Abstract
Background Psychiatric disorders are more common among people undergoing cosmetic procedures than the general population and evaluating mental health can be cumbersome for plastic surgeons. We aim to summarize the available literature in this regard and propose an integrated approach to psychiatric assessment and management of mental health issues among this group.
Methods Electronic search of MEDLINE, Google Scholar, and PsycINFO databases was done to identify relevant peer-reviewed English language articles from inception till April 2020. Generated abstracts were screened for their eligibility. Included articles were grouped according to their thematic focus under the following headings; prevalence of psychiatric morbidity among clients posted for cosmetic surgery, assessment tools, and management of psychiatric morbidity in relation to undergoing cosmetic surgery.
Results A total of 120 articles were reviewed. The prevalence of psychiatric disorder in patients undergoing cosmetic surgery was 4 to 57% for body dysmorphic disorder (BDD); the corresponding figures for depression, anxiety, and personality disorder were 4.8 to 25.8, 10.8 to 22, and 0 to 53%, respectively. A range of tools have been used to assess these disorders and specific measures are also available to assess clinical outcomes following surgery. Screening for these disorders is essential to prevent unnecessary surgical procedures, as well as to ensure timely management of the psychiatric comorbidity.
Conclusion Psychiatric morbidity is a common concomitant in cosmetic surgery. A structured and integrated approach to evaluation and management of psychiatric morbidity will help to optimize postsurgical outcomes.
Keywords: psychiatry, cosmetic surgery, depression, India, plastic surgery
Introduction
Cosmetic surgical procedures refer to operations that revise or change the color, texture, appearance, structure, or position of normal bodily features to achieve a more desirable appearance. It is important to understand the interface between cosmetic surgery and psychiatry in the context of a growing demand for cosmetic surgery. The perception of physical appearance is known to affect self-esteem and mental health. Sometimes, cosmetic surgeons encounter persons seeking aesthetic surgery for some inappropriate and invalid indications due to psychological issues. 1
Studies have suggested that psychiatric disorders are more common among people undergoing cosmetic procedures than the general population. 2 Prevalence of psychiatric disorders in this group increases the risk for patient dissatisfaction and poorer outcomes such as patient distress, adjustment problems, social isolation, worsening of preexisting mental health conditions, and risk of self-harm. 3 6 Hence, identifying the presence of any psychiatric disorder through preoperative screening and conducting a psychological risk assessment (PRA) needs to be an integral aspect during the screening of patients seeking elective appearance-altering procedures.
Evaluating mental health can be cumbersome for plastic surgeons. Furthermore, there are no comprehensive reviews available about the epidemiology, evaluation, and treatment of psychiatric illnesses in persons seeking cosmetic surgery. The current review is intended to address this knowledge gap and to inform clinical practice in the area. The objective of this systematic review is to provide an overview of the prevalence of psychiatric morbidity, assessment, and management of these psychiatric conditions in patients undergoing cosmetic surgery.
Methodology
Search Strategy and Selection of Study
A literature search was performed through electronic databases of MEDLINE via PubMed, PsycINFO, and Google Scholar databases to identify relevant articles using random combination of the following medical subject headings or free text terms, “cosmetic surgery,” “cosmetic procedures,” “psychiatric disorders,” “BDD,” “depression,” “anxiety,” “personality disorders,” “eating disorders,” “co-morbidity” and “management.” An independent search was performed by the two authors in April 2020. The above search strategy was mainly used for PubMed and adapted for other databases as appropriate. Additionally, to ensure a comprehensive search, the reference section of relevant articles was manually screened. Any differences in selection of articles were resolved by mutual discussion till consensus.
We included articles published in English language peer-reviewed journals from inception till April 2020. In case of unavailability of full text articles, attempts were made to contact the authors to seek the same. Unpublished material and conference proceedings were not included in the review. No restriction was imposed on the type of article.
Data Extraction
Data extracted from studies included details such as author names, year, country of study origin, type of cosmetic procedure, psychiatric comorbidity studied and its prevalence, nature of comparator group (if any), and major findings.
Results
The initial search yielded 1,813 results, of which 120 articles were included for review as per the aforementioned selection criteria ( Fig. 1 ). Included studies were grouped into studies providing evidence for psychiatric morbidity, disorder wise among patients posted for cosmetic surgery for cosmetic surgery. Next, we outline the tools used to supplement psychiatric evaluation and discuss the management of psychiatric morbidity in relation to undergoing cosmetic surgery. Finally, we propose an integrated approach for evaluation and management of psychiatric comorbidity among clients undergoing cosmetic surgery.
Fig. 1.
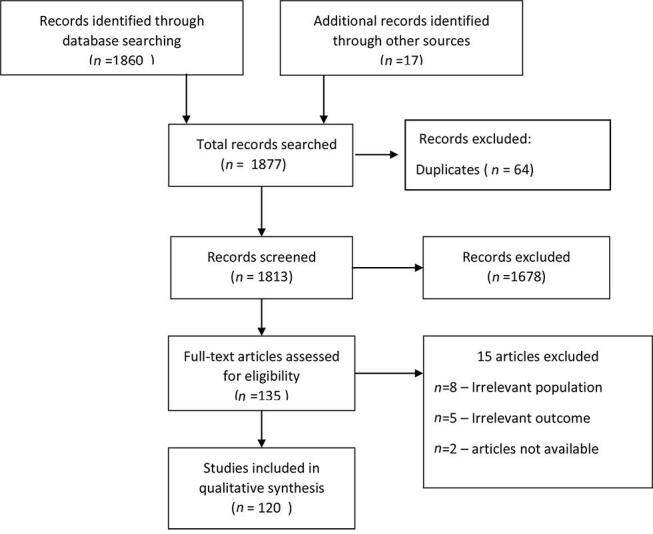
Selection of articles.
Psychiatric Morbidity in Clients Undergoing Cosmetic Surgery
A case control study found that approximately 26% of the cases seeking rhinoplasty had at least one psychiatric diagnosis; of whom 18% had somatoform disorder, 12% had body dysmorphic disorder (BDD), 6% narcissistic personality disorder, and 6% avoidant personality disorder. 7 A large retrospective chart review of patients attending elective plastic surgery revealed that 44% had a psychiatric illness, with 50% of them having major depressive disorder and 32% having generalized anxiety disorder. 8
Below, we summarize studies reporting the prevalence of specific psychiatric illnesses among clients undergoing cosmetic surgery.
Body Dysmorphic Disorder
The most frequently recorded psychiatric illness among patients undergoing cosmetic surgery is BDD. A meta-analysis of 33 studies noted that the prevalence of BDD was greater in patients seeking plastic surgery (15.04%) compared with those seeking dermatologist consultation (12.65%) and was more common in women in both the groups. 9 The prevalence of BDD ranged from 4 to 57% in reviewed studies when compared with 1% in the general population in the United States. 10 11
Few authors have also assessed body image dissatisfaction. Monpellier et al reported that dissatisfaction with body image in patients who underwent bariatric surgery was associated with greater depressive symptoms. 12 The details regarding studies assessing BDD among cosmetic surgery patients are given in Table 1 .
Table 1. Studies assessing body dysmorphic disorder among cosmetic surgery patients.
| Sl. No. | Study (year) and country | Procedure Sample size |
Tools of assessment | Prevalence of BDD |
|---|---|---|---|---|
| Abbreviations: BDDE, body dysmorphic disorder examination; BDDE-SR, BDDQ, body dysmorphic disorder questionnaire; body dysmorphic disorder examination self-report; BDD–YBOCS, body dysmorphic disorder Yale–brown obsessive–compulsive scale; BDI, beck depression inventory; BDSS, body dysmorphic symptoms scale; BSQ, body shape questionnaire; DCQ, dysmorphic concern questionnaire; HADS, hospital anxiety and depression; MBSRQ, -multidimensional body self-relations questionnaire-appearance scales; SCL-90, scale symptom check list-90; SNOT 23, sinonasal outcome test-23. | ||||
| 1 | De Brito et al (2016) 67 and Brazil | Abdominoplasty n = 90 |
1. BDDE (clinician rated) 2. BSQ |
57% |
| 2 | Ramos et al (2019) 68 and Brazil | Rhinoplasty n = 80 |
1. (BDD-YBOCS) 2. (BDSS)-clinician rated |
48%: BDD symptoms 54%: appearance related OC symptoms |
| 3 | Joseph et al (2017) 69 and USA | Facial plastic and oculoplastic surgery n = 597 |
1. BDDQ 2. FACE-Q |
9.7%: BDD, 4.0%: clinically suspected of BDD by surgeons |
| 4 | Joseph et al (2017) 70 and UK | Septo rhinoplasty n = 84 (34 cases and 50 controls) |
1. BDDQ 2. SNOT-23 |
32%: high risk for BDD |
| 5 | Brito et al (2016) 71 and Brazil |
Abdominoplasty (
n
= 90)
Rhinoplasty ( n = 151) Rhytidectomy ( n = 59) |
BDDE | BDD symptoms: Abdominoplasty: 57% Rhinoplasty: 52% Rhytidectomy group: 42% |
| 6 | Woolley et al (2015) 10 and USA | Oculofacial plastic surgery n = 728 |
DCQ (cut-off 9) | 6.9% |
| 7 | Bender et al (2014) 72 and Germany | Functional rhinosurgery n = 186 |
1. BDI 2. PISA body dysmorphic symptom scale |
33.9%: mild or strong indication for BDD 1.7%: depression |
| 8 | Dey et al (2015) 73 and USA | Facial plastic and reconstructive surgery n = 234 |
1. BDDQ 2. BDD-SCID |
Reconstructive surgery: 1.8% Cosmetic surgery: 13.1% |
| 9 | Metcalfe et al (2014) 74 and USA | Breast reconstruction n = 188 |
DCQ | 17% |
| 10 | Dogruk Kacar et al (2014) 75 and Turkey | Dermatology and cosmetic dermatology n = 318 |
Brief self-report BDD screening questionnaire | 6.3% Higher prevalence in cosmetic dermatology (8.6%) than general dermatology (4.2%) |
| 11 | Mr et al (2013) 76 and Iran | Aesthetic rhinoplasty n = 130 |
1. BDDQ 2. HADS |
31.5% |
| 12 | Vargel et al (2001) 77 and Turkey | Cosmetic surgery n = 20 cases and 20 controls |
1. SCL-90 2. BDI 3. MBSRQ |
20% |
| 13 | Sarwer et al (1998) 78 and USA | Cosmetic surgery n = 100 |
1. MBSRQ 2. BDDE-SR |
7% |
Depression, Anxiety Disorders, and Comorbidity
Majority of the studies were conducted on patients receiving aesthetic breast surgeries. 13 16 Of these, four studies reported on depression and anxiety. 13 17 19 The point prevalence of symptoms of depression and anxiety preoperatively ranged from 4.8 to 25.8, and 10.8 to 22%, respectively. 13 14 18 These prevalence rates are high when compared with the prevalence of depressive disorder and anxiety disorder among general population in the World Health Organization (WHO)—World Mental Health Survey, which ranged from 0.8 to 9.6 and 16%, respectively. 20 21 Eating disorder, quality of life, and sexual function were also assessed in some of the studies and the prevalence of eating disorders was found to be 8% preoperatively. 13 15 16 Quality of life and sexual function was found to improve postoperatively. Table 2 summarizes studies evaluating depression and anxiety in patients seeking cosmetic surgery.
Table 2. Depression and anxiety symptoms in clients seeking cosmetic surgery.
| Sl. no. | Study (year) and country | Cosmetic procedure Sample size | Scales | Prevalence |
|---|---|---|---|---|
| Abbreviations: DAS59, Derriford appearance scale; GHQ, general health questionnaire; MINI, mini international neuropsychiatric interview; NEO-FFI, neuroticism-extraversion-openness five-factor inventory; SQLP, Subjective Quality of Life Profile; STAI, state–trait anxiety inventory; TPQ, tri dimensional personality questionnaire (TPQ); YBOCS, Yale–brown obsessive–compulsive scale. | ||||
| 1 | Saariniemi et al (2012) 13 and Finland | Aesthetic augmentation mammaplasty n = 79 |
1. Eating disorder inventory 2. Raitasalo’s modification of the BDI 3. 15D general QOL questionnaire |
Anxiety: Baseline (22%) and 6 months postoperatively (14%) Depression: Baseline (11%) and 6 months postoperatively (8%) Disordered eating: Same rate at baseline and postoperatively (8%) |
| 2 | Paula et al (2018) 14 and Brazil | Cosmetic breast Surgery n = 185 |
BDI (≥15 points) | Depression: Public institutions: 25.8% Private institutions: 11.4% |
| 3 | Wei et al (2018) 18 and China | Aesthetic plastic surgery n = 315 |
HADS | Anxiety: 10.8% Depression: 4.8% Anxiety and depression: 1.9% |
| 4 | Clarke et al (2012) 19 and UK | Cosmetic surgery n = 500 |
1. DAS59 2. HADS 3. Structured clinical interview |
Severe anxiety: 18% Severe depression: 7% |
| 5 | Chahraoui et al (2006) 15 and France | Reduction mammaplasty n = 20 |
1. SQLP 2. STAI 3. GHQ |
Trait anxiety, state anxiety, and quality of life(pain, physical appearance, social life, and inner life) were significantly better at 4 months postoperatively |
| 6 | Beraldo et al (2016) 16 and Brazil | Reduction mammaplasty n = 30 cases and 30 controls |
1. Female sexual function index 2. BDI |
Depression and sexual function scores were significantly better than the control group at 6 months postoperatively |
| 7 | Pavan et al (2013) 17 and Italy | Overweight/obese patients referring to plastic surgery n = 35 cases and 30 controls |
1. BSQ 2. TPQ 3. NEO-FFI 4. MINI 5. YBOCS 6. BDI |
Cases: Ongoing major depression: 8.6% Lifetime major depression: 57.1% Controls: Ongoing major depression: 3.7% Lifetime major depression: 14.8% Patients had higher scores for TPQ Reward Dependence factor (RD4), BSQ and on all obsessive and compulsive aspects in YBOCS Also, higher scores in openness to experience was found in controls on NEO-FFI |
Personality and Associated Dimensions
The prevalence of personality disorders was found to be 53%, which is high when compared with the prevalence in general population in western countries, which is 12.1%. 22 24 Clusters B and C personality disorders are more prevalent in patients who undergo cosmetic surgery, and it also increases the risk for adverse outcomes such as patient dissatisfaction, litigations, and self-harm. 25 The details about personality and associated dimensions are given in Table 3 .
Table 3. Personality and associated dimensions.
| Study (year) and country | Cosmetic procedure Sample size |
Scales | Prevalence |
|---|---|---|---|
| Abbreviations: BDD–YBOCS, body dysmorphic disorder Yale–brown obsessive–compulsive scale; GSI, global severity index; HARS, Hamilton anxiety rating scales; NEO-FFI, neuroticism-extraversion- openness five-factor inventory; SCID, structured clinical interview for DSM disorders; SCL-90-R, symptom checklist-90-revised. | |||
| Golshani et al (2016) 79 and Iran | Cosmetic surgery n = 274 |
1. GSI (>63) 2. SCL-90-R 3. NEO-FFI |
Known psychiatric disorders: 9.9% Openness item had the lowest mean score in contrast to agreeableness and extroversion items in NEO-FFI |
| Del Aguila et al (2019) 22 and Mexico | Cosmetic body contouring surgery n = 87 |
1. Salamanca questionnaire for screening for personality disorders 2. HARS 3. Rosenberg self-esteem scale |
No personality disorder was found Average level of anxiety: 92% High level of self-esteem: 93.15% Average self-esteem: 6.9% |
| Loron et al (2018) 80 and Iran | Cosmetic botulinum toxin type-A (BoNTA) injection n = 200 |
Milton clinical multiaxial inventory 3rd edition | Personality traits Narcistic: 34.5% Histrionic: 27% OC: 4% Others Anxiety disorder: 46% Somatization: 25.5% Dysthymia: 11% |
| Zojaji et al (2014) 81 and Iran | Cosmetic rhinoplasty n = 30 cases and 30 controls |
Millon clinical multiaxial inventory 3rd edition | Cases: Dependent: 6.7% OCPD: 6.7% |
| Bellino et al (2006) 23 and Italy | Cosmetic surgery n = 66 |
1. SCID (DSM-IV), 2. BDD–YBOCS | Personality disorders: 53%. Out of which Narcissistic: 16.7% Borderline: 16.7% Avoidant: 12.1% Paranoid: 9.1% Schizotypal: 7.6% Obsessive–compulsive: 7.6% 16.6% had BDD |
Assessments
The aim of psychological assessment is to evaluate the client’s suitability to undergo the proposed cosmetic procedure, so as to reduce the incidence of adverse outcomes and provide psychological support and treatment to those who need it. It is important to assess each patient prior to cosmetic treatment to identify those with unrealistic expectations, extrinsic motivations, and psychological disorders or vulnerabilities. 26 This assessment also aims to evaluate and address any identified risk of suicide, self-harm or harm to others, and determine if such a risk may be a contraindication for the intended procedure. 27
Psychological Risk Assessment
A comprehensive assessment generally involves a thorough assessment of the client’s psychological and social functioning, developmental history, educational history, relationship history, current mental state, and mental health, including evaluation and identification of any possible mental health disorders. This involves not only obtaining information from the client but also from family members and significant others. 28
Assessment Tools
Both client self-report and clinician-administered scales are available for the evaluation of the client. 29 30 These can be broadly divided into the following:
Tools for broad assessment of psychiatric disorders
Tools for assessment of specific psychiatric disorders
Tools for assessment of clinical outcomes
Tools for a Broader Assessment of Psychiatric Disorders
-
MINI-Plus (Mini-International Neuropsychiatric Interview-Plus) 31
It is a widely used structured diagnostic interview instrument to diagnose psychiatric disorders according to International Classification of Diseases (ICD)-10 and Diagnostic and Statistical Manual of Mental Disorders (DSM)–5. It includes 23 disorders, including BDD.
-
SCID (Structured Clinical Interview for DSM Disorders) 32
The Structured Clinical Interview for DSM-5 Disorders (SCID-5) is a semistructured interview guide for making diagnoses according to DSM-5, administered by a trained mental health professional or clinician who is familiar with the diagnostic criteria of various mental health disorders. It has been published in various forms, including a version for clinicians (SCID-CV).
Tools for Assessment of Specific Psychiatric Disorders in Patients Undergoing Cosmetic Surgery
Tools to assess BDD and body image disturbances, as well as other psychiatric disorders, in patients posted for cosmetic surgery are summarized in Tables 4 5 , respectively.
Table 4. Tools to assess BDD and body image disturbances.
| Instrument | Psychiatric entity | Self/clinician administered | Remarks |
|---|---|---|---|
| Abbreviations: BDD, body dysmorphic disorder; MBSRQ-AS, multidimensional body self-relations questionnaire appearance scales. | |||
| SCID | BDD | Clinician | Gold standard for diagnosis of BDD 82 |
| Body dysmorphic disorder examination (BDDE) 83 | BDD | Clinician |
1. Time-consuming requires 30 minutes to complete
84
2. Use as a tool for BDD has waned in recent years, perhaps due to its particular relevance to eating disorders rather than to BDD 85,86 3. Not suitable to assess severe BDD 87 |
| BDDE self-report 88 | BDD | Self | 1. Addresses the limitations of the BDDE and therefore seems to be more appropriate for use in a cosmetic surgery setting 2. Possess good test–retest reliability and internal consistency 88 |
| Body dysmorphic disorder questionnaire (BDDQ) 89 | BDD | Self | 1. Takes 1–2 minutes to complete 2. Found to have a sensitivity of 100% and specificity of 89% in surgical setting 62,69 |
| BDD questionnaire-dermatology version (BDDQ-DV) 84 | BDD | Self | 1. Validated in the cosmetic surgery setting 2. Sensitivity of 100% and a specificity of 94.7%. |
| Dysmorphic concern questionnaire DCQ 90,91 | BDD | Self | 1. Validated in the cosmetic surgery setting 2. Sensitivity of 72% and a specificity of 90.7%. |
| Yale brown scale for BDD (BDD-YBOCS) 92 | BDD | Clinician | 1. Most widely used measure of BDD severity in research studies 2. Valid, reliable and has demonstrated good internal consistency |
| Body dysmorphic symptoms scale (BDSS) 93 | BDD | Self | Simple, rapid, and objective ten-item self-report measure assessing BDD |
| PISA body dysmorphic symptom scale 93 | BDD | Self | A slightly different version of the BDSS in which question 6 has been altered to detect unrealistic expectations from an intervention |
| Multidimensional body self-relations questionnaire (MBSRQ) 94,95 |
Body image disturbances | Self | 1. Good validity and reliability 2. The MBSRQ-AS includes the following subscales: appearance evaluation, appearance orientation, overweight preoccupation, self-classified weight, and the body areas satisfaction scale (BASS) 95 |
| Body shape questionnaire (BSQ) 96 | Body image disturbances | Self |
1. Easy to fill and can be completed in ~10 minutes
96
2. It is also validated in non-psychopathological population |
| Body image concern inventory (BICI) 97 | Body image disturbances | Self | Reliable, valid, and user-friendly tool for assessing dysmorphic concern 97 |
Table 5. Tools to assess other psychiatric disorders.
| Depression | References to studies that have used the tool in cosmetic surgery patients | |
|---|---|---|
| Hospital anxiety and depression scale 98 |
1. Reliable and valid instrument divided into an anxiety subscale (HADS-A) and a depression subscale (HADS-D)
99
2. Sensitivity and specificity for both HADS-A and HADS-D was ~0.80 100 |
Mr et al (2013)
76
Wei et al (2018) 18 Clarke et al (2012) 19 |
| Beck’s depression inventory (BDI) 101,102 | 1. Self-rated, 21 item scale 2. Second edition represents a revision that is more consistent with current diagnostic criteria for depression 103 |
Monpellier et al (2018)
12
Bender et al (2014) 72 Vargel et al (2001) 77 Paula et al (2018) 14 Pavan et al (2017) 104 Belli et al (2013) 7 Pavan et al (2013) 17 Beraldo et al (2016) 16 |
| Hamilton depression rating scales (HDRS) 105 | 1. Clinician administered 2. Many versions of the scale exist with the number of items usually varying between 17 and 24 and can be applied in ~15 minutes |
Bellino et al (2006) 23 |
| Anxiety | ||
| State–trait anxiety inventory (STAI) 106 | 1. It comprises of 2 subscales namely the State Anxiety Scale (S-Anxiety) which evaluates the current state of anxiety and the trait anxiety scale (T-anxiety) 2. 40 item, self-report scale and the internal consistency coefficients for the scale have ranged from 0.86 to 0.95 with test-retest reliability coefficients ranging from 0.65 to 0.75 106,107 |
Chahraoui et al (2006) 15 |
| Hamilton anxiety rating scales (HARS) 108 | 1. Clinician-based questionnaire consisting of 14 items 2. It has acceptable reliability and validity in adults and has shown good interrater reliability 108–110 |
Del Aguila et al (2019)
22
Bellino et al (2006) 23 |
| Beck anxiety inventory (BAI) 111 | 1. 21 item, self-reported Likert’s scale 2 .It has excellent internal consistency in clinical (0.91) and nonclinical sample (0.91) and a good test–retest reliability in clinical (0.66) and non-clinical (0.65) 112 |
Belli et al (2013) 7 |
| Personality disorders | ||
| Tri dimensional personality questionnaire (TPQ) 113 | 1. 100-item, self-administered instrument. 2. It measures three dimensions, namely, novelty seeking (NS), harm avoidance (HA), and reward dependence (RD) |
Pavan et al (2017)
104
Pavan et al (2013) 17 |
| Neuroticism-extraversion-openness five-factor inventory (NEO-FFI) 114 | 1. Shorter version of the NEO Personality Inventory-Revised 2. It consists of five basic personality factors, neuroticism, extraversion, openness to experience, agreeableness and conscientiousness |
Golshani et al (2016)
79
Pavan et al (2013) 17 |
| Eating disorders | ||
| Eating disorder inventory (EDI) 115 | 1. Self-report questionnaire widely used both to assess psychological features and symptoms of eating disorders. 2. It comprises of three subscales, i.e., drive for thinness, bulimia, and body dissatisfaction |
Saariniemi et al (2012) 13 |
| Binge eating scale 116 | 1. Self rated questionnaire comprising of 16 items: eight items that describe behavioral manifestations and eight items associated with feelings and cognitions 117 | Pavan et al (2017) 104 |
Tools for Assessment of Outcomes following Cosmetic Procedures
-
Derriford Appearance Scale 33 :
The Derriford Appearance Scale 59 (DAS59), comprises of 59 questions measuring the general, social, facial, sexual, and bodily self-consciousness of appearance, as well as negative self-concept and general feelings of hostility and irritability. 33 Among the 59 items, 57 of them measured psychological distress and dysfunction, and two items assessed physical distress and dysfunction. It has a 24-item shorter version called the DAS24, which measures distress in living with problems of appearance in reconstructive plastic surgery patients and in patients distressed by facial aging. It also has good psychometric properties.
-
PreFACE (PREoperative FAcial Cosmetic Surgery Evaluation) 30
This is a brief, objective, self-reported psychological screening questionnaire that can be easily administered by cosmetic surgeons and dentists. It is comprised of a subset of items from the following validated questionnaires: general health questionnaire–30, hospital anxiety and depression scale, Rosenberg’s self-esteem scale, dysmorphic concerns questionnaire, and multidimensional body-self relations questionnaire. These measures were included because they all evaluate many of the psychosocial characteristics of patients who were thought to be dissatisfied with the cosmetic procedure outcome. It uses a scoring system that ranges from 0 to 28, with higher scores indicating increased potential for postoperative dissatisfaction. Authors recommend preoperative psychological counselling for those scoring 11 or more.
Management
Management of Psychiatric Illnesses in Relation to Cosmetic Surgery
Screening of psychiatric illnesses in patients opting for cosmetic surgery is essential to prevent unnecessary surgical procedures, as well as timely management of the psychiatric comorbidity, if present. The management principles of affective disorders and psychosis in these patients are similar to those not undergoing cosmetic surgery. It is advised that these patients with comorbid depression and anxiety disorders must be evaluated carefully postsurgery for the worsening of symptoms and suicidal ideation. The management of BDD, which is the most common psychiatric comorbidity is discussed below. 34 35
Management of Body Dysmorphic Disorder
Cognitive behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs) have been proven to be efficacious. Exposure and response prevention, psychoeducation, motivation enhancement, attention retraining, perception retraining, mindfulness-based interventions, and mirror retraining are the various evidence-based components of CBT for BDD. Out of these, ERP is the mainstay of treatment. 36 CBT aims to identify and replace dysfunctionalbeliefs; it has also been found to decrease the severity of BDD symptoms, as well as associated symptoms of depression, delusions, and improve insight.
CBT can be tailored as per the specific symptom profile of the patient. Habit reversal techniques can be employed for patients with symptoms of skin picking or hair pulling. Long-term monitoring of patients with BDD is advised after cosmetic surgery as they have been found to have an increased risk of self-harm behavior, even a decade after the procedure. 37 38
SSRI are the treatment of choice in pharmacological management. Clomipramine (serotonin reuptake inhibitor) has also been tried. Higher doses and longer duration of the trial (up to 12 weeks), than used for depression, have been recommended for BDD. In the case of treatment-resistant BDD with comorbid depression, switching to another SSRI or clomipramine and augmentation with CBT or atypical antipsychotics are the treatment options available. 37
Management of Other Psychiatric Illnesses
The management of depression and anxiety disorders is similar to that of the general population, through SSRI and behavioral therapy. It is advisable to start benzodiazepines, such as lorazepam or alprazolam, for about 1 to 3 days before surgery for preoperative anxiety, and these can be stopped postoperatively. Guided imagery, music, and relaxation exercises are some of the common nonpharmacological means of management. Also, these patients must be closely followed-up for the worsening of symptoms and the emergence of suicidal ideation following surgery. Psychotic symptoms must be managed by administering antipsychotics. It is imperative to check for drug interactions when psychotropic medication is prescribed.
Clarification of Expectation/Motivation
Several authors have opined that the most common motivation for cosmetic surgery is improving the perception of body image leading to better psychological well-being. 39 40 The motivation for improving their body image by changing external appearance was found to be associated with better patient satisfaction postsurgery. In contrast, unrealistic expectations, poor preoperative understanding of risks and outcomes, subjectively reported defects in appearance without objective corroboration, history of repeated cosmetic surgeries, and history of stressful life events were noted to be associated with poor outcomes. 26
A vast body of literature exists on discussing the patient’s expectations for the procedure. They have been divided into psychological, physical, and interpersonal expectations. 41 Psychological expectations refer to improvement in mood, self-esteem, body image, confidence, or overall psychological well-being. Physical expectation means the correction of the perceived physical defects. Interpersonal expectation denotes the social connotation of being in tandem with the existing social norms and ideals and getting accepted. Out of these, psychological expectations that are based on improving body image are the most difficult to assess by the surgeons. Examples of unrealistic expectations include a disproportionate increase in self-esteem, better relationships, jobs and reversal/stopping of the aging process. 42 43
Postsurgical Outcomes
Aesthetic surgery has been associated with changes in self-esteem, body image, confidence, and quality of life across several cosmetic surgical procedures. 44 A systematic review noted that certain types of cosmetic surgeries had specific outcomes. 45 The majority of cosmetic surgeries had a positive effect on body image and self-esteem compared with other domains. 46
Breast augmentation surgery was consistently associated with better self-esteem, quality of life, satisfaction, lesser anxiety, or depression with varying effects on body image. In contrast, breast reduction surgery was noted to have an improvement in all the parameters with a better effect on health-related quality of life (HRQoL).
Facelift procedure was found to be associated with higher self-esteem and better quality of life but with a negative effect on emotional health with worsening of depression and anxiety symptoms. Rhinoplasty surprisingly, was noted to have no effect on body image, with varying improvements in self-esteem, quality of life, anxiety, and depression. 45
Several studies have noted increased rates of suicides in patients receiving breast augmentation surgery compared with the general population. The rates of suicide ranged from 0.24 to 0.68% across the studies. 47 Further, the elevated risk for suicide continued in the long-term following cosmetic procedure such as breast implants. 48 49
Patient-Reported Postsurgical Outcomes
There is increasing research on patient-reported outcomes (PRO), postsurgery. BREAST-Q, FACE-Q, are some of the popularly used PRO measures. 50 BREAST-Q consists of specific modules for surgeries such as breast reduction, breast augmentation, and breast cancer–related surgery. 51 FACE-Q comprises scales assessing appraisal of facial appearance, quality of life, adverse effects, and process of care. 52 Recently, an Indian study was published using FACE-Q that reported greater patient satisfaction, social functioning, and lesser psychosocial distress in patients who underwent rhinoplasty. 53
PROs act as a measure of the quality of life/HRQoL. Impairment in specific domains of HRQoL entails referral to the appropriate specialty. Patient satisfaction can be used to assess problems and improve communication. 54 They are not only useful in carrying out research but also in improving clinical care and generating data. One example is the BREAST-Q, which was used to assess the quality of care in the United Kingdom, and feedback and targets were given accordingly. 55 56
A synthesized approach toward assessment of patients for cosmetic surgery: “when, where, what, and how?”
The current consensus is that those with psychological issues found at screening can be referred to a mental health professional. However, few advocate the role of mental health professionals in the screening process. Involving a mental health professional at this step might not be feasible due to the wide mental health gap. Screening for psychological morbidity must be done prior to the surgery and periodically afterward to assess for any emergent mental health conditions.
Several screening tools are available, which can be used by the surgeon for screening, which facilitates referring the patients appropriately. 29 Psychiatric history exploring for mood, anxiety, psychotic symptoms, psychoactive substance use, personality disorders, self-harm attempts, along with mental status examination, must be inquired into. In addition, life stressors must also be assessed. The motivation and the expectation of the patient to seek cosmetic surgery must be clarified. 26 57
Substance use, eating disorders, past history of psychiatric illness, suicide attempts, family history of suicide, access to lethal suicide means, borderline personality disorder, and poor social support are recognized as risk factors for for suicide, and warrant referral to a psychiatrist for management. 26 Finally, it is emphasized that patients suspected to be suffering from psychological problems must be referred to a psychiatrist for timely management. It is advisable that psychotropic medication should be prescribed by a psychiatrist, but not by a cosmetic surgeon, given the need for expertise about psychopharmacology and judicious prescription of medication.
Discussion
Patients undergoing cosmetic surgery pose several management-related, as well as ethical and legal, challenges. Hence, there are several issues to be considered while reviewing research on psychiatric issues in these patients
First, the prevalence of psychiatric illness has been varying. This could be due to methodological differences in the characteristics of the study population, the methods of assessment including administration and type of instrument. It was found that prevalence was greater with interview-based methodology in comparison to standardized tools, which revealed lower rates. 22 23 Anxiety or depressive symptoms before surgery can be misconstrued as a syndromal disorder. Furthermore, the differences in the type of cosmetic surgery might also affect the rates of psychiatric illness. There have been several studies reporting higher rates of suicides among those receiving breast implants. 48 58 59 However, it is imperative to look at several confounding factors, such as comorbid depression, social factors, and family history, before confirming a causal association.
Second, the literature on the management of psychiatric illness in cosmetic surgery patients is limited. BDD has been the most commonly studied psychiatric illness in this group. Though CBT has been the treatment of choice, about half of the patients were found to be nonresponsive to CBT. Relatively longer duration of therapy, skills, and competency of the therapist, time of initiation of therapy is some of the factors which could influence the treatment outcome. 37 There is also scarce literature on course, outcome, and management of affective and psychotic illnesses in this subset of patients.
Third, though psychiatric illness is broadly considered as a contraindication to cosmetic surgery, there is an argument that those patients with “less-pathological” or “well-controlled” psychiatric illness might actually benefit from surgery by improvement in their quality of life. 26 46 60 It is advised that the risk-benefit analysis must be done before planning for surgery. Fourthly, “Postsurgery dissatisfaction syndrome (PSDS)” is an understudied entity which can be misdiagnosed as a mood disorder in the postoperative period. PSDS refers to dissatisfaction associated with anxiety, low mood, and somatic symptoms despite objective satisfactory surgical outcomes. 61 It has been associated with preoperative depression and anxiety disorder. Hence, it is necessary to differentiate between PSDS and mood disorder, postsurgery for appropriate management.
Finally, surgical treatment without prior psychological treatment, among those who require it, can result in adverse consequences for the surgeon. Dissatisfied patients may attempt retaliation against the surgeon, whom they believe has worsened their defect. This may take the form of lawsuits, physical assaults, or in some cases, murder. 62 64 One study reported that 2% of plastic surgeons had been physically threatened by a patient with BDD, and 10% have received threats of violence and legal action. 63 64 In another study, 40% of plastic surgeons reported that they had been threatened by a patient with BDD. 62 Since 1991, three plastic surgeons have been murdered by patients with BDD who were unhappy with their surgical results. 63
Occasionally patients with BDD undergo several surgeries, with potentially irreversible outcomes. Others, in a desperate attempt to fix their perceived deformity or to ensure that they receive surgery, subject themselves to “self-surgery,” the consequences of which can be life-threatening. 65 66
Hence, to carefully select patients who are appropriate for cosmetic procedures, validated preoperative screening tools must be used, and working relationships with mental health colleagues must be established. Once the preoperative assessment identifies a potential psychiatric diagnosis, a multidisciplinary team must be involved in the confirmation of diagnosis, consideration of evidence-based treatments, and appropriateness for the procedure in question. Most importantly, after determining the decisional capacity, informed consent must be taken from the patient giving adequate information about the steps of the procedure and associated complications, costs, as well as alternate options, of treatment in a language comprehensible by the patient to avoid any legal issues.
Conclusion
There is a need for prospective and longitudinal studies as majority of the existing studies on patients undergoing cosmetic surgery have been retrospective chart reviews. Validated and standardized tools are warranted for assessment. The effect of CBT or pharmacotherapy in patients with BDD seeking cosmetic surgery needs to be assessed. As the literature is largely confined to BDD, more studies are needed on management and long-term outcomes of other psychiatric illnesses.
Footnotes
Financial DisclosureDetails of Earlier PresentationAuthors’ ContributionsConflict of Interest There are no financial disclosures or sources of support for the present work.
None.
S.B. conceptualized the manuscript, did review of literature, and wrote the first draft of the manuscript. P.P.K. coconceptualized the manuscript, contributed to the review of literature, and cowriter of the first draft of the manuscript. V.M. coconceptualized the manuscript, supervised the work at all stages, and revised the manuscript for intellectual content. All authors read and approved the final version of the manuscript.
None declared.
References
- 1.Ritvo E C, Melnick I, Marcus G R, Glick I D. Psychiatric conditions in cosmetic surgery patients. Facial Plast Surg. 2006;22(03):194–197. doi: 10.1055/s-2006-950177. [DOI] [PubMed] [Google Scholar]
- 2.Hayashi K, Miyachi H, Nakakita N et al. Importance of a psychiatric approach in cosmetic surgery. Aesthet Surg J. 2007;27(04):396–401. doi: 10.1016/j.asj.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 3.Honigman R J, Phillips K A, Castle D J. A review of psychosocial outcomes for patients seeking cosmetic surgery. Plast Reconstr Surg. 2004;113(04):1229–1237. doi: 10.1097/01.PRS.0000110214.88868.CA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crerand C, Franklin M, Sarwer D.MOC-PS(SM) CME article: patient safety: body dysmorphic disorder and cosmetic surgery Plast Reconstr Surg 2008122(4S)1–15. [DOI] [PubMed] [Google Scholar]
- 5.Constantian M B, Lin C P. Why some patients are unhappy: part 2. Relationship of nasal shape and trauma history to surgical success. Plast Reconstr Surg. 2014;134(04):836–851. doi: 10.1097/PRS.0000000000000552. [DOI] [PubMed] [Google Scholar]
- 6.Paraskeva N, Clarke A, Rumsey N. The routine psychological screening of cosmetic surgery patients. Aesthetics 2014;1(12)
- 7.Belli H, Belli S, Ural C et al. Psychopathology and psychiatric co-morbidities in patients seeking rhinoplasty for cosmetic reasons. West Indian Med J. 2013;62(05):481–486. doi: 10.7727/wimj.2013.068. [DOI] [PubMed] [Google Scholar]
- 8.Jang B, Bhavsar D R. The prevalence of psychiatric disorders among elective plastic surgery patients. Eplasty. 2019;19:e6. [PMC free article] [PubMed] [Google Scholar]
- 9.Ribeiro R VE. Prevalence of body dysmorphic disorder in plastic surgery and dermatology patients: a systematic review with meta-analysis. Aesthetic Plast Surg. 2017;41(04):964–970. doi: 10.1007/s00266-017-0869-0. [DOI] [PubMed] [Google Scholar]
- 10.Woolley A J, Perry J D. Body dysmorphic disorder: prevalence and outcomes in an oculofacial plastic surgery practice. Am J Ophthalmol. 2015;159(06):1058–10640. doi: 10.1016/j.ajo.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 11.Anderson R C. Body dysmorphic disorder: recognition and treatment. Plast Surg Nurs. 2003;23(03):125–128, quiz 129. doi: 10.1097/00006527-200323030-00007. [DOI] [PubMed] [Google Scholar]
- 12.Monpellier V M, Antoniou E E, Mulkens S. Janssen IMC, van der Molen ABM, Jansen ATM. Body image dissatisfaction and depression in postbariatric patients is associated with less weight loss and a desire for body contouring surgery. Surg Obes Relat Dis. 2018;14(10):1507–1515. doi: 10.1016/j.soard.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Saariniemi K MM, Helle M H, Salmi A M, Peltoniemi H H, Charpentier P, Kuokkanen H OM. The effects of aesthetic breast augmentation on quality of life, psychological distress, and eating disorder symptoms: a prospective study. Aesthetic Plast Surg. 2012;36(05):1090–1095. doi: 10.1007/s00266-012-9917-y. [DOI] [PubMed] [Google Scholar]
- 14.de Paula P R, Fortes de Arruda F C, Prado M, Neves C G. Prevalence of Depressive symptoms in patients requesting cosmetic breast surgery in Midwestern Brazil. Plast Reconstr Surg Glob Open. 2018;6(10):e1899. doi: 10.1097/GOX.0000000000001899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chahraoui K, Danino A, Bénony H, Frachebois C, Clerc A S, Malka G. Anxiety and subjective quality of life preoperatively and 4 months after reduction mammaplasty. J Psychosom Res. 2006;61(06):801–806. doi: 10.1016/j.jpsychores.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 16.Beraldo F NM, Veiga D F, Veiga-Filho J et al. Sexual function and depression outcomes among breast hypertrophy patients undergoing reduction mammaplasty: a randomized controlled trial. Ann Plast Surg. 2016;76(04):379–382. doi: 10.1097/SAP.0000000000000380. [DOI] [PubMed] [Google Scholar]
- 17.Pavan C, Azzi M, Lancerotto L et al. Overweight/obese patients referring to plastic surgery: temperament and personality traits. Obes Surg. 2013;23(04):437–445. doi: 10.1007/s11695-012-0769-y. [DOI] [PubMed] [Google Scholar]
- 18.Wei L, Ge C, Xiao W, Zhang X, Xu J. Cross-sectional investigation and analysis of anxiety and depression in preoperative patients in the outpatient department of aesthetic plastic surgery in a general hospital in China. J Plast Reconstr Aesthet Surg. 2018;71(11):1539–1546. doi: 10.1016/j.bjps.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Clarke A, Hansen E L, White P, Butler P EM. Low priority? A cross sectional study of appearance anxiety in 500 consecutive referrals for cosmetic surgery. Psychol Health Med. 2012;17(04):440–446. doi: 10.1080/13548506.2011.626433. [DOI] [PubMed] [Google Scholar]
- 20.Demyttenaere K, Bruffaerts R, Posada-Villa J et al. WHO World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 21.Kessler R C, Aguilar-Gaxiola S, Alonso J et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18(01):23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Del Aguila E, Martínez J R, Pablos J L, Huánuco M, Encina V M, Rhenals A L. Personality traits, anxiety, and self-esteem in patients seeking cosmetic surgery in mexico city. Plast Reconstr Surg Glob Open. 2019;7(10):e2381. doi: 10.1097/GOX.0000000000002381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bellino S, Zizza M, Paradiso E, Rivarossa A, Fulcheri M, Bogetto F. Dysmorphic concern symptoms and personality disorders: a clinical investigation in patients seeking cosmetic surgery. Psychiatry Res. 2006;144(01):73–78. doi: 10.1016/j.psychres.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 24.Volkert J, Gablonski T-C, Rabung S. Prevalence of personality disorders in the general adult population in Western countries: systematic review and meta-analysis. Br J Psychiatry. 2018;213(06):709–715. doi: 10.1192/bjp.2018.202. [DOI] [PubMed] [Google Scholar]
- 25.Napoleon A. The presentation of personalities in plastic surgery. Ann Plast Surg. 1993;31(03):193–208. doi: 10.1097/00000637-199309000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Ericksen W L, Billick S B. Psychiatric issues in cosmetic plastic surgery. Psychiatr Q. 2012;83(03):343–352. doi: 10.1007/s11126-012-9204-8. [DOI] [PubMed] [Google Scholar]
- 27.Cosmetic procedure psychological evaluation practice guide. Available at: https://psychology.org.au/cosmetic-procedure-practice-guide. Accessed May 31, 2020
- 28.Sarwer D B, Ritter S, D’Almeida T, Weinrieb R.Preoperative mental health evaluations. In: Hunter CM, Hunter CL, Kessler R, eds. Handbook of Clinical Psychology in Medical Settings: Evidence-Based Assessment and Intervention. New York, NY: Springer2014719–738. [Google Scholar]
- 29.Wildgoose P, Scott A, Pusic A L, Cano S, Klassen A F. Psychological screening measures for cosmetic plastic surgery patients: a systematic review. Aesthet Surg J. 2013;33(01):152–159. doi: 10.1177/1090820X12469532. [DOI] [PubMed] [Google Scholar]
- 30.Honigman R J, Jackson A C, Dowling N A. The PreFACE: a preoperative psychosocial screen for elective facial cosmetic surgery and cosmetic dentistry patients. Ann Plast Surg. 2011;66(01):16–23. doi: 10.1097/SAP.0b013e3181d50e54. [DOI] [PubMed] [Google Scholar]
- 31.Sheehan D V, Lecrubier Y, Sheehan K H et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 20:22–33, quiz 34–57. [PubMed] [Google Scholar]
- 32.First M B.Structured Clinical Interview for the DSM (SCID). In: The Encyclopedia of Clinical Psychology. American Cancer Society20151–6 [Google Scholar]
- 33.Harris D L, Carr A T. The Derriford Appearance Scale (DAS59): a new psychometric scale for the evaluation of patients with disfigurements and aesthetic problems of appearance. Br J Plast Surg. 2001;54(03):216–222. doi: 10.1054/bjps.2001.3559. [DOI] [PubMed] [Google Scholar]
- 34.Singh A R, Veale D.Understanding and treating body dysmorphic disorder Indian J Psychiatry 201961(suppl 1)S131–S135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phillips K A. Body dysmorphic disorder: recognizing and treating imagined ugliness. World Psychiatry. 2004;3(01):12–17. [PMC free article] [PubMed] [Google Scholar]
- 36.Krebs G, Fernández de la Cruz L, Mataix-Cols D. Recent advances in understanding and managing body dysmorphic disorder. Evid Based Ment Health. 2017;20(03):71–75. doi: 10.1136/eb-2017-102702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hong K, Nezgovorova V, Hollander E. New perspectives in the treatment of body dysmorphic disorder. F1000 Res. 2018;7:361. doi: 10.12688/f1000research.13700.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sarwer D B, Brown G K, Evans D L. Cosmetic breast augmentation and suicide. Am J Psychiatry. 2007;164(07):1006–1013. doi: 10.1176/ajp.2007.164.7.1006. [DOI] [PubMed] [Google Scholar]
- 39.Haas C F, Champion A, Secor D. Motivating factors for seeking cosmetic surgery: a synthesis of the literature. Plast Surg Nurs. 2008;28(04):177–182. doi: 10.1097/PSN.0b013e31818ea832. [DOI] [PubMed] [Google Scholar]
- 40.Milothridis P, Pavlidis L, Haidich A-B, Panagopoulou E. A systematic review of the factors predicting the interest in cosmetic plastic surgery. Indian J Plast Surg. 2016;49(03):397–402. doi: 10.4103/0970-0358.197224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pruzinsky T. Psychological factors in cosmetic plastic surgery: recent developments in patient care. Plast Surg Nurs. 1993;13(02):64–69, 119. doi: 10.1097/00006527-199301320-00003. [DOI] [PubMed] [Google Scholar]
- 42.Ritvo E, Riche C L, Stillman M A.Patients with unrealistic expectations. In: Carniol PJ, Monheit GD, eds. Aesthetic Rejuvenation Challenges and Solutions: A World Perspective (Series in Cosmetic and Laser Therapy). New York, NY: Informa UK Ltd.; 2009:6–10 [Google Scholar]
- 43.Carniol P J, Monheit GD.eds. Aesthetic Rejuvenation Challenges and Solutions: A World Perspective (Series in Cosmetic and Laser Therapy). New York, NY: Informa UK Ltd.2009242 [Google Scholar]
- 44.Figueroa C. Self-esteem and cosmetic surgery: is there a relationship between the two? Plast Surg Nurs. 2003;23(01):21–24. doi: 10.1097/00006527-200323010-00005. [DOI] [PubMed] [Google Scholar]
- 45.Brunton G, Paraskeva N, Caird J et al. Psychosocial predictors, assessment, and outcomes of cosmetic procedures: a systematic rapid evidence assessment. Aesthetic Plast Surg. 2014;38(05):1030–1040. doi: 10.1007/s00266-014-0369-4. [DOI] [PubMed] [Google Scholar]
- 46.Cook S A, Rosser R, Salmon P. Is cosmetic surgery an effective psychotherapeutic intervention? A systematic review of the evidence. J Plast Reconstr Aesthet Surg. 2006;59(11):1133–1151. doi: 10.1016/j.bjps.2006.03.047. [DOI] [PubMed] [Google Scholar]
- 47.Zuckerman D M, Kennedy C E, Terplan M. Breast implants, self-esteem, quality of life, and the risk of suicide. Womens Health Issues. 2016;26(04):361–365. doi: 10.1016/j.whi.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 48.Jacobsen P H, Hölmich L R, McLaughlin J K et al. Mortality and suicide among Danish women with cosmetic breast implants. Arch Intern Med. 2004;164(22):2450–2455. doi: 10.1001/archinte.164.22.2450. [DOI] [PubMed] [Google Scholar]
- 49.Villeneuve P J, Holowaty E J, Brisson J et al. Mortality among Canadian women with cosmetic breast implants. Am J Epidemiol. 2006;164(04):334–341. doi: 10.1093/aje/kwj214. [DOI] [PubMed] [Google Scholar]
- 50.Klassen A F, Cano S J, Scott A, Tsangaris E, Pusic A L. Assessing outcomes in body contouring. Clin Plast Surg. 2014;41(04):645–654. doi: 10.1016/j.cps.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 51.Cohen W A, Mundy L R, Ballard T NS et al. The BREAST-Q in surgical research: A review of the literature 2009-2015. J Plast Reconstr Aesthet Surg. 2016;69(02):149–162. doi: 10.1016/j.bjps.2015.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Klassen A F, Cano S J, Scott A, Snell L, Pusic A L. Measuring patient-reported outcomes in facial aesthetic patients: development of the FACE-Q. Facial Plast Surg. 2010;26(04):303–309. doi: 10.1055/s-0030-1262313. [DOI] [PubMed] [Google Scholar]
- 53.Soni K, Patro S K, Aneja J, Kaushal D, Goyal A, Shakrawal N. Post-rhinoplasty outcomes in an Indian population assessed using the FACE-Q appraisal scales: a prospective observational study. J Laryngol Otol. 2020;134(03):247–251. doi: 10.1017/S0022215120000638. [DOI] [PubMed] [Google Scholar]
- 54.Voineskos S H, Nelson J A, Klassen A F, Pusic A L. Measuring Patient-Reported Outcomes: Key Metrics in Reconstructive Surgery. Annu Rev Med. 2018;69:467–479. doi: 10.1146/annurev-med-060116-022831. [DOI] [PubMed] [Google Scholar]
- 55.Jeevan R, Cromwell D, Browne J. Annual national mastectomy and breast reconstruction audit 2011. Leeds (United Kingdom): The NHS Information Centre for Health and Social Care; 2011
- 56.Black N. Patient reported outcome measures could help transform healthcare. BMJ. 2013;346:f167. doi: 10.1136/bmj.f167. [DOI] [PubMed] [Google Scholar]
- 57.Sarwer D B, Zanville H A, LaRossa D et al. Mental health histories and psychiatric medication usage among persons who sought cosmetic Surgery. Plast Reconstr Surg. 2004;114(07):1927–1933, discussion 1934–1935. doi: 10.1097/01.prs.0000142999.86432.1f. [DOI] [PubMed] [Google Scholar]
- 58.Brinton L A, Lubin J H, Murray M C, Colton T, Hoover R N. Mortality rates among augmentation mammoplasty patients: an update. Epidemiology. 2006;17(02):162–169. doi: 10.1097/01.ede.0000197056.84629.19. [DOI] [PubMed] [Google Scholar]
- 59.Pukkala E, Kulmala I, Hovi S-L et al. Causes of death among Finnish women with cosmetic breast implants, 1971-2001. Ann Plast Surg. 2003;51(04):339–342, discussion 343–344. doi: 10.1097/01.sap.0000080407.97677.A5. [DOI] [PubMed] [Google Scholar]
- 60.Biraben-Gotzamanis L, Aouizerate B, Martin-Guehl C, Grabot D, Tignol J.[Body dysmorphic disorder and cosmetic surgery: assessment of 24 subjects with a minimal defect in appearance 5 years after their request for cosmetic surgery] Presse Med 200938(7-8)1062–1067. [DOI] [PubMed] [Google Scholar]
- 61.Gruber R P, Roberts C, Schooler W, Pitman R K. Preventing postsurgical dissatisfaction syndrome after rhinoplasty with propranolol: a pilot study. Plast Reconstr Surg. 2009;123(03):1072–1078. doi: 10.1097/PRS.0b013e318199f63f. [DOI] [PubMed] [Google Scholar]
- 62.Ziglinas P, Menger D J, Georgalas C. The body dysmorphic disorder patient: to perform rhinoplasty or not? Eur Arch Otorhinolaryngol. 2014;271(09):2355–2358. doi: 10.1007/s00405-013-2792-6. [DOI] [PubMed] [Google Scholar]
- 63.Sweis I E, Spitz J, Barry D R, Jr, Cohen M. A review of body dysmorphic disorder in aesthetic surgery patients and the legal implications. Aesthetic Plast Surg. 2017;41(04):949–954. doi: 10.1007/s00266-017-0819-x. [DOI] [PubMed] [Google Scholar]
- 64.Wang Q, Cao C, Guo R et al. Avoiding psychological pitfalls in aesthetic medical procedures. Aesthetic Plast Surg. 2016;40(06):954–961. doi: 10.1007/s00266-016-0715-9. [DOI] [PubMed] [Google Scholar]
- 65.Phillips K A, Menard W, Fay C, Weisberg R. Demographic characteristics, phenomenology, comorbidity, and family history in 200 individuals with body dysmorphic disorder. Psychosomatics. 2005;46(04):317–325. doi: 10.1176/appi.psy.46.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Veale D. Outcome of cosmetic surgery and DIY’ surgery in patients with body dysmorphic disorder. Psychiatr Bull. 2000;24:218–220. [Google Scholar]
- 67.de Brito M JA, Nahas F X, Cordás T A, Tavares H, Ferreira L M. Body dysmorphic disorder in patients seeking abdominoplasty, rhinoplasty, and rhytidectomy. Plast Reconstr Surg. 2016;137(02):462–471. doi: 10.1097/01.prs.0000475753.33215.8f. [DOI] [PubMed] [Google Scholar]
- 68.Ramos T D, de Brito M JA, Suzuki V Y, Sabino Neto M, Ferreira L M. High prevalence of body dysmorphic disorder and moderate to severe appearance-related obsessive-compulsive symptoms among rhinoplasty candidates. Aesthetic Plast Surg. 2019;43(04):1000–1005. doi: 10.1007/s00266-018-1300-1. [DOI] [PubMed] [Google Scholar]
- 69.Joseph A W, Ishii L, Joseph S S et al. Prevalence of body dysmorphic disorder and surgeon diagnostic accuracy in facial plastic and oculoplastic surgery clinics. JAMA Facial Plast Surg. 2017;19(04):269–274. doi: 10.1001/jamafacial.2016.1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Joseph J, Randhawa P, Hannan S A et al. Body dysmorphic disorder in patients undergoing septorhinoplasty surgery: should we be performing routine screening? Clin Otolaryngol. 2017;42(03):508–513. doi: 10.1111/coa.12752. [DOI] [PubMed] [Google Scholar]
- 71.Brito M J, Nahas F X, Cordás T A et al. Prevalence of body dysmorphic disorder symptoms and body weight concerns in patients seeking abdominoplasty. Aesthet Surg J. 2016;36(03):324–332. doi: 10.1093/asj/sjv213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bender M, Rustige L, Lindemann J. [Prevalence of depression and body dysmorphic disorder in patients before functional rhinosurgery] Laryngorhinootologie. 2014;93(11):764–767. doi: 10.1055/s-0034-1390476. [DOI] [PubMed] [Google Scholar]
- 73.Dey J K, Ishii M, Phillis M, Byrne P J, Boahene K DO, Ishii L E. Body dysmorphic disorder in a facial plastic and reconstructive surgery clinic: measuring prevalence, assessing comorbidities, and validating a feasible screening instrument. JAMA Facial Plast Surg. 2015;17(02):137–143. doi: 10.1001/jamafacial.2014.1492. [DOI] [PubMed] [Google Scholar]
- 74.Metcalfe D B, Duggal C S, Gabriel A, Nahabedian M Y, Carlson G W, Losken A. Prevalence of body dysmorphic disorder among patients seeking breast reconstruction. Aesthet Surg J. 2014;34(05):733–737. doi: 10.1177/1090820X14531775. [DOI] [PubMed] [Google Scholar]
- 75.Dogruk Kacar S, Ozuguz P, Bagcioglu E et al. The frequency of body dysmorphic disorder in dermatology and cosmetic dermatology clinics: a study from Turkey. Clin Exp Dermatol. 2014;39(04):433–438. doi: 10.1111/ced.12304. [DOI] [PubMed] [Google Scholar]
- 76.A M . Mr F, Tabrizi A G, Bafghi A F, Sa N. Body dysmorphic disorder in aesthetic rhinoplasty candidates. Pak J Med Sci. 2013;29(01):197–200. doi: 10.12669/pjms.291.2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vargel S, Uluşahin A. Psychopathology and body image in cosmetic surgery patients. Aesthetic Plast Surg. 2001;25(06):474–478. doi: 10.1007/s00266-001-0009-7. [DOI] [PubMed] [Google Scholar]
- 78.Sarwer D B, Wadden T A, Pertschuk M J, Whitaker L A. Body image dissatisfaction and body dysmorphic disorder in 100 cosmetic surgery patients. Plast Reconstr Surg. 1998;101(06):1644–1649. doi: 10.1097/00006534-199805000-00035. [DOI] [PubMed] [Google Scholar]
- 79.Golshani S, Mani A, Toubaei S, Farnia V, Sepehry A A, Alikhani M. Personality and psychological aspects of cosmetic surgery. Aesthetic Plast Surg. 2016;40(01):38–47. doi: 10.1007/s00266-015-0592-7. [DOI] [PubMed] [Google Scholar]
- 80.Loron A M, Ghaffari A, Poursafargholi N. Personality disorders among individuals seeking cosmetic botulinum toxin type A (BoNTA) injection, a cross-sectional study. Eurasian J Med. 2018;50(03):164–167. doi: 10.5152/eurasianjmed.2018.17373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zojaji R, Arshadi H R, Keshavarz M. Mazloum Farsibaf M, Golzari F, Khorashadizadeh M. Personality characteristics of patients seeking cosmetic rhinoplasty. Aesthetic Plast Surg. 2014;38(06):1090–1093. doi: 10.1007/s00266-014-0402-7. [DOI] [PubMed] [Google Scholar]
- 82.Higgins S, Wysong A. Cosmetic surgery and body dysmorphic disorder - an update. Int J Womens Dermatol. 2017;4(01):43–48. doi: 10.1016/j.ijwd.2017.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rosen J C, Reiter J. Development of the body dysmorphic disorder examination. Behav Res Ther. 1996;34(09):755–766. doi: 10.1016/0005-7967(96)00024-1. [DOI] [PubMed] [Google Scholar]
- 84.Dufresne R G, Phillips K A, Vittorio C C, Wilkel C S. A screening questionnaire for body dysmorphic disorder in a cosmetic dermatologic surgery practice. Dermatol Surg. 2001;27(05):457–462. doi: 10.1046/j.1524-4725.2001.00190.x. [DOI] [PubMed] [Google Scholar]
- 85.Body dysmorphic disorder. a treatment manual. Available at: https://epdf.pub/body-dysmorphic-disorder-a-treatment-manual.html. Accessed November 4, 2020
- 86.Wilhelm S, Greenberg J L, Rosenfield E, Kasarskis I, Blashill A J. The body dysmorphic disorder symptom scale: development and preliminary validation of a self-report scale of symptom specific dysfunction. Body Image. 2016;17:82–87. doi: 10.1016/j.bodyim.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Phillips K A, McElroy S L, Dwight M M, Eisen J L, Rasmussen S A. Delusionality and response to open-label fluvoxamine in body dysmorphic disorder. J Clin Psychiatry. 2001;62(02):87–91. doi: 10.4088/jcp.v62n0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rosen J C, Reiter J.Body dysmorphic disorder examination: Self-report. Burlington, VT: University at Burlington1995 [Google Scholar]
- 89.Phillips K A.The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. Revised and Expanded Edition. Oxford, England: Oxford University Press2005432 [Google Scholar]
- 90.Oosthuizen P, Lambert T, Castle D J. Dysmorphic concern: prevalence and associations with clinical variables. Aust N Z J Psychiatry. 1998;32(01):129–132. doi: 10.3109/00048679809062719. [DOI] [PubMed] [Google Scholar]
- 91.Jorgensen L, Castle D, Roberts C, Groth-Marnat G. A clinical validation of the Dysmorphic Concern Questionnaire. Aust N Z J Psychiatry. 2001;35(01):124–128. doi: 10.1046/j.1440-1614.2001.00860.x. [DOI] [PubMed] [Google Scholar]
- 92.Phillips K A, Hollander E, Rasmussen S A, Aronowitz B R, DeCaria C, Goodman W K. A severity rating scale for body dysmorphic disorder: development, reliability, and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychopharmacol Bull. 1997;33(01):17–22. [PubMed] [Google Scholar]
- 93.Perugi G, Akiskal H S, Giannotti D. Frare F, Di Vaio S, Cassano GB. Gender-related differences in body dysmorphic disorder (dysmorphophobia) J Nerv Ment Dis. 1997;185(09):578–582. doi: 10.1097/00005053-199709000-00007. [DOI] [PubMed] [Google Scholar]
- 94.Brown T A, Cash T F, Mikulka P J.Attitudinal body-image assessment: factor analysis of the Body-Self Relations Questionnaire J Pers Assess 199055(1-2)135–144. [DOI] [PubMed] [Google Scholar]
- 95.Cash T F.The Multidimensional Body-Self Relations Questionnaire users’ manual. Norfolk, VA: Old Dominion University; 1994b [Google Scholar]
- 96.Pj C, Mj T ZC, Cg F. The development and validation of the body shape questionnaire. Int J Eat Disord. 1987;6:485–494. [Google Scholar]
- 97.Littleton H L, Axsom D, Pury C LS. Development of the body image concern inventory. Behav Res Ther. 2005;43(02):229–241. doi: 10.1016/j.brat.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 98.Zigmond A S, Snaith R P. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(06):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 99.Herrmann C. International experiences with the hospital anxiety and depression scale–a review of validation data and clinical results. J Psychosom Res. 1997;42(01):17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 100.Bjelland I, Dahl A A, Haug T T, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52(02):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 101.Beck A T, Ward C H, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 102.Beck A T, Steer R A, Garbin M G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8(01):77–100. [Google Scholar]
- 103.Beck A T, Steer R A, Brown G K.Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation1996 [Google Scholar]
- 104.Pavan C, Marini M, De Antoni E et al. Psychological and psychiatric traits in post-bariatric patients asking for body-contouring surgery. Aesthetic Plast Surg. 2017;41(01):90–97. doi: 10.1007/s00266-016-0752-4. [DOI] [PubMed] [Google Scholar]
- 105.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Spielberger C D, Gorsuch R L, Lushene R, Vagg P R, Jacobs G A.Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press1983 [Google Scholar]
- 107.Spielberger C D.State-Trait Anxiety Inventory: Bibliography. 2nd ed. Palo Alto, CA: Consulting Psychologists Press1989 [Google Scholar]
- 108.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(01):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 109.Gjerris A, Bech P, Bøjholm S et al. The Hamilton anxiety scale. Evaluation of homogeneity and inter-observer reliability in patients with depressive disorders. J Affect Disord. 1983;5(02):163–170. doi: 10.1016/0165-0327(83)90009-5. [DOI] [PubMed] [Google Scholar]
- 110.Bech P, Grosby H, Husum B, Rafaelsen L.Generalized anxiety or depression measured by the Hamilton anxiety scale and the melancholia scale in patients before and after cardiac surgery Psychopathology 198417(5-6)253–263. [DOI] [PubMed] [Google Scholar]
- 111.Beck A T, Epstein N, Brown G, Steer R A. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(06):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 112.Bardhoshi G, Duncan K, Erford B T. Psychometric Meta-Analysis of the English Version of the Beck Anxiety Inventory. J Couns Dev. 2016;94(03):356–373. [Google Scholar]
- 113.Cloninger C R.The Tridimensional Personality Questionnaire, Version IV. St Louis, MO: Washington University School of Medicine, 1987b [Google Scholar]
- 114.Costa P T, McCrae R R.Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) Professional Manual. Lutz, FL: Psychological Assessment Resources, Inc 1992b [Google Scholar]
- 115.Garner D M, Olmstead M P, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eat Disord. 1983;2(02):15–34. [Google Scholar]
- 116.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(01):47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 117.Marcus M D, Wing R R, Hopkins J. Obese binge eaters: affect, cognitions, and response to behavioural weight control. J Consult Clin Psychol. 1988;56(03):433–439. doi: 10.1037//0022-006x.56.3.433. [DOI] [PubMed] [Google Scholar]


