chain. The cement was then dried with a 20-gauge suction passed through the myringotomy. The middle ear was packed with a single Gelfoam piece (Pfizer, NY, USA) soaked in ofloxacin to prevent inversion of the tympanic membrane edges. An additional layer of Gelfoam was placed over the lateral tympanic membrane. The procedure was well tolerated by the patient.
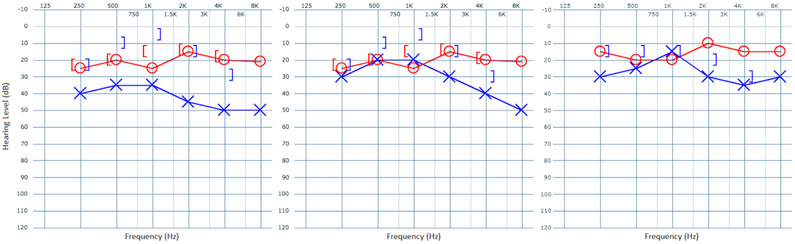
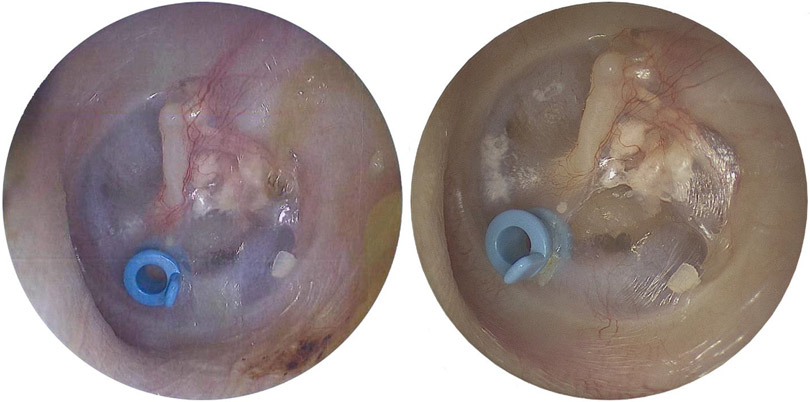
Pre- and post-procedure audiometric findings are shown in Figure 1. At 2-month follow up, the patient’s pure tone average (0.5, 1, 2, 3 kHz) and speech recognition threshold had improved from 37 dB to 26 dB and 35 dB to 20 dB, respectively. Furthermore, at 6-month follow up, slightly improvement was seen in high frequency (4 kHz and 8 kHz) hearing thresholds along with the outcome’s sustainability on pure tone average and speech recognition threshold at 26 dB and 20 dB, respectively (Figure 1, right panel). Repeat examinations at the same follow-up visits showed a healed tympanic membrane that was separated from the incudostapedial joint and bone cement visible in the posterosuperior quadrant between the incus and stapes (Figure 2).
Figure 1.
Two-month (middle panel) and 6-month (right panel) post-procedure audiograms of left ear show air conduction improvement and significant air-bone gap closure compared to the pre-procedure audiogram (left panel).
Figure 2.
Two-month (left panel) and 6-month (right panel) post-procedure microscopic views of the left ear show the healed tympanic membrane is separated from the incudostapedial joint. Bone cement is visible in the posterosuperior quadrant between the incus and stapes.
3. DISCUSSION
In this report we describe an in-office minimally-invasive ossicular chain reconstruction using hydroxyapatite bone cement between the incus and stapes. While this procedure is generally best performed in the operating room under anesthesia,3 this patient had a unique combination of circumstances which prevented surgery. She was pregnant so she could not undergo general anesthesia and was losing her insurance and was concerned she could not have the surgery performed after her pregnancy. This patient’s circumstances were unique; however, this case shows that as a proof of concept, this procedure can be performed in selected patients with an incudostapedial discontinuity. From a technical point, in order to allow better adhesion between the cement and the bones, the mucosa on the incus and stapes capitulum should be partly removed. Preservation of the fibrous band between the incus and stapes helps to hold the hydroxyapatite cement in place. We generally mix only a part of the powder and liquid portion of the cement to allow for changing the ratio such that the mixture is slightly more viscous than usual. This allows better manipulation past the myringotomy to prevent it from adhering to the tympanic membrane and from running down towards the stapes footplate. The myringotomy is held open with a 20-guage suction with “finger off the hole” while the cement is placed and to allow for drying the cement expeditiously. This also allows for rapid removal of cement that may run onto the stapes crura.
Additional cases and longer follow-ups are warranted for comparing this method’s efficacy to other in-office otological procedures. Though only one case, this patient’s 6-month audiogram outcomes are comparable to the reported 1-3 year improvements from operative ossicular reconstruction using various bone cements.3-5 Our plateaued level of audiometric improvement can be an indication of the outcome’s sustainability over a long period of time. Moreover, in a previous effort to similarly perform ossicular chain reconstruction with limited resources, Bedri et al. described 1-stage autologous ossiculoplasty in a developing country with promising results.6 The challenges involved in performing our proposed procedure in the office limit its utility to a specific subset of patients. First, as the local anesthetic is only applied to the external auditory canal and myringotomy site, the patient must be agreeable to tolerating some discomforts during manipulation of the middle ear. Accordingly, patients with concurrent mesotympanic cholesteatoma would likely not tolerate elevation of the retracted tympanic membrane. Second, the patient must still have a decent length of the long process of incus/head of stapes as patients with larger discontinuities may be better suited for prosthetic reconstruction. Other patients who might similarly benefit from this procedure are post-stapedectomy patients where the prosthesis has become loose due to erosion of the long process of incus.
KEYPOINTS.
A novel in-office and minimally-invasive ossicular chain reconstruction using hydroxyapatite bone cement between the incus and stapes is demonstrated.
Better adhesion between the cement and the bones was attained via partly removing the mucosa on the incus and stapes capitulum as well as preserving the fibrous band between the incus and stapes.
This case is a proof of concept, with audiometric improvements in both 2-month and 6-month follow-up periods, especially for selected patients with unique circumstances and an incudostapedial discontinuity.
Footnotes
CONFLICT OF INTERESTS
The authors have no conflict of interests to be declared.
Financial Disclosure: None
References
- 1.Schmidt VB, da Costa SS, Rosito LP, Canali I, Selaimen FA. Myringostapediopexy: is it a natural type III tympanoplasty? Otol Neurotol. 2013; 34(1): 79–82. [DOI] [PubMed] [Google Scholar]
- 2.Watson GJ, Narayan S. Bone cement: how effective is it at restoring hearing in isolated incudostapedial erosion? J Laryngol Otol. 2014; 128(8): 690–693. [DOI] [PubMed] [Google Scholar]
- 3.Babu S, Seidman MD. Ossicular reconstruction using bone cement. Otol Neurotol. 2004; 25(2): 98–101. [DOI] [PubMed] [Google Scholar]
- 4.Goebel JA, Jacob A. Use of Mimix hydroxyapatite bone cement for difficult ossicular reconstruction. Otolaryngol Head Neck Surg. 2005; 132(5): 727–734. [DOI] [PubMed] [Google Scholar]
- 5.Gungor V, Atay G, Bajin MD, Yarali M, Sarac S, Sennaroglu L. Comparison of various bone cement ossiculoplasty techniques and functional results. Acta Otolaryngol. 2016; 136(9): 883–887. [DOI] [PubMed] [Google Scholar]
- 6.Bedri EH, Redleaf M. Ossicular Chain Reconstruction in a Developing Country. Ann Otol Rhinol Laryngol. 2018; 127(5): 306–311. [DOI] [PubMed] [Google Scholar]