Lay summary:
Cancer has substantial economic impacts for patients, their families/caregivers, employers, and the healthcare system. However, there is only limited understanding of how economic issues can affect access to cancer care services and receipt of high-quality of cancer care. Health economics research in cancer is particularly important due to the large and increasing number of cancer patients and survivors, but many factors may create barriers to performing cancer health economics research. This Commentary helps to identify important topics and questions in cancer health economics research and assist in the development of this critical field.
Keywords: neoplasms, economics, cost and cost analysis, policy making
Precis:
Although economic constructs have substantial impact on the delivery of cancer-related services, and cancer and its treatment have substantial economic consequences, there is only limited understanding of how economics affect healthcare delivery, health equity, quality of cancer care, and patient outcomes. This Commentary presents a framework to help identify important topics and research questions in cancer health economics research and assist in the development of this critical field.
Cancer, in addition to impacts on morbidity, mortality, and quality of life, has substantial economic consequences for patients, their families/caregivers, employers, and the healthcare system. Medical care costs for cancer in the U.S. were estimated as $183 billion in 2015 and projected to increase to more than $240 billion in 2030.1 Almost two-thirds of Medicare beneficiaries with cancer were hospitalized at least once within 12 months following diagnosis; their annual Medicare hospital payments totaled more than $5.7 billion.2 Cancer survivors experience substantially greater out-of-pocket expenses than do those without a cancer history,3 Although multiple published studies project costs of cancer treatment,1, 4, 5 there is only limited understanding of other types of cancer-related costs, policy impacts and societal factors on these costs, and economics affecting healthcare delivery, health equity, and quality of cancer care.
Health economics research has been defined as “the application of economic theory, models and empirical techniques to the analysis of decision making by individuals, health care providers and governments with respect to health and health care”.6 Health economics research is particularly relevant for cancer due to the large and increasing number of cancer survivors;7, 8 the widely varying use of and access to multimodal treatments and supportive therapies; the high levels of spending on cancer-related care by patients, employers, public programs, and other stakeholders; and the substantial cancer cost burdens among underserved populations. Despite progress made by cancer health economics researchers, additional information is needed. A critical need exists for research focused on factors influencing patient, provider, health care system, and societal costs related to cancer. More work is needed on the impacts of these costs on quality of care, treatment decisions, outcomes, and health equity. There are opportunities to improve medical care and patient wellbeing by examining economic research topics ranging from cancer prevention and early detection to diagnosis, treatment, survivorship, and end-of-life care.
Health economics research relevant to cancer is currently funded in the U.S. by multiple sources including federal agencies (e.g., the National Cancer Institute [NCI], Centers for Disease Control and Prevention [CDC], Agency for Healthcare Research & Quality [AHRQ]) and private organizations such as the American Cancer Society (ACS). NIH has designated health economics research designed to understand how innovations can most effectively improve health and well-being as a priority area.9 While cancer health economics research already substantially contributes to our understanding of healthcare delivery and policy, this research area is still underdeveloped. A portfolio review of grants funded by NCI over the past five years found that fewer than 1% of grants included economic analysis (including studies of financial hardship, economic policy analysis, budget impact analysis, and willing-to-pay as well as studies of costs and cost-effectiveness).10 Multiple factors may create barriers to cancer health economics research including limited data resources/linkages, training, methods, opportunities for research publication/dissemination, and funding opportunities. Addressing these barriers can advance and strengthen this field.
The Division of Cancer Control and Population Sciences (DCCPS) of the NCI is interested in learning more about unmet needs for conducting health economics research focused on cancer and potential activities to support and enhance this field. As part of the Interagency Consortium to Promote Health Economics Research on Cancer (HEROiC),11 DCCPS will host a virtual conference on the Future of Cancer Health Economics Research on Dec. 2 and 3, 2020 (https://cancercontrol.cancer.gov/events/future-of-heroic). This virtual conference will be free, open to the public, and will be livestreamed as well as recorded. In collaboration with researchers from CDC, ACS, and academia, this conference will include presentations and panels on challenges in conducting economics research across the cancer care continuum and broad discussions of key issues to further advance this growing field.
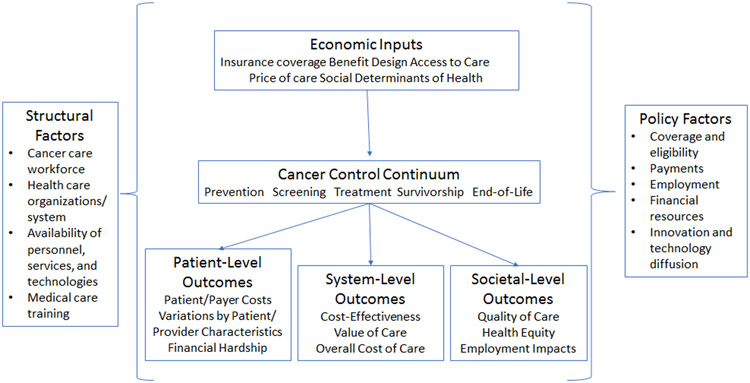
An important consideration for this conference is the scope of cancer health economics research to be discussed. That is, while we do not intend to impose a set definition of cancer health economics research, it is important to identify the topics and research questions on which the conference will focus. To address this, a group of content experts from multiple organizations (the authors of this Commentary) developed an initial cancer health economics research framework. For purposes of this conference, we are particularly interested in two areas of cancer health economics:
- Research on economic outcomes associated with cancer prevention, detection/screening, treatment, and survivorship services, including:
- Costs/expenditures and costs/expenditures relative to benefits/outcomes (e.g., cost-effectiveness);
- Financial hardship/toxicity and similar patient-focused economic impacts; and
- Value of care, including elements of value and value frameworks.
- Research on the economics of the supply, demand, and delivery of cancer prevention, detection/screening, treatment, and survivorship services, including:
- Amounts paid for cancer-related services, including variations in payments by insurers and patients, out-of-pocket costs, payment incentives/penalties, and discount payments for certain care providers (e.g., 340B);
- Effects of cancer-related payments and policies (e.g., insurance plan/benefit design, health care reforms) on the supply, demand, and delivery of cancer-related services, including differential impacts by types/characteristics of health care providers and health care delivery settings as well as impacts on diffusion/availability of new services;
- Impacts of cancer-related payments and policies on disparities/inequity in the supply, demand, and delivery of cancer-related services, including access to care and quality of care; and
- Influence and adequacy of the cancer care workforce and related organizational structures, including issues of training, composition, competition, distribution, and integration, on the supply, demand, and delivery of cancer-related services.
One goal of this framework is to emphasize that cancer health economics research extends beyond the examination of costs/expenditures. That is, this field incorporates the impacts of policies, programs, and environmental, societal, and organizational factors on the supply, demand, and delivery of cancer-related services. The intent of this framework is to encompass research from diverse perspectives that can deepen our understanding of the relationship of economic factors with the delivery of cancer-related services as well as economic studies of implementation/dissemination of cancer care programs. We view this framework as the first iteration of a living document, which will be updated and modified during and following the Future of Cancer Health Economics Research conference.
NCI's mission in conjunction with partners is to lead, conduct, and support cancer research across the nation to advance scientific knowledge and help all people live longer, healthier lives. Cancer health economics research is an important component of this mission and is critical to ensuring access to timely and high-quality cancer care across the care continuum. We look forward to engaging with the cancer community and health economics research stakeholders to advance this important topic.
Acknowledgement:
The views expressed here are those of the authors and do not represent any official position of the National Cancer Institute, National Institutes of Health, or Centers for Disease Control and Prevention.
Contributor Information
Michael T. Halpern, Healthcare Delivery Research Program, National Cancer Institute
Ya-Chen Tina Shih, Department of Health Services Research, University of Texas MD Anderson Cancer Center.
K. Robin Yabroff, Surveillance and Health Services Research, American Cancer Society.
Donatus U. Ekwueme, Division of Cancer Prevention and Control, Centers for Disease Prevention and Health Promotion
Cathy J. Bradley, University of Colorado Cancer Center, University of Colorado
Amy J. Davidoff, Cancer Outcomes, Public Policy, and Effectiveness Research (COPPER) Center, Yale University
Lindsay M. Sabik, Department of Health Policy and Management, University of Pittsburgh
Joseph Lipscomb, Department of Health Policy and Management, Rollins School of Public Health, and the Winship Cancer Institute, Emory University.
References
- 1.Mariotto AB, Enewold L, Zhao J, Zeruto CA, Yabroff KR. Medical Care Costs Associated with Cancer Survivorship in the United States. Cancer Epidemiol Biomarkers Prev. 2020;29: 1304–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halpern MT, Zhang F, Enewold L. Hospitalizations following cancer diagnosis: National values for frequency, duration, and charges. Journal of Clinical Oncology. 2020;38: 12039–12039. [Google Scholar]
- 3.Ekwueme DU, Zhao J, Rim SH, et al. Annual Out-of-Pocket Expenditures and Financial Hardship Among Cancer Survivors Aged 18–64 Years - United States, 2011–2016. MMWR Morb Mortal Wkly Rep. 2019;68: 494–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. 2011;103: 117–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yabroff KR, Lamont EB, Mariotto A, et al. Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst. 2008;100: 630–641. [DOI] [PubMed] [Google Scholar]
- 6.Morris S, Devlin N, Parkin D, Spencer D. Economic Analysis in Healthcare. United Kingdom: John Wiley & Sons, 2012. [Google Scholar]
- 7.Shapiro CL. Cancer Survivorship. N Engl J Med. 2018;379: 2438–2450. [DOI] [PubMed] [Google Scholar]
- 8.American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2019–2021. Atlanta: American Cancer Society, , 2019. [Google Scholar]
- 9.National Institutes of Health. Clarifying NIH Priorities for Health Economics Research. Available from URL: https://grants.nih.gov/grants/guide/notice-files/not-od-16-025.html [accessed Aug. 5, 2020].
- 10.Halpern MT, McCarthy S, Tuovinen P. Inclusion of economic outcomes in NCI grants: A portfolio analysis. Journal of Clinical Oncology. 2020;38: 7047–7047. [Google Scholar]
- 11.Healthcare Delivery Research Program, National Cancer Institute. Interagency Consortium to Promote Health Economics Research on Cancer (HEROiC). Available from URL: https://healthcaredelivery.cancer.gov/heroic/ [accessed Aug. 5, 2020].